Abstract
Background
Chronic daily headache is a major healthcare problem, with significant resource implications for specialist services. Since 1999, GPs in Greater Glasgow have had direct access to computerised tomography (CT) for investigation of chronic daily headache.
Aim
The purpose of this study is to assess the significance of pathology, impact of the service, and GP satisfaction.
Method
The direct-access CT findings in patients between 1999 and 2007 were reviewed. Radiological reports were reviewed for abnormal findings by a radiologist. A neurologist reviewed those cases with abnormalities to assess their potential causation in presenting symptoms. A questionnaire was sent to the referring GP for every patient referred for direct-access CT. Data from the Information Services Division of NHS National Services Scotland was used to estimate potential cost benefits.
Results
A total of 4404 CT scans were performed. Abnormal findings were reported in 461 (10.5%), and the reported abnormalities were considered a potential causative factor for the presenting symptoms in 60 patients (1.4%). Other abnormalities mostly resulted from established cerebrovascular disease and atrophy; 986 GP questionnaires were analysed. The major body of GP opinion (n = 460, 47%) indicated that direct-access CT was their preferred choice for referral of chronic daily headache. If direct-access CT was not available, neurology (n = 448, 45%) and general medicine (n = 379, 38%) would be the commonest referral choices. This study also reveals that 86% did not require further specialist referral. Projecting the GP questionnaire data to the study group gave an approximate cost saving of at least £86 681.81.
Conclusion
Direct-access CT is now the preferred choice of management for patients with chronic daily headache in primary care. Patients and GPs are reassured by a normal scan in the majority of cases. There may be cost savings, although confirmation of cost-effectiveness would require further study.
Keywords: cephalalgia; chronic daily headache; computerised tomography, X-ray; CT scan; general practitioners; patients
INTRODUCTION
Chronic daily headache (headache for ≥15 days per month for longer than 3 months) is a common and potentially disabling condition,1 affecting up to 5% of the population,2,3 This presents a major healthcare problem with significant resource implications for specialist services. While symptoms commonly result from non-structural causes, they may occasionally be due to sinister pathology such as a brain tumour.4 These potential diagnoses can lead to significant anxiety in many patients.5,6 Since 1999, GPs in Greater Glasgow have had direct access to computerised tomography (CT) for investigation of chronic headache. There has been recent government interest in GP direct-access scanning, with an announcement that all patients with suspected cancer are to undergo diagnostic imaging within 1 week by 2014.7 Previously published studies of direct-access CT only determined the incidence of pathology in primary-care-access neuroimaging.8,9 The purpose of this study was to assess the rate and significance of pathology on brain CT in patients presenting to primary healthcare physicians with chronic headache, to assess the outcomes and impact of the service on specialist referrals, to assess potential cost benefits of direct-access CT, nd to assess GP satisfaction with the service.
How this fits in.
Chronic daily headache is a common and disabling condition. GP direct access to computerised tomography (CT) in Greater Glasgow allows faster access to neuroimaging for this group of patients. Previous studies have examined the incidence of pathology in these patients. This study looks not only at rates of pathology but at the resource implications and GP satisfaction with the service. The study found a similar incidence of pathology as previously described but demonstrate GP and patient satisfaction with the service and potential resource and financial savings.
METHOD
A database was used to identify all patients who had been referred for a head CT directly from primary care between February 1999 and March 2007. All patients fulfilled the criteria of chronic headache for longer than 3 months, with a normal erythrocyte sedimentation rate. All patients had an unenhanced CT brain examination performed on an Elscint Elite 2 slice scanner prior to 2001 and a Marconi M8000 4 slice scanner subsequently. Each scan was reviewed and intravenous contrast (100 ml of Niopam 300 by hand injection with 5-minute delay) was administered if necessary. The scans were all reported by a consultant neuroradiologist. Particular attention was given to the assessment of the craniocervical junction, the posterior fossa and parasellar areas, as well as the paranasal sinuses.
The database was used to identify all scans that had been reported as abnormal. The full text of these reports was reviewed by a radiologist. A consultant neurologist with a special interest in headache then reviewed those cases with abnormal imaging findings. Based on the patient's presenting symptoms, the abnormalities were classed as likely to be incidental to, or potentially causative of, the presenting symptoms. The subsequent management of patients with potentially causative abnormalities was reviewed.
The database was then searched for patients with normal scans who had returned for further neuroimaging, to identify any false negatives. Follow-up imaging of the patients with abnormalities was also reviewed to identify false positives.
To assess the impact of the service, a questionnaire was sent to the referring GP for every patient referred for direct-access CT. The questionnaire was sent along with the radiology report of each direct-access CT. The aim of the questionnaire was to collect data regarding choice of referral path, further specialist referral, scan results, and quality and timeliness of the radiology report (Box 1).
