Abstract
Purpose
We examined patient satisfaction with treatment outcomes after shock wave lithotripsy (SWL) and ureteroscopic removal of stone (URS) for proximal ureteral stones.
Materials and Methods
We evaluated 224 consecutive patients who underwent SWL (n=156) or URS (n=68) for a single radiopaque proximal ureteral stone. Stone-free rates, defined as no visible fragment on a plain X-ray; complications; and patient satisfaction were compared. Patient satisfaction was examined through a specifically tailored questionnaire that included overall satisfaction (5 scales) and 4 domains (pain, voiding symptoms, cost, and stone-free status).
Results
The stone-free rates after the first, second, and third sessions of SWL were 36.5%, 65.4%, and 84.6%, respectively. The overall stone-free rate of URS was 82.4%, which was comparable to that of the third session of SWL. Complications were similar between the two groups except for greater steinstrasse in the SWL group. Overall satisfaction and voiding symptoms, cost, and stone-free status showed no significant difference between the groups. In the pain domain, the SWL group had a relatively lower satisfaction rate than did the URS group (p=0.05). Subanalysis showed that the satisfaction rate of the URS group with stone-free status was significantly lower than that of the SWL group in patients with ≥10 mm stones (p=0.032).
Conclusions
Overall treatment outcomes and patient satisfaction were not significantly different between SWL and URS. However, patients undergoing URS for ≥10 mm proximal ureteral stones had lesser satisfaction with stone-free status, because of relatively lower stone-free rates due to upward stone migration. We suggest that factors regarding the subjective satisfaction of patients be included in counseling about treatment options for proximal ureteral stones.
Keywords: Lithotripsy, Patient satisfaction, Ureteral calculi, Ureteroscopy
INTRODUCTION
The optimal treatment modality for proximal ureteral stones of various sizes has not yet been defined. The treatment decision for proximal ureteral stones is made depending on stone factors as well as technical and clinical factors such as availability of treatment modality, patient preference, and doctor's attributes [1-4]. Shock wave lithotripsy (SWL) and ureteroscopic removal of stone (URS) are positioned as the initial treatment options for proximal ureteral stones with a low probability of spontaneous passage. Whereas SWL has been used as the first-line treatment in patients with <10 mm proximal ureteral stones, owing to its lower rate of complications and noninvasiveness [2], it has the disadvantage of a higher retreatment rate and longer period until stone clearance. With technical advances in endoscopy and lithotripters, URS has been reported to have a better chance of stone clearance with a single procedure even for proximal ureteral stones >10 mm [1,5,6]. However, URS requires regional or general anesthesia and has relatively higher complication rates than does SWL.
In order to make recommendations on the optimal treatment choice for proximal ureteral stones, many studies to date have analyzed the outcomes of the two treatment modalities from an objective viewpoint such as stone-free rates and complications [1,5-9]. However, few studies have analyzed the subjective satisfaction of the patients in the treatment of proximal ureteral stones. Subjective satisfaction of the patients should be considered as an important factor because it reflects how much of the patients' expectations were met by the specific treatment. In the present study, we examined patient satisfaction with treatment outcomes in patients who were treated with SWL or URS for proximal ureteral stones.
MATERIALS AND METHODS
We retrospectively evaluated 224 consecutive patients who underwent SWL (n=156) or URS (n=68) for a single, primary, radiopaque proximal ureteral stone between January 2004 and July 2009 at our institute. Patients with radiolucent stones and preexisting ureteral stricture were excluded. After the merits, drawbacks, and possible complications of each method were thoroughly explained to the patients, treatment was determined according to patient choice.
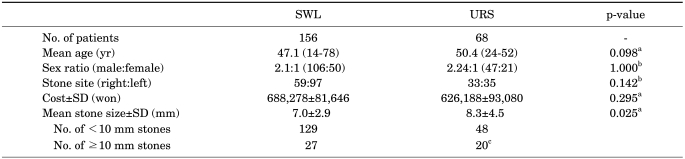
The proximal ureter was defined as the segment between the ureteropelvic junction and the superior margin of the sacroiliac joint. Stone size was determined as the longest diameter in KUB, excretory urography, ultrasonography, or noncontrast computed tomography after magnifying the image 3 to 4 times on a picture archiving communication system at our institute. Patient characteristics are shown in Table 1. The mean stone size was significantly larger in the URS group than in the SWL group. In the URS group, 2 patients had proximal ureteral stones larger than 2 cm.
