Abstract
The validity of the abuse/dependence distinction within alcohol use disorders (AUDs) has been increasingly questioned on psychometric and conceptual grounds. Two types of findings are often cited as support for the validity of this distinction: (1) dependence is more persistent than abuse, and (2) dependence is more highly comorbid with other Axis I and Axis II disorders than is abuse. Using data from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC), we examined the extent to which the current diagnostic algorithm (three of seven dependence criteria for a diagnosis of dependence; one of four abuse criteria for a diagnosis of abuse if dependence criteria are not met) produces this pattern of findings independent of item set. Analyses where all 330 permutations of the 11 AUD criteria were partitioned into a four-item “abuse” set and a seven-item “dependence” set were conducted to examine the relevance of the criteria sets to estimates of persistence and chronicity independent of criteria. Regardless of the criteria employed, the “dependence set” (i.e., 3/7 criteria) always and substantially outperformed the “abuse set” (1/4) with respect to both persistence and comorbidity. These data indicate that chronicity and comorbidity are flawed indicators for the abuse/dependence distinction (and likely other conditions where hierarchical decision rules are employed). In addition, our analyses show that the current set of criteria defining alcohol dependence and abuse are not optimal.
Keywords: alcohol use disorders, alcohol abuse, alcohol dependence, diagnostic algorithms
The Diagnostic and Statistical Manual of Mental Disorders, versions III, III-R, and IV (DSM-III, DSM-III-R, and DSM-IV; American Psychiatric Association, 1980, 1987, 1994) define two categories of alcohol use disorders, alcohol abuse and alcohol dependence. Both diagnostic categories are defined by a set of distinctive symptoms and a different scoring algorithm. The algorithm for dependence requires that an individual has at least three of the seven symptoms of dependence1 in order to have the diagnosis. In contrast, the diagnosis of abuse requires only one of the four symptoms of abuse2 and does not meet the aforementioned dependence criteria, currently or during lifetime. Although the construct of dependence has well established conceptual and empirical foundations, the construct of abuse has been extensively criticized due to its lack of theoretical underpinnings (Martin, Chung & Langenbucher, 2008) and psychometric validity (Grant et al., 2007; Hasin, Hatzenbuehler, Keyes & Ogburn, 2006).
Within DSM-IV there is a hierarchical decision rule such that a diagnosis of dependence supersedes a diagnosis of abuse, suggesting that abuse is less severe and/or a precursor of dependence (Martin et al., 2008). However, unlike the distinction proposed by Edwards and Gross (1976) between alcohol-related disabilities (i.e., consequences) and the alcohol dependence syndrome, there is no clear conceptual relation between abuse and dependence. (In Edwards and Gross’ model, alcohol-related disabilities were correlated dimensions of pathological alcohol use.)
Beyond the conceptual issue of the relation between abuse and dependence are psychometric problems noted by multiple researchers. For example, reliability of abuse diagnoses tends to be significantly lower than that of dependence diagnoses (Hasin et. al, 2006). More significantly, IRT analyses arraying the four abuse and seven dependence criteria along a single latent trait indicate that abuse criteria are not invariably “less severe” than dependence criteria and, in fact, some dependence criteria (e.g., drinking in larger amounts and for longer than intended) are the least severe psychometrically (lowest thresholds) while some abuse criteria (e.g., role interference or legal troubles) are among the most severe (Saha, Chou & Grant, 2006; Saha, Stinson & Grant, 2007). These criticisms have led to the idea that DSM-V should consider the possibility of merging the two criteria sets of dependence and abuse into a one broad category (Gelhorn et al., 2008).
However, there still are some arguments in favor of the distinction between the two disorders. These include the fact that abuse shows a differential association with external criteria, when compared with dependence and the absence of diagnosis (Schuckit & Smith, 2001). However, support for the predictive validity of this distinction is equivocal (Hasin et al., 2006; Martin et al., 2008). Another strong argument is provided by longitudinal studies showing that the course of abuse is different than the course of dependence, suggesting that both disorders are distinctive (Grant, Stinson & Harford, 2001; Hasin, Grant & Endicott, 1990; Schuckit et al., 2001.)
Differential Course of Abuse and Dependence
Hasin et al. (1990) were the first to report differences in course in a prospective, four-year study of male drinkers in the community. These authors found that participants diagnosed with abuse, as defined by the DSM-III-R, were more likely to remit after 4 years than to become dependent, whereas people diagnosed as dependent were more likely to present a chronic course (although 54% of the latter presented abuse or remission at follow-up). Hasin, Van Rossem, McCloud and Endicott (1997) replicated these results in a prospective, one-year study of men and women in the community, using DSM-IV diagnoses. Among participants who met criteria for abuse at baseline, 33% remained in that category one year later, whereas 61% remitted. Among participants diagnosed with dependence, 67% persisted whereas the majority of the non persistent subjects were in full-remission at follow-up, with only 4% meeting criteria for abuse (although according to DSM-IV they would be diagnosed as dependent in partial remission).
More recently, Schuckit, Smith and Landi (2000) presented results of a 5-year follow-up of 435 educated men, half of whom had a family history of alcoholism. At follow-up, 68% of those with a diagnosis of DSM-IV alcohol dependence at baseline remained dependent. In contrast, among participants diagnosed with alcohol abuse at baseline, 36% had the same diagnosis five years later and 11% developed dependence. Using data from the Collaborative Study on the Genetics of Alcoholism (COGA), Schuckit et al. (2001) found that 68% of adult participants (mean age of 42.9 years) diagnosed with alcohol dependence at base line, remained dependent five years later (i.e., had one or more symptoms of dependence or abuse, as defined in DSM-IV for continuing alcohol dependence). However, when including only participants that still had three of the seven criteria for dependence, this percentage dropped to 37%.3 In the case of abuse, the proportion of people at follow-up having at least one symptom of abuse or dependence, and of people meeting criteria for abuse was lower (55% and 36%, respectively). This pattern of results with abuse was replicated in a sample of adolescents (mean age of 16.5 years) from the same study (Schuckit et al., 2008).
In a nationally representative study (the National Longitudinal Survey of Labor Market Experience in Youth; NLSY), Grant et al. (2001) also found differences in the course of dependence and abuse. Although for dependent subjects the percentages of people diagnosed with dependence or abuse at follow-up were similar (26% in both categories), in the case of abuse 28% remained in the same category at follow-up and only 8% became dependent, suggesting that abuse and dependence present different and independent trajectories and that abuse is not just a phase in the development of dependence.
These results have been systematically interpreted in the literature as evidence supporting the distinction between alcohol dependence and alcohol abuse (Grant et al., 2001; Hasin, 2003; Hasin et al., 2003). However, none of these studies has tested if differences in course are related to some aspect of the categories (i.e., the content of their items) beyond the difference in severity that they show at onset (Martin et al., 2008). Moreover, to our knowledge, the possibility that differences in stability between alcohol dependence and alcohol abuse is due to an artifact of the algorithms used to define those disorders has never been suggested nor investigated.
Differential Comorbidity
A related argument proposed in favor of the distinction between the diagnoses of alcohol dependence and abuse is the differential association between those disorders and external criteria (e.g., Hasin & Paykin, 1999). A special case of these attempts of validation is provided by studies showing differences in the association between the two alcohol use disorders and other psychiatric disorders.
