Abstract
Introduction:
Research on the relationship between emotional disorders and smoking often characterizes anxiety and depression at the broad syndrome level. Because of the complex concordance and discordance across and within anxiety and depressive symptoms, research using this approach may be limited. Watson and Clark developed the tripartite model of anxiety and depression, which identifies negative affect (NA), anhedonia and low positive affect (PA), and anxious arousal (AA) as traits that characterize the underlying heterogeneity in emotional symptoms. An emerging literature has examined the relation between the affective constructs in the tripartite model and smoking; however, these findings have not been summarized and integrated. The aim of this report reviews the literature on the association between tripartite affective dimensions (anhedonia and low PA, NA, and AA) and smoking variables (smoking status, heaviness, chronicity, dependence, cessation, craving/urge).
Methods:
Qualitative summarization and integration of findings.
Results:
All three dimensions were consistently associated with smoking status but demonstrated mixed or no relationship with smoking heaviness, chronicity, and dependence. Low PA and anhedonia consistently associated with craving and relapse, even in studies that controlled for other dimensions. Emotional disturbance on multiple dimensions (e.g., low PA + high NA) was associated with disproportionate increases in smoking risk in several studies.
Conclusions:
Tripartite dimensions may each have differential effects on smoking. Anhedonic and low PA individuals (especially those with concurrent NA or AA) may be a high-risk group worthy of targeting for interventions. Continued research of the affective dimensions linked with smoking could inform the etiology of tobacco dependence and lead to more effective smoking interventions that target affect.
Introduction
Emotional (mood and anxiety) disorders and cigarette smoking are highly prevalent and comorbid. Worldwide, an estimated 1 billion individuals smoke tobacco (World Health Organization, 2009). Mood disorders range from approximately 0.8% to 9.6% throughout the world (Demyttenaere et al., 2004), and anxiety disorders range from approximately 2.4% to 18.2% throughout the world (Demyttenaere et al., 2004). Importantly, substantial evidence suggests strong associations between smoking and emotional disorders (Breslau, Kilbey, & Andreski, 1991; Grant, Hasin, Chou, Stinson, & Dawson, 2004; Lasser et al., 2000; Morrell & Cohen, 2006; Williams, Hudson, & Redd, 1982). This association generalizes across multiple subtypes of the depressive (e.g., dysthymia and major depression) and of the anxiety (e.g., panic disorder, generalized anxiety disorder, social phobia, specific phobia, posttraumatic stress disorder) disorders (Grant et al., 2004; Lasser et al., 2000) and is also evident for continuous measures of emotional disturbance (Breslau, 1995; Breslau, Kilbey, & Andreski, 1994; Lerman et al., 1996).
Research suggests a reciprocal and dynamic relationship between emotional disorders and smoking, with evidence that both may be risk factors for each other (Breslau, Peterson, Schultz, Chilcoat, & Andreski, 1998; Kandel, Huang, & Davies, 2001). Despite the complexity of this relationship, there is sufficient evidence from several sources to indicate that emotional disorders play an important role in the onset of smoking for a significant portion of individuals (Breslau, Kilbey, & Andreski, 1993; Orlando, Ellickson, & Jinnett, 2001; Rohde, Kahler, Lewinsohn, & Brown, 2004), emphasizing the importance of understanding the link from emotional disorders to smoking vulnerability. In addition, smokers with emotional disturbance may be less likely to quit, may be more vulnerable to relapse, and may require more cessation attempts to successfully quit (Anda et al., 1990; Covey, 1999; Ginsberg, Hall, Reus, & Munoz, 1995; Glassman et al., 1988; Haas, Munoz, Humfleet, Reus, & Hall, 2004). These findings have led to the development of various cessation treatments meant to target affective disturbance. However, smoking cessation counseling programs incorporating cognitive behavioral therapy for depression or mood management strategies, which mainly focus on negative mood and depressive symptoms, have not proven effective for the majority of smokers (Brown et al., 2001, 2007; Hall et al., 1998, 2002). Thus, further knowledge of the etiological processes linking emotional disturbance and smoking vulnerability is needed to inform the refinement of mood-targeting smoking cessation interventions.
Research on the role of emotional disturbance in smoking has often characterized depression and anxiety at the broad syndrome level (e.g., presence vs. absence of major depression, severity of overall anxious symptomatology). One potential barrier to these efforts is the complex concordance and discordance across and within the various features that comprise anxiety and depressive syndromes. Although anxiety and depression symptoms are putatively distinct from one another, they have proven hard to differentiate empirically, especially on the diagnostic level (Clark & Watson, 1991; Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995). To further complicate matters, there is substantial heterogeneity in the symptomatology within the depressive (Hasler, Drevets, Manji, & Charney, 2004; Shafer, 2006) and anxiety (Ree, French, MacLeod, & Locke, 2008; Smoller & Tsuang, 1998) syndromes.
Watson and Clark proposed a tripartite model of anxiety and depression to characterize the traits underlying the heterogeneity in emotional symptoms, which consists of a shared negative affect (NA)/general distress component that cuts across anxiety and depression (generalized NA), two related constructs specific to depression (anhedonia and low positive affect [PA]), and a specific factor for anxiety (anxious arousal [AA]) (Clark & Watson, 1991; Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995). The tripartite model has garnered considerable attention in the emotional disturbance literature (e.g., Brown, Chorpita, & Barlow, 1998; Joiner et al., 1999; Mausbach, Roepke, Depp, Patterson, & Grant, 2009), and there is relatively consistent support for the validity of this model (Joiner et al., 1999; Mausbach et al., 2009; Watson & Clark, 1997).
Although an empirical literature on the roles of PA and anhedonia, NA, and AA in smoking is emerging, these findings are yet to be summarized and integrated. This is a notable gap in the literature as summarizing and integrating this body of research has the potential to elucidate patterns of findings regarding the relationship between specific underlying affective dimensions and particular aspects of smoking behavior. Such information may help clarify the mechanisms linking emotional disorders and different stages of the tobacco dependence process (i.e., smoking imitation, maintenance, persistence, cessation, and relapse), which could ultimately inform the development of more effective smoking prevention and cessation treatments that target affect.
Accordingly, this integrative review paper aims to: (a) describe the basic tenets of the tripartite model of anxiety and depression, (b) review extant research on the univariate associations of each of the three tripartite dimensions to smoking variables (i.e., smoking status, smoking heaviness and chronicity, nicotine dependence, cessation, and craving/urge), (c) review multivariate analyses that have explored the concomitant relationships of multiple tripartite affective dimensions to smoking variables, and (d) summarize general patterns of findings identified in the review, the resulting clinical implications, and future research directions.
The Tripartite Model of Anxiety and Depression
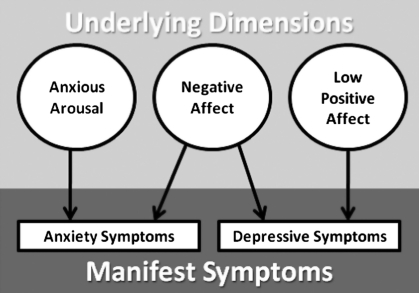
The symptoms of anxiety disorders are phenomenologically heterogeneous and involve a wide array of emotional (e.g., apprehensive feelings, tension, irritability) and physical (e.g., pounding heart, shortness of breath, sweating) symptoms. Depressive symptoms are also heterogeneous, involving a broad constellation of emotional (e.g., loss of interest and pleasure, feelings of hopelessness or helplessness, self-loathing) and physical (e.g., change in appetite, change in sleep, loss of energy) symptoms. The tripartite model proposes that most of the between-person variability in emotional symptoms can be captured by three underlying affective dimensions: NA, anhedonia and low PA, and AA. See figure 1 for a visual representation of the tripartite model.
Figure 1.
Visual representation of the tripartite model of anxiety and depression (Clark & Watson, 1991). Circles represent latent dimensions. Rectangles represent manifest symptoms.
