Abstract
Objectives
To characterize the proportion of older adult ED patients with depression or cognitive impairment. To compare the prevalence of depression or cognitive impairment among ED patients arriving via EMS, as compared to other modes.
Methods
Community-dwelling older adults (age≥60) presenting to an academic medical center ED were interviewed. Participants provided demographic and clinical information, and were evaluated for depression and cognitive impairment. Subjects arriving via EMS were compared to those arriving via other modes using the chi-square test, t-test, and the Wilcoxon rank sum test, where appropriate.
Results
Consent was obtained from 1342 eligible older adults; 695 (52%) arrived via EMS. The median age for those arriving via EMS was 74 (IQR 65, 82), 52% were female, 81% white. 15% of EMS patients had moderate or greater depression, as compared to 14% of patients arriving via other modes (p=0.52). 13% of EMS patients had cognitive impairment, as compared to 8% arriving via other modes (p<0.01). Depressed EMS patients frequently reported a history of depression (47%) and taking antidepressants (51%). Cognitively impaired EMS patients infrequently reported a history of dementia (16%) or taking medications for dementia (14%).
Conclusions
In this cohort of community-dwelling older adult ED patients depression and cognitive impairment were common. As compared to ED patients arriving by other transport means, patients arriving via EMS had similar prevalence of depression but an increased prevalence of cognitive impairment. Screening for depression and cognitive impairment by EMS providers may have value, but needs further investigation.
Keywords: Emergency medical services, Prehospital care, Depression, Cognitive Impairment, Geriatrics
Background
Older adults are the fastest growing segment of the United States population.1 Use of emergency medical services (EMS) by older adults is frequent and rapidly increasing. A recent study showed that individuals aged 65 and older comprised 38% of EMS patients between 1999 and 2003.2 These trends suggest that older adults will comprise an increasing proportion of emergency care patients. 3
Depression and cognitive impairment are common among older adults. Estimates in the United States are that 1-4% of community-dwelling older individuals are depressed,4 and 8-16% manifest clinically important depressive symptoms.5, 6 Additionally, studies report that approximately 10% of community-dwelling older individuals have dementia and approximately 20% suffer from cognitive impairment without dementia.7,8 Primary care physicians do not identify depression and cognitive impairment in up to half of patients with the conditions. As such, patients are not informed about their health status, they cannot inform EMS or ED providers, and do not receive available therapies.9,10,11,12,13, 14 Since EMS providers do not routinely screen for either depression or cognitive impairment and emergency physicians also frequently fail to identify cognitively impaired older patients in the ED, large numbers of affected patients remain undetected.15
The failure to identify older adults with these conditions may have significant consequences upon patient outcomes. Studies have shown that hospitalized depressed or cognitively impaired patients suffer increased morbidity and mortality and use increased healthcare resources, as compared to those who lack these conditions.16,17,18,19,20,21,22,23 Furthermore, a recent study has shown that cognitively impaired older adults often do not understand medical discussions such as discharge and refusal of medical care instructions.24,25
To our knowledge, no study has characterized the proportion of EMS patients who suffer from depression or cognitive impairment. Through this study we aim to describe the characteristics of older adults who presented to an ED. Specifically we aim to compare the proportion of patients who screened positive for depression or cognitive impairment among those arriving at the ED via EMS as compared to arrival independent of EMS. We hypothesize that there would be no difference in depression or cognitive impairment rates between those arriving to the ED via EMS or those arriving by other transport means. Lastly, we aim to describe the characteristics of EMS patients who screened positive for depression or cognitive impairment.
Methods
Study Design
We performed a prospective cohort study of older adults (age≥60) during their ED visits at the University of Rochester Medical Center (URMC) between May 26 and July 31, 2008. The URMC is a 740-bed academic medical center that is the major tertiary referral center for the region. The URMC ED cares for approximately 97,000 patients annually. The institution's Research Subjects Review Board approved the conduct of this study with written consent.
Study Setting and Population
Subjects were eligible during their ED visit if they were age 60 years of age or older and if they presented for medical (including trauma) care. They were excluded if they were institutionalized (e.g., prisoner, nursing home resident), did not speak English, or could not interact with the study staff. Additionally, if the subject lacked decisional capacity and lacked an authorized representative to consent, we could not include them despite being eligible. If a patient presented to the ED more than once during the recruitment period, only their first visit was included in this analysis, resulting in 1 ED visit per subject.
