Abstract
Computed tomography (CT) and magnetic resonance imaging (MRI) are increasingly valuable tools for assessing the urinary tract in adults and children. However, their imaging capabilities, while overlapping in some respects, should be considered as complementary, as each technique offers specific advantages and disadvantages both in actual inherent qualities of the technique and in specific patients and with a specific diagnostic question. The use of CT and MRI should therefore be tailored to the patient and the clinical question. For the scope of this article, the advantages and disadvantages of these techniques in children will be considered; different considerations will apply in adult practice.
Keywords: Magnetic resonance imaging, Computed tomography, Ultrasonography, Child, Kidney, Urinary tract, Diagnostic imaging
Introduction
Computed tomography (CT) was invented by Sir Godfrey Hounsfield and was introduced into medical practice in 1973 [1–3]. The technique relies on the original theory that one can determine what is inside a box by taking X-ray “readings” at all angles around the object (tomograms). A computer then takes input from the X-rays at various angles to create an image of the object in slices, hence the name computed tomography. CT is therefore an X-ray technique and uses ionizing radiation. X-rays (whether conventional, plain radiographs or CT) give pictorial information on the density of an object or material. A CT image is therefore a pictorial demonstration of all the densities in the object, with high-density material (bone, calcium, metalwork) being represented as white and low-density materials being dark grey or black (air, fat). Their density can be measured in Hounsfield units (HU), and this can give the radiologist important information about the type of material (or tissue). Water is used as the reference point and has a value of between –7 and +7 HU (typically 0 HU), bone and other calcification will be of higher density (≥500 HU), fat will be of lower density (–25 to –250 HU), and soft tissues are in the range +10 to +60 HU.
Modern CT scanners are very fast and can scan the abdomen and pelvis in typically 5–7 s once the planning view (the ‘scout’ or ‘scanogram’) has been set up. This has great advantages in children, as for the most part, children will not need to have a general anesthetic to ensure they keep still. Babies can undergo “feed and wrap” and will generally sleep through the scan; toddlers and preschool children can be scanned with encouragement and caregiver support (or occasionally with mild sedation), and older children are easily able to tolerate the short scan times. Modern scanners typically have a slice thickness of <1 mm (0.6–0.75 mm) depending on the manufacturer. This allows for very detailed information that can be reconstructed in other planes, such as sagittal and coronal projections, which are often very helpful to the physician in understanding the image. Three dimensional (3D) images can also be produced in postprocessing, allowing rotating visualization of any part of the image that is required. CT provides a high spatial resolution image (the ability to distinguish two structures an arbitrarily small distance from each other as separate) with low noise, giving exquisite anatomical depiction, but it cannot give as much information with respect to processes within different tissues types, such as inflammation or necrosis, unless these are quite pronounced. The use of intravenously administered contrast medium helps in this respect and would be given routinely unless the main clinical question was regarding calcification or high-density objects (such as when looking for renal calculi). There is almost no indication in children for doing both pre- and postcontrast scans as part of the same examination. The only occasion for routinely performing a precontrast (unenhanced) scan is when evaluating calculi, and if the examination is solely for that purpose, then there is no indication to routinely perform a postcontrast scan as well. Conversely, if there is no diagnostic concern regarding calculi, then only a postcontrast scan should be performed, as there is so little additional diagnostic yield (if any) from doing both a pre- and postcontrast scan, and the significant radiation dose from the additional precontrast scan cannot be justified. All patients should be asked for any history of contrast allergy (or other severe allergies) before contrast is given intravenously (IV). Contrast is always most safely administered in the setting of good effective volume and hydration. Moreover, in the setting of a depressed glomerular filtration rate (GFR), consideration should be given to both hydration and alkalinization and, in some instances, there may be a role for the use of postcontrast dialysis. Planning for imaging children with depressed GFR is best accomplished in a multidisciplinary fashion, with input from both radiologist and nephrologist. Intravenously administered contrast must not be given in severe renal failure unless the patient will subsequently be dialyzed. In mild renal failure, a risk assessment (based on the potential benefit of the examination) must be performed by the clinician, and the patient must be well hydrated beforehand. CT is a high-radiation-dose technique and as such is used much more cautiously and infrequently in children than in adults, with children being many times more biosensitive to radiation than adults. Background radiation is typically 2–3 mSv per year, and a CT scan of the abdomen and pelvis is approximately 2–6 mSv, or the equivalent of 200–300 chest X-rays. Much effort is being made by pediatric radiologists to reduce radiation doses in children, especially in CT imaging, and information regarding this can be found at http://www.pedrad.org/associations/5364/ig/. Consideration should be given to performing specialized imaging studies that are elective in nature in facilities with pediatric expertise and pediatric imaging protocols, if these are available.
