Abstract
Background
Cardiovascular diseases (CVD) are the main cause of death and disability in developed countries. In most cases, the progress of CVD is influenced by environmental factors and multifactorial inheritance. The purpose of this study was to investigate the association between APOE genotypes, cardiovascular risk factors, and a non-invasive measure of arterial stiffness in the Brazilian population.
Methods
A total of 1493 urban Brazilian individuals were randomly selected from the general population of the Vitoria City Metropolitan area. Genetic analysis of the APOE polymorphism was conducted by PCR-RFLP and pulse wave velocity analyzed with a noninvasive automatic device.
Results
Age, gender, body mass index, triglycerides, creatinine, uric acid, blood glucose, blood pressure phenotypes were no different between ε2, ε3 and ε4 alleles. The ε4 allele was associated with higher total-cholesterol (p < 0.001), LDL-C (p < 0.001), total-cholesterol/HDL-C ratio (p < 0.001), LDL/HDL-C ratio (p < 0.001), lower HDL-C values (p < 0.001) and higher risk to obesity (OR = 1.358, 95% CI = 1.019-1.811) and hyperuricemia (OR = 1.748, 95% CI = 1.170-2.611). Nevertheless, pulse wave velocity (p = 0.66) measures were no different between genotypes. The significant association between APOE genotypes and lipid levels persisted after a 5-year follow-up interval, but no interaction between time and genotype was observed for lipids longitudinal behavior.
Conclusion
The ε4 allele of the APOE gene is associated with a worse lipid profile in the Brazilian urban population. In our relatively young sample, the observed effect of APOE genotype on lipid levels was not translated into significant effects in arterial wall stiffness.
Background
Cardiovascular diseases (CVD) are the main cause of death and disability in developed countries. In most cases, the progress of CVD is influenced by multifactorial inheritance and environmental factors [1-4]. Lipoprotein disorders such as elevated low-density lipoprotein cholesterol (LDL-C ≥ 160 mg/dL), low high-density lipoprotein cholesterol (HDL-C < 40 mg/dL) and elevated concentration of triglycerides (TG ≥ 150 mg/dL) are considered significant risk factors in the pathogenesis of CVD [5].
Apolipoprotein E (ApoE) is a glycoprotein that plays a fundamental role in the lipid metabolism. ApoE participates in the clearance of chylomicron remmants and very low-density lipoprotein (VLDL) by serving as a ligand for LDL receptors[6]. It is also important for intestinal cholesterol absorption[7] and plasma lipid maintenance[8]. The APOE gene, located on chromosome 19[9], is composed by three alleles (ε2, ε3 and ε4) that give rise to six different genotypes (ε2/2, ε2/3, ε2/4, ε3/3, ε3/4, and ε4/4)[6]. The ε3 allele differs from the ε2 allele by an amino acid substitution of arginine for cysteine at codon 158, while the ε4 differs from ε3 by a substitution of arginine for cysteine at residue 112[10-12]. Many studies assessing the role of APOE polymorphism on plasma lipids have shown that the presence of the ε4 allele is associated with elevations in LDL-C, while the presence of ε2 is associated with decreased levels of LDL-C[13]. Moreover, some studies have reported that the ε4 allele is associated with coronary heart disease[14] although most of these have been carried out in male subjects.
After the discovery of the APOE gene and knowledge of its genetic variants, several studies have demonstrated the association between the APOE polymorphisms and chronic conditions, such as Alzheimer's disease[15], age-related cognitive decline[16], osteoporosis[17], breast cancer[18], end-stage renal disease[19], atherosclerosis[8], diabetes[20], coronary disease[21] and longevity[22]. Based on these, we aimed to assess the relation between APOE genotype groups with the prevalence of the major CVD risk factors and its possible association with the evolution of the studied phenotypes in a longitudinal study of Brazilian subjects randomly selected from an ethnically mixed urban population.
Our hypothesis was that individuals carrying the ε4 allele had a worse lipid profile when compared with ε2 and ε3 alleles carriers of the APOE polymorphism and that this worse profile would be translated into significantly different measures of arterial stiffness.
