Abstract
The overexpression of cyclooxygenase (COX)-2 is a frequent event in squamous cell carcinomas of the head and neck (HNSCC), and non-steroidal anti-inflammatory drugs, which are potent inhibitors of COX-1 and COX-2, exert chemopreventive effects on HNSCC cancer development. COX-2 promotes the release of the pro-inflammatory mediator prostaglandin E2 (PGE2), which acts on its cell surface G protein-coupled receptors EP1, EP2, EP3, and EP4. Here, we investigated the role of PGE2 and its receptors in cellular proliferation in HNSCC. The expression of COX-2 and EP1-4 was examined in immortalized oral epithelial cells and in a representative panel of HNSCC cell lines, and based on these data EP1-EP3 and COX-2 expression were evaluated by immunohistochemistry in a large clinical sample collection using HNSCC tissue microarrays. The ability of selective COX-2 inhibition to block PGE2 secretion was measured by ELISA specific assays. The effects of PGE2 on cell proliferation were evaluated using PGE2, its stable analog, and EP2 and EP3-specific synthetic agonists. The results presented here show that HNSCC tumoral lesions and their derived cell lines constitutively express COX-2 and the EP1, EP2 and EP3 receptors for PGE2. HNSCC cells secrete PGE2, which can be suppressed by low concentrations of COX-2 selective inhibitors, without inhibiting cell proliferation. Exogenously added stable PGE2 and EP3-specific agonists induce DNA synthesis in all HNSCC cell lines tested. Overall, our study supports the emerging notion that PGE2 produced in the tumor microenvironment by the overexpression of COX-2 in tumoral and inflammatory cells may promote the growth of HNSCC cells in an autocrine and paracrine fashion by acting on PGE2 receptors that are widely expressed in most HNSCC cancer cells. In particular, our findings suggest that EP3 receptor may play a more prominent role in HNSCC cell growth promotion, thus providing a rationale for the future evaluation of this PGE2 receptor as a target for HNSCC prevention strategies.
Keywords: Head and neck cancer, Cyclooxygenase, Prostaglandin E2, PGE2 receptors, EP1, EP2, EP3, EP4, G protein-coupled receptors, Oral cancer
Introduction
With approximately 500,000 new cases and 250,000 deaths annually, squamous cell carcinomas of the head and neck (HNSCC) represents one of the six most common cancers in the world1-2. The survival of HNSCC patients is poor and there has been limited improvement in the last three decades1. Although HNSCC has well recognized risk factors, including tobacco use, excess alcohol consumption, and infection by high risk papillomaviruses2-3, we still have an incomplete knowledge of the mechanisms underlying the malignant progression of this cancer type 2. Of interest, non-steroidal anti-inflammatory drugs, which are potent inhibitors of cyclooxygenase (COX), have been shown to exert chemopreventive effects on cancer development4-7. There are two isoforms of cyclooxygenase: COX-1 and COX-2. While COX-1 is found constitutively expressed in almost all tissues, COX-2 is the enzyme responsible for the high output production of prostanoids (prostaglandins and thromboxanes) from arachidonic acid in multiple pathophysiological conditions, including cancer8. Up-regulation of COX-2 is a frequent event in human malignancies, including colon and lung cancer, and HNSCC, and its up-regulation can be linked with increased angiogenesis and metastasis8-9. Immunohistochemical reactivity for COX-2 in HNSCC has been extensively investigated10-12, and recently described in the context of other molecular alterations 9.
The COX-2-initiated signaling pathways can control cell proliferation; hence molecules involved in COX-2 signaling represent attractive targets in mechanisms-directed cancer prevention and therapy. Indeed, there is a growing interest in developing antagonists for the E series of prostaglandin (EP) receptors, designated as EP1 to EP4. Their procarcinogenic role is supported by knockout animals studies. For example, disruption of the EP2 receptor decreases the number and size of intestinal polyps and the intensity of angiogenesis in genetically colon cancer prone mice, APCMin mice13. EP3 receptor-knockout mice develop less tumor-associated blood vessels due to reduced expression of vascular endothelium growth factor14. However, which EP receptors are expressed in HNSCC has not been fully explored, and the precise role of each EP receptor in HNSCC pathogenesis has yet to be elucidated. Here, we investigated the involvement of EP receptors and the proliferative potential of PGE2. We found that EP1, EP2 and EP3 receptors are widely expressed in HNSCC tissues and their derived cell lines. We also show that the COX-2 metabolite, PGE2, can stimulate HNSCC cell proliferation, and present evidence for a likely predominant role of EP3 receptors.
Materials and Methods
Reagents
PGE2, dmPGE2 (16,16-dimethyl prostaglandin E2), butaprost (EP2 receptor agonist), sulprostone (EP3 receptor agonist), and antibodies against EP1, EP2 and EP4 receptors were purchased from Cayman Chemical (Ann Arbor, MI, USA). EP3 receptor antibody and GAPDH antibody were obtained from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA), and COX-2 antibody was from BD Transduction (San Jose, CA, USA). Celecoxib (COX-2 selective inhibitor) was kindly provided by Pfizer (Sao Paulo, SP, Brazil) and indomethacin was purchase from Sigma-Aldrich (St. Louis, MO, USA). Reagents for electrophoresis were obtained from Bio-Rad (Hercules, CA, USA), Quality Biological (Gaithersburg, MD, USA) and KD Medical (Columbia, MD, USA).