Protocol
Dedicated study staff was present in the ED daily from 8am to 11pm. They were trained to enroll all eligible subjects who were in the ED during those hours. Thus, eligible subjects who arrived in the ED and left during the overnight hours were not included. Some patients who arrived during the day may have also been missed if their ED length of stay was extremely short. For instance, a patient with a myocardial infarction would rapidly go to the cardiac catheterization laboratory and a patient suffering major trauma may rapidly go to the operating room. These patients would not have been approached for enrollment in this study.
The study staff identified potentially eligible patients by monitoring the ED information system tracking board. Study staff approached all potentially eligible subjects and determined whether they had decisional capacity, or a proxy with them to provide informed consent. After determining decisional capacity, study staff obtained informed consent and interviewed the participating subject. The interview included obtaining demographic and clinical variables, determining each patient's mode of arrival, and evaluating depression, cognitive impairment, anxiety, and delirium. Some demographic and clinical information was also obtained via structured chart review. Key variables from chart review included the Emergency Severity Index and the ED disposition.26 However, we obtained the majority of information via self-report to maximize the accuracy of information such as marital status, race, ethnicity, education, and living arrangement.
Related to depression, we asked if they had a depression history and also reviewed the ED medical record to identify any notation regarding depression. Related to cognitive impairment, we asked patients if they had a history of “dementia” or took medications for “memory problems”. We elected not to use the term “cognitive impairment” since we felt that most patients would not understand its meaning. The ED medical record was reviewed for any notation regarding chronic cognitive impairment (e.g., Alzheimer's disease, dementia). If either the patient self-report or the medical record indicated the presence of depression or cognitive impairment, then the condition was considered present.
To evaluate for depression, we used the Patient Health Questionnaire-9 (PHQ-9). It is a short nine item instrument that has been validated in primary care and has excellent test characteristics, with a sensitivity and specificity of 88% (Appendix).27,28 Patients with a symptom score of greater than or equal to 10 were considered to have clinically significant depressive symptoms, which we refer to as depression. To evaluate for cognitive impairment, patients were screened with the Six Item Screener (SIS). It is a short six item instrument validated in primary care with excellent test characteristics. Additionally, it is easy to administer and does not require arm mobility or visuospatial skills, which may be limited in the ED setting due to injuries, medical equipment on the arm, and visual difficulties due to patients' failure to bring glasses to the ED (Appendix).29,30 Greater than two errors on the instrument were considered positive for cognitive impairment to maximize specificity (97%) while accepting a slightly lower sensitivity (50%).29 These instruments were chosen due to their good test characteristics and because they are short taking only a few minutes to complete, do not require special equipment or training; thus they can be easily administered in the acute care setting.
For additional descriptive purposes, we evaluated delirium, an important potential explanation for cognitive impairment, using the Confusion Assessment Method (CAM). The CAM is a validated and widely accepted measure to evaluate for delirium, including in the emergency care setting.15,31 We also evaluated patients for moderate or greater anxiety using the Generalized Anxiety Disorder-7 instrument, a seven item instrument which has been validated although not in emergency care settings.32 These scales were integrated into the interview and chart abstraction form.
The interview and chart abstraction form was tested and revised in an iterative fashion to improve usability and efficiency. Study staff was trained in the use of these scales and the interview and chart abstraction form by the investigators. Study investigators also observed study staff complete interviews before they independently enrolled and screened subjects.
Data Analysis
We analyzed the data using Stata 8.0 (Stata Corp., College Station, TX). Participating individuals were characterized using descriptive statistics. Patients arriving via EMS were compared to those arriving independent of EMS using the chi-square test for dichotomous variables, t-test for normally distributed continuous variables, and the Wilcoxon rank sum test for non-parametric continuous variables. A p-value <0.05 defined statistical significance.
Prior to performing the study, a sample size calculation was performed. Based on previous convenience sample studies, we conservatively estimated that no more than 30% of EMS patients would be depressed and no more than 15% would have cognitive impairment. We wished for the confidence interval to be within 5%, requiring 400 subjects in each arm. For the comparison of patients arriving via EMS to patients arriving via other modes, we wished to identify a 10% difference between the EMS and prevalence of cognitive impairment with 90% power. Similarly, we wished to identify the same difference for depression. To do so, we estimated that we needed 500 subjects in each group. The final targeted sample size, which exceeded these numbers, was driven by calculations from another part of this study not presented here.