TABLE 1.
Baseline patient characteristics
SWL: shock wave lithotripsy, URS: ureteroscopic removal of stone, SD: standard deviation, a: independent sample t-test were used, b: chi-square tests were used, c: including 2 patients with ≥2 cm stones
In situ SWL was performed by using the Storz Modulith SLK (Karl Storz, Kreuzlingen, Switzerland) as an outpatient procedure without intravenous sedation or anesthesia. To ensure patient tolerability, voltage and shock wave were set at 12 KV to 13 KV and 3,000 to 3,500 shocks at a time. The patients were evaluated 1 week after the SWL session by KUB to assess stone passage; if residual stones were observed, repeated SWL was performed. In case of no breakage of the stone after 3 sessions, the patients were advised about salvage treatments of additional SWL or URS and were treated according to patient choice.
URS was performed with an 8/9.8 Fr, 12° semirigid ureterorenoscope (Richard Wolf, Knittlingen, Germany) under general (n= 58) or spinal (n=10) anesthesia. Continuous irrigation was used to obtain and sustain a clear operative visual field. For lithotripsy, the Swiss Lithoclast (Electro Medical Systems, Nyon, Switzerland) was used in 56 patients until December 2008; thereafter, a holmium:YAG laser (Coherent Medical Systems, Palo Alto, CA, USA) and a 550 nm quartz laser fiber were used in 12 patients. After stone fragmentation, basket retrieval of stone fragments was done under direct visualization. At the end of surgery, a 6 Fr double-J stent was placed in 62 patients (91%), and the stent was removed under local anesthesia at postoperative 2 weeks. At postoperative 1 month, excretory urography was performed to assess stone-free status and contrast passage disturbance. Stone fragments that had migrated upward during URS were treated with additional SWL or surveillance according to their size.
Treatment outcomes, including stone-free rates and complications, and patient subjective satisfaction were compared between the two groups. Stone-free status was defined as no visible stone fragment on KUB or excretory urography, and complications were examined regarding steinstrasse, ureteral injury, and urinary tract infection. Patient satisfaction was examined through a specifically tailored questionnaire. The questionnaire was filled out by the patients themselves when they visited the clinic or was completed by doctor's telephone interview. All questionnaires were examined at the time of ultimate stone-free status. The questionnaire included overall satisfaction (5 scales: very satisfied, satisfied, acceptable, dissatisfied, very dissatisfied), and satisfaction or dissatisfaction in 4 domains (pain, voiding symptoms, cost, and stone-free status). Four domains were determined after thorough interview of 3 patients in each group, on the basis of the reasons for dissatisfaction with the treatment modality. Subgroup analysis was performed in patients with <10 mm vs. ≥10 mm stones.
For statistical analyses, commercially available SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used. The Fisher's exact test or the chi-square test was used to compare categorical variables between the two groups. The Student's t-test was used to compare continuous variables. All statistical analyses were 2-sided with p<0.05 defined as statistically significant.
RESULTS
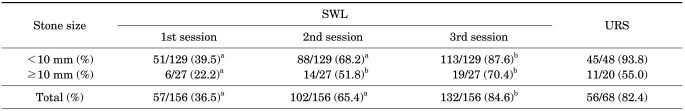
The overall stone-free rates after the first, second, and third sessions of SWL were 36.5%, 65.4%, and 84.6%, respectively (Table 2). The overall stone-free rate of URS was 82.4%, which was significantly higher than that of ≤2 sessions of SWL but was comparable to that of the third session of SWL. In patients with <10 mm stones, the cumulative stone-free rate after the third session of SWL and the stone-free rate of URS were 87.6% and 93.8%, respectively (p=0.288). In patients with ≥10 mm stones, the cumulative stone-free rate after the third session of SWL and the stone-free rate of URS were 70.4% and 55.0%, respectively (p=0.362).
TABLE 2.