Methods
Study Design and Participants
A cross-sectional study of risk factors for cardiovascular diseases was performed in the urban population of the Vitória city, Brazil, using the WHO-MONICA project guidelines[23]. In the first stage of the study, conducted in 1999, 1493 Brazilians of either gender, aged 25 to 64 years were chosen according to the nearest birthday[24]. All participants were submitted to complete clinical and laboratorial investigations for CVD risk factors.
This study was approved by the Ethics Committee for Research on Human Subject of the Espírito Santo Federal University, and all subjects gave written informed consent to participate.
Risk Factors Assessment
Anthropometrical Investigations
Weight and height were measured according to a standard protocol, with participants wearing light clothing and no shoes. Height was measured in centimeters and weight in kilograms using a calibrated balance. Body mass index (BMI) was calculated and obesity defined as BMI ≥ 30Kg/m2[25]. Individuals who had ever smoked more than five cigarettes per day for the last year were classified as smokers[26]. Participants were also submitted to an ethnic classification according to a validated questionnaire for the Brazilian population[27]. Subjects were classified as Caucasian or Afro-descendent according to a set of phenotypic characteristics (skin color, hair texture, shape of the nose and aspect of the lip). On the basis of these characteristics, mulattos are considered racially mixed subjects.
Blood Pressure Phenotype Determination
Blood pressure was measured in the sitting position with the use of a standard mercury sphygmomanometer on the left arm after 5 minutes' rest. The first and fifth phases of Korotkoff sounds were used for systolic (SBP) and diastolic pressure (DBP), respectively. The SBP and DBP were calculated from two readings with a minimal interval of 10 minutes. Hypertension was defined as mean SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg or use of anti-hypertension drugs [28]. Pulse pressure (PP) was the difference between SBP and DBP. The mean blood pressure (MBP) was calculated as the mean pulse pressure added to one-third of the DBP.
Pulse wave measurements
The Carotid-femoral pulse wave velocity (PWV) was analyzed with a noninvasive automatic device (Complior; Colson; Garges les Gonesses, France) by an experienced observer blinded to the clinical characteristics. Briefly, common carotid artery and femoral artery pressure waveforms were recorded noninvasively using a pressure- sensitive transducer (TY-306-Fukuda; Fukuda; Tokyo, Japan). The distance between the recording sites (D) was measured, and PWV was automatically calculated as PWV = D/t, where (t) means pulse transit time. Thirty measurements were repeated over 10 different cardiac cycles, and the mean is used for the final analysis. Because systolic BP has direct influence on PWV, we also adjusted PWV for the mean systolic BP in all groups. The validation of this automatic method and its reproducibility has been previously described[29].
Biochemical Measurement
Blood glucose, TG, lipoprotein fractions and uric acid were assayed by standard techniques in 12-h fasting blood samples [30].This study, diabetes was defined as fasting glucose ≥ 126 mg/dL or use of hypoglycemic drugs. Abnormal biochemical levels were identified when total-cholesterol (TC) ≥ 200 mg/dL, TG ≥ 150 mg/dL, LDL-C ≥ 160 mg/dL, HDL-C < 40 mg/dL and uric acid ≥ 7.0 mg/dL[5,31].
DNA Extraction and APOE genotyping
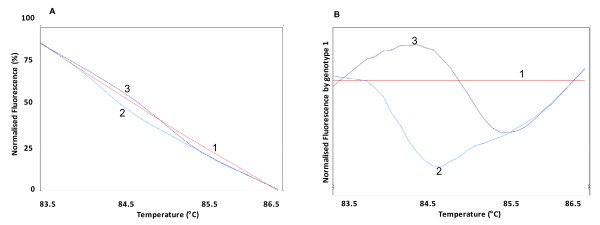
Genomic DNA was extracted from leukocytes in samples of whole blood, following a standard salting-out technique[32]. Genotypes were detected by polymerase chain reaction followed by restriction fragment length polymorphism analysis as previously described[33]. In addition, we have genotyped samples for the APOE polymorphisms (rs7412 and rs429358) by an additional method (HRM analysis - high resolution melting). Briefly, PCR with a fluorescent DNA-intercalating SYTO9® (Invitrogen, Carlsbad, USA) was performed using the primer sequences 5'-GCCGATGACCTGCAGAAG-3' and 5'-CACGCGGCCCTGTTCCAC-3' (fragment size 117 pairs base) and 5'-GCGGACATGGAGGACGTG-3' and 5'- AGCTCCTCGGTGCTCTGG-3' (fragment size 83 pairs base), for rs7412 and rs429358, respectively. In the HRM phase, Rotor Gene 6000® (Qiagen, Courtaboeuf, France) measured the fluorescence in each 0.1°C temperature increase in the range of 70-94°C. Melting curves were generated by the decrease in fluorescence with the increase in the temperature; nucleotide changes resulting from different curve patterns were analyzed and genotyped (Figure 1). Samples of the three observed curves were sequenced (ABI 3500XL Sequencer®, Applied Biosystems, Foster City, CA, USA) to confirm the genotypes indicated by HRM.
