Abstract
Background
Patients with high blood pressure (hypertension) in the community frequently fail to meet treatment goals: a condition labelled as ‘uncontrolled’ hypertension. The optimal way to organise and deliver care to hypertensive patients has not been clearly identified.
Aim
To determine the effectiveness of interventions to improve control of blood pressure in patients with hypertension.
Design of study
Systematic review of randomised controlled trials.
Setting
Primary and ambulatory care.
Method
Interventions were categorised as following: self-monitoring; educational interventions directed to the patient; educational interventions directed to the health professional; health professional- (nurse or pharmacist) led care; organisational interventions that aimed to improve the delivery of care; and appointment reminder systems. Outcomes assessed were mean systolic and diastolic blood pressure, control of blood pressure and proportion of patients followed up at clinic.
Results
Seventy-two RCTs met the inclusion criteria. The trials showed a wide variety of methodological quality. Self-monitoring was associated with net reductions in systolic blood pressure (weighted mean difference [WMD] −2.5mmHg, 95%CI = −3.7 to −1.3 mmHg) and diastolic blood pressure (WMD −1.8mmHg, 95%CI = −2.4 to −1.2 mmHg). An organised system of regular review allied to vigorous antihypertensive drug therapy was shown to reduce blood pressure and all-cause mortality in a single large randomised controlled trial.
Conclusion
Antihypertensive drug therapy should be implemented by means of a vigorous stepped care approach when patients do not reach target blood pressure levels. Self-monitoring is a useful adjunct to care while reminder systems and nurse/pharmacist -led care require further evaluation.
Keywords: hypertension, prevention and control, primary care, systematic review
INTRODUCTION
Hypertension is largely managed in primary care and is an important public health problem in terms of associated stroke and cardiovascular events. It is mostly of unknown aetiology, easy to diagnose, and readily preventable by blood pressure reduction. Extensive epidemiological data have strengthened the well-recognised relationship between blood pressure and risk of cardiovascular disease, and have confirmed the importance of systolic blood pressure as a determinant of risk.1 However, blood pressure goals are achieved in only 25–40% of the patients who take antihypertensive drug treatment,2,3 which is something that has remained unchanged for the last 40 years.4
Use of self-monitoring of blood pressure by patients and professionals has gained popularity and is now recommended in particular patients in certain national and international guidelines; a recent meta-analysis of randomised trials on the subject did suggested a benefit in terms of mean blood pressure and blood pressure control.5 This systematic review aims to update and build upon previous reviews,6,7 by summarising the evidence from randomised controlled trials (RCTs) that evaluate non-pharmacological interventions to improve the management of hypertension in primary care.
How this fits in.
The majority of patients with hypertension who take blood pressure medication fail to reach treatment goals. There is a strong evidence base for the benefits of antihypertensive drug therapy, but there is a lack of clarity on how to organise and deliver care for patients with hypertension in the community. This systematic review of 72 randomised controlled trials shows that self-monitoring leads to a significant decline in systolic and diastolic blood pressure and, as such, may be a useful adjunct to care and is likely to lead to a reduction in cardiovascular events. An organised system of regular review allied to vigorous antihypertensive drug therapy was shown to reduce blood pressure and allcause mortality. Nurse- or pharmacist-led care and appointment-reminder systems may be a promising way of improving blood pressure control, but require further evaluation.
METHOD
Searching and study selection
Studies of patients aged >18 years with essential hypertension in an ambulatory setting were included. The interventions comprised all those that aimed to improve blood pressure control by non-pharmacological means and were classified as:
self-monitoring;
educational interventions directed to the patient;
educational interventions directed to the health professional;
nurse- or pharmacist-led care;
organisational interventions that aimed to improve the delivery of care; or
appointment-reminder systems.
The outcomes assessed were mean systolic and diastolic blood pressure, control of blood pressure, and the proportion of patients followed up at clinic.
Original RCTs were identified by an all-language search in February 2008 of all articles (any year) in the Cochrane Controlled Trials Register and Medline (search strategy shown in Appendix 1); articles dated from January 1980 were searched on Embase. Included studies had to be RCTs with a contemporaneous control group, where patient care in the intervention group(s) was compared with either no intervention or usual care.
Data extraction and analysis
Two of the authors assessed lists of citations and abstracts independently. Differences were resolved by discussion and final adjudication was performed by an additional two authors. Reprints of all potentially relevant citations were obtained and data were independently extracted in duplicate using a structured data-collection form. Study quality was assessed by collection of data on inclusion and exclusion criteria; randomisation procedure; allocation concealment; blinding of participants, providers of care, and outcome assessors; and losses to follow-up.8
The effects on blood pressure outcomes of the six pre-defined intervention categories outlined above were examined. For the outcomes of mean systolic and diastolic blood pressure, pressure differences from baseline to final follow-up in the intervention and control groups were compared and pooled using the weighted mean difference approach.7 For the outcomes of blood pressure control and clinic attendance at follow-up, statistical and clinical significance was evaluated by means of estimating odds ratios (ORs) with 95% confidence intervals (CIs). Individual study definitions of control of blood pressure and attendance at clinic were used. For both continuous and categorical outcomes, the meta-analyses for heterogeneity were checked by visual inspection and by Cochran's C test. Pooled ORs and their 95% CIs were calculated with The Cochrane Collaboration RevMan software (version 5.02).
RESULTS
Trial flow, study characteristics, and quality assessment
The flow of studies through the stages of the systematic review is shown in Figure 1. A total of 72 trials were included in this systematic review (Characteristics of included randomized controlled trials are described in Appendix 2). The reported methodological quality of included studies was generally poor to moderate. The randomisation process was described in 30 (42%) of the 72 trials included, while only 14 (19%) had adequate allocation concealment. In 15 studies (21%), the outcome assessors were blind to the treatment allocation and losses to follow-up of 20% or more occurred in 18 (25%) of studies.
Figure 1.
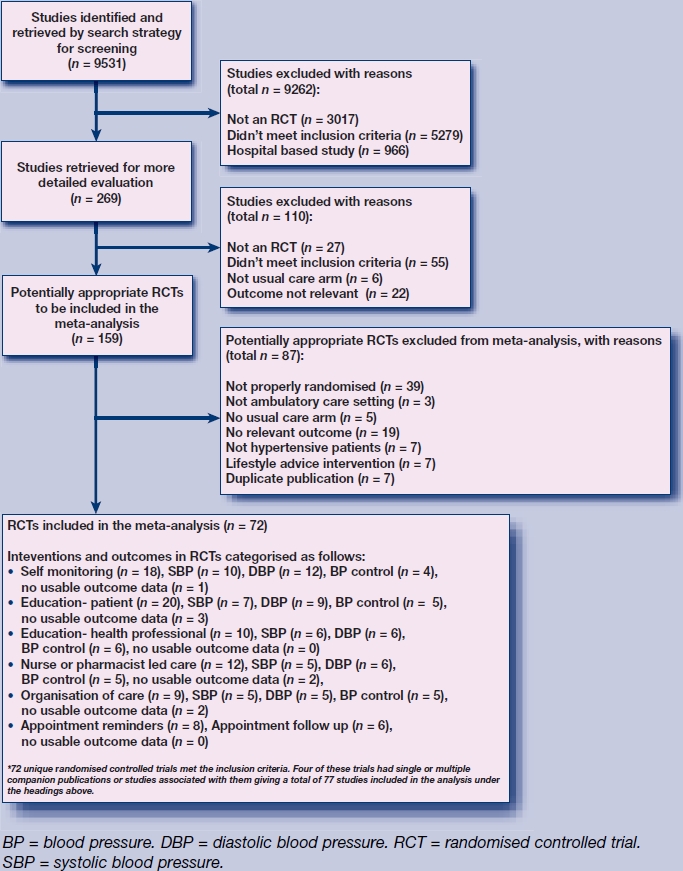
Flow chart for studies through stages of systematic review.
Intervention effects
The impact of interventions is summarised in Table 1 (full data available from authors). There was substantial heterogeneity for several interventions and outcomes. In these situations, pooled data are not reported but the range of results from individual RCTs are presented.
Table 1.