Anxiety and depression are both centered on negative mood states (Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995) and often show a large empirical correlation (Brown et al., 1998; Clark & Watson, 1991; Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995), suggesting a common underlying component between these two constructs. Clark & Watson (1991) identified NA as the central, inseparable, and shared component of anxiety and depression. NA represents the extent to which a person feels upset or unpleasant and includes a diverse range of aversive emotional states such as: upset, distress, anger, guilt, fear, sadness, scornfulness, disgust, and worry.
Anhedonia and low PA have been considered to be representative of the component of affect specific to depression. PA reflects the extent to which a person feels energy and pleasure and includes states such as: happiness, pleasure, energy, delight, interest, enthusiasm, and pride (Clark & Watson, 1991). Low PA is reflected in states such as boredom, fatigue, languor, and attenuated pleasure. Anhedonia is defined as a reduced ability to experience PA in response to pleasant stimuli. An emerging literature suggests that low PA and anhedonia are specific markers of depression (e.g., Leventhal, Chasson, Tapia, Miller, & Pettit, 2006; Snaith, 1993) and can successfully differentiate depression from anxiety (i.e., low PA and anhedonia demonstrate stronger correlations with depression than with anxiety; Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995; Leventhal et al., 2006). It is important to note that though low PA and anhedonia are empirically related with one another (rs = .20–.43; Cook, Spring, & McChargue, 2007; Franken, Rassin, & Muris, 2007; Leventhal, Waters, Kahler, Ray, & Sussman, 2009), they are not identical constructs. Indeed, it is possible for individuals to experience temporary states of low PA, but nonetheless be able to experience pleasure upon encountering a rewarding stimulus. Nonetheless, we included papers utilizing measures of either low PA or anhedonia in this review because these constructs are both indicative of an appetitive deficit that is specific to depression and separate from anxiety.
Although NA and PA are commonly conceptualized as opposite poles of a single continuum, research suggests that these two constructs map onto relatively orthogonal underlying dimensions (Watson, Clark, & Tellegen, 1988). Thus, it is common for individuals to express high NA without concurrently reporting low PA and vice versa. Furthermore, extant data indicate that these two dimensions have unique etiologies and have distinct patterns of relations with relevant external variables (Baker, Cesa, Gatz, & Mellins, 1992; Davidson, Saron, Senulis, Ekman, & Friesen, 1990; Mausbach et al., 2009).
AA reflects the extent to which an individual experiences somatic tension and arousal and includes shortness of breath, feeling dizzy or lightheaded, dry mouth, trembling, shaking, and racing heart (Joiner et al., 1999; Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995). Research indicates that AA is distinct from subjective anxiety (i.e., anxious/apprehensive mood) and can differentiate individuals with panic disorders, which is considered to be a prototypical high-AA syndrome, from individuals with generalized anxiety disorder, which is considered a prototypical disorder of nonspecific distress (Joiner et al., 1999; Watson, Clark, Weber, & Assenheimer, 1995; Watson, Clark, Weber, Assenheimer, et al., 1995), although the symptoms that best characterize and define AA are still in question (Brown et al., 1998; Joiner et al., 1999; Keogh & Reidy, 2000; Nitschke, Heller, Imig, McDonald, & Miller, 2001).
Approach of the Review
Scope of Articles Included in the Review
Although a measure has been developed to specifically assess the three tripartite dimensions (i.e., the Mood and Anxiety Symptom Questionnaire [MASQ; Nitschke et al., 2001; Watson, Clark, Weber, Assenheimer, et al., 1995]), there are a number of measures that assess facets within one of the “meta-constructs” of anhedonia and low PA, NA, and AA. Accordingly, to increase the comprehensiveness of this review, we included studies that utilized measures that we believe assess features that fall into the “meta-constructs” of anhedonia and low PA, NA, and AA, as well as studies using the MASQ.
For example, investigations utilizing the Anxiety Sensitivity Index—Physical Concerns subscale (ASI-PC; Reiss, Peterson, Gursky, & McNally, 1986), which assesses anticipation, apprehension, and fear of AA-related symptoms, were included in the review of the AA–smoking relationship. Although this construct is not part of the tripartite model by Clark and Watson (1991), we included studies incorporating measures of ASI-PC because: (a) AA and ASI-PC are empirically related (rs = .56–.61) and ASI-PC is more robustly associated with AA than alternate anxiety-related measures (Brown, Smits, Powers, & Telch, 2003; Longley, Watson, Noyes, & Yoder, 2006; McLeish, Zvolensky, Yartz, & Leyro, 2008; Zinbarg, Brown, Barlow, & Rapee, 2001) and (b) theoretical contentions propose that fear of AA is a central predisposing factor for panic spectrum and other anxiety disorders (Reiss, 1987; Reiss & McNally, 1985).
Studies using either measures of anhedonia, such as the Snaith–Hamilton Pleasure Capacity Scale (SHAPS; Snaith et al., 1995), that assess inability to experience pleasure in response to normally rewarding stimuli, or measures of global PA (e.g., Profile of Mood States [POMS]-Vigor Scale; McNair, Lorr, & Droppleman, 1971; Positive and Negative Affect Schedule–Positive Affect Scale (PANAS-PA]; Watson et al., 1988) were included in the review of anhedonia and low PA–smoking associations. Studies using global measures of NA, such as the Positive and Negative Affect Schedule–Negative Affect Scale [PANAS-NA; Watson et al., 1988), as indicators of the nonspecific dimension of NA that cuts across anxiety and depression were included in the review of the NA–smoking relation. By contrast, investigations using a measure tapping only a single, narrow emotion within the global NA construct (e.g., irritability, anger, sadness) were not included. Studies utilizing measures of trait affect, recent (e.g., past week) affect, or current state affect were all included, given their theoretical relevance and to increase the breadth of the review.
The focus of this review was to shed light on the influence of tripartite affective dimensions on smoking. However, due to the paucity of research in this area, cross-sectional studies were included. Review of prospective studies was limited to investigations that assessed individual differences in affect at baseline and smoking at a later time point (rather than vice versa). Relatedly, studies exploring whether changes in affect or experimentally induced affect predict smoking behavior were omitted. Finally, inclusion was restricted to studies that evaluated relationships with direct markers of smoking behavior or dependence (i.e., smoking status, smoking heaviness and chronicity, nicotine dependence, cessation, and craving/urges). Studies examining other measures, such as smoking dependence motivation, acute nicotine effects, and tobacco withdrawal are of interest but are considered outside of the scope of this review.
Methodology
Articles were identified by inputting keywords in search databases (PSYCINFO, PubMed, Google Scholar, etc.). Although attempts to locate unpublished findings were not made, concerns regarding publication biases are diminished because the associations of interest to this review for many of the identified articles were reported in preliminary analyses of baseline characteristics (e.g., correlations between affective dimensions and cigarettes per day). Several quantitative (e.g., meta-analysis) and qualitative methods of analysis were considered. Because of the limited number of findings for most of the affect-smoking associations in the review, we ultimately decided on a qualitative approach in which the results of each study were summarized and integrated. Supplementary Table 1 reports the sample, affect measure, outcome variable, and findings of all studies included in the review.
Univariate Associations Between Affective Dimensions of the Tripartite Model and Smoking Variables
All findings reported in this section are results of analyses exploring the relationship between a single tripartite affective dimension and a smoking variable, without examining or adjusting for the concomitant influence of another affective dimension. Although the term “univariate” is used, some of the findings reported in this section are from analyses that statistically adjusted for nontripartite covariates (e.g., demographic characteristics).
