Abstract
Objective
To investigate whether psychosocial factors (i.e., depression, anxiety, and well-being) moderate educational gradients in interleukin-6 (IL-6) levels using data from the Survey of Mid-life Development in the U.S. (MIDUS). The influences of educational attainment and psychosocial factors on IL-6 in middle aged and older adults were also examined.
Design
Telephone interviews and mail surveys were utilized to collect educational attainment and psychosocial information from participants (N = 1028). Respondents also participated in an overnight clinic visit, during which health information and a fasting blood sample was obtained.
Main Outcome Measures
Serum levels of IL-6.
Results
. Greater educational attainment predicted lower levels of IL-6 independent of age and gender, although this effect was attenuated after taking health behaviors, body mass index, waist-to-hip ratio, and chronic illnesses into account. Psychological well-being interacted with education to predict IL-6, such that for those with less education, higher well-being was associated with lower levels of IL-6.
Conclusion
The findings indicate a strong association between education and inflammation, which can be further moderated by psychosocial factors. The health benefits associated with psychological well-being were particularly evident for individuals with low educational attainment.
Keywords: education, well-being, affect, inflammation
Morbidity and mortality associated with cardiovascular disease, diabetes, and cancer vary across socioeconomic gradients, with the lower strata at increased risk for adverse events (for a review, see Adler & Rehkopf, 2008). Emotional processes can also influence physical health, with worse prognoses for individuals with depression and anxiety and better outcomes associated with positive affect and psychological well-being (Pressman & Cohen, 2005; Seeman, 1996; Strine et al., 2008). What is not well understood is how socioeconomic and psychosocial factors interact, that is, work synergistically to predict overall health risk. The present study investigated how education and psychosocial factors independently and interactively predicted levels of one proinflammatory marker, the pleiotropic cytokine interleukin-6 (IL-6). The main objectives were to determine whether positive and negative aspects of psychosocial functioning moderated levels of IL-6 in individuals at increased risk for physiological dysregulation and disease because of low educational attainment.
Socioeconomic Standing (SES) and Inflammatory Processes
Across various measures of SES, individuals in lower strata face an increased likelihood of adverse health outcomes compared to individuals in more favorable socioeconomic positions (González, Artalejo, & Calero, 1998; Loucks et al., 2006; Loucks et al., 2009; Marmot et al., 1991). Associations between SES and markers of inflammation and inflammatory diseases have also been documented. As SES decreases, levels of circulating IL-6 increase, an association documented with several different indices of individual and community-level socioeconomic position, including education, income, wealth, and occupational standing (Gruenewald, Cohen, Matthews, Tracy, Seeman, 2009; Koster et al., 2006; Loucks et al., 2006; Petersen et al., 2008; Pollitt et al., 2008).
Interleukin-6
Inflammation is thought to be involved in the etiology of many diseases, including cardiovascular and rheumatological diseases, osteoporosis, and Alzheimer’s disease (Ershler & Keller, 2000). The important role of localized vascular inflammation in atherosclerosis is now widely accepted, and many treatment options directly or indirectly (e.g., aspirin, statins) aim to reduce inflammation so as to reduce cardiovascular risk (Ridker et al., 2008; Ross, 1999). Elevated levels of IL-6 are predictive of future adverse health events in both healthy and clinical populations, even after controlling for both lifestyle and other clinical risk factors (e.g., Ershler & Keller, 2000; Ridker, Rifai, Stampfer, & Hennekens, 2000). IL-6 is also linked to socioeconomic and psychosocial adversity; low SES and depression (both clinical and subclinical) predict higher serum levels of IL-6 (Gruenewald et al., 2009; Petersen et al., 2008; Howren, Lamkin, & Suls, 2009; Penninx et al., 2003).
Psychosocial Factors and Inflammatory Processes
Depressed mood and anxiety have been found to predict higher levels of IL-6 in both healthy and clinical populations (Al, Kronfol, Seymour, & Bolling, 2005; Dentino et al., 1999; Howren et al., 2009; Miller, Stetler, Carney, Freedland, & Banks, 2002; Penninx et al., 2003; Pitsavos et al., 2006; Tiermeier et al., 2003; Suarez, 2003), although some investigations have reported a lack of association, or occasionally an inverse relationship between negative affect and IL-6 (e.g., Annique et al., 2005; Lespérance, Frasure-Smith, Théroux, & Irwin, 2004; Steptoe, Kunz-Ebrecht, & Owen, 2003; Whooley et al., 2007). Inconsistent findings may reflect differences among populations examined, the factors that were controlled, and variation in the assessment of emotion, ranging from affective state to psychiatric diagnoses.
Relatively fewer investigations have examined positive psychosocial functioning and its relationship to inflammatory markers. Embeddedness in social networks, emotional expressiveness, internal locus of control, and sense of purpose and commitment have all been linked to favorable health outcomes, including reduced incidence of stroke, reduced likelihood of hospital readmission following cardiovascular complications, and reduced all-cause mortality (Chida & Steptoe, 2008; for a review, see Pressman & Cohen, 2005). We focus in this investigation on hedonic well-being, which refers to positive affect, happiness, and life satisfaction, and eudaimonic well-being, which refers to evaluative judgments about one’s purpose and meaning in life and whether personal talents and abilities are being realized (Ryff, 1989; Ryff & Keyes, 1995). Growing evidence supports each type of well-being as predictive of mental and physical health outcomes (Keyes, Shmotkin, & Ryff, 2002; Ryan & Deci, 2001; Ryff & Singer, 2008). Older women scoring higher on eudaimonic, but not hedonic well-being, were shown to have lower plasma IL-6 levels (Friedman, Hayney, Love, Singer, & Ryff, 2007). A study in Britain found that positive affect was inversely related to IL-6 in women, but not in men (Steptoe, O’Donnell, Badrick, Kumari, & Marmot, 2008).