Results
Figure 1 depicts the subject enrollment in the study. There were 2053 patient visits that were eligible and were approached for consent. Of those patient visits which met the inclusion criteria, 81 did not have decisional capacity, or a proxy, and were excluded from participation, 475 refused participation, and 75 refused participation because they were previously enrolled. We obtained consent from 1342 unique individuals who presented at 1422 patient visits, or 69% of all eligible patient visits. The 1342 unique subjects and their first ED visit for the study period serve as the study population for these analyses. Eighty-one individuals, 62 of whom arrived via EMS, could not be consented due to the subjects' lack of decisional capacity and the absence of a proxy. Of the 1342 unique individuals who consented to participate, 695 (52%) arrived via EMS (ground or air) and 647 (48%) arrived independent of EMS. Table 1 shows the demographic and clinical characteristics of the EMS arrivals, as well as the characteristics of those arriving independent of EMS. Of interest, both groups were comparable, except for patients arriving via EMS had less education and more frequently reported having depression, having dementia, taking medications for depression, living in assisted living facilities. Additionally, they were more likely to be admitted to the hospital.
Figure 1. Subject Enrollment in the Study.
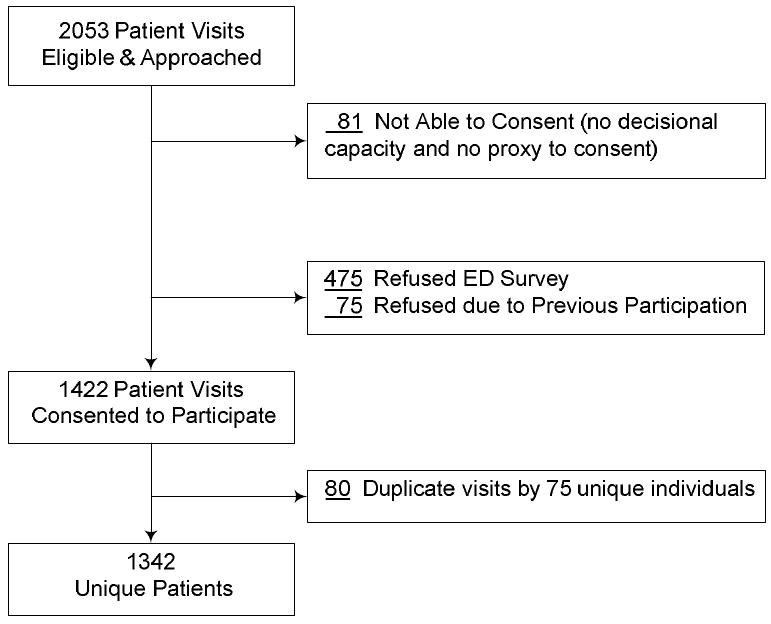
Table 1. Subject Characteristics (N=1342).
| Characteristic | Arrive via EMS (N=695) |
Arrive Independent of EMS (N=647) |
|---|---|---|
| Age, years (median, IQR) | 74 (65, 82) | 70 (65, 78) |
| Gender, Female | 358 (52%) | 343 (53%) |
| Race | ||
| White | 566 (81%) | 522 (81%) |
| Black | 85 (12%) | 105 (16%) |
| Other / Unknown / No Answer | 44 (7%) | 20 (3%) |
| Ethnicity | ||
| Hispanic | 9 (1%) | 4 (1%) |
| Not Hispanic | 650 (94%) | 625 (97%) |
| Unknown / No Answer | 36 (5%) | 18 (3%) |
| Current Marital Status | ||
| Single, never married | 63 (9%) | 56 (9%) |
| Married | 327 (47%) | 342 (53%) |
| Widowed | 192 (28%) | 157 (24%) |
| Divorced / Separated | 81 (12%) | 79 (12%) |
| Unknown / No Answer | 32 (5%) | 13 (2%) |
| Education* | ||
| >High School Diploma | 327 (47%) | 334 (52%) |
| High School Diploma or Less | 333 (48%) | 299 (46%) |
| Unknown / No Answer | 35 (5%) | 14 (2%) |
| Current Living Arrangements* | ||
| Own Home / Apartment | 602 (87%) | 615 (95%) |
| Assisted Living | 52 (7%) | 15 (2%) |
| Other / Unknown / No Answer | 41 (6%) | 17 (3%) |
| Self- or Medical Record-Reported History of: | ||
| Depression* | 130 (19%) | 93 (14%) |
| Dementia * | 32 (5%) | 16 (2%) |
| Self- or Medical Record-Reported Medications (if known) for: | ||
| Depression* | 182 (26%) | 141 (22%) |
| Dementia | 21 (3%) | 16 (2%) |
| ED Use in Past 3 Months | 203 (29%) | 194 (30%) |
| Hospitalized in Past 3 Months | 162 (23%) | 140 (22%) |
| Emergency Severity Index Score* | ||
| 1 | 17 (2%) | 5 (0.8%) |
| 2 | 309 (44%) | 287 (44%) |
| 3 | 341 (49%) | 309 (48%) |
| 4 | 27 (4%) | 43 (7%) |
| 5 | 1 (0.1%) | 3 (0.5%) |
| Chief Complaints (top 10 categories)* | ||