Relations Between Low PA, Anhedonia, and Smoking Variables
Smoking Status
In a study of women (Pomerleau, Zucker, & Stewart, 2003), higher scores on the Center for Epidemiologic Studies Depression Scale–Positive Affect subscale (CESD-PA; Radloff, 1977), which measures reduced happiness and satisfaction with life, were significantly higher in current smokers compared to women who had never smoked. Additionally, women who had ever smoked had marginally significant lower PA compared to women who had never smoked (p < .10) (Pomerleau et al., 2003). These findings parallel results from a prior study in which anhedonia was associated with smoking status in a sample of young adults (McLeish et al., 2008). By contrast, Zvolensky, Kotov, Bonn-Miller, Schmidt, and Antipova (2008) did not find a relationship between anhedonia and smoking status. This discrepancy may be due to the fact that Zvolensky, Kotov, et al. (2008) examined this relationship in a sample of Russians, whereas the other study measuring anhedonia contained a sample of primarily Americans, suggesting that differences in origin of country may potentially alter the strength of the anhedonia–smoking status relationship. Due to the small number of studies, further research is needed to understand the relationship between low PA, anhedonia, and smoking status.
Nicotine Dependence
Findings regarding the relationship between severity of nicotine dependence, measured by the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991), and anhedonia and low PA are mixed. Self-report measures of anhedonia and FTND scores were not significantly associated in samples of college student smokers (Leventhal, Waters, et al., 2009), and community-dwelling adults participating in a laboratory study (Cook et al., 2007); however, other studies found a positive association between FTND and anhedonia in smokers who want to quit (McChargue & Cook, 2007; Zvolensky, Stewart, Vujanovic, Gavric, & Steeves, 2009). Additionally, Leventhal, Kahler, Ray, and Zimmerman (2009) found that psychiatric outpatients with current nicotine dependence were more likely to be rated as having clinically significant current anhedonia by a diagnostic interviewer when compared to those with past nicotine dependence and those with no nicotine dependence. Similar to these mixed findings of anhedonia, Doran et al. (2006) found that POMS-Vigor scores, a unique marker of global PA which measures activated positive mood states, were not associated with nicotine dependence. Similarly, a study of community-dwelling adults seeking treatment for smoking cessation found an association between CESD-PA scores and FTND (Leventhal, Ramsey, Brown, LaChance, & Kahler, 2008). By contrast, McChargue, Cohen, and Cook (2004) found an inverse association between FTND and both POMS-Vigor and PANAS-PA scores in college students. Given the discrepant findings across both samples and measures, additional research is required to elucidate the conditions, populations, and measures for which the anhedonia and low PA relationship with nicotine dependence may or may not exist.
Smoking Heaviness and Chronicity
There are multiple reports that both anhedonia and low PA are not associated with cigarettes per day in daily smokers (anhedonia: Cook et al., 2007; Johnson, Stewart, Zvolensky, & Steeves, 2009; Leventhal, Waters, et al., 2009; Zvolensky, Johnson, Leyro, Hogan, & Tursi, 2009; PA: Becona, Vazquez, Fuentes, & Lorenzo, 1999; Doran et al., 2006; Gregor, Zvolensky, Bernstein, Marshall, & Yartz, 2007; Leventhal et al., 2008), years as a smoker (anhedonia: Cook et al., 2007; Leventhal, Waters, et al., 2009; Zvolensky, Johnson, et al., 2009; PA: Gregor et al., 2007), or age of smoking onset (anhedonia: Leventhal, Waters, et al., 2009). These results are consistent across a variety of scales and a variety of populations (e.g., college students, treatment-seeking adults, non–treatment-seeking adults, and young adults).
Contrary to these findings, there are some reports of significant positive associations between both anhedonia and low PA and smoking heaviness and chronicity. A couple of studies found a positive association between anhedonia and cigarettes per day (Gregor et al., 2007; McLeish, Zvolensky, Bonn-Miller, & Bernstein, 2006) and years as a smoker (Gregor et al., 2007); however, the strength of these relationships is generally small (rs ≤ .18). Similarly, Wills, Sandy, Shinar, and Yaegar (1999) found that lower PA was associated with higher levels of smoking across all grades 7th through 10th and greater increases in smoking over time. Dvorak and Simons (2008) found that PA was negatively associated with past 6-month tobacco-use frequency. The different findings in these last two studies may be explained by their measures of smoking heaviness. Specifically, Wills et al. (1999) measured increase in smoking on a six-point Likert-type scale (1 = never tried, 6 = usually every day) and Dvorak and Simons (2008) measured past 6-month tobacco-use frequency on an eight-point Likert-type scale (1 = no use, 8 = more than once a day). The lowest categories on these measures then captured no use and the highest categories captured only daily smoking and did not account for average number of cigarettes per day beyond daily use. Accordingly, these findings may be more reflective of differences in smoking frequency among occasional smokers rather than smoking heaviness among daily smokers.
Cessation
Retrospective studies of the link between anhedonia and number of prior quit attempts are mixed, with one study showing a positive association (Leventhal, Waters, et al., 2009) and another showing no association (Zvolensky, Johnson, et al., 2009). There may, however, be a unique association between anhedonia and cessation attempts that end in rapid lapse. In a retrospective cross-sectional analysis, Leventhal, Waters, et al. (2009) found that anhedonia was positively associated with a higher proportion of quit attempts ending in rapid lapse (<24 hr). Similarly, a prospective study of self-quitters found that smokers who endorsed anhedonia prior to cessation maintained abstinence for a median of only 0.91 days before they lapsed, which was significantly shorter than those who did not report anhedonia who maintained abstinence for a median of 1.75 days (Niaura et al., 2001).
A prospective study of the link between anhedonia and lapse over a longer period of time found that low pre-quit PA (measured by CESD-PA scale) was associated with lower abstinence rates assessed at three time points (8, 16, 24 weeks) after target quit dates among heavy drinkers receiving cessation counseling and the nicotine patch (Leventhal et al., 2008). In a separate study of smokers participating in a placebo-controlled clinical trial testing fluoxetine for smoking cessation, those with lower precessation PA (i.e., POMS-Vigor scores) were more likely to be abstinent at weeks 1–4 after their target quit date but less likely to be abstinent at weeks 5–10 (Doran et al., 2006). It is important to note that Doran et al. (2006) found that fluoxetine (a medication that may increase positive mood) was effective in maintaining abstinence in those with low baseline PA but was not effective in maintaining abstinence in those with high PA. The use of fluoxetine in that study makes it difficult to compare to the other findings. Overall, these studies generally suggest that anhedonia is a predictor of poor smoking cessation outcome across multiple time points within the cessation process, and particular with rapid lapse. Studies suggest that low PA may be a negative prognostic factor for relapse later in a quit attempt, however, more research is needed to determine the precise role that low PA plays throughout the cessation process.
Craving/Urge
A recent cross-sectional study found that PA was negatively associated with smoking urge in nondeprived smokers (Leventhal, 2010). Similar to this finding of PA and urge, Cook, Spring, McChargue, and Hedeker (2004) found that higher anhedonia was related to greater increases in craving following 24 hr of tobacco deprivation but was not associated with changes in craving following 48 hr of deprivation. Extending these results, Leventhal, Waters, et al. (2009) found that smokers with higher anhedonia were more sensitive to the effects of 12 hr of tobacco deprivation on appetitive smoking urges (i.e., desire to smoke to enhance pleasure) but not aversive urges (i.e., desire to smoke to alleviate NA). These findings suggest that both low PA and anhedonia are associated with strong cigarette cravings, particularly during acute smoking abstinence, although more research is needed to clarify whether these processes play a role in the early relapse vulnerability found for anhedonia.
Relations between NA and Smoking Variables
Smoking Status
Past studies have found that current smokers and ex-smokers reported significantly higher NA than never-smokers among women (Pomerleau et al., 2003) and that NA was positively associated with smoking status in young adults (McLeish, Zvolensky, Marshall, & Leyro, 2009) and adolescents (Leen-Feldner et al., 2007). Additionally, Morissette, Brown, Kamholz, and Gulliver (2006) found that smokers with anxiety disorders reported significantly higher NA than non-smokers with anxiety disorders. Finally, the same study that found PA was not associated with smoking status in Russians also found that NA was not associated with smoking status (Zvolensky, Kotov, et al. 2008), further suggesting that differences in country of origin may influence the smoking status and affect relationship.