Summary of results of interventions on systolic and diastolic blood pressure, blood pressure control and follow-up at clinic
| Systolic blood pressure, mmHg | Diastolic blood pressure, mmHg | Blood pressure control, ORa | ||||
|---|---|---|---|---|---|---|
| Intervention | Pooled estimate (95% CI) | Range of results from individual RCTs | Pooled estimate (95% CI) | Range of results from individual RCTs | Pooled estimate (95% CI) | Range of results from individual RCTs |
| Self-monitoring | −2.5 (−3.7 to −1.3)b | −10 to 5 | −1.8 (−2.4 to −1.2)b | −12 to 0 | 1.0 (0.8 to 1.2) | 0.5 to 1.3 |
| Education (patient) | c | −16 to 1 | c | −9 to 7 | −0.8 (0.8 to 1.0)a | 0.3 to 1.1 |
| Education (physician) | −2.0 (−3.5 to −0.6)b | −7 to 1 | −0.4 (−1.1 to 0.3) | −2 to 1 | 0.9 (0.8 to 0.9) | 0.8 to 1.0 |
| Nurse- or pharmacist-led care | c | −13 to 0 | c | −8 to 0 | c | 0.1 to 0.9 |
| Organisational interventions | c | −12 to 3 | c | −8 to 5 | c | 0.5 to 1.8 |
| Appointment reminders | c | −10 to 5 | c | −7 to 2 | 0.5 (0.4 to 0.7)a | 0.5 to 0.6 |
| Follow-up at clinic (RR) | ||||||
| Intervention | Pooled estimate (95% CI) | Range of results from individual RCTs | ||||
| Appointment reminders | c | 0.1 to 1.4 | ||||
OR of control of blood pressure (‘control’ blood pressure threshold definition taken as that used in each individual RCT), RR <1 blood pressure control greater in intervention group, >1 blood pressure control greater in control group.
P<0.05, heterogeneous results.
No pooled estimate reported.
OR = odds ratio. RCT = randomised controlled trial. RR = relative risk.
Self-monitoring
With regard to self-monitoring (n = 18 RCTs), pooled data from 12 RCTs that reported on differences in mean systolic blood pressure8–19 showed that self-monitoring was associated with a significant reduction of −2.5 mmHg (95% CI = −3.7 to −1.3 mmHg). Pooled data from 14 RCTs on difference of mean diastolic blood pressure,9–22 showed that self-monitoring was associated with a reduction of −1.8 mmHg (95% CI = −2.4 to −1.2 mmHg). In the six RCTs that reported on control of blood pressure,10,12,18,22–24 there was no significant improvement in blood pressure control seen (OR 1.0, 95% CI = 0.8 to 1.2).
Educational interventions
Educational interventions directed to the patient involved 20 RCTs. Eleven RCTs reported mean difference systolic blood pressure,25–35 13 RCTs reported mean difference diastolic blood pressure,25–38 and seven reported blood pressure control.22,23,30,32,33,39,40 For mean difference in systolic blood pressure and diastolic blood pressure outcomes, pooling of results from individual RCTs produced substantial heterogeneity, so pooled mean differences are not valid. The reported mean difference in systolic blood pressure ranged from −16 mmHg to 1 mmHg, and from −9 mmHg to 7 mmHg for mean difference in diastolic blood pressure. In terms of blood pressure control, there was a trend towards improved blood pressure control and this was significant (OR 0.83; 95% CI = 0.75 to 0.91). Educational interventions directed towards the physician (n = 10 RCTs)30,41–49 were not associated with a significant decrease in mean systolic blood pressure or diastolic blood pressure; control of blood pressure produced heterogeneous results (OR ranged from 0.8 to 1.1).
Nurse- or pharmacist-led care
For nurse- or pharmacist-led care (n = 12 RCTs),50–61 the majority of RCTs were associated with improved blood pressure control. However, for all three outcomes, the pooling of results from individual RCTs produced substantial heterogeneity, so pooled mean differences may not be valid. The range of mean difference was from −13 mmHg to 0 mmHg in mean systolic blood pressure (n = 10 RCTs) and from −8 mmHg to 0 mmHg for diastolic blood pressure (n = 12 RCTs); control of blood pressure (n = six RCTs) produced ORs ranging from 0.1 to 0.9.
Organisational interventions
Organisational interventions that aimed to improve the delivery of care were described in nine RCTs.40,41,60–69 For all three outcomes, pooling of results from individual RCTs produced heterogeneous results, so pooled mean differences may not be valid. Of note, the largest RCT, the Hypertension Detection and Follow–Up Program (HDFP),64 produced substantial reductions in systolic blood pressure and diastolic blood pressure across the three groups (weighted mean difference −8.2/−4.2 mmHg, −11.7/−6.5 mmHg, −10.6/−7.6 mmHg for the three strata of entry blood pressure).
Appointment-reminder systems
For appointment-reminder systems (n = 8 RCTs),70–77 the pooled results – although favouring the intervention for follow-up of patients (OR of being lost to follow-up 0.4, 95% CI = 0.3 to 0.5) – are heterogeneous because of the single outlying RCT, and the pooled results should be treated with caution. Pooled data from two small RCTs – one a three-armed study of telephone reminder, mailed reminder, and usual care,76 and the other a parallel study of SMS reminder versus usual care77 – gave heterogeneous results in terms of systolic and diastolic blood pressure, but did show a significant improvement in blood pressure control, OR 0.5 (95% CI = 0.4 to 0.7).
DISCUSSION
In this systematic review, self-monitoring was associated with a significant decline in systolic blood pressure (−2.5 mmHg) and diastolic blood pressure (−1.8 mmHg). Although this blood pressure reduction does not appear substantial in clinical terms, it would, nonetheless, appear to be a useful adjunct to care and is likely to lead to a reduction in mortality and cardiovascular events. This appears to be confirmed in the HDFP study65,66 where an organised system of regular review allied to vigorous antihypertensive drug therapy was shown to reduce blood pressure as well as all-cause mortality.
At 5-year follow-up, the reductions in blood pressure (∼10 mmHg for systolic blood pressure and 5 mmHg for diastolic blood pressure) seen in this study were associated with a significant reduction in all-cause mortality (6.4% versus 7.8%, absolute risk reduction = 1.4%, numbers needed to treat = 71). Nurse- or pharmacist-led care and appointment-reminder systems may be a promising way of improving blood pressure control, but require further evaluation.
A previous meta-analysis of self-monitoring produced similar findings to the current study of modest, but potentially important, benefit in systolic and diastolic blood pressure.5 This is important in light of the fact that self-monitoring is now practised by up to two-thirds of the population that has hypertension in the US and Europe.78
There are also other elements identified from this review that appear to be associated with improved blood pressure control and are consistent with findings from observational studies and previous systematic reviews. A more recent observational study showed that antihypertensive drug therapy was initiated or changed in only 38% of episodes of care, despite documented uncontrolled hypertension for at least 6 months.79 Lack of practice organisation is associated with a failure to achieve treatment surrogate goals in hypertension, diabetes, and secondary prevention of coronary heart disease.80
This review had several limitations. Several RCTs included patients with hypertension who were treated and untreated and had differential rates of antihypertensive drug prescribing.8,18,47,76 Many RCTs contained multifaceted interventions that did not fit into a single intervention category.40,51,67 Consequently, it has been difficult to attribute how far single elements that make up complex interventions exert their independent effect on blood pressure control. Finally, several of the RCTs did not make any recommendations about the need for adjustment of target blood pressure readings when self-monitoring was the intervention being assessed, nor did they appear to anticipate lower blood pressure readings in the self-monitoring group.16,21,22,24 This may have attenuated the impact of self-monitoring on blood pressure control because of failure to intensify treatment. Self-monitoring of blood pressure by patients and blood pressure management by allied healthcare professionals both require further development and evaluation in larger RCTs and prospective studies, including cardiovascular outcomes.
This systematic review does, however, confirm that the most effective way to manage hypertension in the community is through a structured approach combining systematic identification and follow-up, which will include patient self-monitoring allied with appropriate treatment with antihypertensive medications.
Acknowledgments
We are very grateful to Margaret Burke (Cochrane Heart Group) for help with searching and to Shah Ibrahim who was an author on the original review. Our thanks also to Alison Blenkinsopp, Barry Carter, Sandy Logan, Frank Sullivan, Hayden Bosworth, Brian Haynes, David Jewell, Jim Krieger, Richard McManus, Steven Ornstein, Mike Phelan, Mary Rogers, Lin Song, Kelly Zarnke and Peter Whincup concerning clarification about individual RCTs and providing additional data. Thanks to Craig Ramsay for advice concerning factorial trials. We are grateful to Curt Furberg for facilitating contact with the investigators of US-based studies. Our particular thanks to Charlie Ford for information regarding the Hypertension Detection and Follow-Up Program (HDFP) study. Lastly, we are grateful to Debbie Farrell for administrative support.
Appendix 1.
