Abstract
The conference discussed public goods and externalities created as by-products of the food system, including local development, obesity, air and water pollution, climate change, antibiotic resistance, and other public health issues. Multifunctionality is a framework that integrates these diverse issues and has been influential in international policy. This commentary focuses on arguably the most prominent public health issue at the moment: obesity. Though obesity could be considered another multifunctional dimension, its link to other conference topics is tenuous. Using obesity as an argument to promote local produce or achieve other multifunctional outcomes is very questionable. Framing obesity as an issue of poverty or food insecurity trivializes the continuing major problem of hunger worldwide.
Keywords: income, prices, obesity, fruits, vegetables, diet, BMI
INTRODUCTION
The traditional role of the agriculture and food system was fairly simple: supply food (and other commodity outputs like fiber). But the production and distribution of food also create by-products that are not traded on markets and many of them have characteristics of public goods and externalities; that is, these are outputs that either create benefits for or impose costs on society that are not reflected in market prices. Some of those outputs were discussed at the conference Food Systems and Public Health: Linkages to Achieve Healthier Diets and Healthier Communities, including landscape preservation, rural development, air and water pollution, climate change, biodiversity, antibiotic resistance, and population health (including obesity).
Most conference presentations focused on only one of these nonmarket outputs and this commentary, which primarily deals with obesity and affordability, is no exception. Nevertheless, it is useful to first remember that there exists a general framework to integrate those diverse issues, known as multifunctionality. The term is not well known in public health but has a history in international trade policy. I will briefly discuss multifunctionality in the next session because it provides a systems approach to coherently view the broad range of conference topics.
The remainder of the article focuses on a much narrower issue; namely, obesity and affordability. These are obviously issues central to the goal of the journal but were treated somewhat secondarily at the conference. Obesity is arguably the most prominent public health issue at the moment and there is no question that it is related to the food system. Because of obesity's saliency, many groups try to link their goals to obesity. Potentially relevant issues are poverty, affordability, food insecurity, fruit and vegetable production, and local production. Many of those were discussed at the conference and fit into the framework of multifunctionality, but the relationship to obesity is not always clear. There is no shortage of plausible arguments, although their applicability is often narrower than proponents assume. Intriguing hypotheses for some relationships have been proposed, but without taking a closer look at the data, it is difficult to assess their relevance. Though this commentary cannot be a comprehensive review of the evidence, I will comment on what empirical evidence suggests for those questions:
How is obesity changing in the United States (and across subpopulations)?
How does that relate to food prices, income, and affordability?
Is fruit/vegetable consumption declining?
Could more fruit/vegetables or local production make a noticeable dent into obesity trends?
MULTIFUNCTIONALITY
Multifunctionality refers to the linkage between commodity and noncommodity output production in agriculture or, more broadly, food systems. A good review of multifunctionality in the context of world trade was published by the US Department of Agriculture (USDA).1 The concept of multifunctionality provides a good first step of addressing many of the topics from the conference from a systems perspective. Of course, the basic idea that health, sustainability, and food production should be considered jointly is not novel and has appeared over time in a variety of fields (see, for example, Hamm2 in a previous volume of this journal). The Food Systems and Public Health conference mainly discussed negative externalities, including greenhouse gas emissions from agriculture and food distribution, pesticide runoff, water pollution from CAFOs, excess fertilizer use, and antibiotic resistance. Table 1 shows some outcomes that have been discussed within the context of multifunctionality of food systems. It categorizes outcomes into 4 broader groups (positive environmental outcomes, negative environmental outcomes, health outcomes, and social outcomes) and gives a few examples. In France, for example, high value is placed on the “scenic landscape” and “cultural heritage” arguments.
TABLE 1.
Non-market Products of a Multifunctional Food System
| Positive environmental outcomes | Negative environmental outcomes | Health and nutrition outcomes | Social outcomes |
|---|---|---|---|
| Flood control | Water and air pollution | Food security | Viable rural communities |
| Scenic landscape | Depletion of groundwater | Food safety | Traditional lifestyle |
| Biodiversity | Antibiotic resistance | Obesity | Cultural heritage |
| Sustainability | Contribution to climate change | Balanced diets |
In general, the linkage between food production/distribution and any of those outcomes is not fixed but influenced by policy and technological change. Unfortunately, empirical research between these outcomes is fairly limited. In fact, even the most basic economic issue, namely, whether commodity production and rural development are jointly created, remains unclear. This is particularly surprising because one of the traditional roles of agricultural subsidies has been to promote rural development.3 The evidence is to which extent price guarantees and incentives to increase production have benefited rural communities is mixed.