Magnetic resonance imaging (MRI) provides much greater contrast between different soft tissues [4] than does CT, as it relies on obtaining a radiofrequency (RF) signal from alignment and subsequent relaxation of protons in hydrogen atoms in water in the body. Soft tissue throughout the body will have varying water contents depending on cell types and the processes going on in and around those cells (e.g. normal different tissues, inflammation, tumor, infection, etc). An MR scanner uses a powerful magnetic field to align the nuclear magnetization of protons of hydrogen atoms in water (intra- and extracellular), and RF fields are then applied to alter the alignment of this magnetization, causing hydrogen nuclei to produce a rotating magnetic field that is detectable by the scanner. When RF fields are reversed, the protons relax to their normal state and give off a tiny RF signal that is detected by the scanner and is used to construct the image. Different tissues return to their equilibrium state at different rates. By changing the parameters of the scan, this effect is used to create an image that depicts the different tissues by showing the contrast between them. In a typical MRI scan, several different pulse sequences are performed to best exploit the different signals between tissues and give the most information. The main advantage of MRI over CT is that it gives far better contrast resolution (the ability to distinguish the differences between two arbitrarily similar but not identical tissues) and thus its ability to demonstrate changes between normal and pathological tissues. A sequence may last between a few seconds to several minutes, with most routine sequences lasting 1–3 min. Between five and ten sequences would usually be performed. MRI can produce images in any plane desired, and this is achieved by the radiographer or technician when setting up scan parameters. Sequences can be selected specifically to demonstrate particular qualities of tissues, such as water content. For example, with particular values of the echo time (TE) and the repetition time (TR), which are basic parameters of image acquisition, a sequence may take on the property of T2 weighting. On a T2-weighted scan, water- and fluid-containing tissues are bright (most modern T2 sequences are actually fast T2 sequences), and fat-containing tissues are dark. The reverse is true for T1-weighted images. Damaged tissue tends to develop edema, which makes a T2-weighted sequence sensitive for pathology and generally able to distinguish pathologic tissue from normal tissue. Heavily T2-weighted sequences are especially useful in the urinary tract, as water-containing structures are bright white, such as the collecting system and the bladder.
MRI contrast agents are frequently used. Most common of these is gadolinium, which is given intravenously. These agents work by shortening the T1 or T2 relaxation time of protons nearby. Reduction of T1 relaxation time results in a hypersignal with a reduced T2 relaxation time, thus reducing both T2 and T2* signals. Gadolinium is therefore of most benefit in T1-based sequences. A rare but severe complication of gadolinium use is nephrogenic systemic fibrosis (NSF), which causes fibrosis in various tissues and organs. Patients with poor renal function are considered a greater risk of NSF, and therefore, gadolinium contrast agents must only be used with caution in these patients. As a result, gadolinium-containing contrast is now considered contraindicated in patients with an estimated GFR <60 ml/min and especially <30 ml/min [5]. Depressed GFR encompasses both acute and chronic kidney injury. As such, individuals with transient renal dysfunction should also be considered at risk, even though their usual GFR may be normal.
MRI scans will usually take 30–45 min and therefore generally require a general anesthetic in children from approximately 1–6 or 7 years of age. Older children are usually able to cooperate, but if they are unable to remain still and limit any movement for this length of time, they may also require a general anesthetic. Younger children (<12 months) may undergo feed and wrap or sedation. Further details of the practical aspects are covered in the pediatric MRI literature [6–8] (Table 1).
Table 1.
Comparison of advantages and disadvantages between computed tomography (CT) and magnetic resonance (MR) imaging modalities
| CT | MR |
|---|---|
| Uses ionizing radiation, high-dose procedure | Uses magnetic resonance, no ionizing radiation |
| Excellent spatial resolution | Excellent contrast resolution |
| Actual scanning time measured in seconds (typically <10 s) | Actual scanning time measured in minutes (typically 45 min) |
| Rarely requires general anesthetic in children | Frequently requires general anesthetic in children, depending on age |
| Excellent at showing calcification | Poor at showing calcification (signal void) |
| Poor at showing edema or pathological changes in specific tissue types | Excellent at showing edema and pathological changes in specific tissue types |
| Usually requires intravenous contrast (unless looking for calcification when not required) | Usually requires intravenous administration of contrast (but certain sequences can be tailored if this is contraindicated) |
| No known risk of nephrogenic systemic fibrosis (NSF) | Risk of NSF (rare, but renal patients believed to be at increased risk) |
| Widely available | Less widely available, especially for children |
| Less expensive | Expensive |
| Usually available as an emergency imaging technique | Not routinely available as an emergency technique |
| No significant contraindications | Contraindicated in patients with any internal ferrous objects (pacemakers, defibrillators, recent orthopedic metalware, other implanted metallic devices, metallic foreign bodies) |
| Open-style scanners | Generally quite enclosed scanners – risk of claustrophobia |
| Can only scan in one plane (but can do reconstructed images later) | Can scan in any plane |
| Few artefacts | Prone to artefacts depending on sequence type (especially motion artifact) |
Imaging the urinary tract – which modality to use for first-line examination?