Not well understood is the interplay of education, emotion, and cognitive factors (e.g., affect and psychological well-being) in accounting for high or low levels of IL-6. The primary goal of this investigation was to examine whether psychosocial factors, both positive and negative, could moderate educational gradients in IL-6. In particular, the objective was to clarify whether the adverse effects of low educational attainment on circulating IL-6 levels were moderated by the maintenance of a negative or positive cognitive outlook and affective state. We hypothesized that among those with low educational attainment, (a) greater anxious and depressive symptoms would be associated with higher IL-6 levels, while (b) hedonic and eudaimonic well-being would predict lower IL-6. Before testing for these statistical interactions, we also examined the main effects of educational attainment and psychosocial factors on IL-6, after controlling for demographic factors (age, gender), health behaviors (smoking status, alcohol and caffeine consumption, physical activity level, and medication usage), and health status indicators (body mass index (BMI), waist-to-hip ratio (WHR), and number of chronic health conditions). Higher educational attainment and well-being were hypothesized to still be predictive of lower levels of IL-6, after taking into account the control variables, while higher anxious and depressive symptoms were hypothesized to result in higher levels of IL-6.
Method
Participants
MIDUS was begun in 1995 with a national sample of Americans aged 25 to 74, including twins, recruited through a random digit dialing (RDD; Brim, Ryff, & Kessler, 2004). Of the original 7,108 MIDUS I participants, 1,914 were twins. Data collection focused on sociodemographic and psychosocial assessments obtained through phone interviews and self-administered questionnaires (SAQs). In 2004, these assessments were repeated (MIDUS II). The retention rate from MIDUS I to MIDUS II was 75% (adjusted for mortality).
Biological data were collected on a subset of MIDUS II participants. To be eligible, respondents had to complete the telephone and mail surveys and be able and willing to travel to one of three General Clinical Research Centers (GCRC) for an overnight visit. Of those invited to participate, 43% agreed. The primary reasons for refusal were not wanting to travel to the clinic, having other obligations, or being too busy. This response rate is somewhat lower than other epidemiological studies involving a visit to a clinic (e.g., 57% response rate in the Cardiovascular Health Study; Fried et al., 1998). Nonetheless, the biological sample was comparable to the MIDUS II pool from which it was recruited on most sociodemographic factors (age, gender, marital status, income) and multiple health characteristics (subjective health, chronic conditions, health symptoms, BMI). Biological respondents were significantly better educated than nonparticipants, although more than half of the sample had only a high school education or some college.
Data are reported for a sample of 463 males and 565 females ranging in age from 35–86 years (Mean: 58.01, SD: 11.64). These individuals completed a two-day visit to a GCRC, during which they provided a complete medical history and medication information, underwent a physical exam with a physician, and provided a fasting blood draw around 0700 on the morning of the second day. The blood sample was obtained prior to any caffeine or nicotine consumption for the day. Participants also completed a set of SAQs during the stay at the GCRC.
Measures
Education
During the telephone interviews, respondents were asked how many years of school or college they had completed. Twelve response categories ranged from no school to completion of a professional degree. Education was treated as a continuous variable.
Negative Affect
Subscales from the Mood and Anxiety Symptom Questionnaire (MASQ) measured anxious symptoms and were completed during the GCRC visit. The MASQ contains two subscales addressing components of anxiety: General Distress Anxious symptoms and Anxious-Arousal symptoms. The General Distress Anxious scale contains items indicative of anxious mood and general somatic symptoms that occur with anxiety disorder while the Anxious Arousal scale contains items specific to anxiety disorder regarding tension or hyperarousal (Watson et al., 1995). The General Distress Anxious scale had eleven items and an internal consistency of .82 while the Anxious Arousal scale had seventeen items and an internal consistency of .80.
The Center for Epidemiological Studies Depression (CES-D) scale was also included as a well validated instrument for assessing depressive symptoms in large surveys (Radloff, 1977). This 20-item scale had an internal consistency of .89. The CES-D scale was included in these analyses to allow for comparisons of the relationship between depressive symptoms and inflammation between the MIDUS sample and other samples (Penninx et al., 2003, Blumenthal et al., 2003, Bremmer et al., 2008). In the MIDUS cohort, 12.9% of the sample met the criterion for major depression used with the CES-D, namely scores ≥ 16. This percentage is higher than the national yearly prevalence of major depressive disorder (6.7%; Kessler, Chiu, Demler, & Walters, 2005) and higher than the Healthy, Aging, and Body Composition Study cohort (4.8%; Penninx et al., 2003), though comparable to the Longitudinal Aging Study Amsterdam (14.8%; Bremmer et al., 2008).
Well-being
Eudaimonic well-being was based on Ryff’s theoretical framework and included six scales: Autonomy, Environmental Mastery, Personal Growth, Positive Relations with Others, Purpose in Life, and Self-Acceptance (Keyes et al., 2002; Ryff, 1989). Each scale had seven items, and internal consistency for these scales ranged from .69 to .85.
Hedonic well-being was assessed with the High Positive Affect subscale from the MASQ (Watson et al., 1995). This scale contained fourteen items and had an internal consistency of .93.
Demographic Information
Age and gender information was collected from the survey assessments at MIDUS II.
Health Behaviors
Smoking status (categorized as never-smoker, former-smoker, and current-smoker; never-smokers as referent category), alcohol consumption (total number of alcoholic drinks consumed in the past month), caffeine consumption (average number of servings of coffee, tea, or other caffeinated beverages consumed per day), and physical activity level (average number of minutes of moderate or vigorous physical activity per week) were all included as control variables given evidence linking these behaviors with fluctuations in IL-6 (O’Connor & Irwin, 2010). Medication usage, including anti-hypertensives, cholesterol medications, steroid usage, and antidepressants were also included as control variables (dummy coded to indicate current use or non-use). These medications have all shown to affect IL-6 levels (Jain & Ridker, 2005; Kenis & Maes, 2002; Tatli & Kurum, 2005).
Health Status Indicators
BMI and WHR were based on measurements taken by GCRC staff. The chronic health conditions variable was a sum score of self-reported physician diagnosed conditions, including heart disease, high blood pressure, circulation problems, blood clots, heart murmur, transient ischemic attack or stroke, anemia or other blood disease, cholesterol problems, diabetes, asthma, emphysema or chronic obstructive pulmonary disease, tuberculosis, thyroid disease, peptic ulcer disease, cancer, colon polyps, arthritis, glaucoma, cirrhosis or liver disease, or depression. Continuous variables for all health status indicator variables were included in statistical analyses.