The basic idea of multifunctionality appears uncontroversial, but what made it controversial in international trade was that countries used claims of positive environmental externalities to circumvent international trade agreements and maintain traditional production subsidies or government supported prices. Multifunctionality provides an excellent and widely understood framework, but it needs to be filled with more empirical data.
OBESITY, INCOME, AND FOOD PRICES
A population's health and nutrition outcomes rank among the most important outcomes of multifunctional local, national, and international food systems. Food systems have been extraordinarily successful in developed countries of assuring a plentiful food supply, a dramatic change over the past 100 years. The major issue in developed and medium-income countries (like Brazil) now is obesity, no longer a shortage of food, which was experienced by a large fraction of the population even in countries like the United States or in Western Europe less than 100 years ago. Worldwide, of course, hunger remains very real, and undernourishment may currently affect a billion people,4 primarily in sub-Saharan Africa and South Asia.
Obesity has traditionally been the privilege of the wealthy—and it still is in many countries. So a somewhat surprising new development is the concern that low income or high food prices or limited access to food outlets (“food deserts”) cause obesity. Adam Drewnowski proposed a compelling hypothesis.5,6 He argues that the lowest-cost options to obtain a given amount of energy from food is through an energy-dense diet composed of refined grains, added sugars, and fats. The high energy density and palatability of sweets and fats increase energy intake. Lower income people tend to spend less on food overall and specifically less on lower energy-dense (but more costly) foods like fruits and vegetables. A related argument was in a clinical case report by Bill Dietz7 of an obese 7-year-old girl. Dietz argued that the increased fat content of food eaten during times when the family had insufficient income to buy a healthy diet was the primary reason but offered as an alternative hypothesis that obesity is an adaptive response to episodic food insufficiency.
There are other similarly plausible hypotheses that give virtually the opposite predictions and this is why we need to look closely at the data. The basic economic argument is that people consume more when they either get richer or prices fall.8 Moreover, the “full” price is not just money but also the time and effort it takes to obtain it. The full price of a home-prepared meal includes not just ingredients but travel to the store, time preparing the food, time cleaning up. As food becomes relatively cheaper and people become wealthier (both occurred in the past 50 years), the simple economic theory predicts that obesity rates should increase.8 Proponents of this theory would agree with Drewnowski's statement that “obesity in America is, to a large extent, an economic issue”5—even if they reach opposite conclusions about the effects.
There are countless other theories about obesity, so there is no shortage of theories. Even contradictory hypotheses can be correct if they apply to different situations—just as public health and clinical perspectives differ. Eventually, it is an empirical question what the primary effects are and whether there are special situations where other considerations apply. Here, the relevant questions are How is obesity changing in the United States (and across subpopulations)? How does that relate to food prices, income, and affordability? Is fruit/vegetable consumption declining? Could more fruit/vegetables or local production make a noticeable dent into obesity trends?
Let's start with some basic statistics. Price and income data may be important because they shed light on underlying economic trends. In the past 50 years, food prices have declined relative to prices of all other goods (about 10%–15%) and real income has increased substantially.8 Americans spend much less of their disposable income on food than ever—but this smaller share buys a much larger amount of calories (Figure 1).
FIGURE 1.
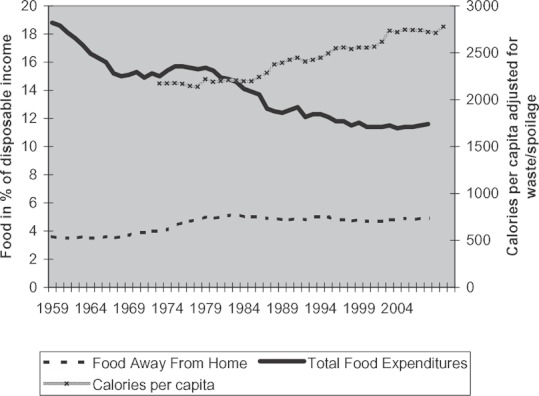
Share of disposable income spent on food has fallen but buys far more calories.
