“We are continually faced with great opportunities which are brilliantly disguised as unsolvable problems.”
(John W. Gardner, 1912–2002)
Why is prevention of depression important?
The disease burden of depression is enormous: now reckoned by the World Health Organization (1996)(1) as the fourth leading contributor to the global burden of disease, and increasing to a position of greatest contributor to illness burden by 2030 in high-income countries (2). Prevalence is substantial and incidence is high, almost 50% of prevalence. At the same time, even under a hypothetical regimen of optimal evidence-based care, the burden of depression, measured in years lived with disabilities, can be averted by only about 25% (3). More precisely, when the interventions are evidence-based and when, in addition, the coverage is 100%, the percentage of years lived with disability avoided is about 34%. However, when coverage rates are more realistically 70%, then the percentage of years lived with disability avoided is about 26%. The implication is clear: needed are better treatments, dissemination (especially in low-income countries) and prevention.
My colleagues and I at the June, 2009 Pittsburgh Conference on Depression Preventions (see Acknowledgments) think of “prevention” as encompassing both preemption of incident and recurrent episodes of major depression; and protection from the developmental complications of depression. It is important, in other words, to take a long-term and developmental perspective on depression, across the life span, not limiting prevention to new episodes of depression in people who are either depression-naïve (first episodes) or with a previous history (recurrent episodes). The complications of depression include early school dropout, interpersonal problems, increase in both medical comorbidity and medical risk factors over time, worsening of cognitive impairment, impairment of mobility, excess disability, and increased mortality (both from suicide and from the interactions between depression and medical, especially cardiovascular and cerebrovascular, diseases). Depression diminishes both healthspan and lifespan. The ultimate goal of depression prevention is to protect and enhance both.
Is prevention (preemption, protection) of depression possible?
Yes: there are very high-quality data supporting the feasibility and efficacy of depression prevention (“preemption”) in at-risk youth (4), in post-stroke patients (5), and in older adults primary care setting (6). A meta-analytic review of 19 trials conducted in mixed-aged samples demonstrated a pooled incidence rate ratio of 0.78 (95% CI: 0.65–0.93), corresponding to a reduction in incidence of diagnosable depression of about 20% over one year. Participants in these trials received targeted, specific psychosocial interventions such as preventive cognitive behavioral therapy, interpersonal psychotherapy, problem-solving therapy, or bibliotherapy (7). With respect to prevention as “protection” (prolonging lifespan and healthspan), participation by older primary care patients in evidence-based depression care management strategies (in the PROSPECT study) (8) has been linked to lower rates of mortality from cancer at 4–5 year follow up (9). Another example of depression prevention as “protection” is provided by maintenance of recovery through prevention of recurrent episodes of major depression (10).
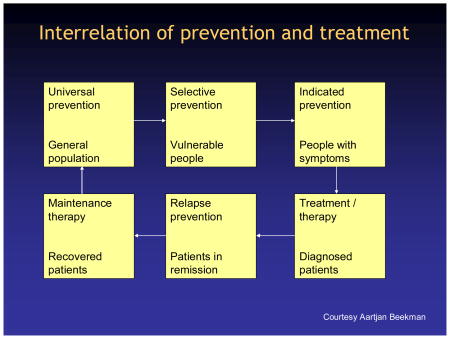
Using language from two Institute of Medicine reports on prevention of mental illness (1994; 2009) (11,12), most studies published to date have embodied either “selective” prevention (i.e., focusing on vulnerable but not yet symptomatic people) or “indicated” prevention (i.e., focusing on persons with sub-threshold symptoms of depression not meeting the diagnostic criteria for syndromal major depression). The reason for using selective and indicated strategies has to do with the need to maximize efficiency of depression prevention through generating the largest possible health gain in the population by targeting the smallest possible group in the most efficient way. From an epidemiological perspective, this amounts to maximizing the “attributable fraction” (i.e., the proportion of cases prevented if the toxic effects of a risk factor could be completely eliminated), while trying to minimize the number- needed-to-treat (NNT) to prevent one case of depression (13). In the studies cited above, NNT’s in the range of 7–9 are typical for “preemption” and about 4 for “protection” from recurrences (10). These estimates of NNT contrast favorably with an NNT of 21 in four large trials of statins for the prevention of a second myocardial infarction (14). The close interrelation of prevention and treatment is depicted below.