| Cardiovascular | 140 (20%) | 117 (18%) |
| Gastrointestinal (includes abdominal pain) | 73 (10%) | 141 (22%) |
| Muscular/skeletal (non-fall) | 98 (14%) | 63 (10%) |
| Respiratory | 59 (8%) | 51 (8%) |
| General Illness / Possible Infection | 49 (7%) | 64 (10%) |
| Fall | 64 (9%) | 20 (3%) |
| Neurological | 40 (6%) | 45 (7%) |
| Dizzy / Near-syncope / Syncope | 64 (9%) | 25 (4%) |
| Pain | 25 (4%) | 32 (5%) |
| Abnormal Lab Test | 16 (2%) | 16 (2%) |
| Disposition from ED* | ||
| Discharged Home From ED / ED Observation Unit | 427 (61%) | 424 (66%) |
| Admitted, Inpatient Unit | 237 (34%) | 208 (32%) |
| Admitted, Intensive Care Unit | 20 (2.9%) | 14 (2.2%) |
| Other / Unknown | 11 (1.6%) | 1 (0.2%) |
| ED Anxiety (GAD-7) | ||
| Anxious, ≥10 points | 74 (11%)a | 58 (9%)b |
| Score (median, IQR) | 2 (0, 5)a | 2 (0, 5)b |
| ED Delirium (Confusion Assessment Method) | ||
| Delirious | 5 (0.7%) | 3 (0.5%) |
p<0.05,
N=678,
N=638
Table 2 shows the prevalence of depression and cognitive impairment of patients arriving via EMS, as tested by study staff in the ED. Depression was identified in 99 / 668 (15%) patients who arrived via EMS and completed the full PHQ-9. Cognitive impairment was identified in 86 / 687 (14%) patients who arrived via EMS and completed the full SIS. When compared to patients who arrived independent of EMS, EMS patients had an almost equal prevalence of depression (15% via EMS, 14% independent of EMS) and a statistically significant increased prevalence of cognitive impairment (13% via EMS, 8% independent of EMS, p<0.01).
Table 2. Depression and Cognitive Impairment Among Patients Arriving via EMS and Independent of EMS.
| Characteristic | Arrive via EMS | Arrive Independent of EMS | |
|---|---|---|---|
| All Patients | Depression (PHQ-9) | ||
| Depressed, ≥10 points | 99 (15%) | 86 (14%) | |
| Score (median, IQR) | 3 (1, 7) | 3 (1, 7) | |
| N=668 | N=634 | ||
| Cognitive Impairment (Six Item Screener)* | |||
| Impaired, >2 errors | 86 (13%) | 53 (8%) | |
| N=687 | N=642 | ||
| Patients Discharged from the ED / ED Observation Unit | Depression (PHQ-9) | ||
| Depressed, ≥10 points | 55 (13%) | 47 (11%) | |
| Score (median, IQR) | 3 (1, 6) | 3 (1, 6) | |
| N=415 | N=415 | ||
| Cognitive Impairment (Six Item Screener) | |||
| Impaired, >2 errors | 46 (11%) | 32 (8%) | |
| N=423 | N=421 | ||
| Patients Admitted to the Hospital | Depression (PHQ-9) | ||
| Depressed, ≥10 points | 43 (18%) | 39 (18%) | |
| Score (median, IQR) | 4 (1, 7) | 4 (2, 8) | |
| N=242 | N=218 | ||
| Cognitive Impairment (Six Item Screener)* | |||
| Impaired, >2 errors | 40 (16%) | 21 (10%) | |
| N=253 | N=220 | ||
p<0.05
We stratified the prevalence of depression and cognitive impairment between those who were discharged from the ED or the ED Observation Unit and those admitted to the hospital to see if differences between patients arriving via EMS and independent of EMS became evident. For depression, no difference was seen. However, the rates of cognitive impairment were significantly higher among patients who arrived via EMS and were admitted to the hospital, as compared to those arriving via other means and admitted to the hospital.
