Abstract
Purpose
We aimed to evaluate the efficacy of warm water sitz baths in patients who have undergone transurethral resection of the prostate (TURP) owing to lower urinary tract symptoms secondary to benign prostatic hyperplasia.
Materials and Methods
We reviewed the records of 1,783 patients who had undergone TURP between 2001 and 2009. In the warm water sitz bath group, patients were instructed to sit in a tub containing lukewarm water at 40-45℃ for 10 minutes each time. Patients were advised to perform the procedure for at least 5 days immediately after the removal of a Foley urethral catheter. The differences in post-TURP complications between the warm water sitz bath group and the no sitz bath group were compared.
Results
After TURP, 359 of the 1,561 patients performed a warm water sitz bath. Complications after TURP, such as hemorrhage, urinary tract infection, urethral stricture, and acute urinary retention were found in 19 (5.3%) and 75 (6.2%) patients in the sitz bath and no sitz bath groups, respectively (p=0.09). There was a significant difference in postoperative complications such as urethral stricture between the warm sitz bath group and the no sitz bath group (p=0.04). The group that did not undergo warm water sitz bath treatment showed a 1.13-fold increased risk of rehospitalization within 1 month after TURP due to postoperative complications compared with the warm water sitz bath group (odds ratio [OR]=1.134; 95% confidence interval [CI], 1.022 to 1.193; p=0.06).
Conclusions
Warm water sitz bath treatment reduced postoperative complications such as urethral stricture. These results suggest that large-scale prospective studies are needed to establish an ideal method and optimal duration of sitz baths.
Keywords: Complications, Hydrotherapy, Transurethral resection of prostate, Urethral stricture
INTRODUCTION
Although medical therapy such as alpha-adrenergic blockers and 5-alpha reductase inhibitors has proven valuable in the treatment of patients with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH), transurethral resection of the prostate (TURP) has served as the gold standard surgical modality for BPH for several decades [1]. However, this procedure can cause complications, including bleeding, hyponatremia, urethral stricture, incontinence, retrograde ejaculation, and bladder neck contracture [2,3]. Furthermore, the incidence of postoperative bleeding complications necessitating blood transfusion has been reported to be as high as 6.4% in the general population [4].
The warm water sitz bath is well known as a safe and low morbidity method of treatment for anorectal and gynecologic conditions [5,6]. Most physicians, including colon and rectal surgeons, recommend warm sitz baths to relieve pain in the perineal region and to promote wound healing, even though there is no rational explanation for this maneuver [7]. However, to our knowledge, there are no reports about the efficacy of warm water sitz baths in the realm of urology. Some urologists do not recommend the warm water sitz bath after TURP because of the risk of postoperative bleeding, whereas others recommend this method for pain relief and patient comfort. Therefore, we evaluated the efficacy of warm water sitz baths during the post-TURP period.
MATERIALS AND METHODS
We reviewed the records of 1,783 patients who had undergone TURP between January 2001 and September 2009. All patients underwent TURP by 3 urologists who have performed the procedure in at least 100 patients. We excluded 222 patients who had been taking medications such as anticoagulants or antiplatelet agents after TURP. Patients were also excluded if they had confirmed prostate cancer, neurogenic bladder dysfunction history, acute or chronic prostatitis, or prostatic abscess within the previous 3 months before TURP. The subjects were divided into 2 groups depending on whether they performed warm sitz baths after TURP or not.
1. Preoperative evaluation
The preoperative workup included determination of the prostate volume as assessed by digital rectal examination and transrectal ultrasonography (BK Medical, Herlev, Denmark), International Prostate Symptom Score (IPSS), quality of life score, uroflowmetry, serum prostate-specific antigen, complete blood count, and blood chemistry.
2. Operative technique
TURP was performed in a similar manner as for standard resection. The operation field was cleaned with Betadine solution and the urethra lubricated with chlorhexidine jelly. Resection was performed by using a 24 F continuous-flow resectoscope and cutting loop (Richard Wolf GmbH, Knittlingen, Germany). During the operation, surgical jelly was frequently applied to the meatus. The electrosurgical generator was set to 150 W for cutting and 60 W for coagulation. At the end of the operation, a 22 Fr Foley catheter coated with standard latex and polyvinyl chloride was inserted and mildly traced for hemostasis until the urine became clear. The postoperative catheterization time was recorded.