Figure 1.
Genotyping of rs7412 through HRM analysis. A: Normalized fluorescence by temperature. B: Normalized fluorescence (based on genotype 1) by temperature. 1: wild-type genotype; 2: heterozygous genotype; 3: homozygous genotype for the APOE rs7412 polymorphism.
Quality control for the APOE polymorphisms (rs7412 and rs429358) was assessed by randomly selecting 96 samples to be re-genotyped using a high resolution melting method (HRM analysis, Rotor Gene 6000®, Qiagen, Courtaboeuf, France) by two independent technicians and these results were 100% concordant.
Statistical Analysis
To evaluate the effect of APOE genotypes on cardiovascular risk factors, subjects were categorized into three groups: ε2 carriers (ε2/ε2 + ε2/ε3 genotypes), ε3 carriers (ε3/ε3 genotype) and ε4 carriers (ε4/ε4 + ε3/ε4 genotypes)[34]. In each model, the homozygous ε3/ε3 genotypes formed the reference group. Thirty-two individuals (2.3%) with ε2/ε4 genotype were excluded from the analysis because of the putative opposite effects of these two alleles on LDL-C levels [35].
Differences in the baseline cardiovascular risk characteristics across the APOE groups were tested by One-Way ANOVA for continuous variables, and χ2 test for categorical parameters. Table 1 shows the comparison of data among all allelic groups. All variables were adjusted for ethnicity, age and gender, except the PWV was adjusted for age, SBP and ethnicity.
Table 1.
Baseline characteristics of participants encoding ε2, ε3 and ε4 alleles of the APOE polymorphism.
| Subject Characteristics n, (%) | ε2 180 (12.3%) | ε3 893 (61.1%) | ε4 388 (26.6%) | p value |
|---|---|---|---|---|
| Gender, male | 76 (42.2%) | 433 (48.5%) | 169 (43.6%) | 0.13 |
| Ethnicity | ||||
| African descendent | 19 (15.6%) | 63 (51.6%) | 40 (32.8%) | |
| Caucasian descendent | 50 (9.1%) | 367 (67.0%) | 131 (23.9%) | 0.002 |
| Mulatto | 111 (14.1%) | 463 (58.5%) | 217 (27.4%) | |
| Smoking status, smokers (%) | 43 (23.9%) | 211 (23.6%) | 101 (26.0%) | 0.66 |
| Diabetes (%) | 13 (7.2%) | 70 (7.8%) | 34 (8.7%) | 0.81 |
| Age, years | 43.8 ± 10.6 | 45.1 ± 10.9 | 44.5 ± 10.8 | 0.28 |
| BMI, kg/m2 | 25.8 ± 4.7 | 26.3 ± 4.9 | 26.4 ± 4.9 | 0.27 |
| SBP, mmHg | 125.9 ± 19.7 | 128.1 ± 21.5 | 129.4 ± 22.6 | 0.15 |
| DBP, mmHg | 83.3 ± 13.9 | 84.5 ± 14.1 | 85.1 ± 14.1 | 0.34 |
| PP, mmHg | 42.6 ± 11.4 | 43.7 ± 13.7 | 44.3 ± 14.3 | 0.34 |
| MBP, mmHg | 97.5 ± 15.2 | 99.0 ± 15.8 | 99.8 ± 16.1 | 0.21 |