We further described the older adult EMS patients who tested positive for depression or cognitive impairment to examine their specific demographic and clinical characteristics (Table 3). It is interesting to note that individuals testing positive for depression reported no history or medications for depression approximately half the time, thus indicating that the presence of depression on the problem list or antidepressants on the medication list does not indicate the existence of clinically important depressive symptoms. Similarly, individuals testing positive for cognitive impairment usually reported no history or medications for dementia, thus indicating that the presence of dementia on the problem list or dementia medications on the medication list does not indicate the existence of cognitive impairment. Anxiety was frequently present among those with depression, but neither anxiety nor delirium were frequently present among those with cognitive impairment.
Table 3. Characteristics of Depressed and Cognitively Impaired EMS Patients.
| Characteristic | Depressed Patients (N=99)* | Cognitively Impaired Patients (N=86)* |
|---|---|---|
| Age, years (median, IQR) | 70 (63, 81) | 81.5 (75, 86) |
| Gender, Female | 52 (53%) | 43 (50%) |
| Race | ||
| White | 81 (82%) | 70 (81%) |
| Black | 15 (15%) | 8 (9%) |
| Other / Unknown / No Answer | 3 (3%) | 8 (9%) |
| Ethnicity | ||
| Hispanic | 3 (3%) | 2 (2%) |
| Not Hispanic | 94 (95%) | 76 (88%) |
| Unknown / No Answer | 2 (2%) | 8 (9%) |
| Current Marital Status | ||
| Single, never married | 14 (14%) | 5 (6%) |
| Married | 42 (42%) | 31 (36%) |
| Widowed | 23 (23%) | 31 (36%) |
| Divorced / Separated | 18 (18%) | 10 (12%) |
| Unknown / No Answer | 2 (2%) | 9 (10%) |
| Education | ||
| >High School Diploma | 34 (34%) | 30 (35%) |
| High School Diploma or Less | 63 (64%) | 50 (57%) |
| Unknown / No Answer | 2 (2%) | 7 (8%) |
| Current Living Arrangements | ||
| Own Home / Apartment | 86 (87%) | 67 (78%) |
| Assisted Living | 8 (8%) | 12 (14%) |
| Other / Unknown / No Answer | 4 (4%) | 7 (8%) |
| Self- or Medical Record-Reported History of: | ||
| Depression | 47 (47%) | 16 (19%) |
| Dementia | 6 (6%) | 14 (16%) |
| Self- or Medical Record-Reported Medications for: | ||
| Depression | 50 (51%) | 25 (29%) |
| Dementia | 5 (5%) | 12 (14%) |
| ED Use in Past 3 Months | 52 (53%) | 29 (34%) |
| Hospitalized in Past 3 Months | 34 (34%) | 21 (24%) |
| Emergency Severity Index Score | ||
| 1 | 1 (1%) | 2 (2%) |
| 2 | 48 (48%) | 42 (49%) |
| 3 | 48 (48%) | 38 (44%) |
| 4 | 2 (2%) | 3 (3%) |
| 5 | 0 (0%) | 1 (1%) |
| Disposition from ED | ||
| Discharged Home From ED / ED Observation | 55 (56%) | 46 (53%) |
| Admitted, Inpatient Unit | 40 (40%) | 39 (45%) |
| Admitted, Intensive Care Unit | 4 (4%) | 1 (1%) |
| ED Depression (PHQ-9), ≥10 points | N/A | 16 (20%) a |
| ED Cognitive Impairment (SIS) | 16 (16%) | N/A |
| ED Anxiety (GAD-7), ≥10 points | 45 (46%) b | 11 (13%) c |
| ED Delirium (Confusion Assessment Method) | 1 (1%) | 2 (2%) c |
N=80;
N=97;
N= 82
Discussion
Depression and cognitive impairment are important conditions that are associated with worse outcomes, both from the diseases themselves and in addition to acute illnesses. This study is the first to characterize and compare the prevalence of depression and cognitive impairment among older adult EMS patients transported to an academic medical center.