In imaging the urinary tract in children, the modality of choice for the initial examination will almost universally be ultrasound (US). US is inexpensive, immediate, painless, requires no sedation or anesthetic, is widely available, and is radiation free. In children, the urinary tract is easily visualized, as usually children have less body fat than adults, and the kidneys and bladder are relatively superficial structures. Children should be scanned both supine and prone, and the posterior approach (with the child lying prone) often gives the best anatomical detail of the kidneys. US can be used to scan in any plane at the discretion of the operator, and whereas the technique is entirely operator dependent, most centers have staff with a high level of skill. In most pediatric centers, it is considered completely unacceptable to proceed to CT or MRI in routine practice unless US had already been performed and had been unable to fully answer the diagnostic question. Acute multiorgan trauma would be the main exception to this. It is common practice in adult medicine to perform a CT scan of the abdomen and pelvis as the first-line examination for renal colic. In children, the first-line examination, even in renal colic, should ideally be US (on radiation dose risk vs. benefit considerations), recognizing that a few children will still need to proceed to CT. However, there is some variation in this practice between North America and Europe and on the availability of US expertise out of hours. Renal colic in children is much less common than in adults, even in children with known stone disease, and their stones pass more readily. US can show renal calculi with exquisite detail, demonstrating stones down to approximately 1–2 mm in diameter, and is also highly sensitive in the bladder. It is less sensitive, however, in the ureters, which may be obscured by bowel and other pelvic structures, so in the context of a normal US and ongoing clinical features suggestive of calculi (colicky pain, hematuria, known existing stone disease), CT may still be indicated. There is further discussion of this topic in the section “Calcification in the urinary tract”. US is the first-choice examination for all other pathologies relating to the kidney and urinary tract.
The use of CT and MR for specific clinical indications
Congenital conditions
In pediatric practice, many congenital conditions of the urinary tract are demonstrated in utero on antenatal scans, whereas some are only detected in infancy or later due to subsequent complications. Ninety percent of fetal kidneys can be identified by 17–20 weeks of gestation and 95% by 22 weeks. Both antenatally and postnatally, US remains the examination of choice in demonstrating kidney and urinary tract anatomy. Structural urinary tract anomalies include renal dysplasia, renal hypoplasia, renal aplasia, multicystic dysplastic kidney, pelviureteric junction obstruction, duplication anomalies, fusion anomalies, renal ectopia, ureteroceles, cystic kidney diseases, and posterior urethral valves. All of these may be demonstrated by US, with additional information being acquired in some cases by other modalities (such as nuclear medicine imaging or fluoroscopy). MRI may subsequently be useful in these patients, as illustrated in Fig. 1 for cystic disease, either in the further workup following US [7, 9] when the clinical question has not been resolved, or when the child presents with (or has) complications that remain unexplained by US or require further delineation [10–12]. Heavily T2-weighted sequences (water-based sequences) are very useful in demonstrating dilatation of the urinary tract secondary to congenital anomalies, such as duplex kidneys with dilated moieties and occult moieties in a previously undiagnosed duplex kidney [13] (Fig. 2), and for demonstrating the exact anatomy of fusion anomalies, such as a crossed, fused, ectopic kidney and horseshoe kidney [4, 6].
Fig. 1.
Magnetic resonance image: coronal T2 sequence in a 6-month-old girl with autosomal dominant polycystic kidney disease showing multiples high-signal cysts throughout both kidneys
Fig. 2.
Magnetic resonance imaging: an unexpected right-sided duplex kidney in a 7-month-old girl whose anatomy could not be delineated by ultrasound, with a tiny lower moiety that is almost hidden by the dilated upper moiety (arrow)
CT arteriography (CTA) is sometimes performed in instances of known horseshoe kidney when surgery is being planned. This is to optimally delineate the multiple vessels that often supply these kidneys before surgery is undertaken. Pelviureteric junction obstruction can usually be diagnosed adequately on US, but a crossing vessel may be demonstrated by MRI (Fig. 3) [14], which cannot be visualized by US; in very gross hydronephrosis, MRI may give a better demonstration of the anatomy (Fig. 4).
Fig. 3.
Magnetic resonance imaging: a 9-year-old boy with right-sided flank pain with a reconstructed postcontrast image showing an inferior pole “crossing” vessel (artery) (arrow) causing right-sided hydronephrosis
Fig. 4.
Magnetic resonance imaging: T2-weighted sequence demonstrating the extent of bilateral pelviureteric junction obstruction, nondilation of ureters, and normal bladder, confirming the obstruction to be at the renal pelvis on both sides
Very complex urogenital anomalies, such as cloacal anomalies in female patients, are usually imaged by US and fluoroscopy in the first instance, but further cross-sectional imaging is invariably required. MRI may offer satisfactory depiction of the anatomy, but frequently, the workup has to occur very soon after birth so that an intermediate management plan can be made before definite surgery can be performed when the infant is older. In this situation, MRI is rarely able to offer sufficient spatial resolution to allow full understanding of the anatomy in these very small patients. In a few very select cases, CT, with a combined distal loopogram and micturating cystogram performed at the time of the scan, as well as contrast intravenously with the scan delayed to excretory phase, can offer exceptional 3D visualization of the entire urogenital tract (Fig. 5). There is little value in a conventional CT alone in these cases, and the routine use of CT is absolutely not advocated.