In an analysis of data from the National Comorbidity Survey (NCS), Kessler et al. (1997) found that the lifetime co-occurrence of alcohol dependence (as defined in the DSM-III-R) with other disorders (including anxiety disorders, affective disorders, drug abuse and dependence, conduct disorder, adult antisocial behavior and antisocial personality disorder) tended to be larger than the corresponding association of alcohol abuse with the same disorders, with the exception of a stronger association between drug abuse with alcohol abuse than with alcohol dependence (although the association with drug dependence was larger for alcohol dependence than for alcohol abuse).
Grant and Harford (1995) reported results from the National Longitudinal Alcohol Epidemiologic Survey (NLAES), a nationally representative study which used DSM-IV diagnoses. Their analysis of past year, prior to past year and lifetime co-occurrence of alcohol use disorders and major depression consistently yielded stronger associations for alcohol dependence than for alcohol abuse. Similar results were found by Hasin and Grant (2002), who analyzed a subsample of former drinkers in NLAES in order to determine the association between past alcohol use disorder and current depression. The association was found to be significant for alcohol dependence but not for alcohol abuse, a result that according to the authors suggests that abuse criteria should not be integrated into the dependence diagnosis, because this could result in increasing heterogeneity and subsequent decrease of the associations with other disorders (Hasin & Grant, 2002). Using the same data set, Grant and Pickering (1996) reported estimations of lifetime comorbidity between alcohol use disorders and drug use disorders (including prescription drugs, sedatives, tranquilizers, amphetamine, cannabis, cocaine and hallucinogen). The associations were almost all significant, and in all cases the association between alcohol abuse and drug abuse was smaller than the association between alcohol dependence and drug dependence.
In a cross-national study investigating patterns of comorbidity across different cultures (the International Consortium in Psychiatric Epidemiology, ICPE), Merikangas et al. (1998) found a consistent pattern of association among DSM-III-R alcohol and drug use disorders and other psychiatric disorders (mood disorders, anxiety disorders, conduct disorders and adult antisocial behavior). Their results show a pattern of associations in which increasing levels of severity [i.e., alcohol or drug use, to problems with alcohol (abuse), to dependence] are related to stronger comorbidity. The fact that these results are the same in the six sites participating in the study (Canada, Germany, Mexico, Netherlands and USA), with the exception of a stronger association of mood disorder with alcohol use than with alcohol problems or dependence in Germany, was interpreted by the authors as evidence of a meaningful continuum of severity that would not be culture-specific.
The most recent report of comorbidity of alcohol use disorders in the general population consists in an analysis of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Hasin, Stinson, Ogburn and Grant (2007) reported past 12 months and lifetime associations of DSM-IV alcohol use disorders and drug use disorder, nicotine dependence, mood disorders, anxiety disorders and personality disorders. The results indicated that current alcohol dependence is significantly associated with drug use disorders, bipolar disorders, and histrionic and antisocial personality disorders, even when the associations were controlled for sociodemographic factors and other comorbidity (when the associations were controlled only for sociodemographic factors, alcohol dependence was significantly associated with all disorders). On the other hand, current alcohol abuse was found to be positively associated only with drug use disorders and negatively associated with schizoid personality disorder (when controlling only for sociodemographic factors, alcohol abuse was associated with drug use disorders and antisocial personality disorder). A similar difference in associations was found when considering lifetime diagnoses.
Is Differential Course and Comorbidity Due to Diagnostic Criteria or Artifacts of the Diagnostic Algorithm?
The accumulated evidence presented thus far seems to be consistent with the idea that alcohol dependence and alcohol abuse are two separate disorders with different levels of severity indicated by the stronger rates of comorbidity associated with dependence when compared to abuse. However, none of the studies has ruled out an alternative explanation for this pattern of results, namely, that the differences in the patterns of association of dependence and abuse with other psychiatric disorders is an artifact of the algorithms defined by the DSM-IV and not a function of the diagnostic criteria specific to each disorder.
The present study was designed to test whether the differential chronicity and comorbodity of alcohol abuse and dependence are attributable to the algorithm used or the specific criteria subjected to the algorithm. It was hypothesized that regardless of the content of criteria employed, diagnoses based on an algorithm of dependence (3 of 7 criteria) would look more “severe” than diagnoses based on an algorithm of abuse (1 of 4 criteria without meeting “dependence”). If the hypothesis is supported, it suggests that, regardless of the intrinsic validity of the constructs of abuse versus dependence, marshalling evidence for the validity of the abuse/dependence distinction on the basis of chronicity or comorbidity is misleading at best and, for all intents and purposes, useless.
Method
Participants
The sample consisted of adults 18 years and older who participated in both waves (2001–2002 and 2004–2005) of the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC; Grant, Moore & Kaplan, 2003; Grant & Kaplan, 2005; Grant et al., 2006), a national, population-based survey of 43,093 adults. Young adults (aged 18–24), Blacks and Hispanics were oversampled by design, and the data set was weighted to account for oversampling and nonresponse. The response rate was 81.0% for Wave 1 and 86.9% for Wave 2 (calculated among those eligible for reinterview). To compare the consistency of AUD diagnosis between Wave 1 and Wave 2, only respondents who participated at both Waves were considered (N = 16,251). In order to be consistent across analyses, the same subsample was used for the analysis of comorbidity.
Assessment of Abuse and Dependence Criteria
Alcohol abuse and dependence were measured through a structured interview, the Alcohol Use Disorders and Associated Disabilities Interview Schedule-IV (AUDADIS-IV; Grant, Dawson & Hasin, 2001). The AUDADIS-IV, designed for lay interviewers, includes multiple items for each abuse and dependence criteria. Several studies have provided support for the reliability of diagnoses based on the AUDADIS-IV (Grant, Harford, Dawson, Chou & Pickering, 1995; Grant, Dawson, et al., 2003).
Assessment of Other Psychopathology
In addition to alcohol abuse and dependence, the AUDADIS-IV provides DSM-IV diagnoses for nicotine dependence and abuse/dependence diagnoses on other 9 substances. Also, other Axis 1 and Axis 2 diagnoses were considered for these analyses, including major depression, dysthymia, bipolar disorder I and II, panic disorder with and without agoraphobia, social phobia, specific phobia, generalized anxiety disorder and all ten personality disorders. For the present analyses, all diagnoses were taken from Wave 1, with the exception of borderline, schizotypal, and narcissistic personality disorders, which were assessed only at Wave 2.
Analysis
Similar analyses were conducted in order to examine the contribution of the scoring algorithm to the estimates of both stability and comorbidity for dependence and abuse. First, the difference in stability or comorbidity between dependence and abuse was estimated using DSM-IV criteria for both disorders4. Then, these estimates were compared with all possible sets of 4 and 7 items taken from the 11 AUD criteria in order to determine if the results found for the DSM-IV diagnoses are significantly different from what would be expected by chance. The analysis of comorbidities involved estimating the association between the AUD diagnoses and 19 other Axis 1 and Axis 2 disorders.
The analysis plan followed a systematic approach that utilizes permutation distributions to determine the "quality" of the current DSM-IV diagnosis structure for abuse and dependence in terms of both persistence and comorbidity. The process begun with creating the permutation distribution for a measure of interest, such as an odds ratio, for all possible permutations of items between the dependence set and the abuse set (i.e., this creates all possible observable values for the measure of interest). The permutation distribution allowed for the determination of whether the current value as computed under the DSM-IV criteria differs significantly from chance or not. Subsequent permutation distributions were created for each of the comorbid diagnoses of interest to determine if the predictive power of the current DSM-IV criteria differs from chance, or not.