MEDLINE search strategya
| 1 exp Hypertension/(167533) |
| 2 (blood adj pressure).ti. (33263) |
| 3 hypertens$.ti. (120524) |
| 4 or/1–3 (208545) |
| 5 exp physicians/ (62183) |
| 6 exp Patient Care Management/ (351254) |
| 7 exp Patient Care Planning/ (40740) |
| 8 exp Patient Care Team/ (40160) |
| 9 exp Patient Education/ (50057) |
| 10 exp Patient Participation/ (11975) |
| 11 exp Ambulatory Care Information Systems/ (1034) |
| 12 exp Feedback/ (21503) |
| 13 exp Information Systems/ (98899) |
| 14 exp Management Information Systems/ (27680) |
| 15 exp Decision Support Systems, Clinical/ (2297) |
| 16 exp Decision Making, Computer-Assisted/ (46651) |
| 17 exp Reminder Systems/ (1144) |
| 18 exp Practice Guidelines/ (42659) |
| 19 exp Guidelines as topic/ (64954) |
| 20 exp Medical Audit/ (10918) |
| 21 exp Medical Records/(56232) |
| 22 exp Medical Records Systems, Computerized/ (13174) |
| 23 exp Primary Health Care/ (49856) |
| 24 exp Physicians, Family/ (11443) |
| 25 exp Primary Nursing Care/ (1868) |
| 26 exp Nurse Practitioners/ (11902) |
| 27 exp Nurse Clinicians/ (6234) |
| 28 exp Health Behavior/ (58847) |
| 29 remind$.tw. (6318) |
| 30 motiv$.tw. (41873) |
| 31 Patient Care/ (4501) |
| 32 Nursing Care/ (24234) |
| 33 Guideline Adherence/ (9258) |
| 34 Ambulatory Care/ (28816) |
| 35 exp Behavior Therapy/ (35585) |
| 36 Counseling/(21055) |
| 37 counsel$.tw. (40826) |
| 38 Motivation/ (34065) |
| 39 self monitor$.tw. (2518) |
| 40 ((patient$ or program$) adj3 (educat$ or manage$ or train$ or teach$)).tw. (121066) |
| 41 self manage$.tw. (3390) |
| 42 ((manage$ or monitor$) adj3 (hypertension or blood pressure)).tw. (9858) |
| 43 Health Promotion/(31545) |
| 44 exp Health Education/ (102113) |
| 45 (reward$ or incentive$).tw. (25369) |
| 46 uncontrol$.tw. (17033) |
| 47 Self Care/(14858) |
| 48 or/5-47 (1087894) |
| 49 4 and 48 (19344) |
| 50 randomized controlled trial.pt. (246660) |
| 51 controlled clinical trial.pt. (76052) |
| 52 Randomized Controlled Trials/ (51847) |
| 53 random allocation/ (59418) |
| 54 double blind method/ (94259) |
| 55 single blind method/ (11548) |
| 56 or/50-55 (416351) |
| 57 animal/ not human/ (3141649) |
| 58 56 not 57 (390135) |
| 59 clinical trial.pt. (439482) |
| 60 exp clinical trials as topic/ (197049) |
| 61 (clin$ adj25 trial$).ti,ab. (139080) |
| 62 ((singl$ or doubl$ or treble$ or tripl$) adj25 (blind$ or mask$)).ti,ab. (93517) |
| 63 placebos/ (26524) |
| 64 placebo$.ti,ab. (106301) |
| 65 random$.ti,ab. (393128) |
| 66 research design/ (50559) |
| 67 or/59-66 (882479) |
| 68 67 not 57 (818962) |
| 69 58 or 68 (840420) |
| 70 49 and 69 (4661) |
Search slightly amended for Cochrane Central Register of Controlled Trials (CENTRAL) and Embase.
Appendix 2.
Characteristics of included randomised controlled trials
| RCT | Population | Intervention | Outcomea | Interpretation |
|---|---|---|---|---|
| McManus et al15 | 441 people receiving treatment in primary care for hypertension but not controled below the target of <140/85 mm Hg. | (1) Patients in the intervention group received treatment targets along with facilities to measure their own blood pressure at their general practice; they were also asked to visit their GP or practice nurse if their blood pressure was repeatedly above the target level. | SBP −2.30 (−5.39 to 0.79) | Positive for SBP |
| (2) Patients in the control group received usual care | DBP −1.10 (−2.75 to 0.55) | |||
| Control not reported | ||||
| Bailey et al18 | Patients with hypertension about to start BP-lowering treatment | (1) Self-monitoring: use of an Omron HEM706 monitor. Asked to record BP twice daily for 8 weeks | SBP 5.0 (−4.7 to 14.7) | No effect SBP, positive effect DBP. Physicians in intervention group not instructed to adjust for self-monitored BP readings |
| (2) Usual care: no self-recording | DBP −2.0 (−3.4 to −0.6) | |||
| Control not reported | ||||
| Carnahan et al16 | Patients with hypertension starting treatment in hospital clinic | (1) Self-monitoring: instructed to use own sphygmomanometer twice a day. | SBP −7.5 (−14.2 to −0.8) | Positive effect SBP, no effect DBP |
| Readings recorded and delivered to the clinic when visiting | DBP 0 (−3.9 to 3.9) | |||
| (2) Usual care | Control not reported | |||
| Friedman et al13 | Taking BP-lowering drugs, SBP ≥160 mmHg or DBP ≥90 mmHg on average two readings | (1) Home monitoring and telecommunication system | SBP −4.0 (−3.9 to 3.1) | No effect SBP, positive effect DBP |
| • Weekly automated home blood pressure recording | DBP −4.4 (−6.5 to −2.3) | |||
| • Telephone-linked computer system to patient | Control not reported | |||
| (2) Usual care | ||||
| Haynes et al21 | Males with hypertension not compliant or at goal DBP (≥90 mmHg) | (1) Patient self-monitoring and education | SBP not reported | No effect DBP |
| (2) Usual care | DBP −3.5 (−7.0 to 0.1) | |||
| Control not reported | ||||
| Johnson et al22 | All taking BP-lowering medication for ≥1 year with uncontrolled hypertension (DBP≥95 mmHg) | (1) Self-recording | SBP not reported | No effect RCT |
| (2) Home visit: BP measured in their homes every 4 weeks with result given to them and physician. Both groups visited at home after 2 weeks | DBP −1.0 (−5.7 to 3.7) | |||
| (3) Both interventions | Control not reported | |||
| (4) Neither intervention | ||||
| Mehos et al19 | People with uncontrolled hypertension SBP 140-179 mmHg and/or DBP 90-109 mmHg | (1) Home blood pressure monitoring | SBP −10.1 (−19.8 to −0.4) | No effect SBP, positive effect DBP |
| (2) Usual care | DBP −6.7 (−13.2 to −0.3) | |||
| Control not reported | ||||
| Pierce et al23 | People with uncontrolled hypertension (SBP ≥160 and/or DBP ≥95 mmHg) | (1) Self-monitoring | SBP not reported | No effect RCT (self-monitoring arm) |
| (2) Health-education programme | DBP not reported | |||
| (3) Both interventions | Control 1.2 (0.6 to 2.7) | |||
| (4) Usual care | ||||
| Rogers et al12 | Change in BP medication because: | (1) Telecommunication service with three components: automated BP at home; central processing of BP readings; weekly reports to both physician and patient | SBP −4.8 (−9.8 to 0.2) | No effect SBP, positive effect DBP, no effect control of blood pressure |
| (1) SBP ≥140 or DBP ≥90 mmHg | (2) Usual care | DBP −4.0 (−7.7 to −0.3) | ||
| (2) Side-effects from drugs | Control 1.1 (0.5 to 2.3) | |||
| (3) SBP >180 or DBP >110 without current antihypertensive therapy | ||||
| Soghikian et al17 | Hypertension but no entry BP level required or defined | (1) Home blood pressure measurement: patients asked to measure BP twice weekly, mail record of BP, medications and side effects to project office every 4 weeks | SBP −3.3 (−6.4 to −0.2) | Positive effect SBP, no effect DBP |
| (2) Usual care | DBP −1.6 (−3.5 to to 0.3) | |||
| Control not reported | ||||
| Vetter20 | Hypertension, SBP 160-200 mmHg or DBP 95-115 mmHg in patients who are untreated or uncontrolled | (1) Home measurement of blood pressure by patients | SBP −0.5 (−2.8 to 1.8) | No effect SBP, positive effect DBP, no effect on control of blood pressure |
| (2) Usual care | DBP −1.3 (−2.4 to −0.2) | |||
| Control 0.8 (0.6 to 1.1) | ||||