| PWV, m/s | 10.0 ± 2.1 | 9.8 ± 2.2 | 9.8 ± 2.1 | 0.66 |
| Triglycerides, mg/dL | 133.7 ± 99.1 | 133.9 ± 124.4 | 145.9 ± 148.6 | 0.28 |
| Total cholesterol, mg/dL | 201.4 ± 50.6 | 215.2 ± 48.3* | 218.6 ± 44.6† | < 0.001 |
| HDL - C, mg/dL | 48.8 ± 14.6 | 45.5 ± 12.7* | 43.2 ± 10.1†‡ | < 0.001 |
| LDL - C, mg/dL | 125.3 ± 35.8 | 143.6 ± 38.9* | 147.9 ± 39.6† | < 0.001 |
| VLDL - C, mg/dL | 25.3 ± 17.2 | 25.5 ± 22.9 | 26.2 ± 15.5 | 0.81 |
| Total cholesterol/HDL - C ratio | 4.3 ± 1.4 | 5.0 ± 1.5* | 5.3 ± 1.5† | < 0.001 |
| LDL - C/HDL - C ratio | 2.8 ± 1.0 | 3.4 ± 1.2* | 3.6 ± 1.3†‡ | < 0.001 |
| Glucose, mg/dL | 103.9 ± 30.1 | 105.8 ± 33.0 | 104.4 ± 31.0 | 0.64 |
| Creatinine, mg/dL | 0.99 ± 0.19 | 0.97 ± 0.20 | 0.96 ± 0.20 | 0.16 |
| Uric acid, mg/dL | 4.7 ± 1.4 | 4.8 ± 1.5 | 5.0 ± 1.6† | 0.04 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pressure pulse; MBP, mean blood pressure; PWV, pulse wave velocity; HDL - C, high-density lipoprotein cholesterol; LDL - C, low-density lipoprotein cholesterol; VLDL - C, very-low-density lipoprotein cholesterol.
ε2 allele = ε2/ε2 + ε2/ε3 genotypes; ε3 allele = ε3/ε3 genotype; ε4 allele = ε3/ε4 + ε4/ε4 genotypes
* ε2 vs ε3, p < 0.05; † ε2 vs ε4, p < 0.05; ‡ ε3 vs ε4, p < 0.05.
All values were adjusted for ethnicity, age and gender except the PWV was adjusted for age, SBP and ethnicity.
Logistic regression analysis was carried out to estimate the odds ratio (OR), with 95% confidence intervals (CI), in order to assess genetic risk factors for common cardiovascular risk. The risk analysis was performed comparing all three groups together. In the Table 2, we present risk estimative for E2 and E4 allele carriers against all other allele groups.
Table 2.
Analysis of the cardiovascular risk factors associated with APOE polymorphism
| APOE ALLELES | ||||||
| ε2 | ε4 | |||||
| VARIABLES | OR | CI 95% | p value | OR | CI 95% | p value |
| Total cholesterol | 0.44 | 0.319 - 0.618 | < 0.001 | 1.571 | 1.218 - 2.026 | 0.001 |
| HDL - C | 0.584 | 0.400 - 0.854 | 0.005 | 1.271 | 0.982 - 1.644 | 0.07 |
| LDL - C | 0.401 | 0.262 - 0.614 | < 0.001 | 1.738 | 1.343 - 2.250 | < 0.001 |
| Uric Acid | 0.500 | 0.237 - 1.056 | 0.07 | 1.748 | 1.170 - 2.611 | 0.006 |
| SBP | 0.786 | 0.526 -1.173 | 0.13 | 1.140 | 0.858 - 1.515 | 0.37 |
| DBP | 1.096 | 0.776 - 1.549 | 0.60 | 0.968 | 0.745 - 1.257 | 0.81 |
| BMI | 0.717 | 0.466 - 1.104 | 0.13 | 1.358 | 1.019 - 1.811 | 0.04 |
Adjusted values for ethnicity, gender and age.