Results
Diagnostic Stability of DSM-IV Abuse and Dependence Diagnoses
At Wave 1, participants were classified as meeting criteria for (past 12 month) dependence (meeting three or more of the seven dependence criteria), abuse (meeting one of the four abuse criteria and less than three of the seven dependence criteria), or no diagnosis (neither past 12-month dependence nor abuse). Stability of (past 12 month) DSM-IV diagnoses provides a reference point for exploring algorithmic influences on the properties of abuse and dependence diagnoses.
The overall measure of consistency of diagnosis between the two Waves was assessed with kappa (k = .30; see Table 1). Four additional relations were of interest: (i) the prognostic significance of a Wave 1 dependence diagnosis for a Wave 2 dependence diagnosis; (ii) the prognostic significance of a Wave 1 abuse diagnosis for a Wave 2 abuse diagnosis (iii) the prognostic significance of a Wave 1 dependence diagnosis for a Wave 2 abuse diagnosis, and (iv) the prognostic significance of a Wave 1 abuse diagnosis for a Wave 2 dependence diagnosis. The magnitude of these relationships was assessed using odds ratios with "no diagnosis" as the reference category.
Table 1.
Cross-classification of (12 month) DSM-IV Alcohol Abuse and Alcohol Dependence Criteria at Wave1 vs. Wave 2 (N=16,251)
| Wave 2 | |||
|---|---|---|---|
| Wave 1 | Dependence | Abuse | No Diagnosis |
| Dependence | 311 | 74 | 362 |
| Abuse | 113 | 209 | 630 |
| No Diagnosis | 470 | 559 | 13523 |
Note. The N represents all participants who had complete data on all alcohol abuse and alcohol dependence criteria at both waves.
A baseline diagnosis of dependence was strongly related to a follow-up diagnosis of dependence (OR=24.7; 95% CI = [20.7, 29.5]). Similarly, baseline abuse diagnoses predicted follow-up abuse diagnoses (OR=8.0; 95% CI = [6.7, 9.6]), albeit not as strongly. The odds ratios of transitioning from abuse to dependence (OR=5.2; 95% CI = [4.1, 6.4]) and dependence to abuse (OR = 5.0; 95% CI = [3.8, 6.4]) were nearly identical. These findings are consistent with the broader literature cited earlier and show higher persistence of dependence than abuse and both diagnoses being more strongly associated with itself over time than with the complementary diagnosis. Superficially, such a pattern of findings suggest that dependence is more “chronic” and there is some specificity with respect to stability (i.e., persistence versus cross-diagnosis). What is not clear, however, is whether such findings are attributable to the different item sets for abuse or dependence or the specific algorithm used to derive diagnoses based on symptoms of “abuse” and “dependence.”
Creating Reference Distributions and Evaluating the Extent that Findings of Greater “Severity” Could be Algorithmic Artifacts
The finding that dependence is the more persistent (and thus more severe in a sense) AUD diagnosis is one of the allegedly strongest facts in favor of maintaining an abuse/dependence distinction. One way to evaluate the contribution of the algorithm to this finding, independent of criteria subjected to the algorithm, is to explore the specificity of item sets. That is, by applying abuse/dependence algorithms (i.e., 1 of 4 and 3 of 7 ala DSM-IV) under all possible partitions of the 11 AUD criteria into a four criteria abuse set and a seven criteria dependence set, we can compare findings generated by random distinctions.
With 11 DSM-IV AUD criteria, there are 330 possible sets of four and seven (i.e., eleven "choose" four and eleven "choose" seven are both equal to 330) criteria. One of the 330 solutions corresponds to the current criteria sets, while the other 329 would represent all the other possible combinations of criteria that results in a set of four and a set of seven. If there is something inherent in the current dependence items that contributes to the chronicity of this diagnosis (i.e., the OR for rediagnosing with a dependence diagnosis is large), then random dependence criteria sets (i.e., that include varying numbers of currently considered abuse criteria) should yield lower measures of chronicity. Similarly, if abuse criteria reflect a less severe condition, abuse criteria sets composed of varying numbers of current dependence criteria should produce higher measures of chronicity than the current abuse criteria.
Thus, we divided the AUD criteria into two sets: one for abuse, A = {a1, a2, a3, a4}, and one for dependence, D = {d1, d2, d3, d4, d5, d6, d7}. Based on those alternative sets, each statistic we are interested in (e.g., ORs for persistence or comorbidity) can be tested by comparing the observed computed values to the same statistics obtained under the other 329 alternatives. This results in a basic permutation test (Mielke & Berry, 2007) where the reference distribution allows us to obtain p-values and related statistics based on the assumption of random labeling of a criterion as either corresponding to abuse or dependence.
If the existing architecture for determining dependence and abuse is significantly different than what would be expected from chance, then very few of the random dependence sets should yield measures of persistence greater than the current dependence set, and the resultant p-value should be small (that is, the DSM-IV based estimate should be at or near the top of the distribution of stability). Were it not for the unknown effects of the hierarchical decision rule where dependence supersedes abuse and if we assume that abuse is inherently unstable, very few of the random abuse sets should yield measures of persistence smaller than the current abuse set, and the resultant p-value should be small. Alternatively, if we were to posit that although abuse is less chronic than dependence but, because it reflects underlying pathology, still somewhat stable, we would hypothesize that the DSM-IV criteria set should yield higher stabilities than random abuse sets. Thus, the prediction of the effects of criteria set composition for abuse is less straightforward than it is for dependence but it would seem that optimal sets would either yield the highest or the lowest stabilities (depending upon ones underlying assumptions about the nature of abuse) but not intermediate stabilities.
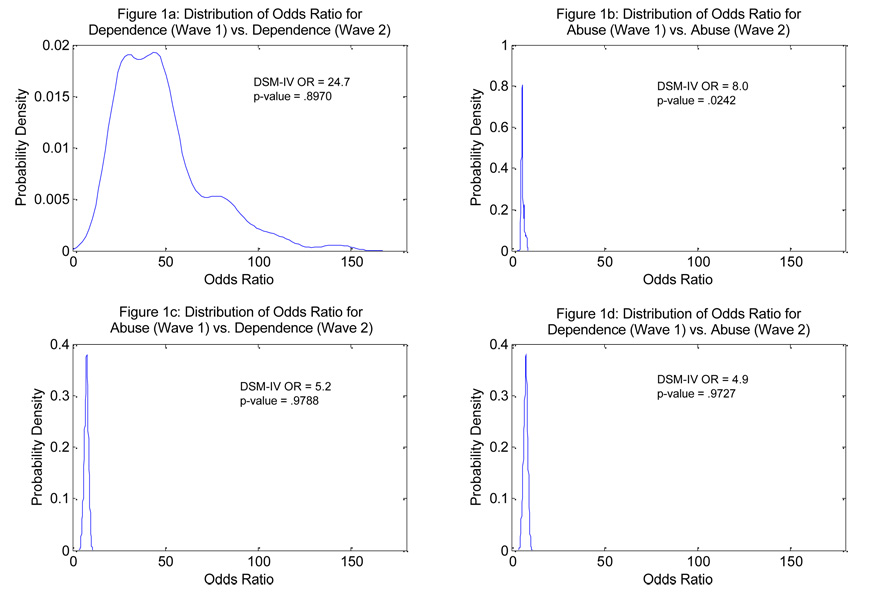
Figure 1 presents the references distributions for the ORs for: (a) Wave 1 dependence predicting Wave 2 dependence (upper left panel) and, (b) a Wave 1 abuse predicting Wave 2 abuse (upper right panel). Before considering these findings further, it is important to highlight the dramatic differences in the distributions of ORs. Specifically, there is no overlap at all in these two reference distributions; the range of observed ORs for rediagnosing with the same diagnosis for dependence is 16.7 to 145.6 (recall, the DSM-IV dependence criteria set yields an OR of 24.7) and the comparable range of the ORs for rediagnosis of abuse is 3.5 to 8.5 (recall, the DSM-IV abuse criteria sets yields an OR of 8). Note that the DSM-IV abuse diagnosis fell in the upper 3% of the reference distribution which is in the opposite direction of what would be predicted if abuse criteria were less severe (and hence less stable) than dependence criteria. (However, as noted above, the possible effects of the hierarchical decision rule rendered that expectation more tentative.) These findings strongly indicate that the finding of greater severity of dependence, operationalized by persistence, can be attributed to algorithmic artifact.