3. Follow-up
One urologist recommended warm water sitz baths and the others did not. In the warm water sitz bath group, patients were instructed to sit in a tub containing lukewarm water for 10 minutes each time. Patients were advised to perform the procedure for at least 5 days immediately after the removal of the Foley urethral catheter. All patients were discharged on the day when the Foley catheter was removed, and the patients in the sitz bath group were instructed to practice the sitz bath immediately after being discharged. Postoperative complications such as hemorrhage, urinary tract infection, urethral stricture, and acute urinary retention were regarded as an incidence of readmission within 1 month after TURP.
4. Statistical analysis
Significance of differences in age, prostate volume, IPSS, operative time, and resection volume among urologists were examined by using ANOVA. The chi-square test was used to determine the significance of differences in post-TURP complications between the 2 groups. Multiple logistic regression analysis was used for the independent risk factors of rehospitalization due to post-TURP complications. Values of p<0.05 were considered significant.
RESULTS
Among 1,561 patients, 359 performed warm water sitz baths after TURP. The mean patient age was 68.1 years (range, 43-97 years). The mean prostate volume was 47.1 cc, operative time was 43.9 minutes, and resection volume was 20.3 cc. There were no significant differences in preoperative or perioperative findings among the urologists (data not shown).
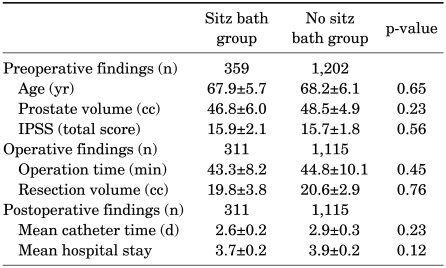
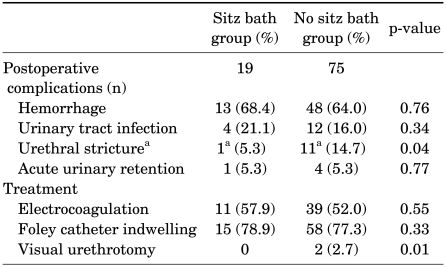
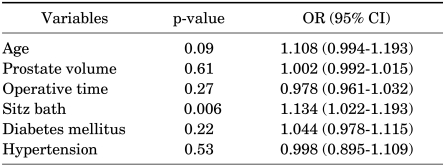
Table 1 shows the comparison of preoperative, operative, and postoperative variables by group. There were no significant differences in the preoperative, operative, or postoperative variables between the sitz bath and no sitz bath groups. Of the 359 men who performed warm water sitz baths, 19 patients (5.3%) were readmitted within 1 month owing to post-TURP complications, whereas 75 patients (6.2%) in the no warm water sitz bath group were readmitted. Of the cases of postoperative complications, urethral stricture developed in 0.28% (1/359) in the sitz bath group and 0.92% (11/1,202) in the no sitz bath group (p=0.04) (Table 2). The odds ratios (ORs) of rehospitalization due to post-TURP complications are summarized in Table 3. There were no significant risk factors for rehospitalization due to post-TURP complications. However, although not statistically significant, the risk of rehospitalization within 1 month after TURP owing to postoperative complications was 1.13-fold higher in the no warm water sitz bath group than in the warm water sitz bath group (p=0.12, OR=1.134, 95% confidence interval [CI] 0.925 to 2.512).
TABLE 1.
Comparison of preoperative, operative, and postoperative variables by group
The values for age, prostate volume, IPSS, operation time, resection volume, mean catheter time, and mean hospital stay are Means±SD. IPSS: International Prostate Symptom Score
TABLE 2.
Postoperative complications and management within 1 month after TURP
TURP: transurethral resection of the prostate, a: p<0.05 by Fisher's exact test
TABLE 3.
Odds ratio of rehospitalization due to post-TURP complications
TURP: transurethral resection of the prostate, OR: odds ratio, CI: confidence interval
In the warm water sitz bath group, 122 patients performed the procedure for 5 days or less after being discharged from the hospital, whereas 237 patients performed the procedure for more than 5 days. However, there were no significant differences in the complication rate according to duration of warm water sitz bath treatment.