Furthermore, studies typically employ psychosocial and/or psychoeducational interventions (rarely pharmacotherapy, with the exception of (5), have empanelled 200–300 subjects, and have conducted observation for incident cases of major and/or minor depression during intervals of 9–12 months (but not usually longer). Published studies to date have not been informed by pathophysiological models of depression pathogenesis and have not yet addressed long-term prevention (beyond a year in most cases). This leaves unanswered the questions as to (1.) the possibility of more specific or personalized interventions based upon pathophysiological models and (2.) the durability of effect detected; that is, is the intervention delaying onset for a relatively short period of time, or is it preempting onset for longer periods of the remaining life span?
What are the challenges facing depression prevention research and practice?
As promising as the efficacy data are, many challenges remain to maximize both the scientific and public health impact of depression prevention research. Chief among these are (1.) the need for more efficacy trials in specific target groups (e.g., post-partum depression, low SES groups and ethnic minorities, and family caregivers); (2.) better pathophysiological models of depression prevention to inform the choice of more specific, biologically based, and personalized interventions in preempting depression and in protection from its complications; (3.) further investigation of the cost-effectiveness of depression prevention ; and (4.) further study of using the internet to disseminate preventive interventions that can be shared globally and reduce health disparities, especially when the local health care system cannot provide care to people who need it.
Pathophysiological approaches to developing models of depression prevention could embrace studies of genetic contributions to the likelihood of onset, the time period of risk, and the likelihood of risk reduction using psychosocial or psychopharmacologic strategies (15). Since most adults are resilient to depression after a disabling medical event or other negative life events such as bereavement, a deeper understanding of genetic liability could help to improve the cost-benefit ratio of depression prevention efforts. Another illustrative example is based on work targeting prevention of emergent major depression during interferon-alpha therapy for hepatitis C (16). Data from this work poses an important question: can one reduce or prevent the incidence of cytokine-reduced depression by protecting or improving sleep quality? We are suggesting the possibility that a deeper, biologically informed understanding of the pathways to depression could lead to more specific, personalized, and efficient strategies than those used to date.
The cost-effectiveness of depression prevention has begun to receive the attention it deserves. Early models utilizing bootstrapping approaches to cost-effectiveness ratios suggest a high probability that self-help approaches based on cognitive-behavioral intervention to prevent depression onset generate better health effects against lower costs, relative to wait list (17). Promising work like this confronts policy makers and citizens alike with an important question: how much are we willing and able to pay to prevent depression? A clearer and more widely disseminated understanding of the costs of depression, both financial and personal, may lead to a consensus that depression prevention services hold great value for individual persons and for society (18).
The use of the internet to disseminate depression prevention strategies is promising and deserves much more study than it has received to date. An example of this is the question of whether improving sleep quality via internet-based CBT approaches to chronic insomnia could lead to reductions in the incidence and/or severity of mental disorders (like depression) and substance use disorders. In order to move forward, however, investigation into internet-based prevention strategies will benefit from the creation of guidelines for reasonable expectations for ethical internet research, for example, assuring that users know that the Website cannot provide crisis intervention.
In the context of public health impact, the experience of the Netherlands in reaching the target populations is instructive. The Netherlands have one of the world’s most efficient and population-oriented health care systems; thus, it is not surprising that the intellectual and health policy leadership for development and dissemination of depression prevention has occurred there probably more than anywhere else. That said, however, a relatively small proportion of persons living with minor depression take advantage of depression prevention services offered in The Netherlands. Possibilities to increase participation rates include strategies addressed to patients and to health care and social service organizations. Strategies aimed at potential participants in depression prevention services could and probably should include media campaigns to reduce stigma (“promotion” and “universal” prevention, to use the IOM’s 2009 lexicon), as well as media campaigns stressing the possibility to prevent depression. Organizational solutions could probably include the offering of coping-with-depression courses through the internet, further embedding preventive services in primary care, and further embedding coping-with-depression courses in broader community interventions. Inevitably, approaches like these will entail efforts to increase awareness in health professionals about the availability and efficacy of preventive services and systematic screening of potential participants. Our hope is that this commentary will serve to move the field in this direction.
Acknowledgments
The following colleagues provided helpful comments on earlier drafts of this article:
Mary Amanda Dew, Ph.D.; Department of Psychiatry, University of Pittsburgh School of Medicine
Filip Smit, Ph.D.; Netherlands Institute of Mental Health and Addiction, and the Department of Epidemiology and Biostatistics, EMGO Institute for Health and Care Research, VU University Medical Centre
Aartjan Beekman, M.D., Ph.D.; Department of Psychiatry, VU University Medical Center and EMGO Institute for Health and Care Research, Amsterdam
Pim Cuijpers, Ph.D.; Department of Psychology, VU University and EMGO Institute for Health and Care Research
Supported by P30 MH071944, R21 NR011149, the University of Pittsburgh Endowment in Geriatric Psychiatry, the John A. Hartford Foundation, and the American Foundation for Suicide Prevention
Footnotes
The following colleagues were participants in the Pittsburgh Conference on Prevention of Depressive Disorders, June 25–27, 2009. This article is informed by the conversations that took place at the conference.