Figure 1.
The four figures represent kernel density plots of the odds ratios obtained from all possible permutation of the item sets.
Furthermore, the distributions in Figure 1 document that the current abuse and dependence criteria do not lead to significantly different results than what we would expect assuming random assignment of criteria to abuse and dependence criteria set. (Although a two-tailed test for abuse persistence would suggest that it is significantly different than chance, a directional hypothesis would have made the opposite prediction.)
Consistent with these conclusions are the results of another set of analyses where we computed kappa coefficients of agreement for Time 1 diagnosis (dependence, abuse, no diagnosis) versus Time 2 diagnosis (dependence, abuse, no diagnosis). Across all 330 permutations kappas ranged from .26 to .33 (kappa using DSM-IV AUD criteria = .30, in the 88th percentile of the referent kappa distribution). These findings indicate that the current choice for abuse and dependence does not lead to a level of consistency that is different than chance assignment.
Comorbidity as a Validating Criterion
In order to examine the consistency of findings across random partitions of the abuse and dependence criteria sets, we conducted a series of analyses analogous to those just described with respect to persistence. Specifically, we estimated the ORs of (past 12 month) abuse and dependence with a range of (past 12 month) Axis I disorders and (lifetime) Axis II disorders. Table 2 shows the results of these analyses. Perhaps of greatest interest is the finding (shown in the rightmost column) of (virtually) no overlap in the distributions of ORs associated with abuse versus those associated with dependence. For each criterion diagnosis, typically 330 out of 330 of the permutations found the OR for dependence to be greater than the OR for abuse. In those few instances where they were less than 100%, they were close to 100% (i.e., greater than 97.8%). These analyses provide convincing demonstration that the greater comorbidity rates associated with dependence, relative to abuse, are likely a function of algorithm.
Table 2.
Comorbidity Expressed as Odds Ratios of DSM-IV Alcohol Use Disorders and Random Criteria Sets with Other Psychiatric Disorders
| Comorbid Dx | AUD Dx | DSM-IV OR |
Mdn OR |
OR Range |
%ile | % D > A |
|---|---|---|---|---|---|---|
| Major Depression | Dependence | 3.9 | 4.4 | 3.4 – 6.8 | 25th | 100 |
| Abuse (w/o D) | 1.1 | 1.6 | 1.1 – 2.7 | 2nd | ||
| Abuse (w or w/out D) | 2.2 | 2.5 | 2.0 – 4.4 | 18th | ||
| Dysthymia | Dependence | 3.1 | 3.4 | 2.6 – 5.6 | 28th | 100 |
| Abuse (w/o D) | 0.6 | 1.3 | 0.6 – 2.2 | 1st | ||
| Abuse (w or w/out D) | 1.7 | 2.0 | 1.6 – 3.9 | 12th | ||
| Bipolar I | Dependence | 6.4 | 6.1 | 4.6 – 9.5 | 61st | 100 |
| Abuse (w/o D) | 1.0 | 2.3 | 0.8 – 4.4 | 1st | ||
| Abuse (w or w/out D) | 2.9 | 3.8 | 2.7 – 7.2 | 8th | ||
| Bipolar II | Dependence | 4.6 | 4.9 | 4.1 – 6.3 | 28th | 100 |
| Abuse (w/o D) | 1.3 | 2.0 | 0.4 – 2.9 | 1st | ||
| Abuse (w or w/out D) | 3.0 | 3.2 | 2.7 – 4.9 | 18th | ||
| Panic w/o ag. | Dependence | 2.3 | 2.4 | 1.9 – 3.0 | 24th | 97.8 |
| Abuse (w/o D) | 1.2 | 1.3 | 1.0 – 3.2 | 12th | ||
| Abuse (w or w/out D) | 1.7 | 1.7 | 1.5 – 3.0 | 56th | ||
| Panic w/ ag. | Dependence | 4.1 | 4.5 | 3.2 – 6.3 | 29th | 100 |
| Abuse (w/o D) | 1.4 | 1.8 | 0.8 – 2.8 | 6th | ||
| Abuse (w or w/out D) | 2.5 | 2.9 | 2.4 – 4.1 | 6th | ||
| Social Phobia | Dependence | 2.7 | 2.9 | 2.3 – 4.1 | 29th | 98.2 |
| Abuse (w/o D) | 1.1 | 1.5 | 1.0 – 2.7 | 3rd | ||
| Abuse (w or w/out D) | 1.7 | 2.0 | 1.6 – 3.0 | 10th | ||
| Specific Phobia | Dependence | 1.8 | 1.9 | 1.6 – 2.4 | 41st | 99.1 |
| Abuse (w/o D) | 1.1 | 1.3 | 1.0 – 1.9 | 1st | ||
| Abuse (w or w/out D) | 1.4 | 1.5 | 1.3 – 2.0 | 5th | ||
| GAD | Dependence | 3.1 | 3.5 | 2.7 – 4.5 | 19th | 100 |
| Abuse (w/o D) | 0.9 | 1.5 | 0.8 – 2.7 | 1st | ||
| Abuse (w or w/out D) | 1.8 | 2.2 | 1.7 – 3.7 | 10th | ||
| Paranoid PD | Dependence | 4.4 | 5.2 | 3.9 – 8.1 | 16th | 100 |
| Abuse (w/o D) | 1.2 | 1.7 | 1.1 – 3.2 | 3rd | ||
| Abuse (w or w/out D) | 2.7 | 2.8 | 2.3 – 5.8 | 25th | ||
| Schizoid PD | Dependence | 3.2 | 3.4 | 2.7 – 4.7 | 27th | 100 |
| Abuse (w/o D) | 1.0 | 1.4 | 1.0 – 2.2 | 2nd | ||
| Abuse (w or w/out D) | 1.9 | 2.1 | 1.7 – 3.3 | 19th | ||
| Schizotypal PD | Dependence | 2.8 | 3.3 | 2.4 – 5.1 | 18th | 100 |
| Abuse (w/o D) | 1.0 | 1.5 | 1.0 – 2.2 | 1st | ||
| Abuse (w or w/out D) | 1.9 | 2.1 | 1.7 – 3.8 | 10th | ||
| Histrionic PD | Dependence | 7.0 | 7.5 | 6.1 – 10.5 | 23rd | 100 |
| Abuse (w/o D) | 1.4 | 2.5 | 1.3 – 4.4 | 1st | ||
| Abuse (w or w/out D) | 3.7 | 4.6 | 3.3 – 8.2 | 9th | ||
| Borderline PD | Dependence | 4.0 | 4.5 | 3.5 – 6.8 | 18th | 100 |
| Abuse (w/o D) | 1.2 | 1.7 | 1.1 – 2.9 | 2nd | ||
| Abuse (w or w/out D) | 2.4 | 2.6 | 2.1 – 5.1 | 31st | ||
| Narcissistic PD | Dependence | 2.9 | 3.4 | 2.7 – 5.0 | 8th | 100 |
| Abuse (w/o D) | 1.1 | 1.4 | 1.0 – 1.9 | 3rd | ||
| Abuse (w or w/out D) | 2.1 | 2.0 | 1.8 – 3.6 | 50th | ||
| Antisocial | Dependence | 6.4 | 7.6 | 5.7 – 11.4 | 12th | 100 |
| Abuse (w/o D) | 2.3 | 2.2 | 1.8 – 4.8 | 66th | ||
| Abuse (w or w/out D) | 4.9 | 4.2 | 3.5 – 9.3 | 84th | ||
| Dependent PD | Dependence | 7.9 | 10.1 | 6.7 – 18.6 | 9th | 100 |
| Abuse (w/o D) | 1.1 | 1.5 | 0.0 – 3.0 | 9th | ||
| Abuse (w or w/out D) | 4.1 | 4.7 | 3.4 – 10.5 | 19th | ||
| Ob-Comp PD | Dependence | 2.2 | 2.3 | 1.9 – 3.2 | 30th | 100 |
| Abuse (w/o D) | 1.1 | 1.4 | 1.0 – 1.6 | 2nd | ||
| Abuse (w or w/out D) | 1.5 | 1.7 | 1.5 – 2.3 | 10th | ||
| Avoidant PD | Dependence | 4.3 | 4.8 | 3.4 – 7.6 | 27th | 99.1 |