Box 1 Questions posed to referring GPs following referral of a patient with chronic headache for direct-access CT
-
▸
Irrespective of the current waiting times, what would your first choice of referral have been for this patient?
-
▸
Given the current waiting times for operations in some specialties, where would you normally have referred the patient if direct-access CT was not available?
-
▸
Did the results reach you within 1 week of the appointment date?
-
▸
Was the issued report understandable and complete?
-
▸
Given the CT scan, will the patient now require a hospital referral?
-
▸
If yes, to which specialty will the patient be referred?
-
▸
Are there any further comments you wish to make?
The Information Services Division (ISD) of NHS National Services Scotland is Scotland's national organisation for health information and statistics.10 The study aimed to use ISD data to perform a cost evaluation of the direct-access CT service. Data collected for April 2008 to April 2009 costed a CT scan at £118.92 and a consultant outpatient appointment at £127.00. The GP questionnaire data regarding referral pathways were projected to the study group, along with data provided by a clinical audit of brain imaging of patients with chronic headache, to allow estimation of any potential cost savings of this service.
RESULTS
During the 8-year study period, a total of 4404 direct-access CT examinations of the brain for chronic headache were performed. The mean age of patients was 43.6 years (range 11.5–99.5 years), and 63% of patients were female.
CT findings
A total of 3943 scans were reported as normal, and abnormal findings were reported in 461 scans (10.5%). Following neurology review, the abnormal findings were thought to be potentially causative in 60 patients (1.4%) and likely to be incidental to the presenting symptoms in 401 scans (9.1%). The abnormalities are detailed in Tables 1 and 2.
Table 1.
Abnormalities on direct-access CT in patients with chronic headache that were likely to be causative of the presenting symptoms (n = 60)
| Abnormality | n | Rate, % |
|---|---|---|
| Brain tumour | 22 | 0.5 |
| Chiari I malformation | 18 | 0.4 |
| Arachnoid cyst | 12 | 0.2 |
| Cerebral aneurysm | 5 | 0.1 |
| Colloid cyst | 2 | 0.04 |
| AVM | 1 | 0.02 |
AVM = Arteriovenous malformation.
Table 2.
Selected abnormalities on direct-access CT in patients with chronic headache that were likely to be incidental to the presenting symptoms
| Abnormality | n | Rate, % |
|---|---|---|
| Small vessel disease | 98 | 2.2 |
| Generalised atrophy | 67 | 1.5 |
| Established infarct | 48 | 1 |
| Lacunar infarct | 19 | 0.4 |
| Focal atrophy | 16 | 0.3 |
| Abnormal calcification | 15 | 0.3 |
| Tonsillar ectopia | 12 | 0.2 |
| Demyelination | 10 | 0.2 |
| Paranasal sinus thickening | 9 | 0.18 |
| Ventricular asymmetry | 8 | 0.16 |
| Cerebellar atrophy | 8 | 0.16 |
| Pineal cyst | 4 | 0.08 |
| Small ventricles | 4 | 0.08 |
| Frontal atrophy | 3 | 0.06 |
| Cavernous angioma | 2 | 0.04 |
| Small chronic subdural haematoma | 2 | 0.04 |
| Giant cisterna magna | 2 | 0.04 |
| Dandy Walker variant | 1 | 0.02 |
| Grey matter heterotopia | 1 | 0.02 |
The 22 tumours diagnosed with CT comprised 14 meningiomas, one low-grade glioma, four pituitary tumours, and three metastases. Of the 14 meningiomas, four were surgically resected and the remainder were being followed up at the time of review. The low-grade glioma demonstrated no growth over the 3-year period of follow-up. Two of the metastatic deposits were from a bronchial primary, one of which was resected. The other metastasis was in the posterior fossa and was also resected. Two of the pituitary tumours were resected, and two were followed-up with imaging.
Twelve of the patients with a Chiari I malformation had no further imaging, and six had magnetic resonance imaging (MRI) studies that confirmed the diagnosis. No patients with a Chiari I had surgical intervention. Of the 12 patients with arachnoid cysts, two required ventricular shunts and follow-up imaging; the remainder had no further imaging or intervention. Two of the five aneurysms were treated endovascularly. The others did not fulfill the criteria for treatment. The two colloid cysts were excised with normal follow-up scans at 5 years. The single occipital arteriovenous malformation was not suitable for treatment.
Seventeen patients who had normal scan reports returned for further neuroimaging. Of these, 15 had CT and two had MRI examinations. No abnormality was demonstrated on these further studies. Therefore, no false negatives were found in this study period.
Two patients who had abnormalities reported on the initial direct-access CT returned for follow-up MRI studies, which were normal. The abnormalities suggested on the direct-access CT were a pituitary lesion and Chiari I malformation. There were therefore two false positives (0.05%).