Cell Lines and Culture Conditions
HNSCC cell lines (HN6, HN12, HN13, HN30, Cal27, UMSCC17B and OSCC3), normal oral keratinocyte spontaneously immortalized cell line (NOK-SI), and, HEK293T cells were maintained in DMEM (Dulbelco's Modified Eagle's Medium) medium supplemented with 10% fetal bovine serum, 100 U/ml penicillin, and 100 μg/ml streptomycin at 37°C in a humidified atmosphere of 5% CO2 and 95% air.
[3H]Thymidine Incorporation Assay
DNA-synthesis assays were performed by measuring the incorporation of [3H] thymidine into cellular DNA. Serum starved subconfluent cell were exposed to antagonists or inhibitors for 1 h, and stimulated with PGE2 or selective EP receptor agonists as indicated for 24 h, adding 0.5 μCi/ml [3H] thymidine for the last 4 h of incubation. Results were expressed as the mean ± S.E.M. for at least three independent experiments. Statistical analysis was performed by ANOVA using GraphPad Prism 5.0 (GraphPad software, San Diego, CA). P values less than 0.05 were considered statistically significant (*p <0.05; **p<0.01; ***p<0.001; NS-not significant).
Western Blotting
HNSCC, oral keratinocytes and HEK293T cells were washed, and lysed in cell lysis buffer (0.2 M Tris pH 7.5, SDS 20%, 14.3 M 2-betamercaptoetanol) containing protease inhibitors. Thirty μg of protein was resolved into SDS-polyacrylamide gel electrophoresis and Westen blotting was conducted using standard techniques.
PGE2 Assay
PGE2 secreted in the conditioned cell culture media of serum-starved cells for 24hs with and without COX inhibitors was measured using a PGE2 EIA kit from Cayman (Ann Arbor, MI, USA) according to the manufacturer's instructions.
Cell Viability Assay
Cell viability assay was performed in serum-starved cells treated or not with COX inhibitors in 96 well plates using the CellTiter 96® AQueous Non-Radioactive Cell Proliferation Assay (MTS) (Promega, Madison, WI, USA), based on the manufacturer's recommendations.
Tissue Microarrays and Immunohistochemistry
Individual formalin-fixed HNSCC tissues and tissue microarrays (TMAs) containing approximately 460 cases were obtained from the NIDCR (Bethesda, MD) 9. Briefly, individual paraffin-embedded HNSCC tissues were arrayed and processed following the standard methodology (www.cancer.gov/tarp). Immunohistochemistry was performed as previously described9, using anti–EP1, anti-EP2 (Cayman Chemicals), anti-EP3 (Santa Cruz Biotechnology, Inc.), for 1 h at room temperature and anti-COX-2 (BD Transduction), anti-p53 (Cell Signaling Technology, Inc.) and anti-EGFR (DAKO) overnight at 4°C. Antibodies were diluted 1:100 in 2.5% BSA in PBS, but p53 monoclonal antibody (1:40). All immunostainings were assessed by two experienced pathologists. Images were taken using ScanScope CS System (Aperio Technologies, Inc., Vista, CA, USA). The tumors were scored according to the % of positive tumors cells: 0 (0-10% positive cells), 1 (10-25% positive cells), 2 (25-50% positive cells), 3 (50-75% positive cells) and 4 (75-100% positive cells) and classified a in well differentiated (WD), moderately differentiated (MD) and poorly differentiated (PD)9. Statistical analysis was performed by Spearman correlation, Kruskall-Wallis and Mann Whitney test. p < 0.05 was considered statistically significant. Cluster program with average linkage based on Pearson's correlation coefficient as the selection variable was used for hierarchical analysis, and visualized using the TreeView program9. Two biomarkers with a close relationship are located next to each other.
Results
HNSCC cell lines and tissues express COX-2 and EP1, EP2, and EP3 receptors
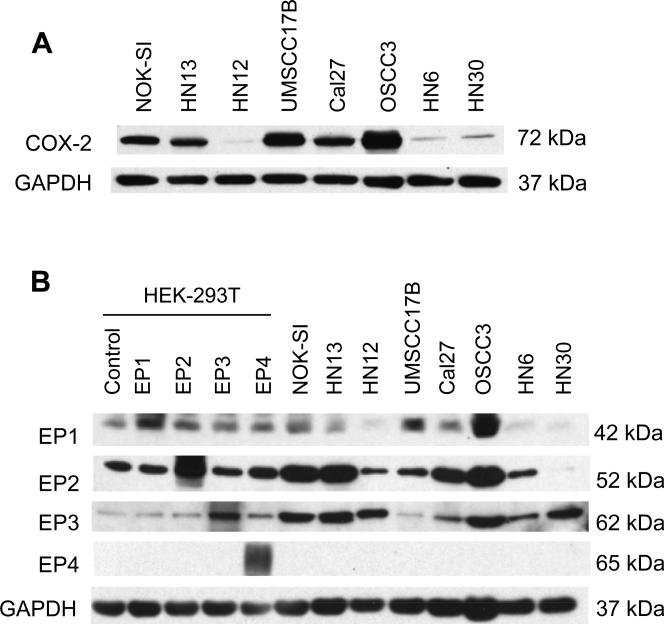
To investigate the expression pattern of COX-2 and the PGE2 receptors EP1-4 in HNSCC, we first performed a Western blotting screening with seven representative HNSCC cell lines, and one human immortalized oral keratinocyte cell line (NOK-SI). Lysates from HEK293T cells transfected with EP1, EP2, EP3 and EP4 expression vectors were used as controls. As shown in Figure 1, all EP receptors were overexpressed in transfected cells. EP1 was detected in four HNSCC cell lines, but EP2 and EP3 were quite widespread, detectable in 6 of the 7 HNSCC cell lines analyzed. None of the HNSCC cell lines expressed EP4 receptors. Normal NOK-SI expressed EP1, EP2, and EP3 but not EP4 receptors. COX-2 expression was observed in 4 out of 7 HNSCC cell lines and in NOK-SI.