Stone-free rates according to treatment method for proximal ureteral stones
SWL: shock wave lithotripsy, URS: ureteroscopic removal of stone, a: p<0.05 between the URS and SWL group, b: p>0.05 between the two groups
Patients who had no breakage of the stone after 3 sessions of SWL mostly chose additional SWL, and ultimately became stone-free after 4 to 9 sessions of SWL, except for 4 patients (2.6%) who were treated with salvage URS. For 12 patients (17.6%) whose fragmented calculi had migrated upward to the kidney during URS, additional SWL was performed in 10 patients because the fragments were considered to be larger than 4 mm. All those fragments were completely removed.
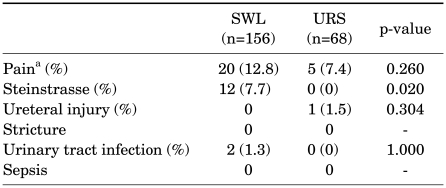
Pain requiring intramuscular injection of nonsteroidal analgesics was more common in the SWL group than in the URS group without statistical significance (12.8% vs. 7.4%). However, steinstrasse was significantly more common after SWL than after URS (7.7% vs. 0%). Other complications, such as ureteral injury, stricture, urinary tract infection, and sepsis, occurred very rarely in both groups (Table 3).
TABLE 3.
Complications according to treatment method
SWL: shock wave lithotripsy, URS: ureteroscopic removal of stone, a: requiring intramuscular injection of nonsteroidal analgesics
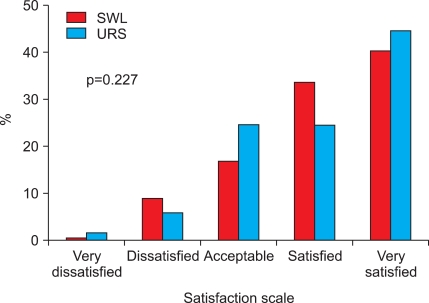
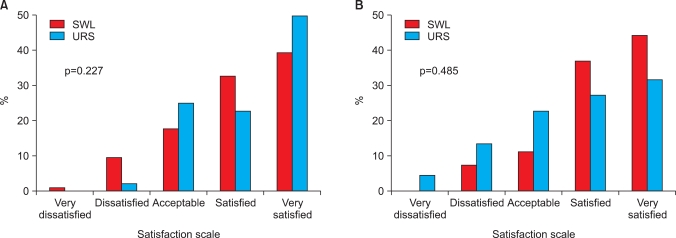
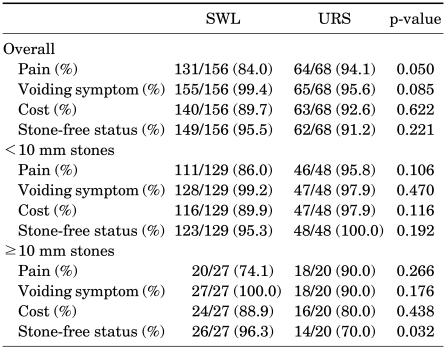
Overall satisfaction was similar between the two groups (Fig. 1). Proportions of 'very satisfied' patients were 40% and 42% of the SWL and URS groups. The overall satisfaction score was also similar between the two groups (Mean±SD, 4.03±0.99 vs. 4.07±1.01; p=0.811). Similarly, subgroup analysis in patients with <10 mm vs. ≥10 mm stones showed comparable overall satisfaction in the two groups (Fig. 2). Mean satisfaction scores±SD in the SWL and URS groups were 4.00±1.01 vs. 4.20±0.89 for <10 mm stones (p=0.205) and 4.18±0.92 vs. 3.75±1.20 for ≥10 mm stones, respectively (p=0.187).
FIG. 1.
Overall satisfaction according to treatment method. SWL: shock wave lithotripsy, URS: ureteroscopic removal of stone.
FIG. 2.
Overall satisfaction in patients with <10 mm (A) and ≥10 mm proximal ureteral stones (B). SWL: shock wave lithotripsy, URS: ureteroscopic removal of stone.