GP questionnaire data
A total of 996 out of 2998 questionnaires were returned (23%); 10 of these were spoilt. The remaining 986 questionnaires were analysed for this study.
Analysis of the GP questionnaire data revealed that by far the largest group of GPs (n = 460, 47%) indicated that direct-access CT would be the preferred choice of referral for investigation of patients with chronic headache. GPs indicated that if direct-access CT had not been available then neurology (n = 444, 45%) and general medicine (375, 38%) clinics would have been the commonest referral choices. Ten per cent of patients would not have been referred for investigation had this service not been available (Figure 1).
Figure 1.
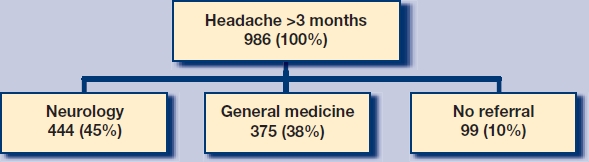
Referral pathways had direct-access not been available.
Following their direct-access CT scan, the majority of patients (848/86%) did not require further specialist referral. GPs responded that of the 138 patients who were referred for specialist opinion, the majority were referred to neurology; general medicine; ear, nose and throat (ENT); and headache clinic, with smaller numbers to neurosurgery, stroke, oncology, ophthalmology and geriatrics (Figure 2).
Figure 2.
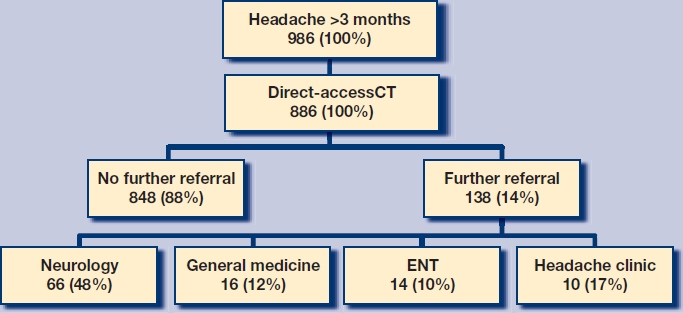
Most common referral pathways with direct-access CT.
The 986 questionnaires returned confirmed that 658 (67%) of the 986 reports issued were received within the specified time of 1 week from the appointment date. Three hundred and nineteen reports took longer than 1 week to reach the GP; 79% of all reports reached the GP within 14 days. The content of the reports was understood and found to be acceptable to 979 of the GPs (99%). Seven (<1%) GPs indicated that the medical terminology used in the report was not understood; 100% of additional comments provided positive feedback about the service.
Cost evaluation
Projecting the referral choices from the GP questionnaire data to the present study group and using the ISD costing data, it is possible to calculate approximate costs with and without the direct-access CT service in place.
Without direct-access CT, it is known that 90% (n = 3964) of the patients would have been referred to a consultant outpatient appointment at a cost of £503 428.
A departmental audit of a local headache clinic assessing patients with headache over a 6-month period in 2006 demonstrated that 29% of patients were referred for neuroimaging (£131 991.68), and 37% of these patients are given a further review appointment (£53 288.93). This gives a total cost of £688 708.61.10
With direct-access CT in place, all 4404 patients would have had a CT scan at a cost of £523 723.68; 14% of these patients then go on to have a consultant outpatient appointment (£78 303.12), giving a total cost of £602 026.80. This would give an approximate saving of at least £86 681.81.
DISCUSSION
Summary of main findings
It was found that the incidence of significant abnormality in patients with chronic headache is low, as anticipated.8,9
Strengths and limitations of the study
No false negatives, and a low number of false positives, were demonstrated during the study period. Patients who did not have follow-up imaging in Greater Glasgow will have eluded the database, although it is felt that these numbers are likely to be representative of an acceptably low level of false negatives and positives.
Comparison with existing literature
Comparing the incidence of pathology to that reported in a recent meta-analysis of MRI screening data in asymptomatic patients (Table 3),11 the present CT study demonstrates slightly lower rates. This may be a reflection of the greater sensitivity of MRI but certainly suggests that the incidence of pathology in this group of patients is no greater than in the asymptomatic population.
Table 3.