| Baqu et al25 | Patients with poorly controlled essential hypertension, defined as systolic blood pressure > or = 140 or diastolic blood pressure > or = 90 mmHg. | (1) The patients were given an OMRON HEM-705CP automatic blood pressure monitor on two occasions, for use during 15 days at weeks 6 and 14. Blood pressure was recorded at each visit (baseline, 6, 8,14,16, and 24 weeks) | SBP not reported | No effect for blood pressure control |
| (2) Usual care | DBP not reported | |||
| Control 1.21 (0.94 to 1.58) | ||||
| Zarnke26 | Average BP readings <160/95 mmHg taking BP lowering drugs or receiving non-pharmacological advice | (1) Patient-directed group: instructed in home BP measurement, measured own BP twice daily and instructed by means of algorithm to change own BP medication | SBP not reported | Positive RCT mean arterial BP improved by −3 mmHg at 8 weeks follow-up |
| Control not reported | ||||
| Artinian et al11 | Hypertension, SBP ≥140 mmHg or ≥90 mmHg or for patients with diabetes ≥130 mmHg or ≥85 mmHg | (1) Home BP telemonitoring: self-monitoring at home and transmitting BP readings over telephone | SBP −26.0 (−40.0 to 11.6) | No effect RCT (pilot study with short follow-up period of 3 months) |
| (2) Nurse-managed community-based BP monitoring | DBP −12.0 (−21.5 to −2.5) | |||
| (3) Usual care | Control not reported | |||
| Midanik et al9 | Untreated patients with hypertension: SBP <180 mmHg and DBP 90–99 mmHg | (1) Self-monitoring: patients trained to take two consecutive readings twice a week. | SBP −2.0 (−7.4 to 3.4) | No effect RCT |
| Sent in readings every 4 weeks for 1 year | DBP 0 (−2.9 to 2.9) | |||
| (2) Usual care | Control not reported | |||
| Rudd et al10 | Hypertension: SBP ≥140 mmHg or DBP ≥90 mmHg in previous 6 months or history of drug treatment | (1) Self-measurement with nurse management based on algorithm | SBP −8.5 (−14.3 to −2.7) | Positive RCT for SBP and DBP |
| (2) Usual care | DBP −3.1 (−6.0 to −0.2) | |||
| Control not reported | ||||
| Earp et al24 | Hypertension treated at outpatient hypertension clinic or general practice clinic | (1) Home visits: over 18 months by nurse or pharmacist. | SBP not reported | No effect RCT |
| (2) Home visits plus involvement of ‘significant other’ – involved daily/several times a week BP monitoring | Control 1.3 (0.6 to 2.7) | |||
| (3) Usual care | ||||
| Billault et al27 | Attended hypertension clinic, no entry SBP/DBP defined | (1) Booklet with personalised standardised medical information explained to patient and their family doctor | SBP −1.1 (−5.8 to 3.6) | No effect RCT |
| (2) Usual care | DBP 1.4 (−1.5 to 4.3) | |||
| Control not reported | ||||
| Burelle et al28 | Uncontrolled and non-adherent patients with hypertension education and special dosing devices | (1) TIME: home visits, education | SBP −7.4 (−22.5 to 7.7) | No effect RCT, very small study |
| (2) Usual care | DBP 7.1 (−5.2 to 19.4) | |||
| Control not reported | ||||
| Cakir et al29 | Persons with hypertension (mean systolic BP of 140 mmHg and/or mean diastolic BP, DBP, of 90 mmHg on 3 separate occasions during a 3-week period), and aged 18–65 years | (1) Patient education (‘lifestyle intervention’) while participants in the (2) control group were provided with routine outpatient services and were asked to maintain their usual lifestyles, including dietary and exercise habits, for 6 months until they were reexamined. | SBP −10.0 (−15.0 to −5.0) | Positive for SBP and DBP |
| DBP −8.6 (−12.3 to −4.9) | ||||
| Control not reported | ||||
| Fielding et al30 | Hypertension, either: SBP ≥140 and/or DBP ≥90 mmHg | • (1) IMPACT consisted of monthly 10-minute individual sessions for patients with counsellor | SBP −8.5 (−14.8 to −2.2) | Positive RCT |
| (2) Usual care | DBP −3.9 (−7.1 to −0.7) | |||
| Control not reported | ||||
| Hennessy et al31 | Total of 10 696 patients with a diagnosis of hypertension cared for by 93 primary care providers. | (1) Academic detailing, provision of provider-specific data about hypertension control, provision of educational materials to the provider, and provision of educational and motivational materials to patients. | Patient education | No effect RCT |
| (2) Usual care | BP 0.00 (−0.73 to 0.73) | |||
| DBP 1.00 (0.56 to 1.44) | ||||
| Control 0.83 (0.76 to 0.92) | ||||
| Physician education | ||||
| SBP 0.00 (−0.73 to 0.73) | ||||
| DBP 1.00 (0.56 to 1.44) | ||||
| Control 0.83 (0.76 to 0.92) | ||||
| Morisky et al40 | BP (mmHg) entry criteria based on age: 20–39: >140/90 40–59: >150/95 ≥60: ≥160/100 | (1) Three interventions: exit interview; instructional session on adherence and follow-up care; group sessions | SBP not reported | Improved BP control but substantially greater numbers lost to follow-up in (C) arm at 2 and 5 years |
| (2) Usual care | DBP not reported | |||
| Control 0.6 (0.4 to 0.9) | ||||
| Mühlhauser et al34 | Hypertension (mean last two measurements ≥160 and/or ≥95 mmHg). | (1) Hypertension treatment and teaching programme | SBP −5.0 (−9.3 to −0.7) | Positive RCT for SBP/DBP, no effect on control of BP |
| (2) Usual care | DBP −3.0 (−0.4 to −0.6) | |||
| Control 1.1 (0.4 to 2.6) | ||||
| Hunt et al32 | Patients with mildly uncontrolled hypertension as defined as a last blood pressure of 140 to 159/90 to 99 mmHg from query of an electronic medical record database. | Patients randomised to intervention (1) were mailed two educational packets approximately 3 months apart. (2) The control group consisted of similar patients receiving usual care for hypertension. | SBP −2.00 (−4.70 to 0.70) | No effect on SBP, DBP |
| DBP −2.00 (−4.25 to 0.25) | ||||
| Control not reported | ||||
| McKinstry et al33 | Parallel, single blind, Single urban general practice over 1 year in the UK of patients with hypertension. | (1) Patient-held guideline with written explicit exhortation to challenge care when appropriate. | SBP −1.00 (−5.73 to 3.73) | No effect for SBP or blood pressure control |
| (2) Usual care | DBP −2.00 (−4.63 to 0.63) | |||
| Control 0.98 (0.60 to 1.60) | ||||
| Roca-Cusachs et al35 | Newly diagnosed patients with hypertension. Mean values were: (E) 156.3/95.8 (C) 160.3/96.1 | (1) Patient education: booklet; educational talks; personal tutorial | SBP1.3 (−4.3 to 6.9) | No effect RCT |
| (2) Usual care | DBP 1.9 (−1.1 to 4.9) | |||
| Control not reported | ||||
| Sackett et al41 | Hypertension ≥95 mmHg | (1) Augmented convenience site physician care | SBP not reported | No effect RCT |
| (2) Mastery learning: via audio-cassette and booklet and re-emphasised by a ‘patient educator’ | DBP not reported | |||
| (3) Both interventions | Control 0.7 (0.3 to 2.1) | |||
| (4) Usual care | ||||
| Tanner et al38 | Hypertension DBP ≥90 mmHg | (1) Intervention group: booklet | SBP not reported | No effect RCT |
| (2) Usual care | DBP 0.2 (−4.7 to 5.1) | |||
| Control not reported | ||||
| Watkins et al36 | Hypertension | (1) Information booklet on hypertension sent out to patients | SBP 0.6 (−3.0 to 4.2) | No effect RCT |
| (2) Usual care | DBP 0.4 (−14 to 2.2) | |||
| Control not reported | ||||
| Webb et al39 | Hypertension; DBP≥90 mmHg | (1) Education: three group education sessions by nurse-health educator | SBP not reported | No effect RCT |
| (2) Counselling: three ‘individualised’ counselling sessions | DBP −3.3 (−7.0 to 0.4) | |||