| Abuse (w/o D) | 1.1 | 1.6 | 1.0 – 3.9 | 1st | ||
| Abuse (w or w/out D) | 2.5 | 2.7 | 2.0 – 5.5 | 28th |
Note. Dx = diagnosis; AUD = alcohol use disorder; OR = Odds Ratio; %ile = percentile; % D > A = Percentage of 330 permutations in which dependence criteria sets have greater odds ratios than abuse criteria sets; GAD = generalized anxiety disorder; ag = agoraphobia; PD = personality disorder; Abuse (w/o D) = alcohol abuse assuming hierarchical decision rule; Abuse (w or w/out D) = alcohol abuse with no hierarchical decision rule.
Table 2 contains information regarding the relationship between various psychological diagnoses with a diagnosis of dependence or abuse. The first column, Comorbid Dx, indicates the diagnosis being examined in conjunction with the second column (i.e., diagnosis of dependence, abuse without dependence, and abuse with or without dependence). The third column provides the observed odds ratio for the relationship with the comorbid diagnosis and the current DSM-IV algorithm, while the following column indicates the median odds ratio of all possible permutations of items as described in the previous section. The fifth column, OR Range, indicates the range under the permutation distribution, and the sixth column provides the observed percentile of the DSM-IV algorithm under the permutation distribution. Finally, as noted above, the last column shows the percentage of times in the permutation distribution that the odds ratio for dependence was greater than that of abuse
It is also useful to consider the findings of how the comorbidity measures of current DSM-IV algorithm compare against the entire distribution of comorbidity measures (assessed via ORs). The third column of Table 2 shows that for each disorder considered, the OR for dependence is higher than for abuse using the DSM-IV criteria sets (replicating a common finding in the literature). However, as illustrated in Table 2, with one exception, the ORs for the DSM-IV criteria sets are in the lower half of the distribution indicating that various other partitions typically provide stronger associations with related psychopathology. Interestingly, with respect to abuse, the criteria set of DSM-IV tends to show significantly lower measures of association than other partitions. This suggests that “swapping” one (or more) abuse and dependence item(s) increases comorbidity for the abuse category (but never sufficiently to be stronger than the weakest association between a “dependence” set and a comorbid condition).
This seeming asymmetry is puzzling but can be attributed to the generally lower base rates of the items in the DSM-IV abuse set (.01, .01, .02, 08; Mdn=.015) versus the DSM-IV dependence set (.01, .02, .03, .06, .07, .08, .08; Mdn=.06) where the median endorsement rate is four times higher in the dependence set than in the abuse sets. Coupled with the inter-item correlation, it is often the case that the more severe items in the abuse set are endorsed simultaneously with three or more of the items in the dependence set. This relationship naturally precludes an individual from diagnosing as “abuse” because of the hierarchical decision rule. This is illustrated in Table 3 which consistently shows a higher percentile of the DSM-IV abuse set when a dependence diagnosis is ignored (i.e., no exclusion). When this permutation distribution is considered, the ORs for the DSM-IV abuse set fall within chance expectation.
Table 3.
Stability of AUD criteria and their relationship with dependence and abuse symptom counts
| Stability Measures | Correlations | ||||||
|---|---|---|---|---|---|---|---|
| Wave 1 | Kappa/ product- moment correlation |
PPV | Tetrachoric | Abuse Total Wave 2 |
Dependence Total Wave 2 |
AUD Total Wave 2 |
|
| Dependence | |||||||
| (r̅ = .36) | Tolerance | .21 | .29 | .54 | .20 | .29 | .29 |
| CutDown | .30 | .43 | .60 | .19 | .32 | .31 | |
| Larger/Longer | .30 | .43 | .60 | .23 | .33 | .34 | |
| Withdrawal | .33 | .40 | .66 | .24 | .35 | .35 | |
| GiveUp | .23 | .24 | .83 | .23 | .23 | .25 | |
| TimeDrinking | .24 | .27 | .73 | .23 | .28 | .29 | |
| Continued | .28 | .35 | .70 | .24 | .32 | .32 | |
| Total(α=.77)a | .33 | .46 | .46 | ||||
| Abuse | |||||||
| (r̅ = .28) | RoleInterference | .26 | .28 | .84 | .23 | .24 | .26 |
| Hazardous | .31 | .36 | .63 | .30 | .25 | .29 | |
| LegalProblems | .06 | .06 | .63 | .15 | .16 | .17 | |
| Interpersonal | .21 | .18 | .76 | .25 | .28 | .30 | |
| Total(α=.50)b | .36 | .34 | .38 | ||||
| AUD | Total(α=.80) | .37 | .47 | .48 | |||
Note. PPV = positive predictive value. In this instance, Kappa and the product-moment correlation are equivalent when the marginal distributions of the agreement table are homogeneous, or nearly so, as in this case (for details, see Cohen, 1961). r̅ = the average inter-item correlation for each set of criteria. CutDown = Persistent desire or unsuccessful efforts to cut down or control drinking. Larger/Longer = Drinking larger amounts or for longer periods than intended. GiveUp = Giving up or reducing important social, occupational or recreational activities in favor of drinking. TimeDrinking = A great deal of time spent in activities to obtain alcohol to drink, or to recover from its effects. Continued = Continued drinking despite knowledge of a physical or psychological problem caused or exacerbated by drinking. RoleInterference = Failure to fulfill major role obligations at work/school/home. Hazardous = Use in hazardous situations. LegalProblems = Legal problems related to drinking. Interpersonal = Social or interpersonal problems.
α corresponds to a mean inter-item correlation of .36.
α corresponds to a mean inter-item correlation of .28.