Nicotine Dependence
Results are mixed regarding the relationship between NA and nicotine dependence, with some studies fining modest-sized statistically significant positive associations (McChargue et al., 2004, Profile of Moods State–Negative Affect Scale [POMS-NA], r = .26; Zvolensky, Gibson, et al., 2008, r =.25) and others finding nonsignificant associations (McChargue et al., 2004, PANAS-NA, r = .09; Leventhal et al., 2008, r = .11). Unexpectedly, one study found that PANAS-NA scores demonstrated a significant inverse association with FTND (r = −.25) (Zvolensky et al., 2004).
Smoking Heaviness and Chronicity
Studies that have examined the link between NA and smoking heaviness have also found varying results. Several investigations have found small to moderate sized, statistically significant positive associations (rs < .33) between cigarettes per day and NA among adult residents of Spain (Becona et al., 1999), Moscow (Zvolensky, Kotov, Antipova, & Schmidt, 2003), and America (Gregor et al., 2007; Johnson et al., 2008; Zvolensky, Bonn-Miller, Bernstein, & Marshall, 2006; Zvolensky, Vujanovic, et al., 2007; Zvolensky, Bernstein, et al., 2007). In contrast, there are other reports of no significant association between cigarettes per day and NA (Gonzalez, Zvolensky, Vujanovic, Leyro, & Marshall, 2008; Gregor, Zvolensky, McLeish, Bernstein, & Morissette, 2008; Leventhal et al., 2008; Zvolensky et al., 2004; Zvolensky, Gonzalez, Bonn-Miller, Bernstein, & Goodwin, 2008).
Concerning tobacco use over time, Dvorak and Simons (2008) found that NA was positively related to past 6-month frequency of tobacco use and that non-smokers reported less NA relative to occasional smokers. Similarly, Wills et al. (1999) found that NA was positively related to higher initial levels of smoking and to more frequent tobacco use throughout adolescence (grades 7–10), when tobacco use was measured on a scale ranging from 1 to 6 (1 = never tried to 6 = usually every day). Although these studies suggest a relationship between NA and tobacco use over time, the highest categories on these measures capture only daily smoking and do not account for average number of cigarettes per day beyond daily use. Thus, more research on the NA–smoking relationship incorporating measures that account for average number of cigarettes per day beyond daily use is needed.
Cessation
A prospective study of smokers trying to quit found that higher pretreatment NA was associated with lower odds of abstinence following treatment (Leventhal et al., 2008). In cross-sectional studies of young adults who had made at least one previous quit attempt, NA and retrospective reports of early lapse propensity (i.e., inability to maintain abstinence for greater than 24 hr) were significantly associated in a sample of Mexican residents (Zvolensky, Bernstein, et al., 2007) but were not significantly associated in a sample of American residents (Zvolensky et al., 2006). More data are needed to clarify the populations and stages in the smoking cessation process in which NA may play a role.
Craving/Urge
A cross-sectional study of nondeprived smokers not interested in quitting found a positive association between NA and urge (Leventhal, 2010). More research is needed to identify whether this relationship can be replicated and extended to other conditions and populations.
Relations Between AA and Smoking Variables
Smoking Status
Smoking status is associated with AA across a variety of measures in adults (McLeish et al., 2008; Morisano, Bacher, Audrain-McGovern, & George, 2009; Williams et al., 1982) and adolescents (Leen-Feldner et al., 2007) and is also associated with fear of experiencing AA-related symptoms in young adults (McLeish et al., 2008) and in individuals with anxiety disorders (Morissette et al., 2006). However, similar to their findings regarding PA and NA, Zvolensky, Kotov, et al. (2008) found that AA was unrelated to smoking status in a Russian sample.
Nicotine Dependence
One study found that AA was positively related to measures of nicotine dependence (Zvolensky, Stewart, et al., 2009), whereas another study found that the tendency to fear the experience of AA-related symptoms was not related to measures of nicotine dependence (Zvolensky et al., 2004). Given the paucity of findings regarding this relationship, additional research is needed to clarify the link between AA and the fear of experiencing AA-related symptoms and nicotine dependence.
Smoking Heaviness and Chronicity
Except for two investigations demonstrating moderately sized significant associations (Johnson et al., 2009, r = .32; Zvolensky, Bernstein, et al., 2007, r = .30), most studies suggest that there is not a significant relationship between cigarettes per day and AA (Gregor et al., 2007; McLeish et al., 2006; Zvolensky, Johnson, et al., 2009; Zvolensky et al., 2003) or the fear of experiencing AA symptoms (Zvolensky et al., 2004, 2006). Similarly, studies have found no relationship between years as a smoker and AA (Gregor et al., 2007; Zvolensky, Johnson, et al., 2009). Thus, evidence tends to suggest that smoking heaviness and chronicity demonstrate little to moderate relation with AA and the fear of experiencing AA-related symptoms.
Cessation
Zvolensky, Johnson, et al. (2009) found that levels of AA were positively associated with number of past serious and unsuccessful quit attempts. In addition, Ladwig, Baumert, Lowel, Doring, and Wichmann (2005) found that active contemplators (participants who actively considered changes and recently made attempts to quit smoking) experienced more severe AA than immotives (participants who were unaware or completely unwilling to change smoking habits). Similar to PA, research suggests that fear of AA symptoms may play a unique role in rapid relapse. Specifically, in two retrospective studies of smokers who had made at least one previous quit attempt, those whose longest quit attempt lasted less than 1 day were more likely to report fear of AA symptoms compared to those whose longest quit attempt lasted more than one day (Zvolensky, Bernstein, et al., 2007; Zvolensky et al., 2006). In contrast, one study found that there were no differences in fear of AA symptoms between those whose longest quit attempt was longer than or equal to 7 days and those whose longest quit attempt was less than 7 days (Zvolensky, Feldner, Eifert, & Brown, 2001). These studies suggest that a relationship may exist between AA-related symptoms and sheer number of quit attempts and potentially between fear of experiencing AA-related symptoms and rapid relapse; however, additional research is needed on the link between AA and duration of quit attempts.
Craving/Urge
To the best of our knowledge, we are unaware of any published studies that have examined the relationship between AA or fear of experiencing AA-related symptoms and cigarette craving/urge.
Multivariate Associations Between Two or More Affective Dimensions of the Tripartite Model and Smoking Variables
There is an emerging literature that has examined the concomitant roles of two or more of the tripartite affective dimensions in smoking (see Supplementary Table 1, multivariate analyses). By exploring the influence of one dimension while statistically controlling for another dimension or by examining the interactive effects of two or more dimensions, a more detailed and sophisticated understanding of the affective underpinnings of smoking behavior can be elucidated.
There have been several investigations of the concomitant role of multiple affective dimensions in smoking status and heaviness. McLeish et al. (2009) found that smokers had higher levels of AA than non-smokers even when controlling for NA in a cross-sectional analysis of young adults. Furthermore, a significant interaction between NA and smoking status in predicting AA was reported, such that the extent to which smokers exhibited higher AA than non-smokers was relatively large among those who also had high NA. Among those with low NA, the corresponding differences in AA by smoking status were less prominent. In a separate cross-sectional study of affective predictors of smoking status, NA was associated with occasional (vs. no history) of tobacco use when controlling for PA and other affective variables; PA did not predict occasional use after controlling for NA (Dvorak & Simons, 2008). While neither PA nor NA predicted daily (vs. occasional) tobacco use, lower levels of PA were associated with daily (vs. no history) of tobacco use when controlling for NA, which did not predict daily use (Dvorak & Simons, 2008). In a study of 7th–12th graders, Wills et al. (1999) found that lower PA was associated with greater frequency of smoking after controlling for NA (which did not associate with smoking beyond variance accounted for by PA). A significant interaction was also reported such that the effects of low PA on smoking frequency were particularly strong among adolescents who also had higher levels of NA.