| (3) Usual care: three appointments with family physician | Control not reported | |||
| Zismer et al36 | Hypertension or ≥140 or ≥90 mmHg | (1) Experimental group A: educational ‘self-care’ intervention: pill taking; appointment keeping; dietary sodium reduction | SBP −15.7 (−26.0 to −5.4) | Positive RCT for SBP/DBP |
| (2) Experimental group B-received additional support from family member | DBP −8.7 (−15.5 to −1.9) | |||
| (3) Usual care | Control not reported | |||
| Coe et al43 | Hypertension mean BP ≥140/95 mmHg | (1) Computer-generated treatment recommendations by algorithm | SBP −1.2 (−10.1 to 7.7) | No effect RCT |
| (2) Usual physician care | DBP 1.1 (−3.6 to 5.8) | |||
| Control not reported | ||||
| Dickinson et al42 | Mean baseline BP 159/89 mmHg | (1) Computer-generated feedback-monthly feedback reports | SBP 1.0 (−8.3 to 10.3) | No effect RCT but improved follow-up at clinic |
| (2) Education programme: three separate self-instructions | DBP −1.0 (−6.9 to 4.9) | |||
| (3) Both | Control 1.0 (0.2 to 3.8) | |||
| (4) Neither | ||||
| Evans et al44 | Hypertension DBP >90 mmHg | (1) Mailed continuous to physicians 14 weekly medical education instalments of information, chart and follow-up appointment system to encourage detection and recall of patients | SBP 0.8 (−4.2 to 5.8) | No effect RCT |
| (2) Usual care | DBP 0.3 (−2.0 to 2.6) | |||
| Control 0.8 (0.5 to 1.5) | ||||
| Hetlevik et al45 | Patients with hypertension | (1) Computer-based decision support system. | SBP −1.5 (−3.2 to 0.2) | No effect RCT |
| Re-enforcement by mean of telephone repetitions seminar on risk intervention | DBP −0.6 (14 to 0.2) | |||
| (2) Usual care | Control not reported | |||
| McAllister et al46 | Patients with hypertension: | (1) Compute-generated feedback to physician on individual patient; inter and intra practice DBP ranking; commentary on treatment by GP according to a ‘stepped-care’ approach. | SBP not reported | No effect RCT |
| (1) DBP >90 mmHg on treatment | (2) Control group filled out same forms but no feedback given | DBP not reported | ||
| Control 0.9 (0.5 to 1.4) | ||||
| Montgomery et al47 | Patients with hypertension aged 60-80 years taking BP-lowering drugs | (1) Computer-based decision support system | SBP −4.0 (−8.3 to 0.3) | No effect RCT |
| (2) Risk chart | DBP 1.0 (−1.2 to 3.2) | |||
| (3) Usual care | Control 1.0 (0.7 to 1.6) | |||
| Ornstein et al48 | Hypertension: Uncontrolled/untreated >140/90 mmHg or on treatment. At baseline 40% (E) and 43.7% (C) had ‘controlled’ BP (<140/90 mmHg) | (1) Multi-method quality improvement | SBP not reported | Positive RCT (for BP control but not for many of the other quality indicators) |
| • Practice site visits | DBP not reported | |||
| • 2-day network meetings in each study year | Control 0.8 (0.7 to 0.9) | |||
| (2) Usual care: received copies of practice guidelines and quarterly performance reports | ||||
| New et al49 | Patients with diabetes and hypertension (>140/80 mmHg) | (1) Educational outreach delivered by specialist nurses | SBP not reported | No effect RCT |
| (2) Usual care | DBP not reported | |||
| Control 1.0 (0.9 to 1.1). | ||||
| Sanders et al50 | Patients with diabetes and hypertension (BP level not defined) | (1) Chart reminder | SBP −6.8 (−11.3 to −2.3) | No effect RCT |
| (2) Usual care | DBP −2.1 (−4.8 to −0.6) | |||
| Control not reported | ||||
| Bogden et al51 | Hypertension, either: | (1) Pharmacist interacted with physicians and patients according to pre-specified checklist | SBP −12.0 (−20.1 to −3.4) | Positive RCT |
| ≥150 or ≥95mmHg | (2) Control: usual medical care | DBP −8.0 (−12.0 to −0.7) | ||
| ≥140 or ≥90 mmHg with CVS risk factors or target organ damage | Control 0.2 (0.1 to 0.5) | |||
| Garcia-Pena et al52 | Hypertension, mean SBP ≥160 or/both DBP ≥90 | (1) Nurse-based intervention: nurses trained in aging and clinical aspects of hypertension | SBP −3.3 (−5.9 to −0.7) | Positive RCT |
| (2) Usual care from institute's clinic and mailed pamphlet about hypertension | DBP −3.7 (−5.1 to −2.3) | |||
| Control 0.1 (0.1 to 0.2) | ||||
| Hawkins et al53 | Hypertension OPD clinic US (42% E) (49% C) | (1) Clinical pharmacist: chronic disease management in OPD setting (medical care monitored by general practice faculty) | SBP 0.0 (−1.9 to 1.9) | No effect RCT but improved follow-up at clinic |
| (2) Usual care by physician | DBP 0.0 (−0.7 to 0.7) | |||
| Control not reported | ||||
| Jewell et al54 | New diagnosis DBP >100 mmHg aged 30-39 years, >105 mmHg aged >40 years | (1) Nurse-led care. Agreed protocol determined treatment and frequency of attendance in both groups. Target was to reduce DBP <90 mmHg | SBP not reported | No effect RCT |
| Uncontrolled DBP >95 mmHg | (2) Usual care using same protocol | DBP not reported | ||
| Control 0.9 (0.2 to 3.6) | ||||
| Logan et al55 | Hypertension (DBP ≥95 mmHg, or DBP 91-94 mmHg and SBP >140 mmHg) | (1) Work-site care by nurse management protocol: including drug regimen and regular review | SBP not reported | Positive RCT for DBP and control of BP |
| (2) Usual care from their own family doctors | DBP −3.9 (−5.2 to −2.6) | |||
| Control 0.4 (0.3 to 0.6) | ||||
| Park et al56 | Hypertension ≥140/90 mmHg | (1) Pharmacist administered monthly patient management: education, medication changes verbal counselling and written information | SBP −13.0 (−22.6 to −3.4) | Positive RCT |
| (2) Traditional pharmacy services | DBP −5.0 (−9.9 to −0.1) | |||
| Control 0.2 (0.1 to 0.8) | ||||
| Solomon et al57 | Treated patients with hypertension | (1) Patient-centred pharmaceutical care model (employing standardised care) implemented by clinical pharmacy residents | SBP −6.9 (−12.7 to −1.1) | Positive effect SBP, no effect DBP |
| (2) Usual care | DBP −0.1 (−4.4 to 3.2) | |||
| Control not reported | ||||
| De Castro et al58 | A total of 71 patients in a single hospital clinic outpatient in Brazil. | (1) C – under routine clinical management and sham intervention | SBP −5.00 (−12.13 to 2.13) | No significant effect for SBP and DBP |
| (2) Intervention – received a pharmaceutical care programme delivered by 9 trained pharmacists: patient education and support | DBP −2.00 (−7.11 to 3.11) | |||
| Control not reported | ||||
| Schroeder et al59 | 245 women and men recruited with uncontrolled hypertension (> or = 150/90 mmHg) from 21 general practices in Bristol, UK. All patients with hypertension coded and latest BP≤150/90 | Participants were randomised to receive (1) nurse-led adherence support or (2) usual care alone. | SBP −1.70 (−6.42 to 3.02) | No effect on SBP or DBP or medication adherence |
| DBP −0.10 (−2.54 to 2.34) | ||||
| Control not reported | ||||
| Sookaneknun et al60 | Adults with hypertension from hospital and 2 primary care units | (1) Patients were monitored monthly by reviewing their medications and supported by providing pharmaceutical care and counseling. | SBP −5.70 (−10.28 to −1.12) | Positive effect for SBP, DBP and BP control |
| (2) usual care | DBP −2.50 (−5.61 to 0.61) | |||
| Control 0.69 (0.41 to 1.17) | ||||
| Tobe et al61 | Diagnosis of hypertension with SBP greater or equal to 130 mmHg | 1) Medical clinic measurement of blood pressure by home care nurse using BpTRU automated oscillometric blood pressure cuff | SBP −7.00 (−13.45 to −0.55) | Positive effect for SBP |