Interleukin-6
Serum IL-6 levels were measured with the Quantikine® high-sensitivity enzyme linked immunosorbent assay (ELISA) kit (R & D Systems, Minneapolis, MN). All values were determined in duplicate; any value over 10 pg/mL was re-run in diluted sera to fall on the standard curve. Assays were completed according to manufacturer’s instructions. The laboratory intra-assay coefficient of variance was 4.09% and the inter-assay coefficient of variance was 13% (as determined by a low and high IL-6 serum pool included in each assay).
Statistical Analyses
Both IL-6 and BMI were log-transformed to achieve normal distributions. All predictor variables included were mean-centered.
Separate hierarchical multiple regression analyses were run for each psychosocial factor. Bivariate associations between education or the psychosocial factors and IL-6 were tested in the first model. The second model added adjustments for demographic factors, which consisted of age and gender when education was the primary predictor variable, and age, gender, and education when a psychosocial factor was being assessed. Model three controlled for the health behaviors (smoking status, alcohol consumption, caffeine consumption, physical activity level, and medication usage), and model four added health status indicators (BMI, WHR, chronic health conditions). The final model examined the interactions between the psychosocial factors and education net of all control variables. All interactions were assessed in separate models.
Results
Descriptive statistics on all variables are provided in Table 1. Missing data were limited: ten individuals had missing IL-6 data, and no more than four individuals had missing data for any psychosocial or control variable. The degrees of freedom vary slightly among analyses, reflective of the missing data.
Table 1.
Descriptive statistics for sample (N = 1028)
| Variable | Mean (SD) | Range | % |
|---|---|---|---|
| IL-6 (pg/mL) | 2.8 (2.8) | 0.16 – 23.0 | |
| Education | |||
| High School graduate, GED or less | 24.5 | ||
| Some college | 29.3 | ||
| College graduate | 46.2 | ||
| Psychosocial Factors | |||
| MASQ Anxious Symptoms | 16.6 (4.5) | 11 – 47 | |
| MASQ Anxious-Arousal | 21.8 (5.2) | 17 – 70 | |
| CES-D Depressive Symptoms | 7.9 (7.7) | 0 – 49 | |
| MASQ Positive Affect | 44.9 (10.0) | 14 – 70 | |
| Autonomy | 37.4 (6.7) | 14 – 49 | |
| Environmental Mastery | 38.8 (7.5) | 11 – 49 | |
| Personal Growth | 39.7 (6.6) | 14 – 49 | |
| Positive Relations with Others | 41.1 (6.8) | 14 – 49 | |
| Purpose in Life | 39.6 (6.5) | 10 – 49 | |
| Self-Acceptance | 38.7 (8.1) | 7 – 49 | |
| Control Variables | |||
| Age | 58.0 (11.6) | 35 – 86 | |
| Gender (% female) | 55.0 | ||
| Medications (% Yes) | |||
| Anti-hypertensive | 34.8 | ||
| Cholesterol lowering | 29.3 | ||
| Corticosteroid | 12.3 | ||
| Anti-depressant | 15.1 | ||
| Smoking Status | |||
| Never smoked | 55.3 | ||
| Former smoker | 33.2 | ||
| Current smoker | 11.5 | ||
| Caffeine (servings per day) | 3.0 (3.0) | 0 – 30 | |
| Alcohol (drinks per month) | 13.1 (23.8) | 0 – 240 | |
| Vigorous/moderate exercise (min/wk) | 337.0 (552.2) | 0 – 4,550 | |
| Chronic Conditions | 2.6 (2.1) | 0 – 12 | |
| BMI | 29.2 (6.0) | 15.0 – 60.4 | |
| WHR | 0.9 (0.1) | 0.6 – 1.6 | |
Note. IL-6 = Interleukin-6; GED = General Educational Development; MASQ = Mood and Anxiety Symptom Questionnaire; CES-D = Center for Epidemiologic Studies Depression; BMI = body mass index; WHR = waist-to-hip ratio.
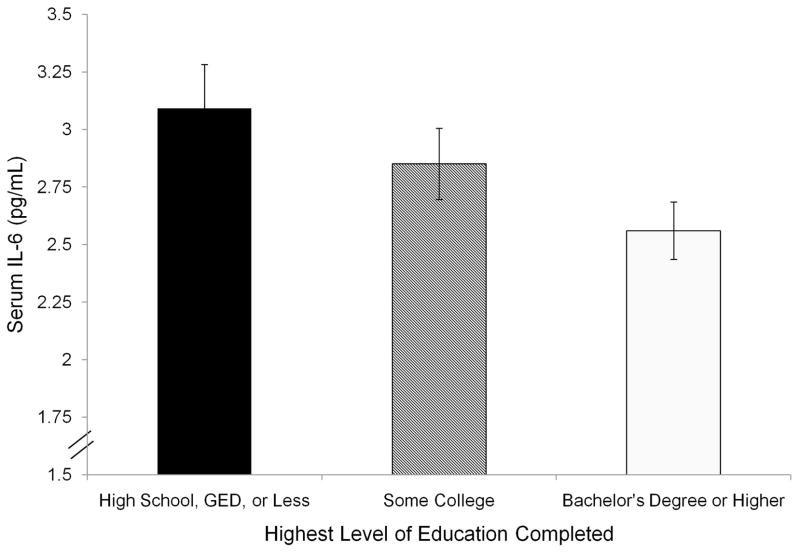
Summaries of multivariate analyses regressing IL-6 on education and psychosocial measures are provided in Table 2. As hypothesized, levels of IL-6 followed the educational gradient: IL-6 decreased with increasing education (Figure 1; β = −0.09, t(1008) = 2.77, p = 0.01). This relationship was attenuated, but still significant, after controlling for age and gender (Table 2, Model 2). However, further adjusting for health behavior (Model 3; β = −.05, p < .09) and health status indicator variables (Model 4; β = −.02, p = .61) attenuated this effect to non-significance.