There have been a few studies examining the concomitant roles of multiple affective dimensions in cessation and other related outcomes. Leventhal, Waters, et al. (2009) found that after adjusting for NA, higher anhedonia was significantly associated with a greater number of previous quit attempts and a greater proportion of early relapses (in which abstinence could not be maintained for longer than 24 hr) but did not predict severity of nicotine dependence, cigarettes per day, and smoking chronicity. In addition, they found that after controlling for the influence of NA, smokers with higher anhedonia were more sensitive to the effects of 12 hr tobacco deprivation on appetitive smoking urges but not on aversive smoking urges. In a prospective study of smokers attempting to quit, lower levels of precessation PA significantly predicted reduced odds of abstinence after controlling for baseline NA and other affective variables; NA did not uniquely predict outcomes after accounting for variance overlapping with PA (Leventhal et al., 2008). Similarly, Zvolensky, Stewart, et al. (2009) found that precessation anhedonia was associated with lapse at Day 1 (after quit attempt) and relapse at Day 1, Day 7, and Day 14 (after quit attempt) above and beyond the influence of AA and other affective variables. In that study, AA did not significantly predict lapse or relapse at any time point after accounting for the effects of anhedonia and other variables. Taken together, these studies suggest that anhedonia and low PA play a particularly influential role in cigarette craving and cessation-related outcomes at multiple time points, above and beyond the influence of NA and AA.
In a similar vein, two retrospective studies of smokers who had made at least one previous quit attempt found that fear of experiencing AA-related symptoms was associated with rapid relapse (<1 day) after controlling for NA, whereas NA was not associated with rapid relapse after accounting for fear of AA symptoms (Zvolensky, Bernstein, et al., 2007; Zvolensky et al., 2006). More research using prospective designs is required to elucidate whether AA-related features are negative prognostic factors for smoking cessation outcomes.
Summary, Conclusions, and Future Directions
The purpose of this paper was to review and to integrate research that has examined associations between the affective dimensions of Watson and Clark's tripartite model of anxiety and depression and smoking variables. Generally, univariate studies suggested that all three of the tripartite dimensions consistently associated with smoking status. By contrast, the relationship of tripartite dimensions to nicotine dependence and smoking heaviness and chronicity among daily smokers was mixed, but more commonly showed modest or no relationship. This pattern could be interpreted as evidence that any type of affective disturbance may be a risk factor or consequence of smoking, regardless of the severity of smoking behavior. However, once daily tobacco use is established, individual differences in affective disturbance (of any type) may not be an influential factor on the severity of smoking behavior. Low PA and anhedonia evidenced consistent univariate relationships with difficulty maintaining abstinence and stronger craving in tobacco deprived and nondeprived smokers. More research is needed to clarify whether AA and NA are linked with cessation and craving.
Multivariate analyses suggest that the tripartite affective dimensions may have multiplicative (amplifying) effects on smoking behaviors, such that having emotional disturbance on multiple dimensions (i.e., high NA and low PA, Wills et al., 1999; high NA and high AA, McLeish et al., 2009) may result in disproportionate increases in smoking risk. Analyses of the unique versus overlapping effects of multiple affective dimensions tend to indicate that low PA and anhedonia are unique and robust risk factors for smoking status, relapse, and craving above and beyond other affective dimensions, whereas NA and AA were not consistently associated with smoking status or relapse after accounting for the influence of PA or anhedonia. Accordingly, low-PA or anhedonic individuals (especially those with concurrent NA or AA) should perhaps be targeted as a high-risk group in prevention and cessation interventions. Furthermore, given findings suggesting a unique relationship between low PA, anhedonia, and relapse, interventions which successfully raise PA and hedonic capacity following cessation may potentially be most effective at buffering relapse during cessation.
It is important to note that although low PA and anhedonia have overlapping features and are both specific to depression, these constructs also have distinct characteristics. Accordingly, anhedonia and PA may perhaps have a multifaceted impact on smoking involving both shared and discrete effects. Both anhedonic and low-PA smokers may share the tendency to smoke in order to increase global PA and counteract withdrawal-related reductions in PA (Leventhal et al., 2008; Leventhal, Waters, et al., 2009; Cook et al., 2007). By contrast, the propensity to use nicotine in order to enhance one's ability to respond more pleasurably to environmental rewards may be specific to anhedonic smokers (Cook et al., 2007) and potentially not present among low-PA smokers who are normally hedonic. These possible distinctions may be important for the development of prevention and cessation interventions as treatments may have to target slightly different areas (i.e., reduced global PA vs. inability to respond pleasurably to rewards) to be effective for the anhedonic individual versus the normally hedonic individual with low PA. However, future research is required to elucidate the types of interventions that could be deployed to target these underlying appetitive mechanisms.
Applying the tripartite model to understand the comorbidity of emotional disorders and smoking can shed light on the reasons why certain mental health disorders are associated with smoking. The documented pattern of univariate and multivariate findings in this review suggests that depressive disorders are related to certain aspects of smoking because of: (a) common variance shared by NA, low PA, and anhedonia (e.g., Leventhal et al., 2008); (b) specific variance in PA and anhedonia that is unique from NA (e.g., Leventhal et al., 2008; Zvolensky, Stewart, et al., 2009; Leventhal, Waters, et al., 2009); and (c) concomitant high NA and low PA, which multiplicatively increases smoking vulnerability (Wills et al., 1999). Thus, low PA and anhedonia (either alone or in combination with high NA) may perhaps underlie a significant portion of the link between depression and aspects of smoking behavior. Drawing conclusions about the reasons why anxiety disorders are associated with smoking is perhaps more difficult because of the heterogeneity of anxiety disorders (e.g., panic disorder vs. generalized anxiety disorder) and the lack of multivariate studies in the smoking literature that have explored the concomitant influence of AA and NA. Nonetheless, preliminary evidence suggests that individuals who experience symptoms or fear of AA and also have high NA may account for a significant portion of the relationship between anxiety and aspects of smoking behavior (McLeish et al., 2009; Zvolensky et al., 2006; Zvolensky, Bernstein, et al., 2007).
There are some limitations in the literature exploring the role of tripartite affective dimensions in smoking and the scope of this review. While studies of the univariate relations of affective dimensions to smoking are becoming more common, research examining relations to certain clinically relevant aspects of smoking behavior (e.g., craving, relapse) is limited and should be targeted in future research. Similarly, studies exploring the concomitant and interactive effects of multiple tripartite dimensions is rare but is nonetheless needed to tease apart the complex interplay of affective disturbance factors in smoking vulnerability. Furthermore, a large number of studies in this review were cross-sectional, which precludes definitive conclusions regarding the temporal features of these relationships and highlights the need for additional research using prospective designs. Additionally, the tripartite model is based on underlying traits that account for heterogeneity in affective disturbance. However, several of the studies included in the review used state measures collected at only one time point and thus may not be reflective of trait disturbances. Finally, although identifying which affective dimensions are linked with specific aspects of the tobacco dependence syndrome will shed light on the underpinnings of smoking behavior, exploration of biobehavioral mechanisms that mediate the influence of affect on smoking will ultimately be of greatest value. Such data are critical for advancing theory regarding the affective basis of tobacco dependence and guiding the development of more refined and effective interventions for smokers with affective disturbance.
Supplementary Material
Supplementary Table 1 can be found at Nicotine and Tobacco Research online (http://www.ntr.oxfordjournals.org/).
Funding
This research was supported, in part, by grant DA016184 awarded by the National Institutes of Health.
Declaration of Interests
None declared.