Discussion
Although we consider the implications of our findings for diagnostic revision, we are not specifically challenging the underlying validity of the construct of dependence which, to our thinking, has been and remains the cardinal AUD diagnosis. We also do not specifically challenge the notion of abuse, at least to the extent that it indicates problems or potential problems that are associated with alcohol consumption (although we do question its utility as a formal diagnosis as described below). We note that a number of authors have addressed these issues and this area of research continues to be one of active debate (e.g., Hasin et al., 2003; Hasin & Beseler, 2009; Hasin et al., 2006; Martin et al., 2008; Slade, Grove & Teesson, 2009; Schuckit & Saunders, 2006).
Specifically, the primary question we posed was whether differential chronicity or strength of comorbidity can be used to validate the abuse/dependence distinction as some have argued (e.g., Grant et al., 2001; Schuckit et al., 2001). Our findings point to a resounding “no!” and indicate that such differential strengths of association are an artifact of the hierarchical and asymmetric decision rules of DSM-IV. Furthermore, the present study illustrates that the current items assigned to the abuse and dependence criteria sets are non-optimal for the purpose of creating a diagnosis that is either stable or is highly comorbid. Prior research that attempted to demonstrate differential stability and comorbidity failed to consider the effects of the diagnostic algorithm that, for all practical purposes, precluded the ability to assess such optimality. Should future diagnostic distinctions within alcohol use disorders be based upon separate criteria sets (e.g., as did DSM-IV abuse and dependence), validation of such distinctions need to consider both item content and decision rules simultaneously when evaluating the validity of such diagnostic distinctions. We intend on extending the elements of the current strategy to search for optimal subsets of items that are designed to either optimize stability, comorbidity, or both. Additionally, optimal subsets could be created for a variety of purposes with varying degrees of predictive validity, depending on the theoretical notions being investigated.
While consistent with the findings of item response theory (IRT), the obtained results should not be viewed as redundant with prior analysis. Specifically, IRT can be viewed as an 'endogenous' procedure in the sense that the IRT analysis on the dependence and abuse criteria are unrelated to their predictive capacity. An analogous problem is when either principal component scores or factor scores are used as predictors. Namely, there is no guarantee that the dimensions that account for the most variance will be related to the outcome variables -- and very often will not be the best predictor. So, although our findings are consistent with those of IRT analyses showing the severity of abuse and dependence criteria overlap, IRT analyses are silent with respect to both issues of stability and external criteria that can be used to assess construct validity. The primary extension of the IRT results is provided with the comparative predicted power of the dependence and abuse criteria sets with those obtained under the permutation distribution.
DSM-IV, like many diagnostic systems, is hierarchically organized (Blashfield & Livesley, 1999). Most relevant for the current discussion, the DSM-IV presents hierarchies of disorders that represent diagnostic “pecking” orders. For example, some diagnoses like Schizophrenia “trump” other related conditions (e.g., Delusional Disorder). Similarly, if the threshold for substance dependence is met, one cannot receive a diagnosis of substance abuse. Unfortunately, empirical support for hierarchical distinctions such as these was not presented before DSM-IV and ICD-10 (and their predecessors) were adopted. In fact, although not many studies have directly examined these, there are challenges to hierarchical and exclusionary rules in the case of schizophrenia and delusional disorder (e.g., Boyd et al., 1984), anxiety disorders (e.g., Andrews, 2000) and mood disorders (e.g., Wakefield, Schmitz, First, & Horwitz, 2007).
Ideally, for two disorders to be distinct, there should be no overlap in major defining features that are required (Kendell, 1975). For example, despite the fact that depressive symptoms can occur in both diagnoses, bipolar I and major depressive disorder are not overlapping diagnoses because a manic episode is necessary in bipolar I disorder but cannot be present in major depressive disorder. Although this example points out general problems with hierarchical diagnoses, the situation is slightly different with respect to the abuse and dependence syndromes. In the case of bipolar I disorder, a manic episode is considered to be categorically distinct from a depressive episode. With respect to abuse and dependence, these syndromes are considered to be related to each other (not categorically distinct), yet their definition involves both different symptom content as well as different level of severity (more or fewer symptoms). Unfortunately, with respect to abuse and dependence, this is not the case. “Abuse” items, in many cases, can be seen as severe or as impairing as many “dependence” items (e.g., Langenbucher et al., 2004; Saha et al., 2006, 2007). Therefore, simply requiring a lower number for one or the other is artificial and only indicates the severity along one dimension. Again, this is not to say that such a distinction is not necessary or is fundamentally invalid. Rather, citing chronicity and comorbidity findings as support for such a distinction is highly fallible with respect to their probative value concerning construct validity.
The question then becomes “what data are necessary to support the validity of DSM-IV hierarchical decision rule concerning the precedence of alcohol dependence syndrome over alcohol abuse syndrome?” Although decision rules can be validated with respect to some forms of external criteria (e.g., specific genotypes, biomarkers), using chronicity and comorbidities as validating criteria appear to be hazardous when decision rules are used to distinguish conditions with overlapping symptomatology. In DSM-IV, abuse and dependence are distinguished by a combination of numbers and assumed types of problems/symptoms. However, our analyses clearly demonstrate that for all intents and purposes, it is only numbers that drive purportedly validating associations with meaningful criteria, calling into account the relevance of the distinction between the abuse and dependence item sets in the DSM-IV.
Returning to the issue of the abuse/dependence distinction, we question whether any hierarchical decision rules are necessary in constructing the alcohol use disorder category and the “value added” contribution of abuse over and above dependence. That is, if someone is heedless and consistently engages in hazardous drinking (e.g., drinking while driving; see Langenbucher & Martin, 1996, for a similar definition of abuse that incorporates some of the current dependence criteria) but shows no symptoms of dependence (that is, the drinker’s brain shows no signs of being alcohol-centric; Sher, Wolf, & Martinez, 2009), why would we think an alcohol use disorder should be used to describe this condition? Moreover, should hazardous use be considered an indicator of an individual disorder (even if still unambiguously a public health problem) if the drinker is unaware of or doesn’t fully believe or appreciate the hazardous nature of the behavior. That is, is ignorance “diagnosable?” Alcohol consumption is strongly associated with fatal and nonfatal pedestrian injuries (Holubowycz, 1995; Ryb, Dischinger, Kufera, & Soderstrom, 2007) but it seems likely that such knowledge is not commonly held by most drinkers who may often engage in “risky” pedestrian activities.
If we adopt the perspective that a mental disorder is a harmful dysfunction (Spitzer & Endicott, 1978; Wakefield, 1992, 1997, 1999), hazardous use by itself might reflect poor judgment which, although harmful, doesn’t necessarily reflect a dysfunction unless we were to assume that poor judgment is ipso facto evidence of dysfunction…seemingly a major leap. It is perhaps possible that an individual is highly specialized in their heedlessness (i.e., does not show generalized poor judgment or heedlessness, see below) and has no evidence of dependence. Should such a situation call for a diagnosis of abuse? Perhaps, but if it were to reserve abuse for such occasions as a stand-alone diagnosis, wouldn’t we logically want to have parallel diagnoses for other isolated heedless activities (e.g., “driving abuse” for non-alcohol-related reckless driving). Indeed, recent evidence suggest that texting while driving represents a risk for motor vehicle crashes that can exceed those associated with legal intoxication (Virginia Tech Transportation Institute, 2009). Do we want to have a texting abuse category or, more generally, an abuse category for every behavior that when associated with a specific context or activity involves heightened risk for adverse consequences? If isolated heedlessness related to alcohol use is someone’s only problem with disinhibition and with no evidence of dependence, why not simply have a V code for nondependent alcohol problems?