Figure 1. HNSCC cell lines express COX-2, EP1, EP2 and EP3 but not EP4 A.
COX-2 expression in HN13, UMSCC17, Cal27, OSCC3 and HN30. B. Expression of the indicated EP receptors was examined in HNSCC cell lines and NOK-SI. Transfected HEK 293T with EP1, EP2, EP3 and EP4 cDNAs (as described in 20) were used as positive controls. GAPDH was used as loading control.
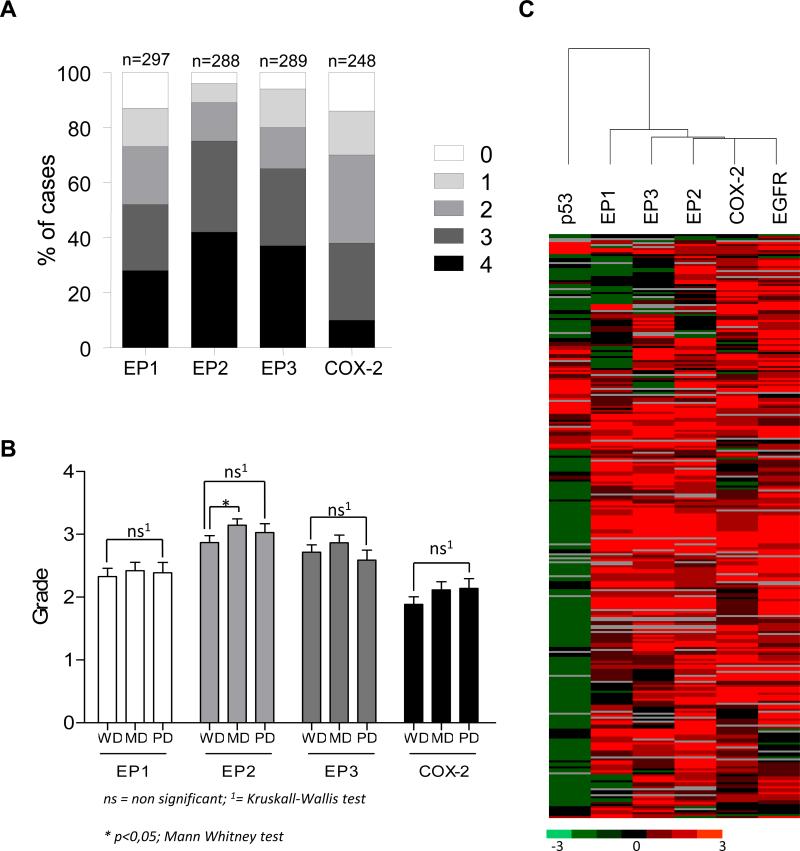
To validate the observations in cell culture, expression analysis was performed by immunohistochemistry in HNSCC TMAs. Analysis of the levels of p53, which reflects the accumulation of its mutant form, and EGFR expression, both of which are highly expressed in HNSCC, served as controls. Two hundred and fourteen cases (86%) were positive for COX-2, 288 (87%) for EP1 receptor, 277 (96%) for EP2 receptor, and 272 for EP3 (94%), with same variations in their staining intensity levels (Figure 2). As a reference, 86 cases were positive for p53 (36%) and 300 for EGFR (97%) as we previously described 9. Most of the positive cases were in a moderate differentiation grade9 for all four markers. Kruskall-Wallis test and the Spearman rank test showed correlation between EP receptors EP1 and EP2, EP1 and EP3, and EP2 and EP3 (Table 1). A correlation was also observed between EP1 and COX-2. The unsupervised cluster analysis and heatmap representation of samples for which at least three of the four markers were available, revealed that COX-2, EP1, EP2 and EP3 clustered together (Figure 3). However, their expression did not correlate with the status of p53 protein expression, suggesting that their upregulation may occur independently form the genetic alterations processes that result in p53 mutations. In this regard, although additional work is necessary, preliminary observations suggest that HNSCC cases expressing p16 are also positive for COX-2 and EP receptors, suggesting the possibility that HPV-associated HNSCC may also express these key pro-inflammatory and growth promoting pathways. Overall, most cancer cells expressing COX-2 also express one or more EP receptors, suggesting that the locally produced PGE2 may act in a paracrine or autocrine fashion on EP receptor-expressing cancer cells.
