Abstract
Lowe syndrome is a rare genetic disease that appears to cause various clinical symptoms involving the eye, nervous system, and kidney. While a mutation of the OCRL1 gene is known to be responsible for this syndrome, the exact pathophysiology remains unclear. Various multi-organ symptoms are characteristic of Lowe syndrome, but skin lesions have rarely been described. Recently, mechanisms for the association of Lowe syndrome and skin lesions have been proposed. We report this case of Lowe syndrome involving multiple epidermal cysts on the scalp in a 6-year-old male child.
Keywords: Epidermal cyst, Lowe syndrome
INTRODUCTION
Lowe syndrome, also known as oculocerebrorenal syndrome, is a rare X-linked recessive disorder that was first described by Lowe in 19521. It is clinically characterized by congenital cataract, mental retardation, and proximal renal tubular dysfunction2. The main cause of Lowe syndrome is mutation of the oculocerebrorenal-low protein (OCRL1) gene on the Xq26 chromosome. It causes deficiency of phosphatidylinositol 4,5-bisphosphate [PtdIns(4,5)P2] 5-phosphatase, an enzyme located in the Golgi apparatus. As a result, dysregulation of this enzyme causes multi-organ damage involving the eye, nervous system, and kidney3.
The association between skin lesions and Lowe syndrome is currently poorly understood. Furthermore, while cyst formation is not currently recognized as a clinical feature of Lowe syndrome, some clinicians have recently suggested that mutation of the OCRL1 gene also elicits cyst formation4,5. We report here the first case of multiple epidermal cysts associated with Lowe syndrome in the Korean dermatologic literature.
CASE REPORT
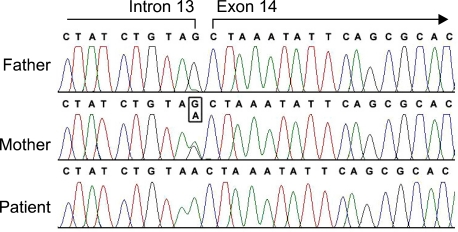
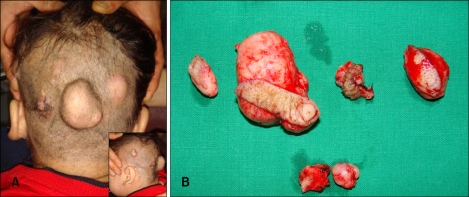
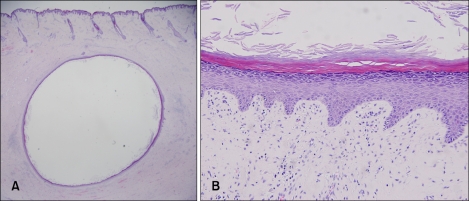
A 6-year-old male child with Lowe syndrome was brought to our clinic by his mother for evaluation and treatment of multiple asymptomatic cystic masses on the temporal and occipital scalp. He suffered from bilateral congenital cataracts, proximal renal tubulopathy (Fanconi type), seizures, cryptorchism, generalized hypotonia, and developmental delay. Direct sequencing of the OCRL1 gene revealed a splice site mutation in exon 14 and his mother was a heterozygous carrier (Fig. 1). Cystic masses on the scalp had developed approximately six months previously and had slowly enlarged recently. In his scalp area, there was no trauma history and he was not in a completely bedridden state. Physical examination revealed variously sized (approximately 1~4 cm diameter), skin colored, deep seated, soft, cystic masses on the temporal and occipital scalp (Fig. 2A). The masses were not associated with tenderness to palpation or bleeding. Some of them were completely excised for an exact diagnosis and to prevent secondary complications (Fig. 2B). Histological examination revealed each cyst to be lined by true epidermis composed of several layers of stratified squamous epithelium and a granular layer, and to contain keratinous materials arranged in laminated layers (Fig. 3). There were other small sized cysts, but his mother did not want further treatment for them.