Supplementary Material
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL. Depression and the dynamics of smoking—A national perspective. JAMA. 1990;264:1541–1545. PMID:2395193. [PubMed] [Google Scholar]
- Baker LA, Cesa IL, Gatz M, Mellins C. Genetic and environmental-influences on positive and negative affect—Support for a 2-factor theory. Psychology and Aging. 1992;7:158–163. doi:10.1037/0882-7974.7.1.158. [PubMed] [Google Scholar]
- Becona E, Vazquez FL, Fuentes MJ, Lorenzo MD. Anxiety, affect, depression and cigarette consumption. Personality and Individual Differences. 1999;26:113–119. doi:10.1016/S0191-8869(98)00129-9. [Google Scholar]
- Breslau N. Psychiatric comorbidity of smoking and nicotine dependence. Behavior Genetics. 1995;25:95–101. doi: 10.1007/BF02196920. doi:10.1007/BF02196920. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kilbey M, Andreski P. Nicotine dependence, major depression, and anxiety in young adults. Archives of General Psychiatry. 1991;48:1069–1074. doi: 10.1001/archpsyc.1991.01810360033005. PMID:1845224. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kilbey MM, Andreski P. Nicotine dependence and major depression—New evidence from a prospective investigation. Archives of General Psychiatry. 1993;50:31–35. doi: 10.1001/archpsyc.1993.01820130033006. PMID:8422219. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kilbey MM, Andreski P. DSM-III-R nicotine dependence in young adults: Prevalence, correlates and associated psychiatric disorders. Addiction. 1994;89:743–754. doi: 10.1111/j.1360-0443.1994.tb00960.x. doi:10.1111/j.1360-0443.1994.tb00960.x. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P. Major depression and stages of smoking. A longitudinal investigation. Archives of General Psychiatry. 1998;55:161–166. doi: 10.1001/archpsyc.55.2.161. doi:10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- Brown M, Smits JA, Powers MB, Telch MJ. Differential sensitivity of the three ASI factors in predicting panic disorder patients’ subjective and behavioral response to hyperventilation challenge. Journal of Anxiety Disorders. 2003;17:583–591. doi: 10.1016/s0887-6185(02)00231-1. doi:10.1016/S0887-6185(02)00231-1. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Niaura R, Abrams DB, Sales SD, Ramsey SE, Miller IW. Cognitive-behavioral treatment for depression in smoking cessation. Journal of Consulting and Clinical Psychology. 2001;69:471–480. doi: 10.1037//0022-006x.69.3.471. doi:10.1037/0022-006X.69.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Niaura R, Lloyd-Richardson EE, Strong DR, Kahler CW, Abrantes AM, Miller IW. Bupropion and cognitive-behavioral treatment for depression in smoking cessation. Nicotine & Tobacco Research. 2007;9:721–730. doi: 10.1080/14622200701416955. doi:10.1080/14622200701416955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. doi:10.1080/14622200701416955. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression—Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. doi:10.1037/0021-843X.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cook JW, Spring B, McChargue D. Influence of nicotine on positive affect in anhedonic smokers. Psychopharmacology. 2007;192:87–95. doi: 10.1007/s00213-006-0688-5. doi:10.1007/s00213-006-0688-5. [DOI] [PubMed] [Google Scholar]
- Cook JW, Spring B, McChargue D, Hedeker D. Hedonic capacity, cigarette craving, and diminished positive mood. Nicotine & Tobacco Research. 2004;6:39–47. doi: 10.1080/14622200310001656849. doi:10.1080/14622200310001656849. [DOI] [PubMed] [Google Scholar]
- Covey LS. Tobacco cessation among patients with depression. Primary Care. 1999;26:691–706. doi: 10.1016/s0095-4543(05)70124-x. PMID:10436294. [DOI] [PubMed] [Google Scholar]
- Dahlstrom W, Welch G, Dahlstrom L. An MMPI handbook: Vol. I, clinical interpretation. Minneapolis, MN: University of Minnesota Press; 1972. [Google Scholar]
- Davidson RJ, Saron CD, Senulis JA, Ekman P, Friesen WV. Approach withdrawal and cerebral asymmetry—Emotional expression and brain physiology. Journal of Personality and Social Psychology. 1990;58:330–341. PMID:2319445. [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Chatterji S. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. doi:10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Doran N, Spring B, Borrelli B, McChargue D, Hitsman B, Niaura R, Hedeker D. Elevated positive mood: A mixed blessing for abstinence. Psychology of Addictive Behaviors. 2006;20:36–43. doi: 10.1037/0893-164X.20.1.36. doi:10.1037/0893-164x.20.1.36. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Simons JS. Affective differences among daily tobacco users, occasional users, and non-users. Addictive Behaviors. 2008;33:211–216. doi: 10.1016/j.addbeh.2007.09.003. doi:10.1016/j.addbeh.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: The schedule for affective disorders and schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. PMID:678037. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Clark DC, Scheftner WA, Gibbons RD. Assessing anhedonia in psychiatric patients. Archives of General Psychiatry. 1983;40:79–84. doi: 10.1001/archpsyc.1983.01790010081010. PMID:6849623. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-IV (SCID) Washington, DC: American Psychiatric Association; 1997. [Google Scholar]
- Franken IH, Rassin E, Muris P. The assessment of anhedonia in clinical and non-clinical populations: Further validation of the Snaith-Hamilton Pleasure Scale (SHAPS) Journal of Affective Disorders. 2007;99:83–89. doi: 10.1016/j.jad.2006.08.020. doi:10.1016/j.jad.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Ginsberg D, Hall SM, Reus VI, Munoz RF. Mood and depression diagnosis in smoking cessation. Experimental and Clinical Psychopharmacology. 1995;3:389–395. doi:10.1037/1064-1297.3.4.389. [Google Scholar]
- Glassman AH, Stetner F, Walsh BT, Raizman PS, Fleiss JL, Cooper TB, Covey LS. Heavy smokers, smoking cessation, and clonidine. Results of a double-blind, randomized trial. JAMA. 1988;259:2863–2866. PMID:3367452. [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, Marshall EC. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. Journal of Psychiatric Research. 2008;43:138–147. doi: 10.1016/j.jpsychires.2008.03.002. doi:10.1016/j.jpsychires.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. doi:10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Gregor K, Zvolensky MJ, Bernstein A, Marshall EC, Yartz AR. Smoking motives in the prediction of affective vulnerability among young adult daily smokers. Behaviour Research and Therapy. 2007;45:471–482. doi: 10.1016/j.brat.2006.03.019. doi:10.1016/j.brat.2006.03.019. [DOI] [PubMed] [Google Scholar]
- Gregor KL, Zvolensky MJ, McLeish AC, Bernstein A, Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: Associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine & Tobacco Research. 2008;10:627–635. doi: 10.1080/14622200801978706. doi:10.1080/14622200801978706. [DOI] [PubMed] [Google Scholar]
- Haas AL, Munoz RF, Humfleet GL, Reus VI, Hall SM. Influences of mood, depression history, and treatment modality on outcomes in smoking cessation. Journal of Consulting and Clinical Psychology. 2004;72:563–570. doi: 10.1037/0022-006X.72.4.563. doi:10.1037/0022-006x.72.4.563. [DOI] [PubMed] [Google Scholar]
- Hall SM, Humfleet GL, Reus VI, Munoz RF, Hartz DT, Maude-Griffin R. Psychological intervention and antidepressant treatment in smoking cessation. Archives of General Psychiatry. 2002;59:930–936. doi: 10.1001/archpsyc.59.10.930. doi:10.1001/archpsyc.59.10.930. [DOI] [PubMed] [Google Scholar]
- Hall SM, Reus VI, Munoz RF, Sees KL, Humfleet G, Hartz DT, Triffleman E. Nortriptyline and cognitive-behavioral therapy in the treatment of cigarette smoking. Archives of General Psychiatry. 1998;55:683–690. doi: 10.1001/archpsyc.55.8.683. doi:10.1001/archpsyc.55.8.683. [DOI] [PubMed] [Google Scholar]
- Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacology. 2004;29:1765–1781. doi: 10.1038/sj.npp.1300506. doi:10.1038/sj.npp.1300506. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. doi:10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Johnson KA, Stewart SH, Zvolensky MJ, Steeves D. Evaluating the mediating role of coping-based smoking motives among treatment-seeking adult smokers. Nicotine & Tobacco Research. 2009;11:1296–1303. doi: 10.1093/ntr/ntp134. doi:10.1093/Ntr/Ntp134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KA, Zvolensky MJ, Marshall EC, Gonzalez A, Abrams K, Vujanovic AA. Linkages between cigarette smoking outcome expectancies and negative emotional vulnerability. Addictive Behaviors. 2008;33:1416–1424. doi: 10.1016/j.addbeh.2008.05.001. doi:10.1016/j.addbeh.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Jr., Steer RA, Beck AT, Schmidt NB, Rudd MD, Catanzaro SJ. Physiological hyperarousal: Construct validity of a central aspect of the tripartite model of depression and anxiety. Journal of Abnormal Psychology. 1999;108:290–298. doi: 10.1037//0021-843x.108.2.290. doi:10.1037/0021-843X.108.2.290. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Huang FY, Davies M. Comorbidity between patterns of substance use dependence and psychiatric syndromes. Drug and Alcohol Dependence. 2001;64:233–241. doi: 10.1016/s0376-8716(01)00126-0. doi:10.1016/S0376-8716(01)00126-0. [DOI] [PubMed] [Google Scholar]
- Keogh E, Reidy J. Exploring the factor structure of the Mood and Anxiety Symptom Questionnaire (MASQ) Journal of Personality Assessment. 2000;74:106–125. doi: 10.1207/S15327752JPA740108. doi:10.1207/S15327752JPA740108. [DOI] [PubMed] [Google Scholar]
- Ladwig KH, Baumert J, Lowel H, Doring A, Wichmann HE. Contemplating to quit current smoking status: Differences in behavioural and psychosocial patterns in a population-based cohort of current smokers. Preventive Medicine. 2005;41:134–140. doi: 10.1016/j.ypmed.2004.10.017. doi:10.1016/j.ypmed.2004.10.017. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. doi:10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Zvolensky MJ, van Lent J, Vujanovic AA, Bleau T, Bernstein A, Feldner MT. Anxiety sensitivity moderates relations among tobacco smoking, panic attack symptoms, and bodily complaints in adolescents. Journal of Psychopathology and Behavioral Assessment. 2007;29:69–79. doi:10.1007/s10862-006-9028-7. [Google Scholar]
- Lerman C, Audrain J, Orleans CT, Boyd R, Gold K, Main D, Caporaso N. Investigation of mechanisms linking depressed mood to nicotine dependence. Addictive Behaviors. 1996;21:9–19. doi: 10.1016/0306-4603(95)00032-1. doi:10.1016/0306-4603(95)00032-1. [DOI] [PubMed] [Google Scholar]
- Leventhal AM. Do individual differences in reinforcement smoking moderate the relationship between affect and urge to smoke? Behavioral Medicine. 2010;36:1–6. doi: 10.1080/08964280903521347. doi:10.1080/08964280903521347. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Chasson GS, Tapia E, Miller EK, Pettit JW. Measuring hedonic capacity in depression: A psychometric analysis of three anhedonia scales. Journal of Clinical Psychology. 2006;62:1545–1558. doi: 10.1002/jclp.20327. doi:10.1002/Jclp.20327. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Kahler CW, Ray LA, Zimmerman M. Refining the depression-nicotine dependence link: Patterns of depressive symptoms in psychiatric outpatients with current, past, and no history of nicotine dependence. Addictive Behaviors. 2009;34:297–303. doi: 10.1016/j.addbeh.2008.11.008. doi:10.1016/j.addbeh.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Ramsey SE, Brown RA, LaChance HR, Kahler CW. Dimensions of depressive symptoms and smoking cessation. Nicotine & Tobacco Research. 2008;10:507–517. doi: 10.1080/14622200801901971. doi:10.1080/14622200801901971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Waters AJ, Kahler CW, Ray LA, Sussman S. Relations between anhedonia and smoking motivation. Nicotine & Tobacco Research. 2009;11:1047–1054. doi: 10.1093/ntr/ntp098. doi:10.1093/Ntr/Ntp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longley SL, Watson D, Noyes R, Jr., Yoder K. Panic and phobic anxiety: Associations among neuroticism, physiological hyperarousal, anxiety sensitivity, and three phobias. Journal of Anxiety Disorders. 2006;20:718–739. doi: 10.1016/j.janxdis.2005.11.005. doi:10.1016/j.janxdis.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Roepke SK, Depp CA, Patterson TL, Grant I. Specificity of cognitive and behavioral variables to Positive and Negative Affect. Behaviour Research and Therapy. 2009;47:608–615. doi: 10.1016/j.brat.2009.04.006. doi:10.1016/j.brat.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McChargue DE, Cohen LM, Cook JW. The influence of personality and affect on nicotine dependence among male college students. Nicotine & Tobacco Research. 2004;6:287–294. doi: 10.1080/14622200410001676323. doi:10.1080/14622200410001676323. [DOI] [PubMed] [Google Scholar]
- McChargue DE, Cook JW. Depression vulnerability within smoking research: How accurate are one-item screening items? Addictive Behaviors. 2007;32:404–409. doi: 10.1016/j.addbeh.2006.05.006. doi:10.1016/j.addbeh.2006.05.006. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, Bonn-Miller MO, Bernstein A. Perceived health moderates the association between smoking rate and panic vulnerability variables among daily smokers. Depression and Anxiety. 2006;23:257–265. doi: 10.1002/da.20170. doi:10.1002/Da.20170. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, Marshall EC, Leyro TM. Negative affectivity as a moderator of the association between smoking status and anxiety sensitivity, anxiety symptoms, and perceived health among young adults. Journal of Nervous and Mental Disease. 2009;197:111–116. doi: 10.1097/NMD.0b013e3181961683. doi:10.1097/Nmd.0b013e3181961683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, Yartz AR, Leyro TM. Anxiety sensitivity as a moderator of the association between smoking status and anxiety symptoms and bodily vigilance: Replication and extension in a young adult sample. Addictive Behaviors. 2008;33:315–327. doi: 10.1016/j.addbeh.2007.09.018. doi:10.1016/j.addbeh.2007.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Profile of mood states manual. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- Morisano D, Bacher I, Audrain-McGovern J, George TP. Mechanisms underlying the comorbidity of tobacco use in mental health and addictive disorders. Canadian Journal of Psychiatry. 2009;54:356–367. doi: 10.1177/070674370905400603. PMID:19527556. [DOI] [PubMed] [Google Scholar]
- Morissette SB, Brown TA, Kamholz BW, Gulliver SB. Differences between smokers and nonsmokers with anxiety disorders. Journal of Anxiety Disorders. 2006;20:597–613. doi: 10.1016/j.janxdis.2005.08.003. doi:10.1016/j.janxdis.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Morrell HER, Cohen LM. Cigarette smoking, anxiety, and depression. Journal of Psychopathology and Behavioral Assessment. 2006;28:281–295. doi:10.1007/s10862-005-9011-8. [Google Scholar]
- Niaura R, Britt DM, Shadel WG, Goldstein M, Abrams D, Brown R. Symptoms of depression and survival experience among three samples of smokers trying to quit. Psychology of Addictive Behaviors. 2001;15:13–17. doi: 10.1037/0893-164x.15.1.13. doi:10.1037/0893-164X.15.1.13. [DOI] [PubMed] [Google Scholar]
- Nitschke JB, Heller W, Imig JC, McDonald RP, Miller GA. Distinguishing dimensions of anxiety and depression. Cognitive Therapy and Research. 2001;25:1–22. doi:10.1023/A:1026485530405. [Google Scholar]