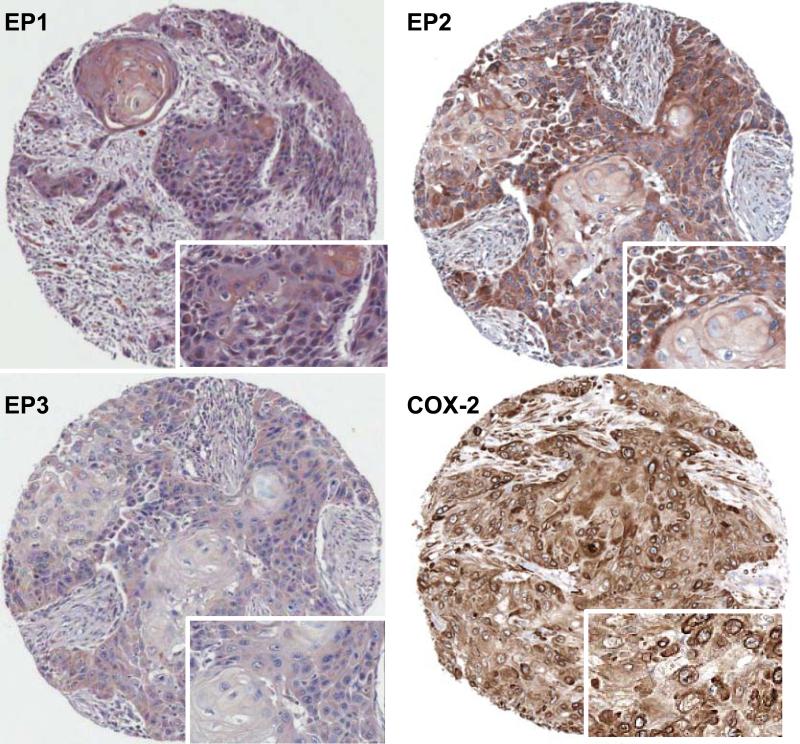
Figure 2. HNSCC tumors express COX-2, EP1, EP2 and EP3.
Representative cores of HNSCC tissues with immunohistochemical staining for the indicated proteins. The four proteins investigated, EP1, EP2, EP3 and COX-2 showed a cytoplasmatic staining. Magnification, x10; insets, x40.
Table 1.
Spearman rank test analyses of the tissue microarray staining
| EP1 | EP2 | EP3 | COX-2 | p53 | EGFR | |
|---|---|---|---|---|---|---|
| EP1 | - | n= 278 p<0.0001*** |
n= 280 p<0.0001*** |
n= 178 p = 0.0264* |
n= 168 p= 0.1067 |
n= 244 p= 0.9020 |
| EP2 | - | - | n= 274 p= 0.0126* |
n= 180 p= 0.0504 |
n= 160 p= 0.0560 |
n= 235 p= 0.6446 |
| EP3 | - | - | - | n= 181 p= 0.1702 |
n= 162 p= 0.1325 |
n= 240 p= 0.6798 |
| COX-2 | - | - | n= 137 p= 0.6700 |
n= 312 p= 0.0025** |
||
| p53 | - | - | n= 254 p= 0.1633 |
p <0,05
p<0,001
p<0,001; n = pair numbers
Figure 3. Expression of PGE2 receptors in human HNSCC.
Immunohistochemical analysis in HNSCC lesions. A-Distribution of the number of positive cases for each marker, depicting their relative staining intensities. B. Distribution of positive cases in relationship to the differentiation degrees. No differences were observed between well differentiated (WD), moderately differentiated (MD) and poorly differentiated (PD) for all proteins (ns) except to EP2 (p<0.05; WD x MD). C. Heat map with cluster analysis showing a strong correlation between EP1, EP2, EP3, and COX-2, suggesting that COX-2 dependent secretion of PGE2 may act in autocrine/paracrine fashion on tumor cells. The expression of EGFR but not p53 correlated with COX-2 and its downstream receptor targets.
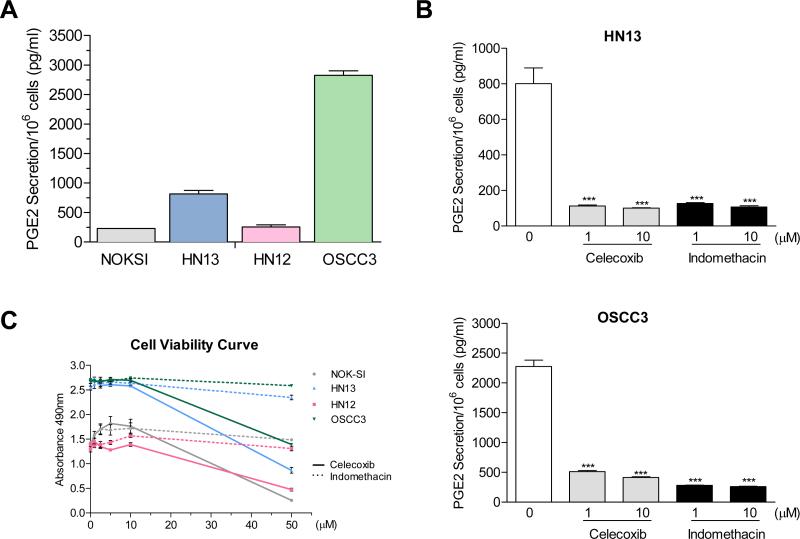
COX-2 inhibitors suppress PGE2 production by HNSCC cell lines but do not affect cell viability
We next explored whether cells expressing both COX-2 and EPs were able to produce PGE2 and to confirm that COX inhibitors were able to reduce its production. Indomethacin is a non-selective COX inhibitor that acts on both COX-1 and COX-2, while celecoxib is a COX-2 selective inhibitor. As an example, HN13 and OSCC3 cell lines produced significant levels of PGE2, which was reduced by indomethacin and celecoxib (Figure 4). Only celecoxib reduced HNSCC cell viability at high concentrations (50 μM), as reported6. However, that was not the case at lower concentrations that may be more clinically relevant, considering that the maximum serum concentration achieved in patients is around 10 μM15, a concentration already effective in inhibiting PGE2 production. On the other hand, NOK-SI cells overexpress COX-2 but release limited amounts of PGE2 (Figure 4A), suggesting that PGE2 production in cancer cells requires molecular alterations in addition to those resulting in COX-2 expression. Together, these observations strongly suggest that COX-2 activity is often elevated in HNSCC cells but that COX-2 inhibition by the use of general or selective COX-2 inhibitors is not sufficient to affect the short term in vitro growth of HNSCC cells at clinically relevant concentrations.