| DBP greater or equal to 80 mmHg | (2) Healthy lifestyle classes stressing a healthier dietary regimen, exercise, smoking cessation and drug adherence | DBP −0.80 (−5.12 to 3.52) | ||
| Diagnosis of type 2 diabetes mellitus | Control not reported | |||
| Tonstad et al62 | Subjects that participated in a health screening with systolic blood pressure 140-169 mmHg and diastolic blood pressure | Randomly allocated either to (1) monthly nurse-led lifestyle counselling (intervention group, n = 31) or to (2) conventional primary care (control group, n = 20) to be followed by lifestyle counselling. | SBP 0.00 (−5.30 to 5.30) | No effect on SBP or DBP |
| 90-99 mmHg at a minimum of three separate readings treated or not treated with antihypertensive drugs. | DBP −1.00 (−4.81 to 2.81) | |||
| Control not reported | ||||
| Bulpitt et al63 | Hypertension, mean BP | (1) Computer-held records: allowed doctor to record clinical information in structured format | SBP −0.4 (−5.9 to 5.1) | No effect RCT |
| 178/105 mmHg (intervention) | (2) Standard hospital notes | DBP 0.2 (−2.6 to 3.0) | ||
| 177/106 mmHg (Control) | Control not reported | |||
| Hypertension Detection and Follow up (HDFP)64–66 | Hypertension DBP ≥90 mmHg | (1) Stepped care, designed to provide rigorous, systematic, antihypertensive drug treatment with: free care; emphasis placed on clinic attendance and compliance; convenience; stepped drug treatment according to BP response; patients seen at intervals determined by their clinic status, at least every 4 months, and generally every 2 months | (1) Stratum 1:90-104 | Positive RCT, reduction in all cause mortality as well |
| (2) Referred care: referred to their ‘primary sources of care, usually own physicians | SBP −8.2 (−9.2 to −7.1) | |||
| DBP −4.2 (−4.7 to −3.7) | ||||
| (2) Stratum 2: 105-114 mmHg | ||||
| SBP −11.7 (−13.7 to −9.7) | ||||
| DBP −7.6 (−9.2 to −6.0) | ||||
| (3) Stratum 3: ≥115 mmHg | ||||
| SBP −10.6 (−13.7 to −7.5) | ||||
| DBP −6.5 (−7.4 to −5.6) | ||||
| Control 0.4 (0.3 to 0.5) | ||||
| Takala et al67,68 | Hypertension, aged 40-49 years, SBP ≥160 mmHg or DBP | (1) ‘Improved treatment system’ included: written instructions; card with details of BP readings, drugs prescribed, time of next appointment; appointments at 1-monthly intervals; invitation for outpatient review; appointment if defaulted on any appointment | Age 40-49 | No effect RCT but improved follow-up at clinic |
| ≥95 mmHg; aged 50-64 years, SBP ≥170 mmHg or DBP ≥105 mmHg. | (2) Usual care | SBP 3.0 (−5.1 to 11.1) | ||
| DBP 3.0 (−1.1 to −7.1) | ||||
| Age 50-59 | ||||
| SBP 3.0 (−5.5 to 11.5) | ||||
| DBP 5.0 (0.7 to 9.3) | ||||
| Control 0.5 (0.2 to 1.0) | ||||
| Turnbull et al69 | Mild to moderate hypertension and aged between 18 and 75 years. | (1) Information communication technology package for risk assessment and management, access to a dietitian commissioned by the program and a tailored set of audiovisual and written material. | SBP −0.70 (−4.41 to 3.01) | No effect on SBP and DBP and blood pressure control |
| (2) Usual care | DBP −0.10 (−1.75 to 1.55) | |||
| Control 1.90 (1.14 to 3.19) | ||||
| Wetzels et al70 | Persons were eligible if had been diagnosed with hypertension and inadequate BP control despite drugs and indication for Rx escalation | A total of 258 patients with high BP despite use of antihypertensive medication were randomly assigned to either (1) continuation of usual care or to the (2) introduction of electronic monitoring. | SBP −2.00 (−7.04 to 3.04) | No effect on SBP and DBP and blood pressure control |
| DBP −1.00 (−3.57 to 1.57) | ||||
| Control 0.69 (0.40 to 1.19) | ||||
| Ahluwalia et al71 | Patients with hypertension (SBP ≥180 mmHg and/or DBP ≥110 mmHg) | (1) Mailed reminder: postcard addressed in the presence of the patient and mailed next day as a reminder to attend clinic | Return to clinic 1.4 (0.5 to 4.4) | No effect RCT |
| (2) Given routine clinic appointment | ||||
| Barnett et al72 | Hypertension mean 150/102 mmHg | (1) Computer reminder to GP: generated automatic reminder to GP | Return to clinic 0.01 (0.0 to 0.2) | Positive RCT |
| (2) Usual care | ||||
| Bloom et al73 | Hypertension ≥140/90 mmHg | (1) Educational material about hypertension, reinforced 1 week later | Return to clinic 0.3 (0.1 to 0.9) | Positive RCT |
| (2) Usual care | ||||
| Cummings et al74 | Newly diagnosed hypertension SBP <140 mmHg and DBP >90 mmHg | (1) Appointment reminder: reminder card sent 1 week in advance of appointment and telephone patients who missed appointments to schedule new ones | Return to clinic 0.5 (0.3 to 0.7) | Positive RCT |
| (2) Usual care | ||||
| Fletcher et al75 | Hypertension DBP ≥100 mmHg | (1) Reminder (letter or phone) to attend follow up appointment at clinic, offer of assistance if problems arose, followed up until attended clinic or missed two consecutive appointments | Return to clinic 0.3 (0.2 to 0.7) | Positive RCT |
| (2) Usual care | ||||
| Krieger et al76 | Hypertension SBP ≥140 mmHg or DBP≥90 mmHg | (1) Outreach and tracking by community health worker | Return to clinic 0.5 (0.3 to 0.7) | Positive RCT |
| (2) Usual care | ||||
| Marquez et al77 | Eighty-five primary care centers in Spain, with a duration of 6 months. | (1) Control – under routine clinical management; | Mail intervention | Positive effect on SBP, DBP and blood pressure control depending on intervention |
| Patients. A total of 636 patients with newly diagnosed uncontrolled hypertension were included. | (2) Mail intervention – received a mailed message reinforcing compliance and reminding or of the visits (15 days, 2 and 4 months) | SBP −0.30 (−3.05 to 2.45) | ||
| (3) Telephone intervention – received a telephone call at 15 days, then at 7 and 15 weeks. | DBP −7.10 (−12.05 to −2.15) | |||
| Control 0.52 (0.34 to 0.79) | ||||
| Telephone intervention | ||||
| SBP −9.50 (−11.95 to −7.05) | ||||
| DBP −0.20 (−1.91 to 1.51) | ||||
| Control 0.57 (0.37 to 0.87) | ||||
| Marquez et al78 | All patients were receiving monotherapy for uncontrolled hypertension. | (1) Patients in the control group received their physician's usual interventions. | SBP 4.70 (−1.29 to 10.69) | No effect SBP, DBP and blood pressure control |
| (2) Patients in the intervention group received messages and reminders sent to their mobile phones 2 days per week during 4 months. | DBP 1.60 (−2.10 to 5.30) | |||
| Control 0.58 (0.22 to 1.54) | ||||
Outcomes: SBP and DBP mean difference in mmHg is reported. Negative figure favours intervention, positive figure favours control or usual care. Control of blood pressure measured according to treatment target definition in each RCT. Odds ratio less than one favours intervention. Return to Clinic: number of patients lost to follow-up at review. Odds ratio less than one favours intervention. BP = blood pressure. C = control. CVS = cardiovascular. DBP = diastolic blood pressure. E = experimental group. OPD = outpatient department. RCT = randomised controled trial. SBP = systolic blood pressure. TIME = Treatment Information on Medications for the Elderly.
Funding body
This study was supported by a Cochrane Fellowship awarded to the lead author by the Health Research Board of Ireland through competitive peer review.