- Orlando M, Ellickson PL, Jinnett K. The temporal relationship between emotional distress and cigarette smoking during adolescence and young adulthood. Journal of Consulting and Clinical Psychology. 2001;69:959–970. doi: 10.1037//0022-006x.69.6.959. doi:10.1037//0022-006x.69.6.959. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Zucker AN, Stewart AJ. Patterns of depressive symptomatology in women smokers, ex-smokers, and never-smokers. Addictive Behaviors. 2003;28:575–582. doi: 10.1016/s0306-4603(01)00257-x. doi:10.1016/S0306-4603(01)00257-X. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Ree MJ, French D, MacLeod C, Locke V. Distinguishing cognitive and somatic dimensions of state and trait anxiety: Development and validation of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA) Behavioural and Cognitive Psychotherapy. 2008;36:313–332. doi:10.1017/S1352465808004232. [Google Scholar]
- Reiss S. Theoretical perspectives on the fear of anxiety. Clinical Psychology Review. 1987;7:585–596. doi:10.1016/0272-7358(87)90007-9. [Google Scholar]
- Reiss S, McNally RJ. The expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. New York: Academic Press; 1985. pp. 107–122. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, Mcnally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. doi:10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Rohde P, Kahler CW, Lewinsohn PM, Brown RA. Psychiatric disorders, familial factors, and cigarette smoking: II. Associations with progression to daily smoking. Nicotine & Tobacco Research. 2004;6:119–132. doi: 10.1080/14622200310001656948. doi:10.1080/14622200310001656948. [DOI] [PubMed] [Google Scholar]
- Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. Journal of Clinical Psychology. 2006;62:123–146. doi: 10.1002/jclp.20213. doi:10.1002/Jclp.20213. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Tsuang MT. Panic and phobic anxiety: Defining phenotypes for genetic studies. American Journal of Psychiatry. 1998;155:1152–1162. doi: 10.1176/ajp.155.9.1152. PMID:9734536. [DOI] [PubMed] [Google Scholar]
- Snaith P. Measuring anxiety and depression. Practitioner. 1993;237:554. PMID:8415387. [PubMed] [Google Scholar]
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A Scale for the Assessment of Hedonic Tone—the Snaith-Hamilton Pleasure Scale. British Journal of Psychiatry. 1995;167:99–103. doi: 10.1192/bjp.167.1.99. PMID:7551619. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Measurement and mismeasurement of mood: Recurrent and emergent issues. Journal of Personality Assessment. 1997;68:267–296. doi: 10.1207/s15327752jpa6802_4. doi:10.1207/s15327752jpa6802_4. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of Brief Measures of Positive and Negative Affect—the PANAS Scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi:10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS. Testing a tripartite model. 2. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. doi:10.1037/0021-843X.104.1.15. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, Mccormick RA. Testing a tripartite model .1. Evaluating the convergent and discriminant validity of Anxiety and Depression Symptom Scales. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. PMID:7897050. [DOI] [PubMed] [Google Scholar]
- Williams SG, Hudson A, Redd C. Cigarette-smoking, manifest anxiety and somatic symptoms. Addictive Behaviors. 1982;7:427–428. doi: 10.1016/0306-4603(82)90013-2. doi:10.1016/0306-4603(82)90013-2. [DOI] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Shinar O, Yaeger A. Contributions of positive and negative affect to adolescent substance use: Test of a bidimensional model in a longitudinal study. Psychology of Addictive Behaviors. 1999;13:327–338. doi:10.1037/0893-164X.13.4.327. [Google Scholar]
- Wilson K, Gullone E, Moss S. The youth version of the Positive and Negative Affect Schedule: A psychometric validation. Behaviour Change. 1998;15:187–193. Accession number: 1998-03269-005. [Google Scholar]
- World Health Organization. WHO report on the global tobacco epidemic, 2009: Implementing smoke-free environments. Belley, France: Imprimerie Nouvelle Gonnet; 2009. [Google Scholar]
- Zerssen Dv. Die Beschwerden-Liste. Klinische Selbstbeurteilungsfragebfgen aus dem Mqnchner Psychiatrischen Informationssystem. Psychis-Manuale, Allgemeiner Teil. Weinheim, Germany: Beltz; 1976. [Google Scholar]
- Zinbarg RE, Brown TA, Barlow DH, Rapee RM. Anxiety sensitivity, panic, and depressed mood: A reanalysis teasing apart the contributions of the two levels in the hierarchical structure of the Anxiety Sensitivity Index. Journal of Abnormal Psychology. 2001;110:372–377. doi: 10.1037//0021-843x.110.3.372. doi:10.1037/0021-843X.110.3.372. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Cardenas SJ, Colotla VA, Marshall EC, Feldner MT. Anxiety sensitivity and early relapse to smoking: A test among Mexican daily, low-level smokers. Nicotine & Tobacco Research. 2007;9:483–491. doi: 10.1080/14622200701239621. doi:10.1080/14622200701239621. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bonn-Miller M, Bernstein A, Marshall E. Anxiety sensitivity and abstinence duration to smoking. Journal of Mental Health. 2006;15:659–670. doi:10.1016/j.addbeh.2005.05.027. [Google Scholar]
- Zvolensky MJ, Feldner MT, Eifert GH, Brown RA. Affective style among smokers—Understanding anxiety sensitivity, emotional reactivity, and distress tolerance using biological challenge. Addictive Behaviors. 2001;26:901–915. doi: 10.1016/s0306-4603(01)00242-8. doi:10.1016/S0306-4603(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, Gregor K. Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research. 2004;28:473–486. doi:10.1023/B:COTR.0000045559.73958.89. [Google Scholar]
- Zvolensky MJ, Gibson LE, Vujanovic AA, Gregor K, Bernstein A, Kahler C, Feldner MT. Impact of posttraumatic stress disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine & Tobacco Research. 2008;10:1415–1427. doi: 10.1080/14622200802238951. doi:10.1080/14622200802238951. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Gonzalez A, Bonn-Miller MO, Bernstein A, Goodwin RD. Negative reinforcement/negative affect reduction cigarette smoking outcome expectancies: Incremental validity for anxiety focused on bodily sensations and panic attack symptoms among daily smokers. Experimental and Clinical Psychopharmacology. 2008;16:66–76. doi: 10.1037/1064-1297.16.1.66. doi:10.1037/1064-1297.16.1.66. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Johnson KA, Leyro TM, Hogan J, Tursi L. Quit-attempt history: Relation to current levels of emotional vulnerability among adult cigarette users. Journal of Studies on Alcohol and Drugs. 2009;70:551–554. doi: 10.15288/jsad.2009.70.551. PMID:19515295. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Cross cultural evaluation of smokers risk for panic and anxiety pathology: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2003;41:1199–1215. doi: 10.1016/s0005-7967(03)00031-7. doi:10.1016/S0005-7967(03)00031-7. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Bonn-Miller MO, Schmidt NB, Antipova AV. Anxiety sensitivity as a moderator of association between smoking status and panic-related processes in a representative sample of adults. Journal of Psychiatric Research. 2008;42:69–77. doi: 10.1016/j.jpsychires.2006.09.012. doi:10.1016/j.jpsychires.2006.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine & Tobacco Research. 2009;11:323–331. doi: 10.1093/ntr/ntn037. doi:10.1093/Ntr/Ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Miller MOB, Bernstein A, Yartz AR, Gregor KL, Gibson LE. Incremental validity of anxiety sensitivity in terms of motivation to quit, reasons for quitting, and barriers to quitting among community-recruited daily smokers. Nicotine & Tobacco Research. 2007;9:965–975. doi: 10.1080/14622200701540812. doi:10.1080/14622200701540812. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.