Fig. 5.
Computed tomography: Reconstructed 3D images showing the complicated anatomy of the urogenital tract in a 3-month-old girl with a cloacal anomaly; the entire urogenital system is demonstrated in one study
Infection
Most commonly, infection of the lower urinary tract presents clinically and is treated empirically. However, in a few more complicated cases, US will be performed to look for complications, such as abscess formation or pyelonephritis, within the kidneys and for the presence of underlying contributory factors, such as stone disease or previously undiagnosed structural anomalies. In most instances, US is able to resolve these clinical issues and is clearly the modality of choice for assessing infection (both in the acute stage and at follow-up). If US cannot answer the diagnostic question, further cross-sectional imaging may sometimes be useful. In the acute setting, with a very ill patient and suspected sepsis related to the urinary tract, CT may add further information regarding, for example, abscess rupture or retroperitoneal fluid (or pus) collections (Fig. 6). CT is useful in showing calcification and extrarenal complications in xanthogranulomatous pyelonephritis, if this has not already been confirmed by US. MRI may be of value after the acute episode for demonstrating underlying structural anomalies if these have not been determined by US.
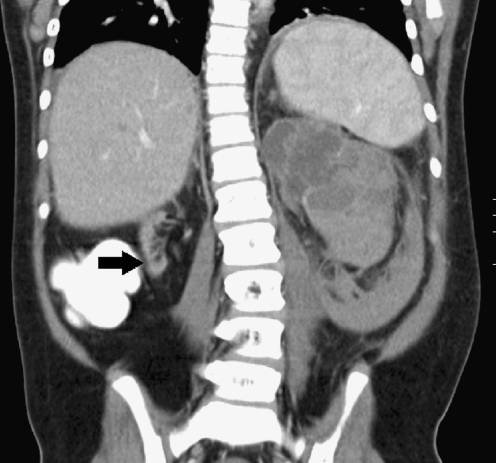
Fig. 6.
Computed tomography: a 15-year-old girl with chronic renal failure on peritoneal dialysis with recent onset of abdominal pain and signs of sepsis. The shriveled right kidney (arrow) is the expected size of both kidneys, but the left kidney shows acute pyelonephritis and is therefore enlarged, dilated, pus-filled, and has ruptured into the retroperitoneum
Trauma
In the acute setting of trauma in children, US is once again the first-line technique in the emergency room. US can quickly demonstrate whether the kidney is still vascularized, if there is physical damage (fracture, laceration, avulsion) of the kidney, and provide some information regarding surrounding complications. If the trauma is believed to be confined solely to the kidney and the child is stable, it may not be necessary to proceed to any further immediate imaging. However, it is frequently the case that these patients have been involved in a complex trauma, and as such, multiple injuries may have occurred. In most cases, major renal injuries are associated with injuries to other major organs, and renal trauma occurs in 8–10% of patients with significant blunt or penetrating abdominal trauma [15, 16]. In this instance, CT is usually performed straight from the emergency room. CT will demonstrate direct trauma to the kidney and to any other intra-abdominal organs and may show retroperitoneal injuries or complications better than US [17]. Typical findings include contusions (shown as ill-defined or sometimes sharply marginated areas of reduced enhancement and excretion), nonexpanding subcapsular hematomas (appearing as a hyperattenuating fluid collection between the renal parenchyma and the renal capsule, at times deforming the underlying kidney), perinephric hematomas (an ill-defined, hyperattenuating fluid collection located between the Gerota fascia and the renal parenchyma), renal lacerations (jagged or linear parenchymal disruptions that can contain fresh or clotted blood), renal lacerations with collecting system involvement (which frequently produce extravasation of urine or contrast agent), and renal segmental infarction appearing as well-delineated, linear or wedge-shaped, often multifocal and nonenhancing areas that extend through the parenchyma in a radial or segmental orientation. Thrombosis, dissection, and laceration of segmental renal arteries are primary causes of segmental infarctions, and such infarctions are frequently associated with other renal injuries. Severe injuries include a shattered or devascularized kidney (which appears nonenhancing, with CTA showing a blind-ending renal artery), ureteropelvic junction (UPJ) avulsions, and complete laceration or thrombosis of the main renal artery or vein. CT of the urinary tract should usually be obtained in severe pelvic trauma prior to surgery. MRI has no indication in the acute setting of trauma. Very occasionally, it may have some value in the follow-up of renal trauma, but in children, this would usually be by US.
Vascular
Both CT and MRI can give excellent information with respect to normal vascular supply to the kidneys and wider urinary tract and in the context of vasculopathies. US would be the first-line investigation, but if anatomical delineation is required – for example, for surgical planning – then CT or MRI can be performed at the surgeon’s and radiologist’s discretion. CT will give better spatial resolution with the CT scan being performed in the arterial phase and allows 3D reconstruction of the vascular tree but at a considerable radiation dose. The clinician must be sure that sufficient information cannot be obtained by another method before proceeding. MRI is increasingly able to offer detailed vascular information with no radiation dose, and this should be considered as an entirely viable alternative in cooperative children (Fig. 7). At the time of writing this article, conventional angiography remained the gold standard for demonstrating subtle abnormalities in the renal vasculature, but it is both invasive and carries a relatively high radiation dose. However, in the diagnosis of subtle renal artery stenosis, for small arteriovenous malformations of the kidney, and for tiny aneurysms such as in polyarteritis nodosa or Wegner’s granulomatosis, it is still the investigation of choice. It is no longer indicated in the diagnosis or workup of renal tumors prior to surgery.