Competing interests
The authors have stated that there are none.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV. Control of hypertension – an important national priority. N Engl J Med. 2001;345(7):534–535. doi: 10.1056/NEJM200108163450709. [DOI] [PubMed] [Google Scholar]
- 3.Burnier M. Blood pressure control and the implementation of guidelines in clinical practice: can we fill the gap? J Hypertens. 2002;20(7):1251–1253. doi: 10.1097/00004872-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Wilber JA, Barrow JG. Hypertension: a community problem. Am J Med. 1972;52(5):653–663. doi: 10.1016/0002-9343(72)90055-1. [DOI] [PubMed] [Google Scholar]
- 5.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004;329(7458):145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebrahim S. Detection, adherence and control of hypertension for the prevention of stroke: a systematic review. Health Technol Assess. 1998;2(11):i–iv. 1–78. [PubMed] [Google Scholar]
- 7.Fahey T, Schroeder K, Ebrahim S. Educational and organisational interventions used to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract. 2005;55(520):875–882. [PMC free article] [PubMed] [Google Scholar]
- 8.Higgins JPT, Altman DG. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008) 2008. The Cochrane Collaboration. [Google Scholar]
- 9.Midanik LT, Resnick B, Hurley LB, et al. Home blood pressure monitoring for mild hypertensives. Public Health Rep. 1991;106(1):85–89. [PMC free article] [PubMed] [Google Scholar]
- 10.Rudd P, Miller NH, Kaufman J, et al. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17(10):921–927. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 11.Artinian NT, Washington OG, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: a pilot study. Heart Lung. 2001;30(3):191–199. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- 12.Rogers MA, Small D, Buchan DA, et al. Home monitoring service improves mean arterial pressure in patients with essential hypertension: a randomized controlled trial. Ann Intern Med. 2001;134(11):1024–1032. doi: 10.7326/0003-4819-134-11-200106050-00008. [DOI] [PubMed] [Google Scholar]
- 13.Friedman RH, Kazis LE, Jette A, et al. A telecommunications system for monitoring and counseling patients with hypertension. Impact on medication adherence and blood pressure control. Am J Hypertens. 1996;9(4 Pt 1):285–292. doi: 10.1016/0895-7061(95)00353-3. [DOI] [PubMed] [Google Scholar]
- 14.Halme L, Vesalainen R, Kaaja M, et al. Self-monitoring of blood pressure promotes achievement of blood pressure target in primary health care. Am J Hypertens. 2005;18(11):1415–1420. doi: 10.1016/j.amjhyper.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 15.McManus RJ, Mant J, Roalfe A, et al. Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. BMJ. 2005;331(7515):493. doi: 10.1136/bmj.38558.393669.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carnahan JE, Nugent CA. The effects of self-monitoring by patients on the control of hypertension. Am J Med Sci. 1975;269(1):69–73. doi: 10.1097/00000441-197501000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Soghikian K, Casper SM, Fireman BH, et al. Home blood pressure monitoring. Effect on use of medical services and medical care costs. Med Care. 1992;30(9):855–865. [PubMed] [Google Scholar]
- 18.Bailey B, Carney SL, Gillies AA, Smith AJ. Antihypertensive drug treatment: a comparison of usual care with self blood pressure measurement. J Hum Hypertens. 1998;13(2):147–150. doi: 10.1038/sj.jhh.1000758. [DOI] [PubMed] [Google Scholar]
- 19.Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000;20(11):1384–1389. doi: 10.1592/phco.20.17.1384.34891. [DOI] [PubMed] [Google Scholar]
- 20.Vetter W, Hess L, Brignoli R. Influence of self-measurement of blood pressure on the responder rate in hypertensive patients treated with losartan: results of the SVATCH study. J Hum Hypertens. 2000;14:235–241. doi: 10.1038/sj.jhh.1000977. [DOI] [PubMed] [Google Scholar]
- 21.Haynes RB, Sackett DL, Gibson ES, et al. Improvement of medication compliance in uncontrolled hypertension. Lancet. 1976;1(7972):1265–1268. doi: 10.1016/s0140-6736(76)91737-2. [DOI] [PubMed] [Google Scholar]
- 22.Johnson AL, Taylor DW, Sackett DL, et al. Self-recording of blood pressure in the management of hypertension. Can Med Assoc J. 1978;119(9):1034–1039. [PMC free article] [PubMed] [Google Scholar]
- 23.Pierce JP, Watson DS, Knights S, et al. A controlled trial of health education in the physician's office. Prev Med. 1984;13(2):185–194. doi: 10.1016/0091-7435(84)90050-1. [DOI] [PubMed] [Google Scholar]
- 24.Earp JA, Ory MG, Strogatz DS. The effects of family involvement and practitioner home visits on the control of hypertension. Am J Pub Health. 1982;72(10):1146–1154. doi: 10.2105/ajph.72.10.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dalfói Baqué A, Capillas Peréz R, Guarch Rocarias M, et al. [Effectiveness of self-measurement of blood pressure in patients with hypertension: the Dioampa study] Aten Primaria. 2005;35(5):233–237. doi: 10.1157/13072786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zarnke K, Feagan B, Mahon J, Feldman R. A randomized study comparing a patient-directed hypertension management strategy with usual office-based care. Am J Hypertension. 1997;10:58–67. doi: 10.1016/s0895-7061(96)00305-6. [DOI] [PubMed] [Google Scholar]
- 27.Billault B, Degoulet P, Devries C, et al. Use of a standardized personal medical record by patients with hypertension: a randomized controlled prospective trial. MD Comput. 1995;12(1):31–35. [PubMed] [Google Scholar]
- 28.Burrelle TN. Evaluation of an interdisciplinary compliance service for elderly hypertensives. J Geriatr Drug Ther. 1986;1(2):23–51. [Google Scholar]
- 29.Cakir H, Pinar R. Randomized controlled trial on lifestyle modification in hypertensive patients. West J Nurs Res. 2006;28(2):190–209. doi: 10.1177/0193945905283367. [DOI] [PubMed] [Google Scholar]
- 30.Fielding JE, Knight K, Mason T, et al. Evaluation of the IMPACT blood pressure program. J Occup Med. 1994;36(7):743–746. [PubMed] [Google Scholar]
- 31.Hennessy S, Leonard CE, Yang W, et al. Effectiveness of a two-part educational intervention to improve hypertension control: a cluster-randomized trial. Pharmacotherapy. 2006;26(9):1342–1347. doi: 10.1592/phco.26.9.1342. [DOI] [PubMed] [Google Scholar]
- 32.Hunt JS, Siemienczuk J, Touchette D, Payne N. Impact of educational mailing on the blood pressure of primary care patients with mild hypertension. J Gen Intern Med. 2004;19(9):925–930. doi: 10.1111/j.1525-1497.2004.40046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKinstry B, Hanley J, Heaney D, et al. Impact on hypertension control of a patient-held guideline: a randomised controlled trial. Br J Gen Pract. 2006;56(532):842–847. [PMC free article] [PubMed] [Google Scholar]
- 34.Mühlhauser I, Sawicki PT, Didjurgeit U, et al. Evaluation of a structured treatment and teaching programme on hypertension in general practice. Clin Exp Hypertens. 1993;15(1):125–142. doi: 10.3109/10641969309041615. [DOI] [PubMed] [Google Scholar]
- 35.Roca-Cusachs A, Sort D, Altimira J, et al. The impact of a patient education programme in the control of hypertension. J Hum Hypertens. 1991;5(5):437–441. [PubMed] [Google Scholar]
- 36.Watkins CJ, Papacosta AO, Chinn S, Martin J. A randomized controlled trial of an information booklet for hypertensive patients in general practice. J R Coll Gen Pract. 1987;37(305):548–550. [PMC free article] [PubMed] [Google Scholar]
- 37.Zismer DK, Gillum RF, Johnson CA, et al. Improving hypertension control in a private medical practice. Arch Intern Med. 1982;142(2):297–299. [PubMed] [Google Scholar]
- 38.Tanner GA, Noury DJ. The effect of instruction on control of blood pressure in individuals with essential hypertension. J Adv Nurs. 1981;6(2):99–106. doi: 10.1111/j.1365-2648.1981.tb03198.x. [DOI] [PubMed] [Google Scholar]
- 39.Webb PA. Effectiveness of patient education and psychosocial counseling in promoting compliance and control among hypertensive patients. J Fam Pract. 1980;10(6):1047–1055. [PubMed] [Google Scholar]
- 40.Morisky DE, Levine DM, Green LW, et al. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983;73(2):153–162. doi: 10.2105/ajph.73.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sackett DL, Haynes RB, Gibson ES, et al. Randomised clinical trial of strategies for improving medication compliance in primary hypertension. Lancet. 1975;1(7918):1205–1207. doi: 10.1016/s0140-6736(75)92192-3. [DOI] [PubMed] [Google Scholar]
- 42.Dickinson JC, Warshaw GA, Gehlbach SH, et al. Improving hypertension control: impact of computer feedback and physician education. Med Care. 1981;19(8):843–854. doi: 10.1097/00005650-198108000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Coe FL, Norton E, Oparil S, et al. Treatment of hypertension by computer and physician – a prospective controlled study. J Chronic Dis. 1977;30(2):81–92. doi: 10.1016/0021-9681(77)90077-7. [DOI] [PubMed] [Google Scholar]