DISCUSSION
Warm water sitz baths are frequently recommended after anorectal operations, even though no scientific evidence is available to indicate that sitz baths can promote faster healing or offer reductions in postoperative symptoms [5,8]. The exact physiology of the benefits of warm sitz baths is as yet unknown, although a plausible hypothesis was proposed by Spitzbart and Scharner [9]. He observed that the incidence of spontaneous micturition increased in patients with urinary retention after hemorrhoidectomy while performing warm sitz baths, even though there were no significant changes in the vesical pressure or electromyogram (EMG) activity of the external urethral sphincter with water baths. He proposed that the micturition on sitting in a warm water bath might be initiated by reflex internal urethral sphincter relaxation. The thermosphincteric reflex elicited by a warm sitz bath may lead to relaxation of the internal urethral sphincter, thereby causing vesical contraction and micturition [9]. Furthermore, other perceived benefits include improved anal hygiene and symptomatic relief for some patients [10]. However, there is also a report that contradicts the benefit of sitz baths [11]. That study concluded that sitz baths did not show effects such as pain relief, wound healing, or reduction in consumption of analgesics, and thus that there is no evidence for prescribing sitz baths in the posthemorrhoidectomy period. Even though there are inconsistent findings regarding the benefits of sitz baths, we found a trend toward a lower incidence rate of rehospitalization after TURP in the warm water sitz bath group. Future prospective studies are needed to support the use of sitz baths in the post-TURP period. As far as we know, this is the first study to determine the efficacy of warm water sitz baths in patients who have undergone TURP.
Despite the improvements not only in surgical instruments but also in surgical technique, the rate of morbidity was as high as 30%, including bleeding, infection, urinary retention, incontinence, urethral stricture, and bladder neck stenosis [12,13]. Of these complications, urethral stricture after TURP results from infection, mechanical trauma, ischemic urethral mucosa, prolonged indwelling catheter time, use of local anesthesia, and electrical injury [14,15]. In our study, we observed that the incidence of urethral stricture after TURP was lower in the warm water sitz bath group than in the no sitz bath group. Oladokun et al reported, although not a study of TURP, that sitz baths after episiotomy promoted postoperative wound healing [16]. The mechanism of the process is not yet clear. Park et al observed that maintaining the temperature of the urethra with warm irrigation solution during combined transurethral resection and vaporization of the prostate decreased the incidence of urethral stricture compared with the room temperature irrigation solution group [17]. They observed that a lower temperature might be another cause of urethral stricture after TURP. The mechanical damage in the urethral mucosa leads to leakage of urine, resulting in inflammation and scar formation. In the case of our study, the procedure and sitz bath were not done simultaneously but at different times, but the study by Oladokun et al suggests that the wound healing effect of sitz baths takes place by keeping the temperature warm and promoting vasodilation, which leads to improved circulation [16]. From this point of view, postoperative care with warm water sitz baths might have the benefit of preventing inflammation and scar formation. Future prospective controlled trials are needed to elucidate the underlying mechanism explaining how warm water sitz baths lower the incidence of urethral stricture.
The present study had some limitations. Because our study had a retrospective design, there were no data on monitoring or objective assessment of symptoms and outcomes of warm sitz baths. Another limitation of our study was that we depended on the patients' self-report of whether they practiced warm sitz baths or not. Even though proper instructions for performing warm sitz baths were given to the patients, we cannot be sure what the temperature of the water or duration of the procedure was. An ideal method for sitz baths and an optimal duration need to be elucidated. Also, the fact that the data were collected from 3 surgeons may be another limiting factor. Surgeons who recommend sitz baths and surgeons who do not may have different surgical techniques, which may lead to different postoperative complication rates.
CONCLUSIONS
Warm sitz baths reduced postoperative complications such as urethral stricture in our study. These results suggest that large-scale prospective studies are needed to establish more current and reasonable guidelines for care during the post-TURP period.
Footnotes
The authors have nothing to disclose.