Fig. 7.
Magnetic resonance imaging: gadolinium-enhanced MR angiography demonstrating arterial anatomy in an 11-year-old girl with a known horseshoe kidney
MRI plays an important role in the workup of children waiting for renal transplant. Whereas initial assessment of their native vessels [aorta, inferior vena cava (IVC), iliac and femoral vessels] may be by US, proceeding to MRI may be necessary if the US is technically inadequate (due to the presence of bowel gas or other structures) or if it is indeterminate. Conventionally, gadolinium contrast agents have been given to best illustrate the vessels, but in patients who are known to be in renal failure (hence the need for transplant), gadolinium is no longer given due to the risk of NSF. In these patients, MR angiography (MRA) is still achieved using tailored sequences [true fast imaging with steady-state precession (FISP) and time-of-flight (TOF) sequences], which obviate the need for intravenously administered contrast. It is also helpful in patients who have had renal transplant and in whom the anatomy may be difficult to demonstrate by US.
Calcification in the urinary tract
Stone disease and calcification relating to the urinary tract in children deserves special mention, as its imaging management differs to that in adults. US is a highly effective imaging tool when looking for calcification (nephrocalcinosis) and calculi within the kidney. Subtle nephrocalcinosis may be demonstrated by using a high-resolution probe when it has not been demonstrated by a conventional linear probe, and the pediatric sonographer should always use both techniques if nephrocalcinosis is being sought. There is no indication to use CT or MRI when diagnosing nephrocalcinosis in children unless there is a specific concern regarding the additional presence of calculi, which may be difficult to delineate by US in the presence of particularly florid nephrocalcinosis.
Children’s smaller body habitus allows good visualization of even tiny calculi within the collecting system, parenchyma, and bladder. If the ureters are dilated, US may also show calculi in the upper and lower third of the ureter but remains consistently poor at demonstrating calculi in the middle third of the ureter. In a select group of patients, it may be appropriate to proceed to CT, but CT should not be routine imaging for stone disease children. It is, however, highly sensitive (97%) and specific (96%) for urinary tract calculi and is undoubtedly an excellent technique in this respect [18]. Children who may benefit from CT include those with a high body mass index (BMI) in whom US cannot sufficiently penetrate soft tissues for adequate visualization, those in whom US is not tolerated, children with severe scoliosis in whom there is not a suitable acoustic window to access the kidneys, children who continue to have symptoms of stone disease in which no calculi have been demonstrated by repeated US, and children in whom a history of stone disease is known but symptoms are out of proportion to US findings. It must be remembered that many children will have recurrent calculi, and it is therefore highly undesirable to perform a high radiation dose examination on every occasion for an underlying benign condition with a normal life expectancy. If CT is requested, it should be performed with a low-dose technique and without intravenously administered contrast (which would obscure any calcific focus) [19, 20].
Neoplastic
Many tumors may involve the urinary tract depending on the organ of origin and the age of the child. Renal malignancies represent about 6% of cancer diagnoses in children <15 years of age. Wilms tumor is by far the most common of the renal tumors, representing approximately 95% of cases overall and 96% in children <5 years (Fig. 8).
Fig. 8.
Computed tomography showing the extent of a large, left-sided Wilms tumor in a 2-year-old girl with thrombus extending the full length of the inferior vena cava (IVC) and into the right atrium (between arrows)
In all instances, the first imaging should be by US, which can confirm the presence of the mass and can usually (but not always) determine the organ of origin. However, further cross-sectional imaging is indicated for further anatomical delineation, information on tissues characteristics, and to establish staging. In centers with pediatric MRI, this is absolutely the imaging modality of choice: it provides a wealth of information regarding the tumor itself, provides a base-line for follow-up (thus avoiding repeated CTs), and can provide accurate staging. Sequences will typically include T1- and T2-weighted sequences, short-tau inversion recovery (STIR) sequences, apparent diffusion coefficient (ADC) sequences, and postgadolinium contrast-enhanced 3D fast low-angle shot (FLASH) sequences in a combination of axial and coronal planes. ADC sequences are relatively new in abdominal imaging (but have been used extensively in the brain for some time). These sequences give information about how easily water can diffuse in and between cells; thus, a tumor with densely packed cells will return low signal intensity and will appear dark on this MRI sequence. If it, or a part of it, is undergoing necrosis, it will return a higher (whiter) signal intensity. This is especially useful when monitoring a tumor to assess its response to treatment such as chemotherapy and to follow-up for recurrence. MRI can give information as to IVC and renal vein patency (Fig. 8) if this has not already been determined with certainty by US. Detailed MRA may also be performed, if necessary, to allow surgical planning. In centers with no access to MRI, then CT still provides good information, recognizing that it cannot supply tissue-specific information as MRI and that it incurs a heavy radiation burden. Follow-up of treated tumors should be by US where possible, although many cancer protocols determine that MRI (or CT) should be performed at specifically determined intervals.