Almost all the decline came from food at home, the share of disposable income for food away from home increased a little bit but stayed relatively constant as shown in Figure 1. That, of course, means that Americans spent a lot more in absolute terms on food away from home and also that an increasing share of total food expenditures was for food away from home. In 1970, Americans spent one third of their food dollars on food away from home (ie, dollars for food away from home divided by all food expenditures), which grew to 39% in 1980, 45% in 1990, and 47% in 2001. Again, that can be interpreted as a price effect: the full price to obtain food has declined even more than price statistics indicate because of greater convenience, variety, and ubiquitous availability of food. Technological change has created an environment were a multitude of ready-to-eat foods are available anywhere at any time.9 Urban areas, rather than food deserts, have become food swamps. Food or images of food provide cues to eat and connect with survival instincts.10 The ubiquitous availability of foods can be overwhelming and artificially stimulate hunger and cravings for food, regardless of physiological needs,10 eventually resulting in what former Food and Drug Administration (FDA) chief David Kessler calls “conditioned hypereating.”9
The changes in our environment (not only for food but also for physical activity) have their counterparts in weight trends. Figure 2 shows the average body mass index (BMI), stratified by educational achievement. The most striking effect is the similarity in weight gain over time across groups, very consistent with an environmental change that affects everybody similarly. This parallel trend is not limited to educational subgroups and stratifying by other characteristics, including by income, shows similar parallel increases.11 The second noticeable feature of Figure 2 is that at every point in time, there is a pronounced difference in mean BMI by educational achievement, with higher weight among less educated groups. That could provide some evidence for the poverty–obesity link, although education is not income and the continuous educational gradient is not explained by a poverty affect.
FIGURE 2.
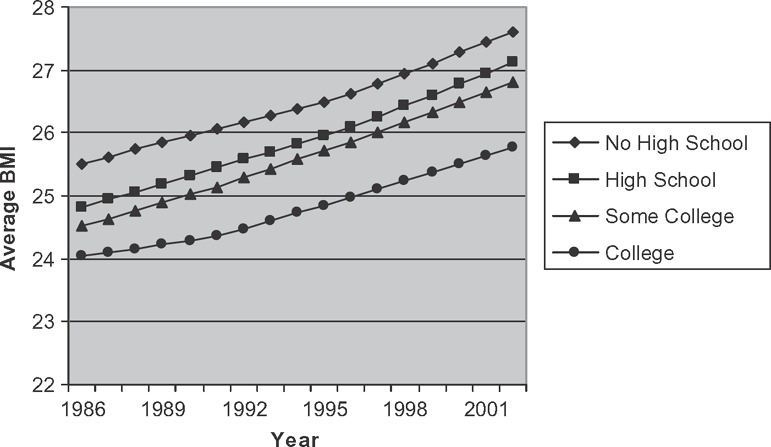
Trends in average body mass index by education.
Source: Author's calculation based on Behavioral Risk Factor Surveillance Survey.
So let us take a look at income. Unfortunately, it is difficult to draw similar time series for income because of the way data have been collected. But we can split the lowest and the highest income groups for two (or more) time points (Figure 3). There is indeed a big difference for women in the expected direction but not for men. If low income were the primary cause of obesity, why would this theory only apply to half the population? Even for women, the interpretation of the causal effect is questionable: there is an unambiguous association and the causal direction may be in the opposite direction. Longitudinal data show that women who are obese as adolescents or young adults are more likely to end in families with lower income and even in poverty, regardless of baseline status; however, this is not the case for men.12 The marriage market remains a very important determinant for a woman's socioeconomic status, even though increased labor market participation rates have substantially reduced its role compared to the past.
FIGURE 3.
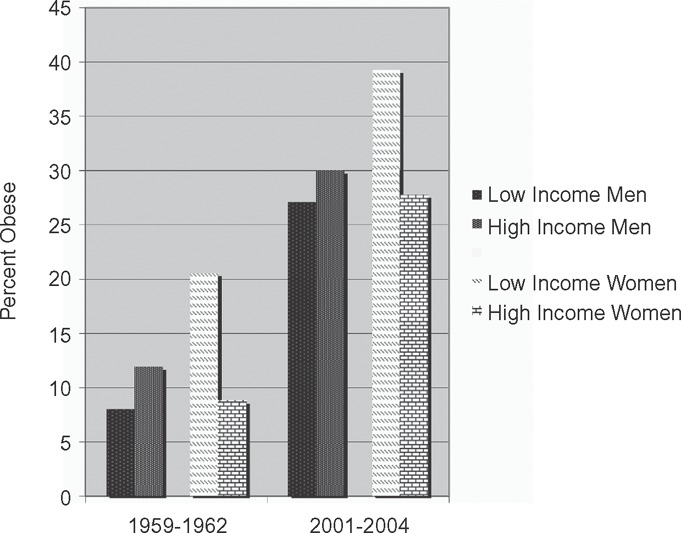
Income and obesity correlated among US women but not among men.