Table 2.
Hierarchical Regression of Psychosocial Factors on log-transformed Interleukin-6 (N = 1028)
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5* | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Without Controls | + Demographics | + Health Behaviors | + Health Status | Interaction | ||||||
| β | p | β | p | β | p | β | p | β | p | |
| Education | −.09 | .01 | −.07 | .03 | −.05 | .09† | −.02 | .61 | ||
| Negative Affect | ||||||||||
| MASQ Anxious Symptoms | .01 | .80 | .04 | .17 | .02 | .54 | −.00 | .97 | −.01 | .77 |
| MASQ Anxious-Arousal | .14 | .00 | .13 | .00 | .07 | .02 | .04 | .26 | −.01 | .80 |
| CES-D Depressive Symptoms | .07 | .03 | .10 | .00 | .05 | .09† | .02 | .46 | −.05 | .06† |
| Hedonic Well-being | ||||||||||
| MASQ Positive Affect | −.01 | .66 | −.04 | .17 | −.01 | .85 | .02 | .46 | .09 | .00 |
| Eudaimonic Well-Being | ||||||||||
| Autonomy | .02 | .54 | −.01 | .75 | .00 | .98 | −.02 | .54 | .03 | .36 |
| Environmental Mastery | −.01 | .75 | −.07 | .04 | −.03 | .29 | −.02 | .54 | .06 | .03 |
| Personal Growth | −.09 | .00 | −.10 | .00 | −.09 | .01 | −.06 | .06† | .04 | .12 |
| Positive Relations with Others | .02 | .47 | −.02 | .49 | −.02 | .58 | .00 | .95 | .06 | .03 |
| Purpose in Life | −.07 | .03 | −.08 | .02 | −.05 | .10 | −.03 | .37 | .06 | .03 |
| Self-Acceptance | −.05 | .09† | −.09 | .01 | −.05 | .10 | −.03 | .30 | .06 | .05 |
Note. MASQ = Mood and Anxiety Symptom Questionnaire; CES-D = Center for Epidemiologic Studies Depression. All coefficients reported are standardized. Model 1 contains the bivariate correlation with IL-6. Model 2 adds age, gender, and education if the primary variable is a psychosocial factor. Model 3 adds smoking status, alcohol consumption, caffeine consumption, amount of moderate to vigorous physical activity, and medication usage. Model 4 adds BMI (log transformed), WHR, and chronic health conditions. Model 5 adds an interaction term between the particular psychosocial variable and education.
The model 5 coefficients are those for the interaction term.
p < .10.
Bolded coefficients are significant at p < .05.
Figure 1.
Mean levels of IL-6 (+SE) by educational attainment in three categories: (1) individuals with a high school education, GED, or less, (2) individuals with some college education, but no degree, and (3) individuals with a bachelor’s degree or higher.
As hypothesized, higher scores on the anxious-arousal scale and depressive symptoms were related to higher IL-6 [Table 2, Model 1; anxious arousal: β = .14, t(1007) = 4.35, p < 0.001; depressive symptoms: β = .07, t(1006) = 2.13, p = 0.03]. Including age, gender, and education in the models did not affect these associations (Table 2, Model 2). Adjusting for health behaviors attenuated the effect of depressive symptoms to non-significance, though the relationship between anxious arousal symptoms and IL-6 remained significant after controlling for health behaviors, β = .07, t(995) = 2.26, p = .02. This relationship became non-significant, however, when health status indicators were added to the model, β =.04, t(992) = 1.14, p = .26. All main effects of anxious and depressive symptoms on IL-6 were unchanged when positive affect was entered as an additional covariate into the models. After entering the eudaimonic well-being scales into the models as additional covariates, all main effects were attenuated to non-significance.
As hypothesized, the eudaimonic measure of personal growth was inversely related to IL-6 in bivariate analyses, β = −.09, t(1007) = 2.88, p < 0.01. Adjusting for demographic factors, health behaviors, and health status indicators attenuated this relationship, though it remained marginally significant with all control variables included, β = −.06, t(992) = 1.93, p < 0.06 (Table 2, Models 2–4). This association was unaffected by adjustments for the negative psychosocial variables. No other measure of hedonic or eudaimonic well-being was associated with IL-6 levels in main effect adjusted or unadjusted models.
Several psychosocial variables interacted with education in the prediction of IL-6 after controlling for demographic factors, health behaviors, and health status indicators (Table 2, Model 5). All subsequent interactions were interpreted in models containing all control variables. Of the negative psychosocial factors, CES-D depressive symptoms trended toward moderating the effect of education on IL-6, t(990) = 1.91, p < 0.06. In accordance with hypotheses, for individuals with low educational attainment, higher depressive symptoms were associated with higher IL-6, β = .09, t(990) = 1.93, p = .05. The interaction between CES-D depressive symptoms and education in the prediction of IL-6 was unaltered by the inclusion of hedonic or eudaimonic well-being in the models entered as individual variables or as a collective set.
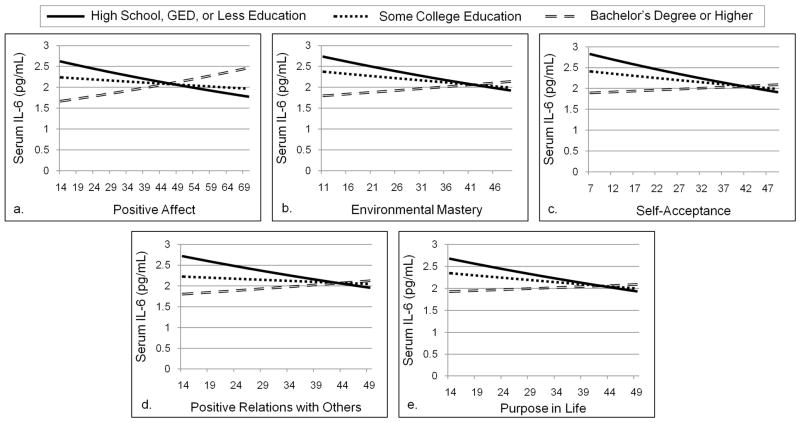
Both hedonic and eudaimonic well-being moderated the effect of education on IL-6 in the 9expected direction. There was a significant interaction between education and positive affect, t(992) = 3.04, p < 0.01 (Figure 2a). This effect remained significant independent of the negative psychosocial factors, examined as additional covariates. Likewise, four of the six eudaimonic well-being measures - environmental mastery, positive relations with others, purpose in life, and self-acceptance - significantly moderated the effect of education on IL-6 [Figure 2b-2e; environmental mastery: t(991) =2.20, p < .03; positive relations with others: t(992) = 2.19, p < .03; purpose in life: t(991) = 2.12, p = .03; self-acceptance: t(991) = 2.01, p < .05]. The associations between education and environmental mastery, positive relations with others, and purpose in life were unchanged by the inclusion of the negative psychosocial variables collectively in the model, although the association between education and self-acceptance was attenuated to marginal significance with the addition of the negative psychosocial variables.