We found that depression is common among older adult EMS patients, with 15% testing positive for moderate or severe depressive symptoms using the PHQ-9. The prevalence of moderately depressed older adults was similar among ED patients arriving via EMS as compared to independent of EMS. Our findings are similar to results from community-based studies and one previous ED-based study that included adults of all ages.33 However, the prevalence is notably less than the prevalence among medically hospitalized inpatients and appreciably less than a Canadian ED-based study.34 One may have expected that our prevalence would have approached the hospitalized patient prevalence. However, only 38% of consenting EMS patients were admitted. When stratified by disposition (Table 2), EMS patients admitted to the hospital did have a slightly greater prevalence.
We also found that cognitive impairment is common among older adult EMS patients, with 13% testing positive on the SIS. This prevalence is similar to other ED-based studies. However, our study likely underestimates the true prevalence of cognitive impairment, particularly among patients who arrived via EMS. To participate in this study, subjects needed to show decisional capacity or have an available proxy to provide consent. Eighty-one subjects (Figure 1), 62 of whom arrived via EMS, lacked decisional capacity and lacked a proxy who could provide consent; thus, they were excluded. We anticipate that most of these individuals would have been cognitively impaired, thus increasing the prevalence, particularly among older adults arriving via EMS.
The traditional manner in which both depression and cognitive impairment are identified, through patient provided medical history and medication lists, was remarkably poor at identifying individuals with depressive symptoms or individuals with cognitive impairment. Depression could be identified in almost half the patients, but cognitive impairment could be identified in relatively few patients.
Given the notable proportion of community-dwelling older adult EMS patients with depression or cognitive impairment and the disproportionately greater prevalence of cognitive impairment among EMS patients, as compared to patients arriving via other means, it seems that prehospital identification of these conditions potentially has value. By knowing if patients are cognitively impaired, EMS providers can better gauge the accuracy of patient statements and their understanding of medical instructions if the patients refuse care. Furthermore, prehospital identification of depression and cognitive impairment can provide important information to ED, hospitalist, and primary care physicians. Those physicians could use that knowledge as they evaluate patients and consider whether the patient is safe for discharge after medical care. Information regarding depression can lead to earlier medical and social interventions, thereby reducing morbidity and mortality. Information regarding cognitive impairment can lead to investigations and subsequent interventions. For instance, it can result in an identification of and treatment for delirium that may not be otherwise identified. It can also result in an identification of dementia, thus leading to proactive inpatient interventions to prevent delirium and outpatient medical and social interventions to treat dementia and reduce the personal and caregiver burden.
Prior to implementation of prehospital screening for depression and cognitive impairment, three steps are necessary. First, for EMS providers to properly examine older adults for depression and cognitive impairment, official examination instruments and training in using those instruments need to be provided. Currently, EMS providers receive no training in these medical conditions as part of any national curricula.35, 36 Second, the accuracy and value of performing this evaluation of depression and cognitive impairment in the prehospital setting must be validated. Finally, although a benefit seems likely from evaluating for these conditions, a rigorous outcomes study is needed.
The characteristics of depressed older adults and the characteristics of cognitively impaired older adults in this study were of significant interest. We found that community-dwelling depressed patients who used EMS services for transport to an ED reported frequent EMS use and frequent hospitalizations. This observation warrants further investigation and may warrant creation of programs to see if EMS and ED care can be averted for these patients. Additionally, very few of our cognitively impaired subjects were delirious when evaluated using the CAM. This number may be artificially low because patients had to have decisional capacity or a proxy present to participate, but it may also relate to challenges of applying the CAM in the ED setting. It is possible that cognitive impairment evaluations in the EMS or ED setting may require use of an alternate instrument, such as the CAM-ICU, or require the development of a new instrument that is practical in the emergency care setting.