Alternatively, if poor judgment or poor behavior regulation is part of a more pervasive syndrome (e.g., antisocial personality disorder; problem behavior syndrome, Jessor & Jessor, 1977) without evidence of dependence, it would seem more appropriate to classify it there with, perhaps, a qualifier with associated alcohol problems. Such a qualifier could be used to indicate problems associated with dependence as well. The value of distinguishing a diagnosis from a qualifier would seem to hinge on whether or not the symptoms under consideration are referencing primary or secondary manifestations of the underlying disorder and whether it is clinically useful.
With advances in behavioral assessment of alcohol-related phenotypes closer to neurobiological models of dependence (e.g., incentive sensitization; Robinson & Berridge, (2003), we might be able to move closer to assessing our constructs more directly using “implicit” behavioral measures (Sher et al., 2009) and not rely on self-report which has, unfortunately, become the foundation of diagnostic research in mental disorders. In the interim, however, we need to be cautious in the types of conclusions we draw from interpreting patterns of correlations with varied outcomes related to course and comorbidity if our goal is to provide meaningful validation.
Until such time that more direct assessments of key “dysfunctions” or similar processes are available, diagnosis will continue to rely on patient or collateral reports or clinician observations of signs and symptoms of alcohol-related pathology. The ultimate items sets and thresholds for such diagnoses cannot be fully anticipated at this time (although prior data and theory on the alcohol dependence syndrome [e.g., Edwards & Gross, 1976] or cardinal symptoms of dependence as in the “withdrawal gate” model [Langenbucher et al., 2000] represent viable starting points). However, based on the current analyses, the hierarchical decision rule currently employed in the DSM-IV’s abuse/dependence criteria should be abandoned.
Summary Recommendations
If the hierarchical decision rule is to be abandoned, what should be done? At least two alternative approaches appear viable at present. As noted above, if framers of DSM-V wish to maintain a distinction between the alcohol dependence syndrome and alcohol-related disabilities ala Edwards and Gross (1976), it would seem most justifiable to view these as correlated but not hierarchically organized diagnoses (or dimensions). Although such a distinction may be hard to justify based on psychometric work that fails to reliably demonstrate the implied factor structure (e.g., Langenbucher et al., 2004; Martin, Chung, Kirisci & Langenbucher, 2006; Saha et al., 2006. But see Harford & Muthén, 2001 for a two-factors solution that, although similar to the dependence/abuse structure, does not maintain the same criteria assigned to each category), the conceptual distinction is clear and could be useful for needs assessment, treatment planning, and psychoeducational approaches..
Alternatively, we could combine criteria sets to derive a single AUD criteria set (Martin et al., 2008) as is currently under consideration for DSM-V (American Psychiatric Association, 2010). This latter approach would resolve the psychometric mess that the current system has generated. However, it fails to resolve an important conceptual distinction between “dysfunction” as manifested by deranged psychobiological processes (i.e., dependence which we view as primary) and “problems” (which we see as either secondary to dependence, secondary to another disorder such as syndromal externalizing disorders, or just a direct manifestation of psychosocial immaturity or trait-like heedlessness).
We would argue that the tendency to want to lump consequence items with dependence items stems, in part, from our over-reliance on self-report for psychiatric diagnosis. That is, without the ability to directly assess primary underlying pathology, we look for secondary indicators to gauge the harm in its stead. This is akin to diagnosing diabetes on the basis of its medical complications (e.g., on heart, eyes, nerves) rather than on blood glucose levels. A constellation of associated conditions can increase suspicion of a specific underlying problem but is not equivalent to it. Consequently, we would argue for a conceptually pure and psychometrically sound dependence criteria set that is the cardinal diagnosis, perhaps with subtyping based on the degree or kinds of problems associated with dependence. In the absence of such dependence, such “abuse” problems could be viewed simply as a feature of another disorder (e.g., conduct disorder, antisocial personality disorder, or borderline personality disorder) or a V code.
Supplementary Material
Acknowledgments
This research was supported by NIH grants K05AA017242 and R01AA016392 to Kenneth J. Sher, K25AA017456 to Douglas Steinley, and P60AA011998 to Andrew C. Heath.
Footnotes
The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ABN
The seven dependence criteria are (1) tolerance, (2) withdrawal, (3) drinking larger amounts or over a longer period than intended, (4) persistent desire or unsuccessful efforts to cut down or control drinking, (5) a great deal of time spent in activities to obtain alcohol, or to recover from its effects, (6) giving up or reducing important social, occupational or recreational activities because of drinking, and (7) continued drinking despite knowledge of a physical or psychological problem that is likely to have been caused or exacerbated by drinking.
The four abuse criteria are (1) failure to fulfill major role obligations at work, school or home, (2) drinking in situations in which it is physically hazardous, (3) legal problems related to drinking, and (4) drinking despite having social or interpersonal problems caused or exacerbated by alcohol.
The study by Schuckit et al. (2001) is the only one, among the studies reviewed here, that reports both an estimate of chronicity for dependence as defined in the DSM-IV (requiring the presence of only one of the 11 AUD symptoms) and an estimate requiring three or more dependence symptoms. The latter provides a more useful comparison of persistence of dependence and abuse but is not included in the other reports.
In order to provide meaningful comparisons, stability was calculated ignoring the requirement of ruling out a lifetime dependence diagnosis to get a diagnosis of abuse.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed., text revision. Washington, DC: Author; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Alcohol-use disorder [Web page] 2010 February 10; Retrieved from http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=452.