Figure 4. PGE2 secretion in HNSCC cells.
A. PGE2 secretion levels in NOK-SI, HN13, HN12, and OSCC3 cells. B. PGE2 secretion inhibition in OSCC3 and HN13 as representative cells treated with celecoxib and indomethacin for 24h. No differences were observed regarding the COX-2 selectivity of these drugs. Lower doses (1 and 10 μM) were able to inhibit PGE2 secretion (p<0.001). C. MTS viability curve. Drug doses able to inhibit PGE2 secretion had no biological effects in both HNSCC cells and in NOK-SI after 24h of treatment. Similar results were observed after treatment for longer periods of time (2 and 3 days, not shown). Only higher doses decreased cell viability.
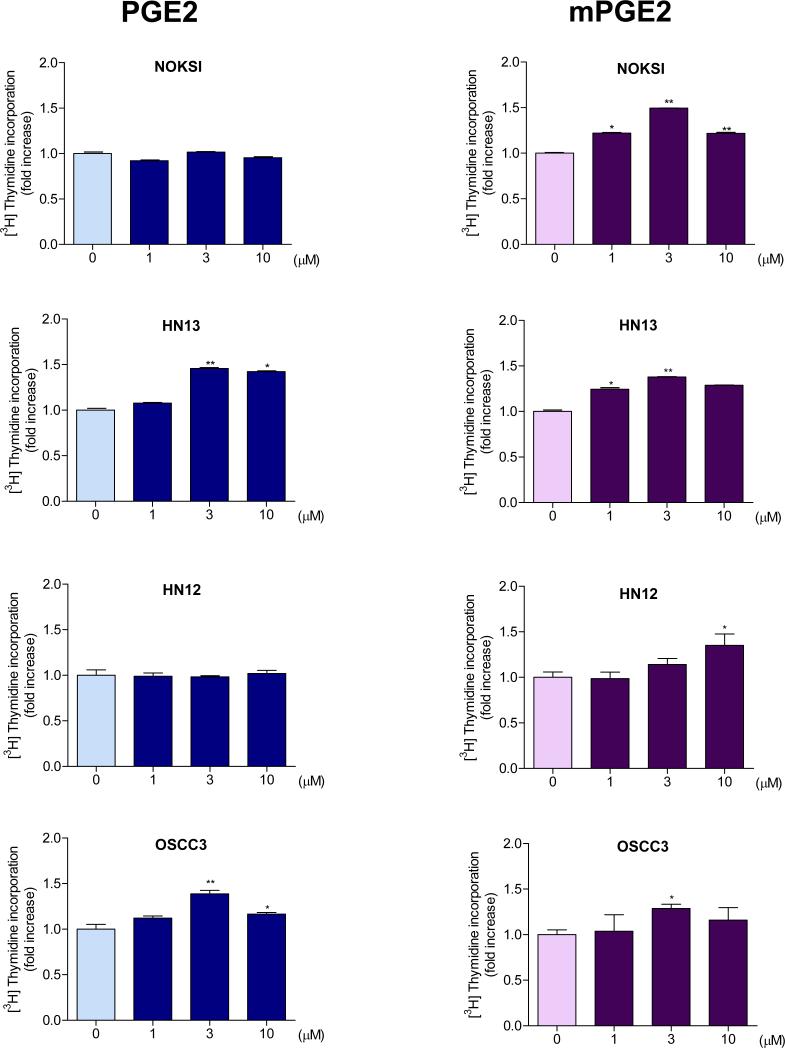
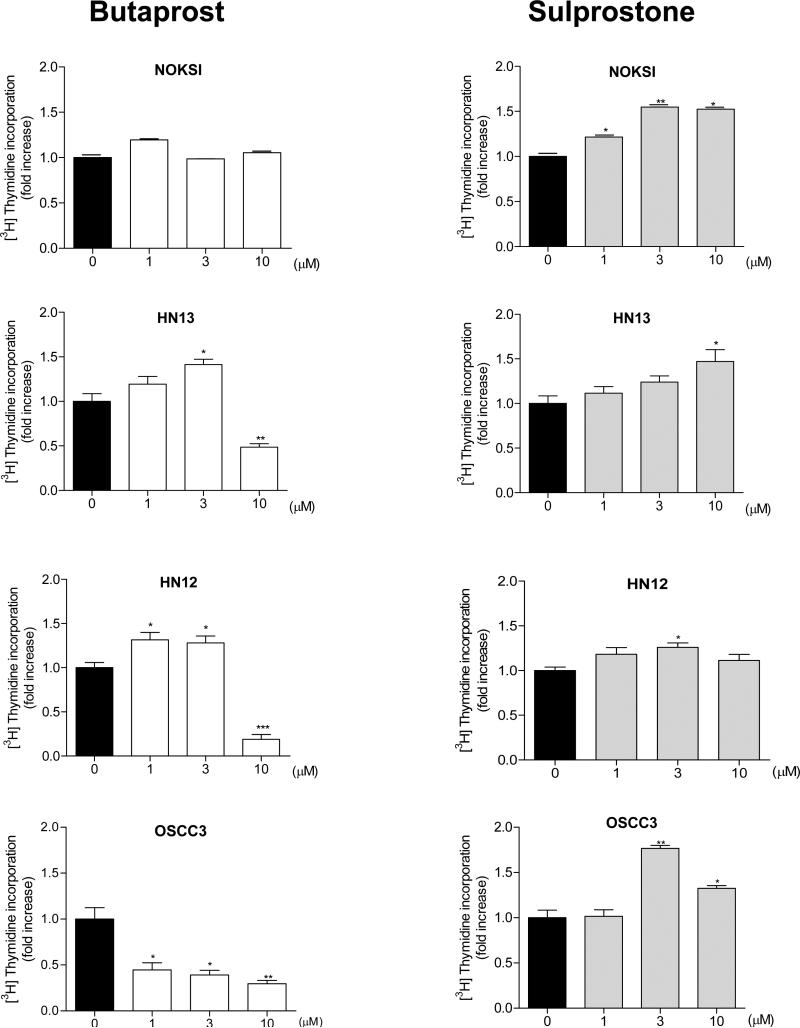
PGE2, dmPGE2, butaprost and sulprostone can induce cell proliferation in HNSCC cell lines
We next explored whether exogenous PGE2 can promote HNSCC cell proliferation and if so addressed which EP receptors contribute to the growth promoting activity of PGE2 in HNSCC cell lines. For these experiments, we stimulated HNSCC cells with PGE2, dmPGE2 (a stable PGE2 analog), butaprost (selective EP2 agonist) and sulprostone (selective EP3 agonist). Both PGE2 and dmPGE2 induced HNSCC cell proliferation significantly (Figure 5). However dmPGE2 proved to be more potent as it stimulated cell proliferation in the three HNSCC cell lines HN13, and in NOK-SI, while PGE2 induced proliferation in HN13 and OSCC3 cells. This difference likely arises from the fact that mPGE2 is a stable analog of PGE2, hence it may remain active for the extended period of time required for mitogenic assays.
Figure 5A. PGE2 and dmPGE2 DNA-synthesis induction in HNSCC cell lines.
HNSCC cell lines were stimulated with the indicated concentrations of PGE2 and mPGE2, and DNA synthesis was investigated by [3H] thymidine incorporation. Similar results were obtained in 2-3 independent experiments for each cell line.
As part of an effort to address which receptors are involved in this growth induction, cells were treated with butaprost and sulprostone, two EP-specific agonists, and found that sulprostone is more efficient than butaprost (Figure 5B). This observation strongly suggests that in HNSCC EP3 is more relevant for cell proliferation induction than EP2. Indeed, sulprostone stimulated all cell lines analyzed. Interestingly at higher doses (10 μM) butaprost dramatically reduced cell proliferation in HN13 and HN12 cells and even lower doses of this drug (1 μM) reduced OSCC3 cell proliferation. This suggests that in some HNSCC cells EP2 may exert a growth inhibitory activity, while EP3 may elicit a pro-proliferative response. As both receptors are activated by PGE2, these data suggest that the balance between these two opposing activities may ultimately determine the biological response to locally produced PGE2.