Figure 2.
Well-being moderated the effect of education on IL-6. Lines represent simple effects of psychosocial factors on IL-6 for categories according to educational attainment, controlling for age, gender, smoking status, alcohol consumption, caffeine consumption, physical activity, medication usage, BMI, WHR, and chronic health conditions. The inverse relationship between IL-6 and well-being for individuals with a high school education or less is significant in all panels, with the exception of panel d, where the simple effect was marginally significant. The positive relationship between positive affect and IL-6 for individuals with a college degree or higher was also significant. Figure 2a. With education interpreted as a continuous variable, the simple effect of positive affect at one standard deviation below the mean on education was not significant. Figure 2b. With education interpreted as a continuous variable, the simple effect of environmental mastery at one standard deviation below the mean on education was marginally significant. Figure 2c. With education interpreted as a continuous variable, the simple effect of positive relations with others at one standard deviation below the mean on education was not significant.
Figure 2 displays the significant interactions between well-being and education (categorized for ease of presentation as college degree earners, individuals who had completed some college without earning a degree, and individuals with a high school education, GED, or less). Simple slopes of the effects of a psychosocial variable for each education category were compared. These effects mostly converged with tests of significance using education measured continuously (i.e., simple effects at the mean and plus and minus one standard deviation on education); the differences are noted in the figure caption.
In accordance with hypotheses, positive affect had a significant, negative effect on IL-6 for individuals with a high school education or less, β = −.09, t(992) = 1.93, p = .05. However, individuals with at least a college degree displayed the opposite effect. Contrary to predictions, positive affect was positively related to IL-6 for college degree earners, β = .10, t(992) = 2.56, p = .01. Simple effects of the eudaimonic well-being measures for individuals with a high school education were all in the hypothesized direction. IL-6 was inversely related to environmental mastery (β = −.09, t(991) = 2.06, p = .04), purpose in life (β = −.10, t(991) = 2.19, p < .03), and self-acceptance (β = −.10, t(991) = 2.18, p = .03). IL-6 also trended towards a negative relationship with positive relations with others, β = −.08, t(991) = 1.75, p = .08.
Supplemental Analyses: Influence of Twin Status on Reported Relationships
Additional analyses assessed whether genetic influences among the identical and fraternal twins (N = 338) affected the findings reported above. Three modified samples were created that contained only one randomly selected member from each twin pair. All models were re-run, and results were considered to differ when two out of the three modified samples demonstrated an effect inconsistent with those reported above. Changes in the size of coefficients as well as changes in significance were assessed. However, none of the above results were affected by the inclusion of the twins, nor was statistical significance undermined by excluding one member of each twin pair.
Discussion
As predicted, IL-6 levels were inversely related to education and significantly correlated with anxious-arousal and depressive symptoms in bivariate analyses. These effects remained significant after accounting for age and gender, although the relationships were attenuated to non-significance after adjusting for health behaviors and health status indicators. Nevertheless, respondents’ positive psychological status, specifically their sense of own personal growth significantly predicted lower IL-6, and this effect remained after taking into account all control variables. These main effect results complement previous work linking higher IL-6 to lower educational attainment, higher negative affect, and a lower sense of well-being (Friedman et al., 2007; Gruenewald et al., 2009; Howren et al., 2009; Petersen et al., 2008; Pitsavos et al., 2006) and also highlight the role of health behaviors and clinical health status as important contributors to these associations (Gruenewald et al., 2009; Koster et al., 2006; Loucks et al., 2006). Extensive adjustments for health practices and health status indicators were included in this analysis to sharpen the focus on psychosocial moderation of the relationship between education and IL-6, though this may have diminished the ability to detect significant main effects of education and negative affect on IL-6.
The central focus of this study was to investigate how psychosocial factors moderated the relationship between education and IL-6. Consistent with the hypotheses, individuals with low education and high depressive symptoms had the highest levels of IL-6. However, it should be noted that the omnibus interaction assessing the moderating effect of depression on educational gradients in IL-6 was only marginally significant. This coupling of low educational status and depression is especially worrisome given that individuals in lower socioeconomic positions are at an increased risk for developing depression (Lorant et al., 2003), and they may not possess the resources, either material or psychological, to seek out and afford treatment.
Conversely, positive psychosocial factors were found to attenuate the biological impact of lower educational attainment. Positive affect, environmental mastery, purpose in life, and self-acceptance had the largest effects on individuals with a high school degree or less. At high levels of hedonic and eudaimonic well-being, those with a high school degree or less appear to have comparable IL-6 levels to individuals with a college degree (Figure 2). A similar association was observed between IL-6 and positive relations with others, although this was marginally significant. In contrast to predictions, for individuals with a college degree, positive affect was positively related to IL-6. While this is not the first description of unique biological correlates of high positive affect (Pressman & Cohen, 2005), given that it emerged as a synergistic effect of education and positive affect, further research is needed to confirm such a differential relationship across the education continuum.