Fig. 1.
Direct sequencing of OCRL1 gene of this patient disclosed a splice site mutation in exon 14 (IVS13-1G>A), and his mother was a heterozygous carrier.
Fig. 2.
(A) Multiple, skin colored, deep seated cystic masses on the temporal and occipital scalp. (B) Intraoperative gross view of excised cysts.
Fig. 3.
(A) The cyst was lined by thin walls and contained keratinous materials (H&E, ×12.5). (B) The cystic walls were composed of several layers of stratified squamous epithelium with a granular layer and the cyst contained keratinous materials arranged in laminated layers (H&E, ×200).
DISCUSSION
Lowe syndrome, also known as oculocerebrorenal syndrome, is a rare X-linked recessive disorder that is typically affects the eye, nervous system, and kidney1. Its estimated prevalence is about 1 in 500,000 and it occurs mainly in male children; female cases are extremely rare6. In Lowe syndrome, the OCRL1 gene on the Xq26 chromosome is mutated and causes deficiency of phosphatidylinositol 4,5-bisphosphate [PtdIns(4,5)P2] 5-phosphatase, an enzyme located in the Golgi apparatus. Simultaneous accumulation of its precursor phosphatidylinositol 4,5-bisphosphate 5-phosphate also occurs. While such dysregulation of the Golgi apparatus is generally accepted to be causative of Lowe syndrome, a widely accepted unifying hypothesis explaining the various clinical symptoms has yet to be reached1,3,7.
Lowe syndrome appears to have various clinical symptoms and it affects multiple organs such as the eye, nervous system, and kidney. At birth, congenital cataract is the most common finding, with other ocular diseases such as glaucoma, corneal cheloid, corneal opacity, nystagmus, and amblyopia also seen3,8,9. In the nervous system, neonatal hypotonia and loss or decrease of deep tendon reflexes are frequent initial symptoms with motor development retardation, mental retardation, seizures and growth and development delays also reported1,10. Renal tubular dysfunction (Fanconi-type) is characteristic, with proteinuria, aminoaciduria, phosphaturia, hypercalciuria, hypophosphatemia and metabolic acidosis associated with worse disease severity. Nephrocalcinosis, nephrolithiasis, loss of glomerular filtration, focal fibrosis and hypertrophy of basement membrane are also seen and continued deterioration of renal function eventually leads to renal failure1,11. Additionally, protean features such as frontal bossing, deep-set eyes, and chubby cheeks commonly occur, with accompanying cryptorchism and skeletal anomalies such as rickets and pathologic fracture also possible1,12.
Recently, much research has been conducted regarding Lowe syndrome. However, there has been comparatively little research regarding the associated skin lesions. To our knowledge, there are only three published reports in the English literature about the skin lesions associated with Lowe syndrome4,5,13, and there are none in the Korean literature. Nandedkar et al.4 reported a case of Lowe syndrome with eruptive vellus hair cyst. Erdogan et al.5 reported a case of accompanying trichoepithelioma, and Batirbaygil and Turgut13 reported a case consisting of multiple eruption cysts in the oral cavity and hematoma formation. Nandedkar et al.4 found that abnormally high level of extracellular lysosomal enzymes, leaving these enzymes free to cause tissue destruction. Therefore they suggested that cyst formation is a result of localized reaction intended to wall off the destructive enzymes. It means that loss of cellular control caused by accumulation of phosphatidylinositol 4,5-bisphosphate 5-phosphate and extracellular release of lysosomal enzymes cause cystic lesions to prevent enzyme accumulation and subsequent tissue damage.
Our case is easily differentiated from Gardner syndrome which is also associated with multiple epidermal cysts. The cysts of Gardner syndrome are usually accompanied by various cutaneous lesions, osteomas, and intestinal polyposis. Moreover, Gardner syndrome is an autosomal-dominant disease with a known mutation in the APC gene located at chromosome 5q21.