Comparison of satisfaction in the 4 domains is shown in Table 4. The SWL group had a lower satisfaction rate in the pain domain than did the URS group, without reaching statistical significance (84.0% vs. 94.1%, p=0.050). A trend was observed for a slightly lower satisfaction rate in the voiding symptom domain for the URS group, but it was not statistically significant. In the cost domain, the two groups showed similar satisfaction rates. Subgroup analysis based on stone size showed that satisfaction rates in the 4 domains for <10 mm stones were similar between the groups, whereas the satisfaction rate for stone-free status of the URS group was significantly lower than that of the SWL group in patients with ≥10 mm stones (70.0% vs. 96.3%, p=0.032).
TABLE 4.
Satisfaction rates in four domains according to treatment method
SWL: shock wave lithotripsy, URS: ureteroscopic removal of stone
DISCUSSION
Both SWL and URS are acceptable first-line treatments for ureteral stones including proximal ureteral stones [3]. Besides objective outcomes such as stone-free rates and complications, patient perception of the specific treatment modality is another important consideration in determining the treatment method for proximal ureteral stones. However, patient perception has not been assessed as much as objective outcomes. In the current study, we examined subjective patient satisfaction with objective outcomes in patients undergoing SWL or URS for proximal ureteral stones.
We found that the stone-free rates of URS and the cumulative stone-free rates of 3 sessions of SWL were comparable between the two groups (82.4% vs. 84.6%). In our study, the overall stone-free rate of URS was comparable to other studies with stone-free rates ranging from 75% to 93% [5-7,10], whereas the stone-free rate after initial SWL (37%) was relatively lower than in other studies with stone-free rates ranging from 50% to 86% [5-7,10-12]. We suggest that this finding is mainly attributable to different SWL follow-up protocols. Most prior studies evaluated the stone-free rates of initial SWL at 1 month or 3 months after treatment [5-7,11,12], whereas we evaluated patients at 1 week after initial SWL and performed additional SWL in cases of residual stones.
Notably, whereas the stone-free rates (93.8%) of URS for <10 mm proximal ureteral stones was similar to other series with stone-free rates from 90% to 100% [5,7,13], the stone-free rates in ≥10 mm proximal ureteral stones (55%) was much lower than in those recent series using holmium:YAG laser lithotripsy, for which stone-free rates ranged from 76.8% to 93% [5-7]. The lower stone-free rates in our patients undergoing URS for ≥10 mm proximal ureteral stones may be attributable to the following reasons. First, most (82%) of our patients undergoing URS were treated with a pneumatic lithotripter, which is associated with an upward migration rate ranging from 5.5% to 33% [14-17]. Knispel et al reported that only 51% of patients undergoing URS with the Swiss Lithoclast were stone-free immediately after URS because of frequent fragment migration [14]. Lee et al also reported that only 35% of patients undergoing URS using a lithoclast or ultrasound lithotripter for large proximal ureteral stones ≥15 mm were stone-free after one session of URS [16]. Second, we did not use any instruments during the study period, such as the N-trap, to prevent the fragmented fragments from migrating into the kidney.
Both the SWL and URS groups in this study had low overall complication rates, consistent with other reports [3,13]. The two groups were similar in complication rates except for greater steinstrasse in the SWL group. We believe that both treatment modalities can be performed without major complications in most proximal ureteral stones.
In the present study, we examined overall patient satisfaction and also 4 domains of patient satisfaction. Whereas overall patient satisfaction was comparable (Fig. 1), satisfaction rates in the 4 domains differed somewhat between the two groups (Table 4). In the pain domain, the SWL group had a relatively lower satisfaction rate. The reason for this finding may be attributable to the following reasons. First, SWL was performed without sedation or anesthesia and thus the procedure itself caused more pain. Second, despite the lesser invasiveness of SWL, it entails a relatively longer period until stone-free status is reached, consequently resulting in lesser satisfaction in the pain domain. The slightly lower satisfaction rate in the voiding symptom domain of the URS group seems to have been due to irritation symptoms related to the double-J stent. Although most prior studies have found URS to be more cost-effective than SWL in ureteral stones [6,7,18], our results showed similar satisfaction in the cost domain between the URS and SWL groups. Similarly, overall satisfaction with stone-free status was comparable between the two groups. Overall, 94.1% and 90.4% of the URS and SWL groups scored satisfaction with their treatment method as ≥ 3 points (acceptable), which suggests that both methods are good treatment options for proximal ureteral stones (Fig. 1).