Overall, those who reported a high sense of well-being did not appear to be as burdened biologically -- in terms of cells and tissues that produce IL-6 -- by low educational attainment. That these effects persisted after controlling for health behavior and health status indicators underscores the salubrious benefits of psychological well-being above and beyond those associated with a healthy lifestyle. It is important to note that these results remained significant after adjusting for negative affect (per recommendation of Pressman & Cohen, 2005), thereby reinforcing the view that well-being and ill-being are not merely opposite ends of a continuum, but distinctive processes with unique health correlates (Ryff et al., 2006). Further, the effects of well-being are independent of each other; there is no evidence to suggest that these healthful effects are overlapping. When the other eudaimonic well-being scales were added to the model, the interaction between that particular well-being scale and education remained significant (data not shown). Prior work has documented overall health benefits of happiness and living well (Chida & Steptoe, 2008; Pressman & Cohen, 2005; Ryff, Singer, & Love, 2004; Seeman, 1996; Steptoe, Wardle, & Marmot, 2005), but the important message of the current results is that the health benefits are especially salient for those with lower educational attainment.
Other moderating influences may be relevant in the interplay of SES, psychosocial factors, and health. Expanding on psychosocial factors, one promising avenue may be to assess how perceived sense of control interacts with education. Ross and Mirowsky (1999) argued that education increases one’s sense of control, and thereby, may also influence the likelihood of practicing beneficial health behaviors. Further, Lachman and Weaver (1998) demonstrated that among individuals with low income, those who had a high sense of control had comparable self-rated health to those with a high income. Sociodemographic factors, like age, gender, and race, may also moderate the relationships between education and inflammatory markers. For example, higher IL-6 and CRP levels were associated with lower levels of education in whites and blacks, but the trends were not significant among Hispanic and Chinese individuals (Ranjit et al., 2007). Likewise, controlling for chronic health conditions and BMI reduced the relationships between education and IL-6 and CRP to non-significance in white females and black males, but these relationships remained significant in black females and white males (Gruenewald et al., 2009). In sum, growing evidence suggests that socioeconomic factors are linked to inflammatory markers differentially across various demographic groups. The moderating effects of these sociodemographic factors were not assessed in the current analyses, though they may explain why the main effects of education and negative affect on IL-6 were not confirmed in this sample once health behaviors and health status indicators were taken into account.
Moderating analyses must also be augmented by analyses probing the mediating processes through which education and psychosocial factors translate into better health outcomes. Behavioral processes constitute one important mechanistic pathway underlying these relationships. Individuals with higher educational attainment and well-being are less likely to smoke, to be obese, and are more likely to exercise (Adler, 2009). Education may increase awareness of these behaviors in promoting health, and well-being may contribute to placing value in one’s future health. Adjusting for health behavior and health status indicators attenuated the association between education and IL-6 to non-significance in the current analyses. Of these factors, adiposity is of particular interest because 15–35% of circulating IL-6 may be produced by fat tissue (Mohamed-Ali et al., 1997). Even so, psychological well-being was found to moderate the educational gradient in IL-6 independent of health behaviors, health status indicators, and demographic factors. Thus, positive psychosocial functioning may relate to lower IL-6 through mechanisms beyond promoting a healthy lifestyle, perhaps by buffering the negative effects of stress. Individuals in lower socioeconomic positions are more likely to be exposed to chronic stress (Adler & Rehkopf, 2008) and to have increased daily cortisol release and to develop glucocorticoid and insulin resistance related to metabolic syndrome. Positive psychosocial functioning has previously been linked to decreased cortisol output, decreased HPA axis reactivity, and enhanced immune function (Berk, Felten, Tan, Bittman, & Westengard. 2001; Cohen, 2004; Pressman & Cohen, 2005; Ross & Mirowsky, 1999; Steptoe et al., 2008), suggesting factors that may offset the physiological concomitants (e.g., circulating levels of IL-6) related to low educational attainment.
IL-6 was the sole cytokine marker of proinflammatory biology in this investigation. IL-6 is a potent stimulator of the production and release of other inflammatory markers, such as C-reactive protein (CRP) and fibrinogen (Heinrich, Castell, & Andus, 1990). IL-6 was chosen to be the specific focus because of its previous link to eudaimonic well-being in a sample of aging women (Friedman et al., 2007), and we have evidence that IL-6 partially mediates the relationship between SES and CRP and fibrinogen (Friedman & Herd, 2010). These results highlight the need to investigate other physiological aberrations and to link up the dysregulation with clinical outcomes in terms of the likely relationship to both socioeconomic and psychological factors.
Several limitations should be acknowledged. First, individuals included in these biological analyses were better educated than the participant pool from which they were recruited, which may limit generalization to less educated groups. The composition of this sample may have contributed to the non-significant educational gradient once health behaviors and health status indicators were taken into account. Nevertheless, the coefficients for the relationship between education and IL-6 were comparable to those reported in the Framingham Offspring Study, where over 50% of the sample had a high school education or less (Loucks et al., 2006). Only 6.8% of the sample was non-white, also limiting generalization to racial/ethnic minorities. Another issue was the inclusion of 338 identical and fraternal twins, and genetic relatedness could affect the likelihood of finding associations, although supplemental analyses indicated that the presence of the twin pairs did not modify results.
Given the cross-sectional nature of the design, the direction of influence among the predictor and outcome variables is not readily resolved. However, education is generally completed in early adulthood, so it is unlikely that our middle-aged and older sample had experienced recent changes in their educational attainment (92% reported the same level of education at MIDUS I and MIDUS II). Using education as an index of SES may make it less susceptible to problems of possible reverse causation. The matter of how to model education is also open to alternative approaches. We treated education as a continuous variable, consistent with work of Ross and Mirowsky (1999) showing that years in school, regardless of degree, has the strongest effects linking education to perceived health and physical functioning. However, links between education and health may also depend on degree completion, which is positively linked to occupational status, better working conditions, and greater access to health care. Further, recent evidence from Friedman and Herd (2010) suggests that income mediates the relationship between education and inflammatory markers, thereby suggesting additional conceptual and analytic strategies for connecting socioeconomic standing to health. For the purpose of this analysis, we chose to focus on education as a valuable index of SES, given its cross-time stability, more limited susceptibility to health selection issues, and usefulness as an individual difference variable (compared to household income, for example).