Figure 5B. Effect of the EP2 agonist, butaprost, and the EP3 agonist, sulprostone, on DNA synthesis in the indicated HNSCC cells.
The EP3 agonist (sulprostone) is a potent mitogen in all HNSCC cell lines tested, whereas the EP2 agonist (butaprost) may exert a variable proliferative or antiproliferative effect.
Discussion
Accumulating evidence shows that COX-2 is widely overexpressed in HNSCC9,11,16-17. Consequently, HNSCC are able to secrete PGE2 16,18-19, but the contribution of PGE2 receptors to HNSCC progression is not fully established. In colon cancer, COX-2 overexpression and PGE2 production is often linked with EP2 activation, which triggers growth promoting signaling pathways such as β-catenin20 as well as leukocyte recruitment and angiogenesis21 by multiple G-protein regulated intracellular signaling pathways4, 21, 22. Aligned with previously published reports, COX-2 was found to be overexpressed in most HNSCC cases, although its expression was observed in 50% of the HNSCC cell lines analyzed. This difference may arise from the observation that COX-2 expression may be reduced in HNSCC during late stages of oral carcinogenesis23, which are the likely origin of most HNSCC cell lines. On the other hand, while inflammatory processes within the tumor microenvironment may account for the widespread expression of COX-2 in tumoral and stromal cells in vivo, COX-2 expression in cultured HNSCC cell lines is variable, as it may depend on multiple molecular mechanisms intrinsically disregulated in these cells24-25. However, even HNSCC cells that do not express COX-2 constitutively can still respond mitogenically to PGE2, as these cancer cells often express one or more PGE2 receptors.
While the role of PGE2 receptors in cancer is well established for colon and lung cancer4, few studies have evaluated their participation in HNSCC6. EP3 antagonists were shown to diminish the growth of HNSCC cells6, aligned with our present observation that EP3 agonists promote mitogenic responses in most HNSCC cell lines tested. In addition, we show here that EP1, EP2 and EP3 receptors are expressed in almost all tumor tissues and cell lines analyzed. While EP4 appears to play a role in colon cancer together with EP220, none of the HNSCC cell lines expressed this EP receptor, suggesting that this receptor likely does not participate in HNSCC, even if these cells may express some EP4 mRNA6, 26. Expression of EP1 and EP3 has been suggested to have prognostic value in HNSCC6, albeit most previous studies analyzed EP1 and EP3 only at the mRNA level26. For example, mRNA expression analysis suggested that EP3 does not contribute to tumor behavior26, but others proposed that EP3 may participate in HNSCC6. On the other hand, EP2 may participate in oesophageal carcinomas27-28 but it may be less relevant for HNSCC as judged by its more limited ability to promote HNSCC cell growth.