Limitations
Our findings have to be considered in conjunction with this study's limitations. First, although we were able to approach and consent 69% of eligible subjects, a number of eligible individuals were not included. These subjects potentially could have differed from those included in our analyses. For instance, subjects without decisional capacity and without a proxy were excluded due to the need for written consent, thus the information we could collect on these individuals was limited. Three-fourths of these individuals arrived via EMS and all likely were cognitively impaired. Thus, our prevalence estimates are likely lower than the true estimates, particularly for cognitive impairment. Second, we only evaluated EMS patients at one of four hospitals in our community. It is possible that our sample is not generalizable to the community at-large. Third, we used two widely used instruments, the PHQ-9 and SIS, to identify depression and cognitive impairment, respectively. While they are widely used for research and clinical purposes, they are not “gold standard” diagnostic instruments and have not been specifically validated in the emergency care setting. Thus, some false positive and false negative findings may exist.
Conclusion
In this cohort of community-dwelling older adult ED patients depression and cognitive impairment were common. As compared to ED patients arriving by other transport means, patients arriving via EMS had similar prevalence of depression but an increased prevalence of cognitive impairment. Screening for depression and cognitive impairment by EMS providers may have value, but needs further investigation.
Supplementary Material
Acknowledgments
Dr. Shah is supported by the Paul B. Beeson Career Development Award (NIA 1K23AG028942).
Dr. Conwell was partially supported by NIH grant R24 MH071604.
Dr. Richardson was partially supported by the US Department of Veteran's Administration Center of Excellence Canandaigua, NY
Footnotes
This work was presented at the Society for Academic Emergency Medicine Annual Meeting in New Orleans, LA, May 2009.
References
- 1. [May 1, 2004]; http://www.census.gov/main/www/cen2000.html.
- 2.Nawar EW, Niska RW, Xu J. Advance data from vital and health statistics. 386. Hyattsville, MD: National Center for Health Statistics; 2007. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Summary. [PubMed] [Google Scholar]
- 3.Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008;51(6):769–774. doi: 10.1016/j.annemergmed.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 4.Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307–311. doi: 10.1192/bjp.174.4.307. [DOI] [PubMed] [Google Scholar]
- 5.Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community. Psychiatric Services. 1999;50:1158–1166. doi: 10.1176/ps.50.9.1158. [DOI] [PubMed] [Google Scholar]
- 6.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 7.Graham JE, Rockwood K, Beattie BL, et al. Prevalence and severity of cognitive impairment with and without dementia in an elderly population. Lancet. 1997;349:1793–1796. doi: 10.1016/S0140-6736(97)01007-6. [DOI] [PubMed] [Google Scholar]
- 8.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology. 2007;29:125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romanelli J, Fauerbach J, Buch D, et al. The significance of depression in older patients after myocardial infarction. J Am Geriatr Soc. 2002;50:817–822. doi: 10.1046/j.1532-5415.2002.50205.x. [DOI] [PubMed] [Google Scholar]
- 10.Unutzer J, Katon W, Callahan CM, et al. Depression in a sample of 1801 depressed older adults in primary care. J Am Geriatr Soc. 2003;51:505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- 11.Callahan CM, Hendrie HC, Tierney WM. Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann Intern Med. 1995;122:422–429. doi: 10.7326/0003-4819-122-6-199503150-00004. [DOI] [PubMed] [Google Scholar]
- 12.Boise L, Neal BM, Kaye J. Dementia assessment in primary care: Results from a study in three managed care systems. J Gerontol A Biol Sci Med Sci. 2004;59:M621–M626. doi: 10.1093/gerona/59.6.m621. [DOI] [PubMed] [Google Scholar]
- 13.Bush C, Kozak J, Elmslie Screening for cognitive impairment in the elderly. Can Fam Physician. 1996;43:1763–1768. [PMC free article] [PubMed] [Google Scholar]