Comparison of selected abnormalities with the rates found in an asymptomatic population study
| Abnormality | Current study CT in chronic daily headache (n = 4 404), % | Morris et al11 MRI in asymptomatic population (n = 19 559), % |
|---|---|---|
| Tumour | 0.5 | 0.7 |
| Chiari 1 | 0.4 | 0.24 |
| Arachnoid Cyst | 0.2 | 0.5 |
| Aneurysm | 0.1 | 0.35 |
| Cavernoma | 0.04 | 0.16 |
| Colloid Cyst | 0.04 | 0.04 |
| AVM | 0.02 | 0.05 |
AVM = Arteriovenous malformation
Implications for clinical practice and future research
If there is a low yield of pathology in patients with chronic headache then why continue this service? The study argues that there are important benefits to the patient and GP, and there are also cost benefits. There is a reduced waiting time for patients to be scanned as they do not have to wait for a specialist clinic appointment. In the majority of patients (86%) this gives early and complete reassurance that there is no structural cause for their headaches. This not only provides reassurance for the patient and referring GP, but may have economic benefits due to lower uptake of resources.12
GPs have indicated that they are satisfied with this service, and direct-access CT is the preferred choice for management of patients with chronic headache. The study also demonstrates an 80% reduction in initial referrals to neurology clinics and a 94% reduction in initial referrals to general medical outpatient clinics for patients with chronic headache. There was an 83% reduction in the total number of patients referred for a specialist opinion.
The cost-effectiveness of this service is less clear. The study demonstrates a saving of £86 681.81, although this figure is dependent on a large number of variables. For example, if there is an increase in the number of patients from secondary clinics requiring imaging, then the savings with direct-access CT will be increased. If, however, patients who are initially reassured by a normal scan subsequently require secondary referral, then the savings will be reduced. Some patients with chronic headache may be managed in the primary care setting by GPs with specialist interest in headache, which may further reduce the cost of management.13 Further study of the long-term referral and investigation pathways of direct-access CT patients would be required to clarify the cost-effectiveness of the service.
Although the yield of pathology in this group of patients is low, this study demonstrates important benefits to the patient and GP of providing early reassurance in the majority of cases. There are potential cost savings, although this benefit is less clear with current data and would require appropriate prospective data collection.
Acknowledgments
Thanks to Andrea Slow (data manager, INS), and Jane Logan (Radiographer, INS).
Competing interests
The authors have stated that there are none.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Midgette LA, Scher AI. The epidemiology of chronic daily headache. Curr Pain Headache Rep. 2009;13(1):59–63. doi: 10.1007/s11916-009-0012-2. [DOI] [PubMed] [Google Scholar]
- 2.Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106(1–2):81–89. doi: 10.1016/s0304-3959(03)00293-8. [DOI] [PubMed] [Google Scholar]
- 3.Scher AI, Stewart WF, Liberman J, Lipton RB. Prevalence of frequent headache in a population sample. Headache. 1998;38(7):497–506. doi: 10.1046/j.1526-4610.1998.3807497.x. [DOI] [PubMed] [Google Scholar]
- 4.Schankin CJ, Ferrari U, Reinisch VM, et al. Characteristics of brain tumour associated headache. Cephalalgia. 2007;27(8):904–911. doi: 10.1111/j.1468-2982.2007.01368.x. [DOI] [PubMed] [Google Scholar]
- 5.Galego JC, Moraes AM, Cordeiro JA, Tognola WA. Chronic daily headache: stress and impact on the quality of life. Arq Neuropsiquiatr. 2007;65(4B):1126–1129. doi: 10.1590/s0004-282x2007000700006. [DOI] [PubMed] [Google Scholar]
- 6.Ridsdale L, Clark LV, Dowson AJ, et al. How do patients referred to neurologists for headache differ from those managed in primary care? Br J Gen Pract. 2007;57(538):388–395. [PMC free article] [PubMed] [Google Scholar]
- 7.Oliver Ellis. GPs are to refer suspected cancer patients for tests in a week under new scheme. BMJ. 2009;339:b3994. doi: 10.1136/bmj.b3994. [DOI] [PubMed] [Google Scholar]
- 8.Benamore RE, Wright D, Britton I. Is primary care access to CT brain examinations effective? Clin Radiol. 2005;60(10):1083–1089. doi: 10.1016/j.crad.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 9.White PM, Halliday-Pegg JC, Collie DA. Open access neuroimaging for general practitioners — diagnostic yield and influence on patient management. Br J Gen Pract. 2002;52(474):33–35. [PMC free article] [PubMed] [Google Scholar]
- 10.ISD Scotland. Latest statistics. http://www.isdscotland.org/isd/CCC_FirstPage.jsp (accessed 21 Oct 2010)
- 11.Morris Z, Whiteley WN, Longstreth WT, Jr, et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2009;339:b3016. doi: 10.1136/bmj.b3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howard L, Wessely S, Leese M, et al. Are investigations anxiolytic or anxiogenic? A randomised controlled trial of neuroimaging to provide reassurance in chronic daily headache. J Neurol Neurosurg Psychiatry. 2005;76(11):1558–1564. doi: 10.1136/jnnp.2004.057851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ridsdale L, Doherty J, McCrone P, et al. A new GP with special interest headache service: observational study. Br J Gen Pract. 2008;58(552):478–483. doi: 10.3399/bjgp08X319440. [DOI] [PMC free article] [PubMed] [Google Scholar]