In summary, the biggest and most striking phenomenon is that the large average weight gains over time are fairly similar in all population. A second-order effect is the existence of consistent differences at every point in time between subpopulations. Those differences have been fairly stable in the last 20 years (which at least for income groups must be a reversal from 100 years ago). Changes in the differences between groups over time are minor in comparison, although they also exist. So a number of theories can be consistent with some parts of the data—for example, the association between poverty and obesity among women—but may be limited in their generalizability to time trends or the general population.
OBESITY AND FRUITS AND VEGETABLES
Weight gain is both about energy intake and energy expenditure and there have been changes in physical activity patterns, but those changes are more subtle than changes in dietary patterns and do not fit weight trends very well.13,14 On the other hand, there were big changes in eating patterns, including the shift toward eating out, increasing serving sizes, and much more snacking between meal times. The general tenor in public debates is that diet quality has deteriorated by a shift toward “junk food,” that cross-sectional disparities in obesity rates are caused by lack of access to “healthy food,” or that healthy food has become too expensive. The implication, which seemed to be believed by many conference participants, would be that increased fruit/vegetable supply (partly through more local production) can be an important tool in containing obesity, adding an additional multifunctional benefit to fruit/vegetable production.
There are some arguments in favor of this idea: Americans eat less fruits and vegetables than recommended by dietary guidelines; current production would be insufficient to achieve guideline consumption; individuals who eat more fruits/vegetables tend to be thinner. Economic trends may also shift incentives in a direction that is not conducive to healthier eating patterns. Relative to the consumer price index, sugar, sweets, fats, and oils all became cheaper; soft drinks were among the items that became (relatively) the cheapest.13 On the other hand, the price index for fresh fruit and vegetables averaged across a year appeared to increase faster, but this could be an artifact of increased availability out of season. Prices are higher out of season, but in earlier years there were no comparison prices because those foods were just not available at all.
However, preventing obesity is not about eating more food, regardless of how local or organic or fresh, but about eating less. Fruit/vegetable consumption has increased, not fallen, whereas obesity rates increased. Figure 4 shows the increase in availability for fresh produce, about 75 pounds per capita per year over the last 30 years. Total produce (which includes frozen, canned, other uses) has increased similarly. Moreover, the biggest increases are in the most recommended groups. Availability of dark green vegetables has gone up from 4 pounds per capita per year in 1970 to 29 pounds in 2007; deep yellow from 15 pounds in 1970 to 22 pounds in 2007. For specific examples, bell peppers increased from 2 to 7 pounds and broccoli from 1.5 to 8.7 pounds. In contrast, relatively little changed for starchy vegetables, like potatoes (which, of course, in absolute magnitudes account for much more).
FIGURE 4.
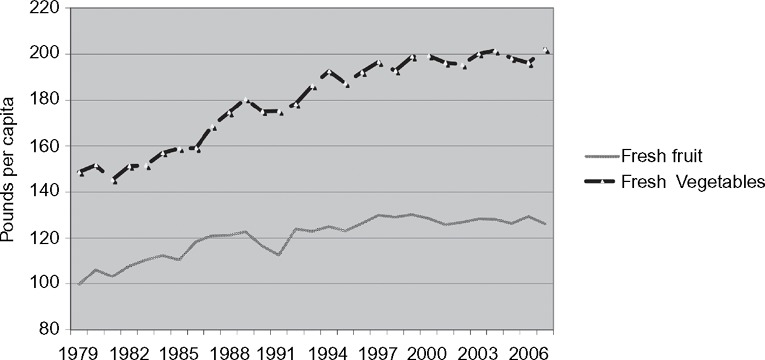
Fresh fruit and vegetables per capita availability.
There are other ways to calculate production and disappearance data, but essentially they all show the same qualitative picture; namely, that fruit and vegetable consumptions increased. The lowest numbers I could find were for loss-adjusted food availability. The USDA estimated that, in 1995, the fresh fruit and vegetable category had the greatest food losses at 19.6% and the added fats and oils category had losses amounting to 7.1%. Using the loss-adjusted categories, fruit consumption per capita increased by 15% and vegetable consumption by 23% from 1970 to 2007 but apparently without preventing obesity.