Renal functional MRI
US, CT, and MRI all provide good anatomic images [21] of the kidney and urinary tract, but MRI (both in adults and children) has developed very rapidly over recent years and has great potential in the near future to change the way the urinary tract is imaged after the initial US. Uniquely, MRI can also give functional information on the kidneys [4, 22], unlike the other cross-sectional modalities. Traditionally, nuclear medicine studies have been employed for this purpose, but they give poor spatial resolution and provide only relative information rather than absolute values with respect to renal function. MRI is therefore alone in being able to give both anatomical and functional information. Functional renal imaging techniques such as contrast-enhanced MR renography [23, 24], and unenhanced techniques such as diffusion-weighted imaging (DWI) and blood-oxygen-level-dependent (BOLD) imaging, have shown considerable promise in evaluating renal function in health and disease. Whereas this is a relatively new area in clinical terms, it is rapidly advancing and crossing over from being a research technique to offering a real clinical alternative to existing techniques for assessing renal function [25]. Technically, it is no different performing this in children than in adults, but – as with all MRI in children – the rate-limiting step for the technique is the child’s ability to remain completely still through a long scan without the need for general anesthesia. It is likely, therefore, that it will be incorporated into the repertoire of renal imaging for older children in the reasonably near future but probably not for younger children unless there is a very specific indication.
-
Contrast-enhanced MR renography:
The basis of the technique relies on dynamic contrast enhancement of the kidneys using MRI to monitor transit of contrast material, typically a gadolinium chelate, through the renal cortex, the medulla, and the collecting system. Most gadolinium contrast agents are cleared by glomerular filtration and pass through capillaries and renal tubules, causing renal tissue signal intensity to increase. By analyzing renal tissue enhancement as a function of time, clinically important single-kidney parameters such as renal blood flow [24], GFR, and cortical and medullary blood volumes can be determined and can be plotted graphically to generate various functional parameter curves. Split renal function can be calculated [25]. Current indications in adult imaging include functional imaging in renal artery stenosis and assessing potential allograft dysfunction in the early postoperative period, potentially avoiding the need for biopsy to distinguish between acute tubular necrosis and acute rejection. It should be noted that as this technique relies on administration of gadolinium as a contrast agent, it is not suitable for patients with renal failure, due to the risk of NSF.
-
Diffusion-weighted MRI:
DWI has traditionally been used in imaging stroke victims, as it is very sensitive in detecting acute ischemia. The ADC calculation can be used in vivo for quantifying the combined effects of capillary perfusion and diffusion. This technique was referred to above in tumor assessment; however, it also has applications in assessing renal insufficiency with studies showing good correlation between GFR and ADC values, highlighting the potential role for evaluating renal dysfunction in native kidneys. DWI also appears to have a future role in renal allograft evaluation and renal artery stenosis.
-
Blood-oxygen-level-dependent (BOLD) MRI:
BOLD MRI can be used for noninvasive but direct measurement of renal oxygenation [26]. It exploits the paramagnetic effect of deoxyhemoglobin for acquisition of images sensitive to local oxygen concentration. Again, it has application in the context of renal artery stenosis and renal allograft dysfunction but also in diabetic nephropathy
Conclusion
Imaging of the urinary tract in children relies on US as the first-line imaging modality; however, MRI has an invaluable role to play, with CT playing a lesser part. Considerations specific to children revolve around radiation dose issues with CT and the need (or not) for a general anesthetic in MRI. It is crucial that the clinical question is clearly established and the study chosen is tailored to the specific child after discussion between the clinician and the radiologist. MRI is the technique of choice for imaging tumors and congenital anomalies when these cannot be satisfactorily delineated by US, and it should generally be regarded as an excellent advanced problem-solving technique. CT is indicated in multisystem trauma and in some children with renal calculi. Functional MRI is rapidly developing in the adult world, and some applications are becoming relevant in children. Center-specific expertise may lead to a certain study being performed in one setting versus a different study in another. This factor may be an important consideration in choosing which modality is appropriate. For elective imaging, referral of the patient to a center with pediatric expertise for superior study should be considered, if it is a realistic option. Ultimately, it is the collaboration between the nephrologist and the radiologist that will lead to the best imaging modality for each patient.
Self-assessment questions
(Answers appear following the reference list)
- Which examination has the highest sensitivity for detecting renal-tract calculi in children?
- CT with contrast enhancement
- CT without contrast enhancement
- CT with contrast enhancement and delayed images to show the level of obstruction
- MRI using a T1-weighted sequence
- US in the hands of an experienced operator who is aware of the clinical history
- Which patient cannot have an MRI examination?
- A child with claustrophobia
- A child with end-stage renal failure in whom gadolinium is therefore contraindicated
- A baby 5 days old who is on a ventilator
- A child who had a CT the previous day
- A child with a pacemaker
- Which series has the highest radiation dose?