Indeed, which EP receptor can transduce PGE2-induced proliferative signals in HNSCC is poorly understood. We observed that PGE2 can induce DNA-synthesis in HNSCC cells, with dmPGE2 more potent than PGE2, given its enhanced stability. The EP2 agonist butaprost and the EP3 agonist sulprostone can induce cell proliferation, but the EP2 agonist reduced proliferation at higher doses, while sulprostone promoted DNA-synthesis in all cell lines tested. Altogether, our emerging results based on EP agonist selectivity and levels of EP receptor expression suggest that while EP2 may play a role in HNSCC, EP3 may represent the most widely and likely candidate to mediate the proliferative responses to PGE2, and hence to this potent inflammatory mediator that accumulates in HNSCC lesions.
The knowledge of dysregulated molecular mechanisms underlying the maintenance and the progression of HNSCC may provide a rational foundation to explore new treatment modalities and may provide valuable tools for the development of novel molecular-targeted therapies. COX-2 seems to act in the initial phases of HNSCC progression, but its specific targets are yet to be identified. In this regard, PGE2 is likely to accumulate at very high levels in the tumor microenvironment, as it can be produced by the action of COX2 expressed in both cancer and stromal cells. Hence, by acting on EP receptors expressed in HNSCC cells, PGE2 may contribute to increase HNSCC cell proliferative potential. In this regard, COX-2 and PGE2 blocking therapies, as well as EP3-specific antagonists, may represent helpful approaches as adjuvants in HNSCC treatment for patients at the initial stages of HNSCC development.
Acknowledgements
ACA was supported by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brazil). This work was supported by the Intramural Research Program, National Institutes of Dental and Craniofacial Research (NIDCR), National Institute of Health (NIH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest:
None Declared
References
- 1.Conway DI, Hashibe M, Boffetta P, Wunsch-Filho V, Muscat J, La Vecchia C, et al. Enhancing epidemiologic research on head and neck cancer: INHANCE - The international head and neck cancer epidemiology consortium. Oral Oncol. 2009;45(9):743–6. doi: 10.1016/j.oraloncology.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Molinolo AA, Amornphimoltham P, Squarize CH, Castilho RM, Patel V, Gutkind JS. Dysregulated molecular networks in head and neck carcinogenesis. Oral Oncol. 2009;45(4-5):324–34. doi: 10.1016/j.oraloncology.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curado MP, Hashibe M. Recent changes in the epidemiology of head and neck cancer. Curr Opin Oncol. 2009;21(3):194–200. doi: 10.1097/CCO.0b013e32832a68ca. [DOI] [PubMed] [Google Scholar]
- 4.Dorsam RT, Gutkind JS. G-protein-coupled receptors and cancer. Nat Rev Cancer. 2007;7(2):79–94. doi: 10.1038/nrc2069. [DOI] [PubMed] [Google Scholar]
- 5.Fujino H, Chen XB, Regan JW, Murayama T. Indomethacin decreases EP2 prostanoid receptor expression in colon cancer cells. Biochem Biophys Res Commun. 2007;359(3):568–73. doi: 10.1016/j.bbrc.2007.05.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoshikawa H, Goto R, Mori T, Mitani T, Mori N. Expression of prostaglandin E2 receptors in oral squamous cell carcinomas and growth inhibitory effects of an EP3 selective antagonist, ONO-AE3-240. Int J Oncol. 2009;34(3):847–52. doi: 10.3892/ijo_00000211. [DOI] [PubMed] [Google Scholar]
- 7.Kismet K, Akay MT, Abbasoglu O, Ercan A. Celecoxib: a potent cyclooxygenase-2 inhibitor in cancer prevention. Cancer Detect Prev. 2004;28(2):127–42. doi: 10.1016/j.cdp.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Greenhough A, Smartt HJ, Moore AE, Roberts HR, Williams AC, Paraskeva C, et al. The COX-2/PGE2 pathway: key roles in the hallmarks of cancer and adaptation to the tumour microenvironment. Carcinogenesis. 2009;30(3):377–86. doi: 10.1093/carcin/bgp014. [DOI] [PubMed] [Google Scholar]
- 9.Molinolo AA, Hewitt SM, Amornphimoltham P, Keelawat S, Rangdaeng S, Meneses Garcia A, et al. Dissecting the Akt/mammalian target of rapamycin signaling network: emerging results from the head and neck cancer tissue array initiative. Clin Cancer Res. 2007;13(17):4964–73. doi: 10.1158/1078-0432.CCR-07-1041. [DOI] [PubMed] [Google Scholar]
- 10.Nathan CO, Leskov IL, Lin M, Abreo FW, Shi R, Hartman GH, et al. COX-2 expression in dysplasia of the head and neck: correlation with elF4E. Cancer. 2001;92(7):1888–95. doi: 10.1002/1097-0142(20011001)92:7<1888::aid-cncr1706>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 11.Itoh S, Matsui K, Furuta I, Takano Y. Immunohistochemical study on overexpression of cyclooxygenase-2 in squamous cell carcinoma of the oral cavity: its importance as a prognostic predictor. Oral Oncol. 2003;39(8):829–35. doi: 10.1016/s1368-8375(03)00105-2. [DOI] [PubMed] [Google Scholar]