The problem may lie elsewhere. The 2005 US Dietary Guidelines introduced the concept of “discretionary calories” to address two dietary goals simultaneously: energy balance and the need for essential nutrients. The amount of calories for each goal differs and depends upon age, physical activity levels, and diet quality. The amount of discretionary calories is what is left over once individuals have satisfied essential nutrients through intake of recommended food items and can range from 130 calories for older sedentary women to over 500 calories for very physically active individuals. People who exceed their discretionary calories either have an energy imbalance or are at risk for malnutrition—or both. Discretionary calories should not be understood as the amount of junk food that can be consumed. The relationship between reduction in cancer risk and intake of fresh fruits and vegetables is continuous, so discretionary calories could also be used to increase fruit/vegetable consumption beyond guideline recommendations. But if candy and sodas become part of the diet, better to keep those calories under the threshold amount for discretionary calories.
However, that is not what we are likely to find anywhere. Instead, wherever we collected data, whether in Louisiana, poorer neighborhoods in Los Angeles, or minority communities in Northern California, the average number of excess calories from just a few selected snack items and soft drinks were beyond total discretionary calories and the discrepancy to guidelines was larger than for fruits/vegetables.15 Using 5-a-day as a standard because it has been the most widely promoted target (although now there are higher goals), the shortfall in fruits/vegetables was 10% to 20%, but excess discretionary calories were 60% to 120% (in both cases, Louisiana had the highest discrepancies). Most importantly, calories from snacks and sugar-sweetened beverages are higher than recommended discretionary calories in every population subgroup, even among people who say that they try to eat less to lose/maintain weight. Discretionary calories are more important predictors of BMI than fruit and vegetable consumption or physical activity levels at the population level. Increased physical activity reduced excess discretionary calories, although not to zero; increased fruit/vegetable consumption slightly reduced snack calories but by less than the additional calories that come with the fruit (at least cross-sectionally, we see little evidence for substitution).
The role of prices is unclear. A USDA study estimated annual retail price per pound and per serving for 69 forms of fruits and 85 forms of vegetables across the United States and more than half were estimated to cost 25 cents or less per serving.16 At that time, consumers could have even met a 7-a-day goal (3 servings of fruits and 4 servings of vegetables daily) for 64 cents, which is even affordable to low-income households, representing 16% of their daily food expenditures.16 Reducing prices may have little effect on behavior of low-income groups because they do not appear to be very price sensitive, meaning that even a large subsidy would result only in a very small increase in consumption.17 On the other hand, there are geographic price variations and higher produce prices have been linked to larger weight gain among children.18,19 The causal link is unclear, and the result could very well be caused by other confounding factors, although an intriguing hypothesis is that the effect may be through school food purchasing decisions. School food services are highly responsive to price variations given the large amount of purchases and budget constraints. USDA reimbursements for school meals are identical across the United States, so school food services facing higher costs will need to economize somewhere. Of course, this is exactly where linkages to local production could have a particularly high impact and several pilot programs have explored this.
DISCUSSION
The conference discussed public goods and externalities created as byproducts of the food system, including local development, air and water pollution, climate change, antibiotic resistance, and other public health issues. Multifunctionality is a framework that integrates these diverse issues and may help to provide a common framework to the diverse issues discussed at the conference.
In public health, the overriding policy concern these days is obesity. Though there are many attempts to link obesity with other goals (even organic production has been mentioned), I do not believe that there are many connections. Framing obesity as an issue of poverty or food insecurity is not very well supported by data at the population level. Weight has increased similarly in all population groups and lower income men are not more likely to be overweight than higher income men. With 1 billion people worldwide who face hunger as a real threat and are truly food insecure (and not obese), trying to make obesity a food insecurity story trivializes a major problem.
If people can get more produce, won't they eat less candy? That seems unlikely. More variety means more eating, not less; there is limited evidence that people substitute (outside clinical settings); and as far as obesity is concerned, juice is not different from soda. A 2009 report by the Institute of Medicine on food deserts also points to total consumption and that “greater fruit and vegetable consumption alone will not reduce weight without the qualification to moderate energy intake.”20 Unaffordability of produce may not be the problem as far as obesity is concerned—it is excess availability and affordability of other things.