Quantitative variables were expressed as the mean ± standard deviation, while qualitative variables were expressed as percentage. Hardy-Weinberg equilibrium for the distribution of the genotype groups was estimated using the Haploview software. All statistical analyses were carried out using SPSS software (v. 16.0), with the level of significance set at p < 0.05.
Results
The frequency of APOE genotypes among 1461 participants were: ε2/ε2 - 0.4%, ε2/ε3 - 9.7%, ε2/ε4 - 2.3%, ε3/ε3 - 61.0%, ε3/ε4 - 24.4% and ε4/ε4 - 2.2%. The allele frequencies were: ε2 - 10.1%, ε3 - 61.0% and ε4 - 26.6%. The genotype distributions for APOE polymorphisms (rs7412 and rs429358) were in Hardy-Weinberg equilibrium (p > 0.05). The ethnicity proportion was different among the APOE allele groups (p = 0.002), where the number of Caucasians is higher than Afro-descendent in the ε3 allele group (67.0% vs. 51.6%, respectively). Comparative analysis failed to indicate a significant difference among APOE groups and age (p = 0.28), gender (p = 0.13), diabetes (p = 0.81) and smoking status (p = 0.66) (Table 1).
Association Between Hemodynamic Phenotypes and APOE Polymorphism
Hemodynamic phenotypes of SBP (p = 0.15), DBP (p = 0.34), MBP (p = 0.21), PP (p = 0.34) and PWV (p = 0.66) showed no association with APOE allele groups (Table 1). Similarly, risk analysis performed by multiple logistic regression failed to detect significant genetic risk for high SBP (ε2 carriers: OR = 0.786, 95% CI = 0.526-1.173, ε4 carriers: OR = 1.140, 95% CI = 0.858-1.515) and high DBP (ε2 carriers: OR = 1.096, 95% CI = 0.776-1.549) and ε4 carriers: OR = 0.968, 95% CI = 0.745-1.257) (Table 2).
Association Between Biochemical and Metabolic Phenotypes and APOE Polymorphism
Biochemical measurement of TC, LDL-C, HDL-C, TC/HDL ratio and LDL-C/HDL and uric acid were associated with the APOE polymorphism, even after adjustment for ethnicity, age and gender. Values of TC (p < 0.001), LDL-C (p < 0.001), TC/HDL ratio (p < 0.001) and LDL/HDL-C ratio were higher in ε4 and ε3 when compared to ε2 allele carriers. However, for TC, LDL-C and TC/HDL-C no difference was observed between ε2 and ε3 alleles (p > 0.05). The HDL-C values (p < 0.001) were lower in ε4 and ε3 alleles when compared with ε2 allele carriers. In addition, ε3 carriers showed higher HDL-C values when compared with ε4 allele carriers. The uric acid values (p = 0.04) were lower in ε2 allele when compared with ε4 allele carriers. Other variables, such as TG (p = 0.28), VLDL-C (p = 0.81), glucose (p = 0.64), creatinine (p = 0.16) and BMI (p = 0.27) failed to show association with APOE groups (Table 1).
The ε2 allele confers protection for high TC (OR = 0.444, 95% CI = 0.319-0.618), low HDL-C (OR = 0.584, 95% CI = 0.400-0.854), high LDL-C (OR = 0.401, 95% CI = 0.262-0.614), while ε4 allele confers risk for elevated levels of TC (OR = 1.571, 95% CI = 1.218-2.026), LDL-C (OR = 1.738, 95% CI = 1.343-2.250), uric acid (OR = 1.748, 95% CI = 1.170-2.611) and BMI (OR = 1.358, 95% CI = 1.019-1.811) (Table 2).
Discussion
The main finding of the present study was that APOE genetic variability is associated with cardiovascular risk factors in a Brazilian urban population. Increased LDL-C, TC, TC/HDL-C ratio, LDL-C/HDL-C ratio and decreased HDL-C values were observed in individuals harboring the ε4 allele. However, this genetic variant was not associated with the arterial stiffness phenotype.