Notwithstanding these issues, a unique strength of this study is the diverse set of psychosocial measures that were assembled to examine the relationship between education and proinflammatory biology. This investigation is one of the first to demonstrate an interaction between education and psychosocial factors in predicting IL-6 levels in a large American population. Well-being was associated with lower IL-6, and depressive symptoms were associated with higher IL-6 in individuals with low educational attainment. These results highlight how interactive modeling can provide a more complete and compelling understanding of the ways in which socioeconomic and psychosocial factors jointly predict levels of IL-6 in systemic circulation.
Acknowledgments
This research was supported by a grant from the National Institute on Aging (P01-AG020166) to conduct a longitudinal follow-up of the MIDUS investigation. The original study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. We thank the staff of the Clinical Research Centers at the University of Wisconsin- Madison, UCLA, and Georgetown University for their support in conducting this study. Supported by the following grants M01-RR023942 (Georgetown), M01-RR00865 (UCLA) from the General Clinical Research Centers Program and 1UL1RR025011 (UW) from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources, National Institutes of Health. The authors also extend gratitude to Gayle Love, Barry Radler, and Dorothy Brar for their conscientious dedication that made this project possible.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/HEA
Contributor Information
Jennifer A. Morozink, Department of Psychology, University of Wisconsin- Madison
Elliot M. Friedman, Institute on Aging, University of Wisconsin- Madison
Christopher L. Coe, Department of Psychology and Harlow Center for Biological Psychology, University of Wisconsin- Madison
Carol D. Ryff, Department of Psychology and Institute on Aging, University of Wisconsin- Madison
References
- Adler NE. Health disparities through a psychosocial lens. American Psychologist. 2009;64:663–673. doi: 10.1037/0003-066X.64.8.663. [DOI] [PubMed] [Google Scholar]
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Al AL, Kronfol Z, Seymour E, Bolling SF. Effects of mood state and psychosocial functioning on plasma interleukin-6 in adult patients before cardiac surgery. International Journal of Psychiatry in Medicine. 2005;35(4):363–376. doi: 10.2190/2ELG-RDUN-X6TU-FGC8. [DOI] [PubMed] [Google Scholar]
- Annique S, Dorien T, Richel L, Gunter K, Joris D, Harry JC, et al. Inflammatory markers in depressed post-myocardial infarction patients. Journal of Psychiatric Research. 2005;39:137–144. doi: 10.1016/j.jpsychires.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Berk LS, Felten DL, Tan SA, Bittman BB, Westengard J. Modulation of neuroimmune parameters during the eustress of humor-associated mirthful laughter. Alternative Therapies in Health and Medicine. 2001;7:62–76. [PubMed] [Google Scholar]
- Brim OG, Ryff CD, Kessler RC. How healthy are we: A national study of well- being at midlife. Chicago: University of Chicago Press; 2004. [Google Scholar]
- Chida Y, Steptoe A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosomatic Medicine. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59(8):676– 684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Dentino AN, Pieper CF, Rao KMK, Currie MS, Harris T, Blazer DG, et al. Association of interleukin-6 and other biologic variables with depression in older people living in the community. Journal of the American Geriatrics Society. 1999;47(1):6–11. doi: 10.1111/j.1532-5415.1999.tb01894.x. [DOI] [PubMed] [Google Scholar]
- Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annual Review of Medicine. 2000;51:245–270. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, et al. Risk factors for 5-year mortality in older adults: The Cardiovascular Health Study. Journal of the American Medical Association. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychology. 2007;26(3):305–313. doi: 10.1037/0278-6133.26.3.305. [DOI] [PubMed] [Google Scholar]
- Friedman EM, Herd P. Income, education, and inflammation: Differential associations in a national sample (the MIDUS study) Psychosomatic Medicine. 2010;72:290–300. doi: 10.1097/PSY.0b013e3181cfe4c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González MA, Artalejo FR, Calero JR. Relationship between socioeconomic status and ischaemic heart disease in cohort and case-control studies: 1960–1993. International Journal of Epidemiology. 1998;27:350–358. doi: 10.1093/ije/27.3.350. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Cohen S, Matthews KA, Tracy R, Seeman TE. Association of socioeconomic status with inflammation markers in black and white men and women in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Social Science and Medicine. 2009;69:451–459. doi: 10.1016/j.socscimed.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochemical Journal. 1990;265:621–636. doi: 10.1042/bj2650621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosomatic Medicine. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- Jain MK, Ridker PM. Anti-inflammatory effects of statins: Clinical evidence and basic mechanisms. Nature Reviews: Drug Discovery. 2005;4:977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- Kenis G, Maes M. Effects of antidepressants on the production of cytokines. International Journal of Neuropsychopharmacology. 2002;5:401–412. doi: 10.1017/S1461145702003164. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CLM, Shmotkin D, Ryff CD. Optimizing well-being: The empirical encounter of two traditions. Journal of Personality and Social Psychology. 2002;82:1007–1022. [PubMed] [Google Scholar]
- Koster A, Bosma H, Penninx BWJH, Newman AB, Harris TB, van Eijk JTM, et al. Association of inflammatory markers with socioeconomic status. Journal of Gerontology: Medical Sciences. 2006;61A(3):284–290. doi: 10.1093/gerona/61.3.284. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lespérance F, Frasure-Smith N, Théroux P, Irwin M. The association between major depression and levels of soluble intercellular adhesion molecule 1, interleukin-6, and C-reactive protein in patients with recent acute coronary syndromes. American Journal of Psychiatry. 2004;161:271–277. doi: 10.1176/appi.ajp.161.2.271. [DOI] [PubMed] [Google Scholar]