- Enhanced CT of the abdomen and pelvis with a delayed series
- Enhanced CT of the abdomen and pelvis without a delayed series
- MRI with T1, T2, post-gadolinium TI and ADC sequences, in coronal and axial planes, of the abdomen and pelvis, with a delayed series
- Unenhanced CT of the abdomen only, followed up by unenhanced CT of the abdomen (only) 4 weeks later
- MRI of the abdomen and pelvis followed up by CT of the abdomen and pelvis 6 weeks later
- Which of the following is poorly demonstrated on MRI?
- Urine
- Blood
- Calcium
- Renal medulla
- Renal cortex
- Regarding NSF, which of the following is false?
- NSF does not occur in healthy patients with normal renal function
- The risk of NSF is increased in patients with a low GFR
- The relationship between NSF and MRI contrast agents has only been recognized in the last 5 years
- The risk of NSF is not reduced by dialysis
- All types of gadolinium contrast agents pose a similar risk of NSF in patient with renal failure
Footnotes
Answers
1. b. CT without contrast enhancement has the highest sensitivity for detecting calculi but carries a heavy radiation dose penalty. It is therefore NOT the first examination of choice in children. US should always be used in the first instance, and CT only when there is still diagnostic difficultly. Contrast may obscure the presence of stones, as it is also of high density (white).
2. e. A pacemaker is generally considered an absolute contraindication to MRI, as it may become deprogrammed or pulse erratically in the strong magnetic field. (In absolutely exceptional cases, a clinical decision can be made to turn some pacemakers off or turn them to fixed-pulse mode). A child with claustrophobia may have MRI under sedation or general anesthetic if clinically indicated. Modern sequences often obviate the need for gadolinium in patients with end-stage renal failure. The age of the patient and the previous imaging history would not affect the clinical decision to request MRI.
3. a. This series involves scanning through the abdomen and pelvis on two occasions. The absence or presence of intravenously administered contrast agent makes no difference to radiation dose. MRI does not involve radiation.
4. c. Calcium (such as in renal calculi) contains no water and therefore does not have protons that are easily influenced by magnetic fields, and as such, it returns almost no signal (signal void) on all sequences and is difficult to detect.
5. e. Not all gadolinium contrast agents are the same. Omniscan and Magnevist are thought to pose increased risk due to the chelate to which the gadolinium is attached, with these compounds being more likely to release free gadolinium ions into the body. Dotarem is currently considered to be the least likely agent to allow release of free gadolinium ions.
References
- 1.Ambrose J, Hounsfield G. Computerized transverse axial tomography. Br J Radiol. 1973;46:148–149. doi: 10.1259/0007-1285-46-552-1023. [DOI] [PubMed] [Google Scholar]
- 2.Hounsfield GN. Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol. 1973;46:1016–1022. doi: 10.1259/0007-1285-46-552-1016. [DOI] [PubMed] [Google Scholar]
- 3.Hounsfield GN. Computed medical imaging. Science. 1980;210:22–28. doi: 10.1126/science.6997993. [DOI] [PubMed] [Google Scholar]
- 4.Grattan-Smith JD, Jones RA. MR urography in children. Pediatr Radiol. 2006;36:1229–1132. doi: 10.1007/s00247-006-0222-2. [DOI] [PubMed] [Google Scholar]
- 5.Kanal E, Barkovich AJ, Bell C, Borgstede JP, Bradley WG, Jr, Froelich JW, Gilk T, Gimbel JR, Gosbee J, Kuhni-Kaminski E, Lester JW, Jr, Nyenhuis J, Parag Y, Schaefer DJ, Sebek-Scoumis EA, Weinreb J, Zaremba LA, Wilcox P, Lucey L, Sass N. ACR guidance document for safe MR practices: 2007. AJR Am J Roentgenol. 2007;188:1447–1474. doi: 10.2214/AJR.06.1616. [DOI] [PubMed] [Google Scholar]
- 6.Grattan-Smith JD, Little SB, Jones RA. MR urography in children: how we do it. Pediatr Radiol. 2008;38(Suppl 1):S3–S17. doi: 10.1007/s00247-007-0618-7. [DOI] [PubMed] [Google Scholar]
- 7.Grattan-Smith JD, Jones RA. Magnetic resonance urography in children. Magn Reson Imaging Clin N Am. 2008;16:515–531. doi: 10.1016/j.mric.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Grattan-Smith JD. MR urography: anatomy and physiology. Pediatr Radiol. 2008;38(Suppl 2):S275–S280. doi: 10.1007/s00247-008-0793-1. [DOI] [PubMed] [Google Scholar]