- 12.Renkonen J, Wolff H, Paavonen T. Expression of cyclo-oxygenase-2 in human tongue carcinoma and its precursor lesions. Virchows Arch. 2002;440(6):594–7. doi: 10.1007/s00428-002-0616-y. [DOI] [PubMed] [Google Scholar]
- 13.Sonoshita M, Takaku K, Oshima M, Sugihara K, Taketo MM. Cyclooxygenase-2 expression in fibroblasts and endothelial cells of intestinal polyps. Cancer Res. 2002;62(23):6846–9. [PubMed] [Google Scholar]
- 14.Amano H, Hayashi I, Endo H, Kitasato H, Yamashina S, Maruyama T, et al. Host prostaglandin E(2)-EP3 signaling regulates tumor-associated angiogenesis and tumor growth. J Exp Med. 2003;197(2):221–32. doi: 10.1084/jem.20021408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schonthal AH, Chen TC, Hofman FM, Louie SG, Petasis NA. Celecoxib analogs that lack COX-2 inhibitory function: preclinical development of novel anticancer drugs. Expert Opin Investig Drugs. 2008;17(2):197–208. doi: 10.1517/13543784.17.2.197. [DOI] [PubMed] [Google Scholar]
- 16.Gallo O, Masini E, Bianchi B, Bruschini L, Paglierani M, Franchi A. Prognostic significance of cyclooxygenase-2 pathway and angiogenesis in head and neck squamous cell carcinoma. Hum Pathol. 2002;33(7):708–14. doi: 10.1053/hupa.2002.125376. [DOI] [PubMed] [Google Scholar]
- 17.Chan G, Boyle JO, Yang EK, Zhang F, Sacks PG, Shah JP, et al. Cyclooxygenase-2 expression is up-regulated in squamous cell carcinoma of the head and neck. Cancer Res. 1999;59(5):991–4. [PubMed] [Google Scholar]
- 18.Schuon R, Brieger J, Franke RL, Jakob R, Mann WJ. Increased PGE2 levels in nonmalignant mucosa adjacent to squamous cell carcinoma of the head and neck. ORL J Otorhinolaryngol Relat Spec. 2005;67(2):96–100. doi: 10.1159/000084996. [DOI] [PubMed] [Google Scholar]
- 19.Snyderman CH, Milanovich M, Wagner RL, Johnson JT. Prognostic significance of prostaglandin E2 production in fresh tissues of head and neck cancer patients. Head Neck. 1995;17(2):108–13. doi: 10.1002/hed.2880170206. [DOI] [PubMed] [Google Scholar]
- 20.Castellone MD, Teramoto H, Williams BO, Druey KM, Gutkind JS. Prostaglandin E2 promotes colon cancer cell growth through a Gs-axin-beta-catenin signaling axis. Science. 2005;310(5753):1504–10. doi: 10.1126/science.1116221. [DOI] [PubMed] [Google Scholar]
- 21.Narumiya S. Prostanoids and inflammation: a new concept arising from receptor knockout mice. J Mol Med. 2009;87(10):1015–22. doi: 10.1007/s00109-009-0500-1. [DOI] [PubMed] [Google Scholar]
- 22.Sugimoto Y, Narumiya S. Prostaglandin E receptors. J Biol Chem. 2007;282(16):11613–7. doi: 10.1074/jbc.R600038200. [DOI] [PubMed] [Google Scholar]
- 23.Saba NF, Choi M, Muller S, Shin HJ, Tighiouart M, Papadimitrakopoulou VA, et al. Role of cyclooxygenase-2 in tumor progression and survival of head and neck squamous cell carcinoma. Cancer Prev Res (Phila Pa) 2009;2(9):823–9. doi: 10.1158/1940-6207.CAPR-09-0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Husvik C, Bryne M, Halstensen TS. Epidermal growth factor-induced cyclooxygenase-2 expression in oral squamous cell carcinoma cell lines is mediated through extracellular signal-regulated kinase 1/2 and p38 but is Src and nuclear factor-kappa B independent. Eur J Oral Sci. 2009;117(5):528–35. doi: 10.1111/j.1600-0722.2009.00669.x. [DOI] [PubMed] [Google Scholar]
- 25.Soland TM, Husvik C, Koppang HS, Boysen M, Sandvik L, Clausen OP, et al. A study of phosphorylated ERK1/2 and COX-2 in early stage (T1-T2) oral squamous cell carcinomas. J Oral Pathol Med. 2008;37(9):535–42. doi: 10.1111/j.1600-0714.2008.00656.x. [DOI] [PubMed] [Google Scholar]
- 26.Camacho M, Leon X, Fernandez-Figueras MT, Quer M, Vila L. Prostaglandin E(2) pathway in head and neck squamous cell carcinoma. Head Neck. 2008;30(9):1175–81. doi: 10.1002/hed.20850. [DOI] [PubMed] [Google Scholar]
- 27.Kuo KT, Wang HW, Chou TY, Hsu WH, Hsu HS, Lin CH, et al. Prognostic role of PGE2 receptor EP2 in esophageal squamous cell carcinoma. Ann Surg Oncol. 2009;16(2):352–60. doi: 10.1245/s10434-008-0242-2. [DOI] [PubMed] [Google Scholar]
- 28.Yu L, Wu WK, Li ZJ, Wong HP, Tai EK, Li HT, et al. E series of prostaglandin receptor 2-mediated activation of extracellular signal-regulated kinase/activator protein-1 signaling is required for the mitogenic action of prostaglandin E2 in esophageal squamous-cell carcinoma. J Pharmacol Exp Ther. 2008;327(1):258–67. doi: 10.1124/jpet.108.141275. [DOI] [PubMed] [Google Scholar]