In public health campaigns against tobacco, alcohol, and illicit drugs, messages have been direct and explicit—don't smoke, don't drink, and don't take drugs. In contrast, campaigns addressing obesity have shied away from that and instead have encouraged people to consume more fruits and vegetable and low-fat foods. Over the past few decades it appears that Americans have taken this advice and the USDA food disappearance data show increased fruit and vegetable consumption. This has not reduced the consumption of other foods. The largest increase in macronutrients was carbohydrates, with a smaller increase in fats.
Many policy interventions are focusing on “positive” messages, such as increasing fruit and vegetable consumption and increasing physical activity. But an emphasis on reducing discretionary calorie consumption, particularly sugar-sweetened sodas and salted snacks, may be a promising lever to reduce overweight and obesity and should receive more attention. The majority of adults exceed the amount of recommended discretionary calories for energy balance. Though increasing fruit and vegetable consumption may be a laudable goal for other health reasons, it is unlikely to be an effective tool for obesity prevention.
Acknowledgments
This article was prepared for the Healthy Eating Research Program of the Robert Wood Johnson Foundation. Partial funding was provided by NICHD, R01HD057193.
REFERENCES
- 1.US Dept of Agriculture. The Use and Abuse of Multifunctionality. Available at: http://www.ers.usda.gov/briefing/WTO/PDF/multifunc1119.pdf.
- 2.Hamm MW. Linking sustainable agriculture and public health: opportunities for realizing multiple goals. J Hunger Environ Nutr. 2008;3:169, 185. [Google Scholar]
- 3.Organisation for Economic Co-operation and Development. Multifunctionality in Agriculture: Evaluating the Degree of Jointness, Policy Implications. Paris, France: Organisation for Economic Co-operation and Development Publishing; 2008. [Google Scholar]
- 4.Food and Agriculture Organization of the United Nations. The State of Food Insecurity in the World. Food and Agriculture Organization; 2009. [Google Scholar]
- 5.Drewnowski A. Obesity and the food environment: dietary energy density and diet costs. Am J Prev Med. 2004;27(3, suppl):154, 162. doi: 10.1016/j.amepre.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6, 16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 7.Dietz WH. Does hunger cause obesity? Pediatrics. 1995;95:766, 767. [PubMed] [Google Scholar]
- 8.Variyam JN. The price is right: economics and the rise in obesity. Amber Waves. 2005.
- 9.Kessler DA. The End of Overeating—Taking Control of the Insatiable American Appetite. New York, NY: Rodale; 2009. [Google Scholar]
- 10.Cohen DA, Farley TA. Eating as an automatic behavior. Prev Chronic Dis. 2008;5:A23. [PMC free article] [PubMed] [Google Scholar]
- 11.Truong KD, Sturm R. Weight gain trends across sociodemographic groups in the United States. Am J Public Health. September 2005;95:1602, 1606. doi: 10.2105/AJPH.2004.043935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329:1008, 1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 13.Sturm R. Childhood obesity—what we can learn from existing data on societal trends, part 1. Prev Chronic Dis. 2005;2:A12. [PMC free article] [PubMed] [Google Scholar]
- 14.Sturm R. Stemming the global obesity epidemic: what can we learn from data about social and economic trends? Public Health. 2008;122:739, 746. doi: 10.1016/j.puhe.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen DA, Sturm R, Scott M, Farley TA, Bluthenthal R. Not enough fruits or vegetables or too much cookies, candy, salty snacks, or soda? Implications for obesity control from Los Angeles and Louisiana. Public Health Rep. 2010. p. 125. [DOI] [PMC free article] [PubMed]
- 16.Reed J, Frazão E, Itskowitz R. How Much Do Americans Pay for Fruits and Vegetables? US Dept of Agriculture; 2004. Agriculture Information Bulletin No. 790. [Google Scholar]
- 17.Dong D, Lin BH. Fruit and Vegetable Consumption by Low-income Americans: Would a Price Reduction Make a Difference? US Dept of Agriculture; 2009. Economic Research Report No. (ERR-70). [Google Scholar]
- 18.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119:1059, 1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Sturm R, Datar A. Food prices and weight gain during elementary school: 5-year update. Public Health. 2008;122:1140, 1143. doi: 10.1016/j.puhe.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute of Medicine and National Research Council. The Public Health Effects of Food Deserts: Workshop Summary. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]