Aartjan Beekman, M.D., Ph.D.; Terry Brugha, M.D.; Pim Cuijpers, Ph.D.; Mary Amanda Dew, Ph.D.; Linda Garand, Ph.D., RN, CS; Judy Garber, Ph.D.; Ulrich Hegerl, M.D.; Amy M. Kilbourne, Ph.D., M.P.H.; Eric Lenze, M.D.; Cathy Mihalopoulos, Ph.D.; David Mohr, Ph.D.; Ricardo F. Muñoz, Ph.D.; Charles F. Reynolds III, M.D.; Robert G. Robinson, M.D.; Barry Rovner, M.D.; Filip Smit, Ph.D.; Geesje Thomassen, M.S.; Annemieke van Straten, Ph.D.; Benjamin Van Voorhees, M.D., M.P.H.;
Reference List
- 1.World Health Organization. The Global Burden of Disease. Cambridge, MA: Harvard University Press; 1996. Global Health Statistics: A compendium of incidence, prevalence and mortality estimates for over 200 conditions. [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrews G, Issakidis C, Sanderson K, et al. Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry. 2004;184:526–533. doi: 10.1192/bjp.184.6.526. [DOI] [PubMed] [Google Scholar]
- 4.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;301:2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson RG, Jorge RE, Moser DJ, et al. Escitalopram and problem-solving therapy for prevention of poststroke depression: Randomized controlled trial. JAMA. 2008;299:2391–2400. doi: 10.1001/jama.299.20.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van’t Veer-Tazelaar PJ, van Marwijk HW, van Oppen P, et al. Stepped-care prevention of anxiety and depression in late life: a randomized controlled trial. Arch Gen Psychiatry. 2009;66:297–304. doi: 10.1001/archgenpsychiatry.2008.555. [DOI] [PubMed] [Google Scholar]
- 7.Cuijpers P, van SA, Smit F, et al. Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. Am J Psychiatry. 2008;165:1272–1280. doi: 10.1176/appi.ajp.2008.07091422. [DOI] [PubMed] [Google Scholar]
- 8.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 9.Gallo JJ, Bogner HR, Morales KH, et al. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146:689–698. doi: 10.7326/0003-4819-146-10-200705150-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reynolds CF, Dew MA, Pollock BG, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354:1130–1138. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine, Committee on Prevention of Mental Disorders, Division of Biobehavorial Science and Mental Disorders. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academy Press; 1994. [Google Scholar]
- 12.Institute of Medicine. Preventing mental, emothional, and behavioral disorders among young people: Progress and prossibilities. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 13.Smit F, Ederveen A, Cuijpers P, et al. Opportunities for cost-effective prevention of late-life depression: An epidemiological approach. Arch Gen Psychiatry. 2006;63:290–296. doi: 10.1001/archpsyc.63.3.290. [DOI] [PubMed] [Google Scholar]
- 14.Therapeutics Initiative: Evidence based drug therapy: do statins have a role in primary prevention? [accessed February 17, 2006];2006 at http://www.ti.ubc.ca/PDF/48.pdf.
- 15.Lenze EJ, Munin MC, Skidmore ER, et al. Onset of depression in elderly persons after hip fracture: Implications for prevention and early intervention of late-life depression. J Am Geriatr Soc. 2007;55:81–86. doi: 10.1111/j.1532-5415.2006.01017.x. [DOI] [PubMed] [Google Scholar]
- 16.Lotrich FE, Ferrell RE, Rabinovitz M, et al. Risk for depression during interferon-alpha treatment is affected by the serotonin transporter polymorphism. Biol Psychiatry. 2009;65:344–348. doi: 10.1016/j.biopsych.2008.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smit F, Willemse G, Koopmanschap M, et al. Cost-effectiveness of preventing depression in primary care patients: randomised trial. Br J Psychiatry. 2006;188:330–336. doi: 10.1192/bjp.188.4.330. [DOI] [PubMed] [Google Scholar]
- 18.Smit F, Cuijpers P, Oostenbrink J, et al. Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ. 2006;9:193–200. [PubMed] [Google Scholar]