- 9.Grattan-Smith JD, Jones RA. MR urography: technique and results for the evaluation of urinary obstruction in the pediatric population. Magn Reson Imaging Clin N Am. 2008;16:643–660. doi: 10.1016/j.mric.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Greenbaum LA. Renal dysplasia and MRI: a clinician’s perspective. Pediatr Radiol. 2008;38(Suppl 1):S70–S75. doi: 10.1007/s00247-007-0586-y. [DOI] [PubMed] [Google Scholar]
- 11.Little SB, Jones RA, Grattan-Smith JD. Evaluation of UPJ obstruction before and after pyeloplasty using MR urography. Pediatr Radiol. 2008;38(Suppl 1):S106–S124. doi: 10.1007/s00247-007-0669-9. [DOI] [PubMed] [Google Scholar]
- 12.Cerwinka WH, Damien Grattan-Smith J, Kirsch AJ (2008) Magnetic resonance urography in pediatric urology. J Pediatr Urol 4:74–82, quiz 82-83 [DOI] [PubMed]
- 13.Lipson JA, Coakley FV, Baskin LS, Yeh BM. Subtle renal duplication as an unrecognized cause of childhood incontinence: diagnosis by magnetic resonance urography. J Pediatr Urol. 2008;4:398–400. doi: 10.1016/j.jpurol.2008.01.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calder AD, Hiorns MP, Abhyankar A, Mushtaq I, Olsen OE. Contrast-enhanced magnetic resonance angiography for the detection of crossing renal vessels in children with symptomatic ureteropelvic junction obstruction: comparison with operative findings. Pediatr Radiol. 2007;37:356–361. doi: 10.1007/s00247-007-0416-2. [DOI] [PubMed] [Google Scholar]
- 15.Kawashima A, Sandler CM, Corl FM, West OC, Tamm EP, Fishman EK, Goldman SM. Imaging of renal trauma: a comprehensive review. Radiographics. 2001;21:557–574. doi: 10.1148/radiographics.21.3.g01ma11557. [DOI] [PubMed] [Google Scholar]
- 16.McAninch J. Renal injuries. In: Gillenwater J, Grayhack J, Howards S, Duckett J, editors. Adult and pediatric urologyMosby. Mo: St Louis; 1996. pp. 539–553. [Google Scholar]
- 17.Lee YJ, Oh SN, Rha SE, Byun JY. Renal trauma. Radiol Clin North Am. 2007;45:581–592. doi: 10.1016/j.rcl.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Smith RC, Verga M, McCarthy S, Rosenfield AT. Diagnosis of acute flank pain: value of unenhanced helical CT. AJR Am J Roentgenol. 1996;166:97–101. doi: 10.2214/ajr.166.1.8571915. [DOI] [PubMed] [Google Scholar]
- 19.Kalra MK, Maher MM, D’Souza RV, Rizzo S, Halpern EF, Blake MA, Saini S. Detection of urinary tract stones at low-radiation-dose CT with z-axis automatic tube current modulation: phantom and clinical studies. Radiology. 2005;235:523–529. doi: 10.1148/radiol.2352040331. [DOI] [PubMed] [Google Scholar]
- 20.Memarsadeghi M, Heinz-Peer G, Helbich TH, Schaefer-Prokop C, Kramer G, Scharitzer M, Prokop M. Unenhanced multi-detector row CT in patients suspected of having urinary stone disease: effect of section width on diagnosis. Radiology. 2005;235:530–536. doi: 10.1148/radiol.2352040448. [DOI] [PubMed] [Google Scholar]
- 21.Kirsch AJ, Grattan-Smith JD, Molitierno JA., Jr The role of magnetic resonance imaging in pediatric urology. Curr Opin Urol. 2006;16:283–290. doi: 10.1097/01.mou.0000232051.66718.34. [DOI] [PubMed] [Google Scholar]
- 22.Rohrschneider WK, Haufe S, Clorius JH, Troger J. MR to assess renal function in children. Eur Radiol. 2003;13:1033–1045. doi: 10.1007/s00330-003-2005-6. [DOI] [PubMed] [Google Scholar]
- 23.Jones RA, Schmotzer B, Little SB, Grattan-Smith JD. MRU post-processing. Pediatr Radiol. 2008;38(Suppl 1):S18–S27. doi: 10.1007/s00247-007-0616-9. [DOI] [PubMed] [Google Scholar]
- 24.Martin DR, Sharma P, Salman K, Jones RA, Grattan-Smith JD, Mao H, Lauenstein TC, Burrow BK, Tudorascu DL, Votaw JR. Individual kidney blood flow measured with contrast-enhanced first-pass perfusion MR imaging. Radiology. 2008;246:241–248. doi: 10.1148/radiol.2461062129. [DOI] [PubMed] [Google Scholar]
- 25.Chandarana H, Lee VS. Renal functional MRI: Are we ready for clinical application? AJR Am J Roentgenol. 2009;192:1550–1557. doi: 10.2214/AJR.09.2390. [DOI] [PubMed] [Google Scholar]
- 26.Hofmann L, Simon-Zoula S, Nowak A, Giger A, Vock P, Boesch C, Frey FJ, Vogt B. BOLD-MRI for the assessment of renal oxygenation in humans: acute effect of nephrotoxic xenobiotics. Kidney Int. 2006;70:144–150. doi: 10.1038/sj.ki.5000418. [DOI] [PubMed] [Google Scholar]