In the subgroup analysis based on stone size, satisfaction rates in the 4 domains for <10 mm stones showed a pattern similar to that of the entire patient population (Table 4). However, patients undergoing URS for ≥10 mm proximal ureteral stones had significantly lesser satisfaction with stone-free status. In addition, a trend toward lesser satisfaction in the cost domain in this URS subgroup was observed. As expected, lower satisfaction with stone-free status in this subgroup of patients undergoing URS was mainly attributable to lower stone-free rates. In our study, although it did not reach statistical significance, the overall satisfaction score in the URS group with ≥10 mm proximal ureteral stones was slightly lower than that of the SWL group (4.18±0.92 vs. 3.75±1.20). These findings also may be due to lesser satisfaction with stone-free status in this subgroup. Our results for patient satisfaction in the subgroups with ≥10 mm proximal ureteral stones indicate that despite preoperative explanation of possible upward migration of stone fragments during URS with large stones, expectation of stone-free status may be greater in patients undergoing surgery than in those undergoing SWL. In addition, unless the possible necessity of ancillary procedures after URS for large proximal ureteral stones is explained, patient satisfaction may be much lower despite rapid symptomatic relief, compared with that of patients undergoing SWL. In this context, surgeons should be aware of high patient expectations for treatment success and reluctant patient attitudes toward ancillary treatment after surgery.
We acknowledge that our results have possible biases. Most importantly, we did not use validated questionnaires. To date, several validated questionnaires are being used to assess general quality of life (QoL) (such as SF-36 and EuroQol) and stent-related QoL (such as the ureteral stent symptom questionnaire [19]). However, so far, there is no validated questionnaire for measuring subjective satisfaction specific to proximal ureteral stones. We assessed patient perception with our specifically tailored questionnaire because several validated questionnaires for general QoL are not enough to discriminate satisfaction in patients undergoing URS or SWL for proximal ureteral stones. In addition, because our study was retrospective, we examined patient satisfaction at the time of ultimate stone-free status. The time of examining the questionnaire may affect the results regarding patient satisfaction. Nevertheless, we believe that our results analyzing patient perception as well as objective treatment outcomes highlight the importance of subjective patient satisfaction as one of the considerations in determining the treatment method for proximal ureteral stones. Besides analyzing objective outcomes, further study focusing on patient QoL and satisfaction with the use of an appropriate, validated questionnaire is warranted to determine the optimal treatment method for proximal ureteral stones.
CONCLUSIONS
Overall treatment outcomes and patient satisfaction were not significantly different between SWL and URS, whereas significant proportions of patients undergoing URS for ≥10 mm proximal ureteral stones had residual fragments due to upward stone migration. Despite rapid symptomatic relief, patients who underwent URS for ≥10 mm proximal ureteral stones seemed to have less satisfaction with stone-free status because of relatively lower stone-free rates compared with SWL. We suggest that factors regarding subjective satisfaction of the patients should be included when counseling patients on treatment options for proximal ureteral stones.
Footnotes
The authors have nothing to disclose.