Corroborating our results, Medina-Urrutia et al[13] demonstrated associations between the ε4 allele of the APOE polymorphism and higher concentrations of TC, LDL-C and lower HDL-C levels when compared with the ε2 allele carriers in Mexican adolescents. Similarly, Shu Liang et al[36] studying 168 healthy Chinese individuals showed associations between the ε4 allele with increased TC and LDL-C values. However, HDL-C was not associated with the genetic variant studied. In the Brazilian population, de-Andrade et al[37] studying individuals of both genders described associations between the ε4 allele and higher TG and total and non-HDL levels only in women. Additionally, Mendes-Lana et al[38] showed that ε4 allele carriers present increased risk for dyslipidemia when compared to ε2 allele carriers. However, De França et al[39] failed to demonstrate an association between the ε4 allele with increased TC and LDL-C values in healthy children, suggesting that at least part of the described effect is age-dependent. In fact, although a large number of studies show associations between APOE polymorphisms with cardiovascular risk and lipid profile phenotypes in different populations [40,41], some studies failed to demonstrate this association [42,43].
Some functional studies may help in explaining our findings. Miettinen et al[44] found a significant higher cholesterol absorption in subjects with ε3 and ε4 alleles compared with those carrying the ε2 allele after a normal diet. In addition, Weintraub et al[45] showed that the slower hepatic clearance of dietary fat in ε2/3 subjects could result in up-regulation of LDL receptors and a subsequent decrease in plasma LDL-C levels.
Arterial stiffness and hypertension are the most important risk factors for cardiovascular diseases [2,46]. Several studies have demonstrated association of these with the metabolic profile [47,48]. The present study failed to demonstrate an association between APOE polymorphisms with blood pressure phenotypes and arterial stiffness. Corroborating some results of this study, Fuzikawa et al[49]studied 1406 Brazilian elderly individuals and found no association between APOE genotype and hypertension. Similarly, Carmo-Martins et al[50] studied 672 Portuguese subjects and failed to demonstrated an association with blood pressure.
Focusing on the arterial stiffness, studies[51] have showed that the unfavorable lipid profile is associated with lower arterial complacence due to reduced NO bioavailability induced by dyslipidemia. Thus, we expected ε4 allele carriers of the APOE polymorphism would have a higher arterial stiffness when compared to ε2 allele carriers. However, this was not evident in this study, perhaps due to the little difference in mean lipid fractions between the groups as well as the relative young age of studied individuals. Studies involving the APOE polymorphism with arterial stiffness phenotype remain scarce in the literature. Thereby, further studies involving the APOE polymorphism with arterial stiffness phenotype are needed to clarify these issues.
Classically, obesity and hyperuricemia have shown to have important roles in the development of cardiometabolic disease [3,52,53]. This study showed that ε4 allele is associated with higher uric acid levels when compared to ε2 allele carriers. In addition, the presence of the ε4 allele offered increased risk for obesity and hyperuricemia. Unlike our findings, Liberopoulos et al[54] studying healthy individuals showed that the ε4 allele was associated with lower uric acid levels when compared to allele ε2. Similar to our study, ε2 allele was associated with lower serum levels of TC. Among the mechanisms that may explain the higher prevalence of hyperuricemia in individuals carrying the ε4 allele of APOE polymorphism in our study could be the hyperinsulinemia associated with an unfavorable lipid profile. Several studies[55] have confirmed that under-excretion of uric acid into the urine caused by the effect of insulin on the urinary tubular tract has been demonstrated with physiological hyperinsulinemia acutely reducing urinary uric acid which could lead to a higher concentration of this protein in the bloodstream. Due to the controversial results and few existing data, studies of the association between APOE polymorphism and uric acid need to be further conducted. Similarly, studies associating obesity phenotypes with APOE polymorphism have shown controversial results. Corroborating our results, Carmo-Martins et al.[50] showed that obese subjects (BMI ≥ 30 Kg/m2) are more prevalent in the ε4 allele group than in the ε2 allele group. In another study, Kolovou et al[56] showed in coronary heart disease patients that the prevalence of obese individuals was higher in the ε4 allele than in the ε2 allele group. Nevertheless, other studies failed to show this association [57]. The relationship between dyslipidemia and obesity is well established in the literature. However, the mechanism by which apolipoprotein E would influence obesity is not clear. Karagiannides et al[58] showed through an experimental study that rat ApoE3knock in after a high-fat diet gained more weight than animals that did not express the APOE protein and animals that expressed isoform APOE2. Considering that in vitro receptor binding studies established that lipid-bound ApoE3 and ApoE4 have a similar affinity for LDLr, whereas lipid-bound ApoE2 has a much lower affinity[59], we hypothesize that this higher affinity of APOE4 isoform could result in increased lipid deposition in the adipose tissue.