- 14.Boustani M, Callahan CM, Unverzagt FW, et al. Implementing a screening and diagnosis program for dementia in primary care. J Gen Intern Med. 2005;20:572–577. doi: 10.1111/j.1525-1497.2005.0126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193–200. doi: 10.1111/j.1553-2712.2008.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koenig HG, Shelp F, Goli V, et al. Survival and healthcare utilization in elderly medical inpatients with major depression. J Am Geriatr Soc. 1989;37:599–606. doi: 10.1111/j.1532-5415.1989.tb01249.x. [DOI] [PubMed] [Google Scholar]
- 17.Parikh R, Robinson R, Lipsey J, et al. The impact of post-stroke depression on recovery in activities of daily living over a 2-year follow-up. Ach Neurol. 1990;47:785–789. doi: 10.1001/archneur.1990.00530070083014. [DOI] [PubMed] [Google Scholar]
- 18.Mossey JM, Knott K, Craik R. The effects of persistent depressive symptoms on hip fracture recovery. J Gerontol. 1990;45:M163–M168. doi: 10.1093/geronj/45.5.m163. [DOI] [PubMed] [Google Scholar]
- 19.Unutzer J, Schoenbaum M, Kanton WJ, et al. Healthcare costs associated with depression in medically ill fee for service Medicare participants. J Am Geriatr Soc. 2009;57:506–510. doi: 10.1111/j.1532-5415.2008.02134.x. [DOI] [PubMed] [Google Scholar]
- 20.Unutzer J, Patrick DL, Simon G, et al. Depressive symptoms and the cost of health services in HMO patients aged 65 years and older. JAMA. 1997;277:1618–1623. doi: 10.1001/jama.1997.03540440052032. [DOI] [PubMed] [Google Scholar]
- 21.Callahan CM, Hui SL, Nienaber NA, et al. Longitudinal study of depression and health services use among elderly primary care patients. J Am Geriatr Soc. 1994;42:833–838. doi: 10.1111/j.1532-5415.1994.tb06554.x. [DOI] [PubMed] [Google Scholar]
- 22.Ballard C, Neill D, O-Brien J, et al. Anxiety, depression, and psychosis in vascular dementia. J Affect Disorders. 2000;59:97–106. doi: 10.1016/s0165-0327(99)00057-9. [DOI] [PubMed] [Google Scholar]
- 23.Steele C, Rovner B, Chase GA, et al. Psychiatric symptoms and nursing home placement of patients with Alzheimer's disease. Am J Psychiatry. 1990;147:1049–1051. doi: 10.1176/ajp.147.8.1049. [DOI] [PubMed] [Google Scholar]
- 24.Bryce SN, Han JH, Kripalani S, et al. Cognitive impairment and comprehension of emergency department discharge instructions in older patients. Ann Emerg Med. 2009;54:S80–S81. doi: 10.1016/j.annemergmed.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chugh A, Williams MV, Grigsby J, Coleman EA. Better transitions: Improving comprehension of discharge instructions. Front Health Serv Manage. 2009;25(3):11–32. [PubMed] [Google Scholar]
- 26.Baumann MR, Strout TD. Triage of geriatric patients in the emergency department: validity and survival with the Emergency Severity Index. Ann Emerg Med. 2007;49(2):234–240. doi: 10.1016/j.annemergmed.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The MacArthur Initiative on Depression and Primary Care. [April 19, 2010]; www.depression-primarycare.org.
- 29.Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Shah MN, Karuza J, Rueckmann E, Swanson P, Conwell Y, Katz P. Reliability and validity of prehospital case finding for depression and cognitive impairment. Journal of the American Geriatric Society. 2009;57:697–702. doi: 10.1111/j.1532-5415.2009.02185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lewis L, Miller D, Morley J, et al. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;13:142–145. doi: 10.1016/0735-6757(95)90080-2. [DOI] [PubMed] [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 33.Hoyer D, David E. Screening for depression in emergency department patients. J Emerg Med. 2008 doi: 10.1016/j.jemermed.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 34.McCusker J, Bellavance F, Cardin S, Trepanier S. Screening for geriatric problems in the emergency department: Reliability and validity. Academic Emergency Medicine. 1998;5(9):883–893. doi: 10.1111/j.1553-2712.1998.tb02818.x. [DOI] [PubMed] [Google Scholar]
- 35.US Department of Transportation/National Highway Traffic Safety Administration. Emergency Medical Technician Paramedic: National Standard Curriculum. Release of 1998 [on-line] [June 29, 2006]; Available at http://www.nhtsa.gov/people/injury/ems/EMT-P/disk_1%5B1%5D/index.htm.
- 36.US Department of Transportation/National Highway Traffic Safety Administration. Emergency medical technician-basic: National standard curriculum [on-line] [December 26, 2004]; Available at http://www.nhtsa.dot.gov/people/injury/ems/pub/emtbnsc.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