- 44.Evans CE, Haynes RB, Birkett NJ, et al. Does a mailed continuing education program improve physician performance? Results of a randomized trial in antihypertensive care. JAMA. 1986;255(4):501–504. [PubMed] [Google Scholar]
- 45.Hetlevik I, Holmen J, Krüger O. Implementing clinical guidelines in the treatment of hypertension in general practice. Evaluation of patient outcome related to implementation of a computer-based clinical decision support system. Scand J Prim Health Care. 1999;17(1):35–40. doi: 10.1080/028134399750002872. [DOI] [PubMed] [Google Scholar]
- 46.McAlister NH, Covvey HD, Tong C, et al. Randomised controlled trial of computer assisted management of hypertension in primary care. Br Med J (Clin Res Ed) 1986;293(6548):670–674. doi: 10.1136/bmj.293.6548.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Montgomery AA, Fahey T, Peters TJ, et al. Evaluation of a computer-based clinical decision support system and chart guidelines in the management of hypertension in primary care: a randomised controlled trial. BMJ. 2000;320(7236):686–690. doi: 10.1136/bmj.320.7236.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ornstein S, Jenkins RG, Nietert PJ, et al. A multimethod quality improvement intervention to improve preventive cardiovascular care: a cluster randomized trial. Ann Intern Med. 2004;141(7):523–532. doi: 10.7326/0003-4819-141-7-200410050-00008. [DOI] [PubMed] [Google Scholar]
- 49.New JP, Mason JM, Freemantle N, et al. Educational outreach in diabetes to encourage practice nurses to use primary care hypertension and hyperlipidaemia guidelines (EDEN): a randomized controlled trial. Diabet Med. 2004;21(6):599–603. doi: 10.1111/j.1464-5491.2004.01213.x. [DOI] [PubMed] [Google Scholar]
- 50.Sanders KM, Satyvavolu A. Improving blood pressure control in diabetes: limitations of a clinical reminder in influencing physician behaviour. J Contin Edu Health Prof. 2002;22(1):23–32. doi: 10.1002/chp.1340220104. [DOI] [PubMed] [Google Scholar]
- 51.Bogden PE, Abbott RD, Williamson P, et al. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med. 1998;13(11):740–745. doi: 10.1046/j.1525-1497.1998.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Garcia-Peña C, Thorogood M, Armstrong B, et al. Pragmatic randomized trial of home visits by a nurse to elderly people with hypertension in Mexico. Int J Epidemiol. 2001;30(6):1485–1491. doi: 10.1093/ije/30.6.1485. [DOI] [PubMed] [Google Scholar]
- 53.Hawkins D, Fridler F, Douglas H, et al. Evaluation of a clinical pharmacist in caring for hypertensive and diabetic patients. Am J Hosp Pharm. 1979;36(10):1321–1325. [PubMed] [Google Scholar]
- 54.Jewell D, Hope J. Evaluation of a nurse-run hypertension clinic in general practice. Practitioner. 1988;232(1447):484–487. [PubMed] [Google Scholar]
- 55.Logan AG, Milne BJ, Achber C, et al. Work-site treatment of hypertension by specially trained nurses. A controlled trial. Lancet. 1979;2(8153):1175–1178. doi: 10.1016/s0140-6736(79)92397-3. [DOI] [PubMed] [Google Scholar]
- 56.Park JJ, Kelly P, Carter BL, Burgess PP. Comprehensive pharmaceutical care in the chain setting. J Am Pharm Assoc (Wash) 1996;NS36(7):443–451. doi: 10.1016/s1086-5802(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 57.Solomon DK, Portner TS, Bass GE, et al. Clinical and economic outcomes in the hypertension and COPD arms of a multicenter outcomes study. J Am Pharm Assoc (Wash) 1998;38(5):574–584. doi: 10.1016/s1086-5802(16)30371-0. [DOI] [PubMed] [Google Scholar]
- 58.De Castro MS, Fuchs FD, Santos MC, et al. Pharmaceutical care program for patients with uncontrolled hypertension. Report of a double–blind clinical trial with ambulatory blood pressure monitoring. Am J Hypertens. 2006;19(5):528–533. doi: 10.1016/j.amjhyper.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 59.Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: a randomized controlled trial. Fam Pract. 2005;22(2):144–151. doi: 10.1093/fampra/cmh717. [DOI] [PubMed] [Google Scholar]
- 60.Sookaneknun P, Richards RM, Sanguansermsri J, Teerasut C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann Pharmacother. 2004;38(12):2023–2028. doi: 10.1345/aph.1D605. [DOI] [PubMed] [Google Scholar]
- 61.Tobe SW, Pylypchuk G, Wentworth J, et al. Effect of nurse-directed hypertension treatment among First Nations people with existing hypertension and diabetes mellitus: the Diabetes Risk Evaluation and Microalbuminuria (DREAM 3) randomized controlled trial. CMAJ. 2006;174(9):1267–1271. doi: 10.1503/cmaj.050030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tonstad S, Alm CS, Sandvik E. Effect of nurse counselling on metabolic risk factors in patients with mild hypertension: a randomised controlled trial. Eur J Cardiovasc Nurs. 2007;6(2):160–164. doi: 10.1016/j.ejcnurse.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 63.Bulpitt CJ, Beilin LJ, Coles EC, et al. Randomised controlled trial of computer-held medical records in hypertensive patients. Br Med J. 1976;1(6011):677–679. doi: 10.1136/bmj.1.6011.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hypertension Detection and Follow-up Program. Therapeutic control of blood pressure in the Hypertension Detection and Follow-up Program. Hypertension Detection and Follow-up Program Cooperative Group. Prev Med. 1979;8(1):2–13. doi: 10.1016/0091-7435(79)90024-0. [DOI] [PubMed] [Google Scholar]
- 65.Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562–2571. [PubMed] [Google Scholar]
- 66.Hypertension detection and follow-up Program Cooperative Group. The effect of treatment on mortality in ‘mild’ hypertension: results of the hypertension detection and follow-up program. N Engl J Med. 1982;307(16):976–980. doi: 10.1056/NEJM198210143071603. [DOI] [PubMed] [Google Scholar]
- 67.Takala J, Niemelä N, Rosti J, Sievers K. Improving compliance with therapeutic regimens in hypertensive patients in a community health center. Circulation. 1979;59(3):540–543. doi: 10.1161/01.cir.59.3.540. [DOI] [PubMed] [Google Scholar]
- 68.Takala J. Screening, treatment and adherence to treatment for hypertension. Scand J Prim Health Care. 1983;1(3–4):114–119. doi: 10.3109/02813438309038478. [DOI] [PubMed] [Google Scholar]
- 69.Turnbull DA, Beilby JJ, Ziaian T, et al. Disease management for hypertension: a pilot cluster randomized trial of 67 Australian general practices. Disease Management and Health Outcomes. 2006;14(1):27–35. [Google Scholar]
- 70.Wetzels GE, Nelemans PJ, Schouten JS, et al. Electronic monitoring of adherence as a tool to improve blood pressure control. A randomized controlled trial. Am J Hypertens. 2007;20(2):119–125. doi: 10.1016/j.amjhyper.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 71.Ahluwalia JS, McNagny SE, Kanuru NK. A randomized trial to improve follow-up care in severe uncontrolled hypertensives at an inner-city walk-in clinic. J Health Care Poor Underserved. 1996;7(4):377–389. doi: 10.1353/hpu.2010.0216. [DOI] [PubMed] [Google Scholar]
- 72.Barnett GO, Winickoff RN, Morgan MM, Zielstorff RD. A computer-based monitoring system for follow-up of elevated blood pressure. Med Care. 1983;21(4):400–409. doi: 10.1097/00005650-198304000-00003. [DOI] [PubMed] [Google Scholar]
- 73.Bloom JR, Jordan SC. From screening to seeking care: removing obstacles in hypertension control. Prev Med. 1979;8(4):500–506. doi: 10.1016/0091-7435(79)90324-4. [DOI] [PubMed] [Google Scholar]
- 74.Cummings KM, Frisof KB, Demers P, Walsh D. An appointment reminder system's effect on reducing the number of hypertension patients who drop out from care. Am J Prev Med. 1985;1(5):54–60. [PubMed] [Google Scholar]
- 75.Fletcher SW, Appel FA, Bourgeois MA. Management of hypertension. Effect of improving patient compliance for follow-up care. JAMA. 1975;233(3):242–244. doi: 10.1001/jama.233.3.242. [DOI] [PubMed] [Google Scholar]
- 76.Krieger J, Collier C, Song L, Martin D. Linking community-based blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health. 1999;89(6):856–861. doi: 10.2105/ajph.89.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Márquez Contreras E, Vegazo Garcia O, Claros NM, et al. Efficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension. ETECUM–HTA study. Blood Press. 2005;14(3):151–158. doi: 10.1080/08037050510008977. [DOI] [PubMed] [Google Scholar]
- 78.Márquez Contreras E, de la Figuera Von Wichmann M, Gil Guillén V, et al. [Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert)] Aten Primaria. 2004;34(8):399–405. doi: 10.1016/S0212-6567(04)78922-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52(1):10–29. doi: 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PubMed] [Google Scholar]
- 80.Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162(4):413–420. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 81.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]