References
- 1.Souverein PC, Erkens JA, de la Rosette JJ, Leufkens HG, Herings RM. Drug treatment of benign prostatic hyperplasia and hospital admission for BPH-related surgery. Eur Urol. 2003;43:528–534. doi: 10.1016/s0302-2838(03)00089-7. [DOI] [PubMed] [Google Scholar]
- 2.Hammadeh MY, Madaan S, Hines J, Philp T. 5-year outcome of a prospective randomized trial to compare transurethral electrovaporization of the prostate and standard transurethral resection. Urology. 2003;61:1166–1171. doi: 10.1016/s0090-4295(03)00109-2. [DOI] [PubMed] [Google Scholar]
- 3.Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007;94:1201–1208. doi: 10.1002/bjs.5916. [DOI] [PubMed] [Google Scholar]
- 4.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243–247. doi: 10.1016/s0022-5347(17)40731-2. [DOI] [PubMed] [Google Scholar]
- 5.Janicke DM, Pundt MR. Anorectal disorders. Emerg Med Clin North Am. 1996;14:757–788. doi: 10.1016/s0733-8627(05)70278-9. [DOI] [PubMed] [Google Scholar]
- 6.Friend WD. Hot sitz baths. Med J Aust. 1995;162:448. doi: 10.5694/j.1326-5377.1995.tb139999.x. [DOI] [PubMed] [Google Scholar]
- 7.McConnell EA. Giving your patient a sitz bath. Nursing. 1993;23:14. doi: 10.1097/00152193-199312000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein D, Halevy A, Negri M, Levy N, Gelertner I, Ziv Y. A prospective, randomized double-blind study on the treatment of anal fissures with Nitroglycerin ointment. Harefuah. 2004;143:713–717. 767, 766. [PubMed] [Google Scholar]
- 9.Spitzbart H, Scharner W. The importance of the ascendent sitz bath in gynecology. Zentralbl Gynakol. 1970;92:1248–1252. [PubMed] [Google Scholar]
- 10.Gupta PJ. Warm sitz bath does not reduce symptoms in posthaemorrhoidectomy period: a randomized, controlled study. ANZ J Surg. 2008;78:398–401. doi: 10.1111/j.1445-2197.2008.04485.x. [DOI] [PubMed] [Google Scholar]
- 11.Shafik A. Role of warm water bath in inducing micturition in postoperative urinary retention after anorectal operations. Urol Int. 1993;50:213–217. doi: 10.1159/000282487. [DOI] [PubMed] [Google Scholar]
- 12.Jaffe JS, McCullough TC, Harkaway RC, Ginsberg PC. Effects of irrigation fluid temperature on core body temperature during transurethral resection of the prostate. Urology. 2001;57:1078–1081. doi: 10.1016/s0090-4295(01)00993-1. [DOI] [PubMed] [Google Scholar]
- 13.Hanania NA, Zimmerman JL. Accidental hypothermia. Crit Care Clin. 1999;15:235–249. doi: 10.1016/s0749-0704(05)70052-x. [DOI] [PubMed] [Google Scholar]
- 14.Balbay MD, Ergen A, Sahin A, Lekili M, Ulucay S, Karaagaoglu E. Development of urethral stricture after transurethral prostatectomy: a retrospective study. Int Urol Nephrol. 1992;24:49–53. doi: 10.1007/BF02552117. [DOI] [PubMed] [Google Scholar]
- 15.Pansadoro V, Emiliozzi P, Defidio L, Scarpone P, Tati G. Urethral stricture following transurethral resection of the prostate. The role of local anaesthetics. Br J Urol. 1993;72:930–932. doi: 10.1111/j.1464-410x.1993.tb16300.x. [DOI] [PubMed] [Google Scholar]
- 16.Oladokun A, Babarinsa IA, Adewole IF, Omigbodun AO, Ojengbede OA. A sitz bath does not improve wound healing after elective episiotomy. J Obstet Gynaecol. 2000;20:277–279. doi: 10.1080/01443610050009601. [DOI] [PubMed] [Google Scholar]
- 17.Park JK, Lee SK, Han SH, Kim SD, Choi KS, Kim MK. Is warm temperature necessary to prevent urethral stricture in combined transurethral resection and vaporization of prostate? Urology. 2009;74:125–129. doi: 10.1016/j.urology.2008.12.057. [DOI] [PubMed] [Google Scholar]