- Andrews G. The anxiety disorder inclusion and exclusion criteria in DSM-IV and ICD-10. Current Opinion in Psychiatry. 2000;13:139–141. [Google Scholar]
- Blashfield RK, Livesley WJ. Classification. In: Millon T, Blaney PH, Davis Rd, editors. Oxford textbook of psychopathology. New York: Oxford; 1999. pp. 3–28. [Google Scholar]
- Boyd JH, Burke JD, Gruenberg E, Holzer CE, Rae DS, George LK, Nestadt G. Exclusion criteria of DSM-III: A study of co-occurrence of hierarchy-free syndromes. Archives of General Psychiatry. 1984;41:983–989. doi: 10.1001/archpsyc.1984.01790210065008. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: Provisional description of a clinical syndrome. British Medical Journal. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelhorn H, Hartman C, Sakai J, Stallings M, Young S, Rhee SH, Crowley T. Toward DSM-V: An item response theory analysis of the diagnostic process for DSM-IV alcohol abuse and dependence in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:1329–1339. doi: 10.1097/CHI.0b013e318184ff2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version (AUDADIS-IV) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Alcohol Research & Health. 2006;29:79–91. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering RP. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug & Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey. Drug & Alcohol Dependence. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Muthen BO, Hsiao-ye Y, Hasin DS, Stinson FS. DSM-IV alcohol dependence and abuse: Further evidence of validity in the general population. Drug and Alcohol Dependence. 2007;86:154–166. doi: 10.1016/j.drugalcdep.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KD. Source and Accuracy Statement for the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- Grant BF, Moore TC, Kaplan KD. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Grant BF, Pickering RP. Comorbidity betweeen DSM-IV alcohol and drug use disorders: Results from the National Longitudinal Alcohol Epidemiologic Survey. Alcohol Health & Research World. 1996;20:67–72. [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Harford T. The 5-year course of alcohol abuse among young adults. Journal of Substance Abuse. 2001;13:229–238. doi: 10.1016/s0899-3289(01)00078-5. [DOI] [PubMed] [Google Scholar]
- Harford TC, Muthén BO. The dimensionality of alcohol abuse and dependence: A multivariate analysis of DSM-IV symptom items in the National Longitudinal Survey of Youth. Journal of Studies on Alcohol. 2001;62:150–157. doi: 10.15288/jsa.2001.62.150. [DOI] [PubMed] [Google Scholar]
- Hasin DS. Classification of Alcohol Use Disorders. Alcohol Research & Health. 2003;27:5–17. [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Beseler CL. Dimensionality of lifetime alcohol abuse, dependence and binge drinking. Drug and Alcohol Dependence. 2009;101:53–61. doi: 10.1016/j.drugalcdep.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. Major depression in 6050 former drinkers: Association with past alcohol dependence. Archives of General Psychiatry. 2002;59:794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Grant BF, Endicott J. The natural history of alcohol abuse: Implications for definitions of alcohol use disorders. The American Journal of Psychiatry. 1990;147:1537–1541. doi: 10.1176/ajp.147.11.1537. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Hatzenbuehler ML, Keyes K, Ogburn E. Substance use disorders: Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) and International Classification of Diseases, tenth edition (ICD-10) Addiction. 2006;101:59–75. doi: 10.1111/j.1360-0443.2006.01584.x. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Paykin A. Alcohol dependence and abuse diagnoses: Concurrent validity in a nationally representative sample. Alcoholism: Clinical and Experimental Research. 1999;23:144–150. [PubMed] [Google Scholar]
- Hasin DS, Schuckit MA, Martin CS, Grant BF, Bucholz KK, Helzer JE. The validity of DSM-IV alcohol dependence: what do we know and what do we need to know? Alcoholism: Clinical & Experimental Research. 2003;27:244–252. doi: 10.1097/01.ALC.0000060878.61384.ED. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hasin DS, van Rossem R, McCloud S, Endicott J. Differentiating DSM-IV alcohol dependence and abuse by course: Community heavy drinkers. Journal of Substance Abuse. 1997;9:127–135. doi: 10.1016/s0899-3289(97)90011-0. [DOI] [PubMed] [Google Scholar]
- Holubowycz OT. Age, sex, and blood alcohol concentration of killed and injured pedestrians. Accident Analysis and Prevention. 1995;27:417–422. doi: 10.1016/0001-4575(94)00064-s. [DOI] [PubMed] [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. New York, NY: Academic Press; 1977. [Google Scholar]
- Kendell RE. The concept of disease and its implications for psychiatry. British Journal of Psychiatry. 1975;127:305–315. doi: 10.1192/bjp.127.4.305. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Labouvie E, Martin CS, Sanjuan PM, Bavly L, Kirisci L, Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Martin CS. Alcohol abuse: Adding content to category. Alcoholism: Clinical & Experimental Research. 1996;20:270A–275A. doi: 10.1111/j.1530-0277.1996.tb01790.x. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Martin CS, Labouvie E, Sanjuan PM, Bavly L, Pollock NK. Toward the DSM-V: The Withdrawal-Gate Model versus the DSM-IV in the diagnosis of alcohol abuse and dependence. Journal of Consulting and Clinical Psychology. 2000;68:799–809. [PubMed] [Google Scholar]
- Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: Implications for DSM-V. Journal of Abnormal Psychology. 2006;115:807–814. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Langenbucher JW. How should we revise diagnostic criteria for substance use disorders in the DSM-V? Journal of Abnormal Psychology. 2008;117:561–575. doi: 10.1037/0021-843X.117.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Auilar-Gaziola S, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: Results of the international consortium in psychiatric epidemiology. Addictive Behaviors. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Mielke PW, Berry KJ. Permutation Methods. New York: Springer; 2007. [Google Scholar]
- Robinson TE, Berridge KC. Addiction. Annual Review of Psychology. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- Ryb GE, Dischinger PC, Kufera JA, Soderstrom CA. Social, behavioral and driving characteristics of injured pedestrians: A comparison with other unintentional trauma patients. Accident Analysis and Prevention. 2007;39:313–318. doi: 10.1016/j.aap.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Saha TD, Chou S, Grant BF. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug and Alcohol Dependence. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Danko GP, Smith TL, Bierut LJ, Bucholz KK, Edenberg HJ, Hinga B. The prognostic implications of DSM-IV abuse criteria in drinking adolescents. Drug and Alcohol Dependence. 2008;97:94–104. doi: 10.1016/j.drugalcdep.2008.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Saunders JB. The empirical basis of substance use disorders diagnosis: Research recommendations for the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-V) Addiction. 2006;101:170–173. doi: 10.1111/j.1360-0443.2006.01611.x. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL. A comparison of correlates of DSM-IV alcohol abuse or dependence among more than 400 sons of alcoholics and controls. Alcoholism: Clinical and Experimental Research. 2001;25:1–8. [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Danko GP, Bucholz KK, Reich T, Bierut LB. Five-year clinical course associated with DSM-IV alcohol abuse or dependence in a large group of men and women. The American Journal of Psychiatry. 2001;158:1084–1090. doi: 10.1176/appi.ajp.158.7.1084. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Landi NA. The 5-year clinical course of high-functioning men with DSM-IV alcohol abuse or dependence. The American Journal of Psychiatry. 2000;157:2028–2035. doi: 10.1176/appi.ajp.157.12.2028. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Wolf ST, Martinez JA. How can etiological research inform the distinction between normal drinking and disordered drinking? In: Scheier LM, editor. Handbook of drug use etiology. Washington, DC: American Psychological Association; 2009. pp. 225–246. [Google Scholar]
- Slade T, Grove R, Teesson M. A taxometric study of alcohol abuse and dependence in a general population sample: Evidence of dimensional latent structure and implications for DSM-V. Addiction. 2009;104:742–751. doi: 10.1111/j.1360-0443.2009.02498.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J. Medical and mental disorder: Proposed definition and criteria. In: Spitzer RL, Klein DF, editors. Critical issues in psychiatric diagnosis. New York: Raven Press; 1978. pp. 15–39. [Google Scholar]
- Virginia Tech Transportation Institute. New Data from VTTI Provides Insight into Cell Phone Use and Driving Distraction [Web page] 2009 July 27; Retrieved from http://www.vtti.vt.edu/PDF/7-22-09-VTTI-Press_Release_Cell_phones_and_Driver_Distraction.pdf.
- Wakefield JC. Disorder as harmful dysfunction: A conceptual critique of DSM-III--R's definition of mental disorder. Psychological Review. 1992;99:232–247. doi: 10.1037/0033-295x.99.2.232. [DOI] [PubMed] [Google Scholar]
- Wakefield JC. When is development disordered? Developmental psychopathology and the harmful dysfunction analysis of mental disorder. Development and Psychopathology. 1997;9:269–290. doi: 10.1017/s0954579497002058. [DOI] [PubMed] [Google Scholar]
- Wakefield JC. Evolutionary versus prototype analyses of the concept of disorder. Journal of Abnormal Psychology. 1999;108:374–399. doi: 10.1037//0021-843x.108.3.374. [DOI] [PubMed] [Google Scholar]
- Wakefield JC, Schmitz MF, First MB, Horwitz AV. Extending the bereavement exclusion for major depression to other losses: Evidence from the National Comorbidity Survey. Archives of General Psychiatry. 2007;64:433–440. doi: 10.1001/archpsyc.64.4.433. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.