References
- 1.Kijvikai K, Haleblian GE, Preminger GM, de la Rosette J. Shock wave lithotripsy or ureteroscopy for the management of proximal ureteral calculi: an old discussion revisited. J Urol. 2007;178:1157–1163. doi: 10.1016/j.juro.2007.05.132. [DOI] [PubMed] [Google Scholar]
- 2.Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. The American Urological Association. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997;158:1915–1921. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 3.Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 4.Matlaga BR. Contemporary surgical management of upper urinary tract calculi. J Urol. 2009;181:2152–2156. doi: 10.1016/j.juro.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Lam JS, Greene TD, Gupta M. Treatment of proximal ureteral calculi: holmium:YAG laser ureterolithotripsy versus extracorporeal shock wave lithotripsy. J Urol. 2002;167:1972–1976. [PubMed] [Google Scholar]
- 6.Wu CF, Shee JJ, Lin WY, Lin CL, Chen CS. Comparison between extracorporeal shock wave lithotripsy and semirigid ureterorenoscope with holmium:YAG laser lithotripsy for treating large proximal ureteral stones. J Urol. 2004;172:1899–1902. doi: 10.1097/01.ju.0000142848.43880.b3. [DOI] [PubMed] [Google Scholar]
- 7.Wu CF, Chen CS, Lin WY, Shee JJ, Lin CL, Chen Y, et al. Therapeutic options for proximal ureter stone: extracorporeal shock wave lithotripsy versus semirigid ureterorenoscope with holmium:yttrium-aluminum-garnet laser lithotripsy. Urology. 2005;65:1075–1079. doi: 10.1016/j.urology.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Kim SS, Sung BM, Ahn SH. Comparison of shock wave lithotripsy (SWL) and rigid ureteroscopic stone removal (URS) for treatment of upper ureteral stones. Korean J Urol. 2004;45:444–448. [Google Scholar]
- 9.Park CM, Ryu SH, Jeon SS, Chai SE. Comparison of extracorporeal shock wave lithotripsy (ESWL) and ureteroscopic lithotripsy (URS) for treatment of upper ureteral calculi. Korean J Urol. 2001;42:379–383. [Google Scholar]
- 10.Park H, Park M, Park T. Two-year experience with ureteral stones: extracorporeal shockwave lithotripsy v ureteroscopic manipulation. J Endourol. 1998;12:501–504. doi: 10.1089/end.1998.12.501. [DOI] [PubMed] [Google Scholar]
- 11.Pace KT, Weir MJ, Tariq N, Honey RJ. Low success rate of repeat shock wave lithotripsy for ureteral stones after failed initial treatment. J Urol. 2000;164:1905–1907. [PubMed] [Google Scholar]
- 12.Nabi G, Baldo O, Cartledge J, Cross W, Joyce AD, Lloyd SN. The impact of the Dornier Compact Delta lithotriptor on the management of primary ureteric calculi. Eur Urol. 2003;44:482–486. doi: 10.1016/s0302-2838(03)00312-9. [DOI] [PubMed] [Google Scholar]
- 13.Parker BD, Frederick RW, Reilly TP, Lowry PS, Bird ET. Efficiency and cost of treating proximal ureteral stones: shock wave lithotripsy versus ureteroscopy plus holmium:yttrium-aluminum-garnet laser. Urology. 2004;64:1102–1106. doi: 10.1016/j.urology.2004.07.040. [DOI] [PubMed] [Google Scholar]
- 14.Knispel HH, Klän R, Heicappell R, Miller K. Pneumatic lithotripsy applied through deflected working channel of miniureteroscope: results in 143 patients. J Endourol. 1998;12:513–515. doi: 10.1089/end.1998.12.513. [DOI] [PubMed] [Google Scholar]
- 15.Aridogan IA, Zeren S, Bayazit Y, Soyupak B, Doran S. Complications of pneumatic ureterolithotripsy in the early postoperative period. J Endourol. 2005;19:50–53. doi: 10.1089/end.2005.19.50. [DOI] [PubMed] [Google Scholar]
- 16.Lee YH, Tsai JY, Jiaan BP, Wu T, Yu CC. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopic lithotripsy for management of large upper third ureteral stones. Urology. 2006;67:480–484. doi: 10.1016/j.urology.2005.09.067. [DOI] [PubMed] [Google Scholar]
- 17.Aghamir SK, Mohseni MG, Ardestani A. Treatment of ureteral calculi with ballistic lithotripsy. J Endourol. 2003;17:887–890. doi: 10.1089/089277903772036208. [DOI] [PubMed] [Google Scholar]
- 18.Wolf JS, Jr, Carroll PR, Stoller ML. Cost-effectiveness v patient preference in the choice of treatment for distal ureteral calculi: a literature-based decision analysis. J Endourol. 1995;9:243–248. doi: 10.1089/end.1995.9.243. [DOI] [PubMed] [Google Scholar]
- 19.Joshi HB, Newns N, Stainthorpe A, MacDonagh RP, Keeley FX, Jr, Timoney AG. Ureteral stent symptom questionnaire: development and validation of a multidimensional quality of life measure. J Urol. 2003;169:1060–1064. doi: 10.1097/01.ju.0000049198.53424.1d. [DOI] [PubMed] [Google Scholar]