- Lorant V, Deliége D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Loucks EB, Lynch JW, Pilote L, Fuhrer R, Almeida ND, Richard H, et al. Life-course socioeconomic position and incidence of coronary heart disease: The Framingham Offspring Study. American Journal of Epidemiology. 2009;169:829–836. doi: 10.1093/aje/kwn403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loucks EB, Sullivan LM, Hayes LJ, D’Agostino RB, Sr, Larson MG, Vasan RS, et al. Association of education level with inflammatory markers in the Framingham Offspring Study. American Journal of Epidemiology. 2006;163:622–628. doi: 10.1093/aje/kwj076. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Smith GD, Stansfeld S, Patel C, North F, Head J, et al. Health inequalities among British civil servants: The Whitehall II study. The Lancet. 1991;337:1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Miller GE, Stetler CA, Carney RM, Freedland KE, Banks WA. Clinical depression and inflammatory risk markers for coronary heart disease. American Journal of Cardiology. 2002;90:1279–1283. doi: 10.1016/s0002-9149(02)02863-1. [DOI] [PubMed] [Google Scholar]
- Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-α, in vivo. Journal of Clinical Endocrinology and Metabolism. 1997;82(12):4196–4200. doi: 10.1210/jcem.82.12.4450. [DOI] [PubMed] [Google Scholar]
- O’Connor M, Irwin MR. Links between behavioral factors and inflammation. Clinical Pharmacology and Therapeutics. 2010;87:479–482. doi: 10.1038/clpt.2009.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx BWJH, Kritchevsky SB, Yaffe K, Newman AB, Simonsick EM, Rubin S, et al. Inflammatory markers and depressed mood in older persons: Results from the Health, Aging, and Body Composition Study. Biological Psychiatry. 2003;54:566–572. doi: 10.1016/s0006-3223(02)01811-5. [DOI] [PubMed] [Google Scholar]
- Petersen KL, Marsland AL, Flory J, Votruba-Drzal E, Muldoon MF, Manuck SB. Community socioeconomic status is associated with circulating interleukin-6 and C-reactive protein. Psychosomatic Medicine. 2008;70:646–652. doi: 10.1097/PSY.0b013e31817b8ee4. [DOI] [PubMed] [Google Scholar]
- Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: The ATTICA Study. Atherosclerosis. 2006;185:320–326. doi: 10.1016/j.atherosclerosis.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Pollitt RA, Kaufman JS, Rose KM, Diez-Roux AV, Zeng D, Heiss G. Cumulative life course and adult socioeconomic status and markers of inflammation in adulthood. Journal of Epidemiology and Community Health. 2008;62:484–491. doi: 10.1136/jech.2006.054106. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Ranjit N, Diez-Roux AV, Shea S, Cushman M, Ni H, Seeman T. Socioeconomic position, race/ethnicity, and inflammation in the Multi-Ethnic Study of Atherosclerosis. Circulation. 2007;116:2383–2390. doi: 10.1161/CIRCULATIONAHA.107.706226. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto AM, Jr, Kastelein JJP, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. The New England Journal of Medicine. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Rifai N, Stampfer MJ, Hennekens CH. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000;101:1767–1772. doi: 10.1161/01.cir.101.15.1767. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Refining the association between education and health: The effects of quantity, credential, and selectivity. Demography. 1999;36:445–460. [PubMed] [Google Scholar]
- Ross R. Atherosclerosis An inflammatory disease. The New England Journal of Medicine. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annual Review of Psychology. 2001;52:141–166. doi: 10.1146/annurev.psych.52.1.141. [DOI] [PubMed] [Google Scholar]
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57:1069–1081. [Google Scholar]
- Ryff CD, Keyes CLM. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Love GD, Urry HL, Muller D, Rosenkranz MA, Friedman EM, et al. Psychological well-being and ill-being: Do they have distinct or mirrored biological correlates? Psychotherapy and Psychosomatics. 2006;75:85–95. doi: 10.1159/000090892. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Singer BH. Know thyself and become what you are: A eudaimonic approach to psychological well-being. Journal of Happiness Studies. 2008;9(1):13–39. [Google Scholar]
- Ryff CD, Singer BH, Love GD. Positive health: Connecting well-being with biology. Philosophical Transactions: Biological Sciences. 2004;349(1449):1383–1394. doi: 10.1098/rstb.2004.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE. Social ties and health: The benefits of social integration. Association of Educational Psychologists Journal. 1996;6(5):442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Kunz-Ebrecht SR, Owen N. Lack of association between depressive symptoms and markers of immune and vascular inflammation in middle-aged men and women. Psychological Medicine. 2003;33:667–674. doi: 10.1017/s0033291702007250. [DOI] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Badrick E, Kumari M, Marmot M. Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: The Whitehall II Study. American Journal of Epidemiology. 2008;167(1):96–102. doi: 10.1093/aje/kwm252. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wardle J, Marmot M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proceedings of the National Academy of Sciences. 2005;102(18):6508–6512. doi: 10.1073/pnas.0409174102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strine TW, Mokdad AH, Balluz LS, Gonzalez O, Crider R, Berry JT, et al. Depression and anxiety in the United States: Findings from the 2006 behavioral risk factor surveillance survey. Psychiatric Services. 2008;59(12):1383–1390. doi: 10.1176/ps.2008.59.12.1383. [DOI] [PubMed] [Google Scholar]
- Suarez EC. Joint effect of hostility and severity of depressive symptoms on plasma interleukin-6 concentration. Psychosomatic Medicine. 2003;65:523–527. doi: 10.1097/01.psy.0000062530.94551.ea. [DOI] [PubMed] [Google Scholar]
- Tatli E, Kurum T. A controlled study of the effects of carvedilol on clinical events, left ventricular function and proinflammatory cytokines levels in patients with dilated cardiomyopathy. Canadian Journal of Cardiology. 2005;21:344–348. [PubMed] [Google Scholar]
- Tiermeier H, Hofman A, van Tuijl HR, Kiliaan AJ, Meijer J, Breteler MMB. Inflammatory proteins and depression in the elderly. Epidemiology. 2003;14(1):103–107. doi: 10.1097/00001648-200301000-00025. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995;104(1):3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Caska CM, Hendrickson BE, Rourke MA, Ho J, Ali S. Depression and inflammation in patients with coronary heart disease: Findings from the Heart and Soul Study. Biological Psychiatry. 2007;62:314–320. doi: 10.1016/j.biopsych.2006.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]