The precise etiology of the cystic lesions associated with Lowe syndrome remains uncertain. It may be that the lesions are coincidental rather than secondary to biochemical changes induced by Lowe syndrome. Thus, further reports and large scale research on the dermatologic findings of Lowe syndrome are necessary.
References
- 1.Lowe CU, Terrey M, MacLachan EA. Organic aciduria, decreased renal ammonia production, hydrophthalmos and mental retardation; a clinical entity. AMA Am J Dis Child. 1952;83:164–184. doi: 10.1001/archpedi.1952.02040060030004. [DOI] [PubMed] [Google Scholar]
- 2.Loi M. Lowe syndrome. Orphanet J Rare Dis. 2006;1:16. doi: 10.1186/1750-1172-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suchy SF, Olivos-Glander IM, Nussabaum RL. Lowe syndrome, a deficiency of phosphatidylinositol 4,5-bisphosphate 5-phosphatase in the Golgi apparatus. Hum Mol Genet. 1995;4:2245–2250. doi: 10.1093/hmg/4.12.2245. [DOI] [PubMed] [Google Scholar]
- 4.Nandedkar MA, Minus H, Nandedkar MA. Eruptive vellus hair cysts in a patient with Lowe syndrome. Pediatr Dermatol. 2004;21:54–57. doi: 10.1111/j.0736-8046.2004.21112.x. [DOI] [PubMed] [Google Scholar]
- 5.Erdogan F, Ismailogullari S, Soyuer I, Ferahbas A, Poyrazoglu H. Different seizure types and skin lesions in oculocerebrorenal syndrome of Lowe. J Child Neurol. 2007;22:427–431. doi: 10.1177/0883073807301928. [DOI] [PubMed] [Google Scholar]
- 6.Mueller OT, Hartsfield JK, Jr, Gallardo LA, Essig YP, Miller KL, Papenhausen PR, et al. Lowe oculocerebrorenal syndrome in a female with a balanced X;20 translocation: mapping of the X chromosome breakpoint. Am J Hum Genet. 1991;49:804–810. [PMC free article] [PubMed] [Google Scholar]
- 7.Lichter-Konecki U, Farber LW, Cronin JS, Suchy SF, Nussbaum RL. The effect of missense mutations in the RhoGAP-homology domain on ocrl1 function. Mol Genet Metab. 2006;89:121–128. doi: 10.1016/j.ymgme.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Suk KW, Lee SJ, Kim WS. Two cases of oculocerebrorenal syndrome in two brothers diagnosed after congenital cataract surgery. J Korean Ophthalmol Soc. 2006;47:1502–1511. [Google Scholar]
- 9.Walton DS, Katsavounidou G, Lowe CU. Glaucoma with the oculocerebrorenal syndrome of Lowe. J Glaucoma. 2005;14:181–185. doi: 10.1097/01.ijg.0000158850.07732.05. [DOI] [PubMed] [Google Scholar]
- 10.Choi BS, Lee YJ, Park SE, Nam SO. Two cases of Lowe syndrome. J Korean Child Neurol Soc. 2002;10:374–377. [Google Scholar]
- 11.Cho HY, Lee BH, Choi HJ, Ha IS, Choi Y, Cheong HI. Renal manifestations of Dent disease and Lowe syndrome. Pediatr Nephrol. 2008;23:243–249. doi: 10.1007/s00467-007-0686-9. [DOI] [PubMed] [Google Scholar]
- 12.Kim SW, Yu YS, Kim IO, Cheong HI, Hwang YS, Choi Y. Two cases of oculocerebrorenal syndrome of Lowe. J Korean Pediatr Soc. 1999;42:419–423. [Google Scholar]
- 13.Batirbaygil Y, Turgut M. Lowe syndrome: case report. J Clin Pediatr Dent. 1999;23:357–359. [PubMed] [Google Scholar]