Our study has potential limitations. First, it should be noted that the relative young age of the studied population may preclude the identification of the association between the studied genotype and measures of arterial stiffness. Second, we did not evaluate the use of cholesterol-lowering drugs, which could confound the observed associations. Finally, if we have measured insulin and urinary uric acid levels in this population, we could shed light into the proposed mechanism for the association of APOE polymorphism and serum uric acid.
In conclusion, the present study confirms the close association between APOE polymorphism and the lipid profile in individuals from the general population, but failed to show this genetic risk factor as an important modulator of arterial distensibility in this same sample.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ROA and SRSF participated in the design of the study, performed the statistical analysis and drafted the manuscript. PCJLS and NEF contributed to acquisition of data and its interpretation. RSC, JGM and JEK contributed to conception and design of the study. ACP conceived of the study, participated in its design, coordination and helped to draft the manuscript. All authors read and approved the manuscript.
Contributor Information
Rafael O Alvim, Email: alvimfaefid@ig.com.br.
Silvia RS Freitas, Email: silvia.sampaio.freitas@hotmail.com.
Noely E Ferreira, Email: noely.ferreira@incor.usp.br.
Paulo CJL Santos, Email: pacaleb@usb.br.
Roberto S Cunha, Email: robertos.sa@hotmail.com.
José G Mill, Email: jgmill@npd.ufes.br.
José E Krieger, Email: krieger@incor.usp.br.
Alexandre C Pereira, Email: alexandre.pereira@incor.usp.br.
References
- Kreisberg RA, Oberman A. Clinical review 141: lipids and atherosclerosis: lessons learned from randomized controlled trials of lipid lowering and other relevant studies. J Clin Endocrinol Metab. 2002;87(2):423–437. doi: 10.1210/jc.87.2.423. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Grundy SM. Obesity, metabolic syndrome, and coronary atherosclerosis. Circulation. 2002;105(23):2696–2698. doi: 10.1161/01.CIR.0000020650.86137.84. [DOI] [PubMed] [Google Scholar]
- Niskanen LK, Laaksonen DE, Nyyssonen K, Alfthan G, Lakka HM, Lakka TA, Salonen JT. Uric acid level as a risk factor for cardiovascular and all-cause mortality in middle-aged men: a prospective cohort study. Arch Intern Med. 2004;164(14):1546–1551. doi: 10.1001/archinte.164.14.1546. [DOI] [PubMed] [Google Scholar]
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Mahley RW, Innerarity TL, Rall SC Jr, Weisgraber KH. Plasma lipoproteins: apolipoprotein structure and function. J Lipid Res. 1984;25(12):1277–1294. [PubMed] [Google Scholar]
- Kesaniemi YA, Ehnholm C, Miettinen TA. Intestinal cholesterol absorption efficiency in man is related to apoprotein E phenotype. J Clin Invest. 1987;80(2):578–581. doi: 10.1172/JCI113107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davignon J, Gregg RE, Sing CF. Apolipoprotein E polymorphism and atherosclerosis. Arteriosclerosis. 1988;8(1):1–21. doi: 10.1161/01.atv.8.1.1. [DOI] [PubMed] [Google Scholar]
- Das HK, McPherson J, Bruns GA, Karathanasis SK, Breslow JL. Isolation, characterization, and mapping to chromosome 19 of the human apolipoprotein E gene. J Biol Chem. 1985;260(10):6240–6247. [PubMed] [Google Scholar]
- Kolovou G, Damaskos D, Anagnostopoulou K, Cokkinos DV. Apolipoprotein E gene polymorphism and gender. Ann Clin Lab Sci. 2009;39(2):120–133. [PubMed] [Google Scholar]
- Scott J, Knott TJ, Shaw DJ, Brook JD. Localization of genes encoding apolipoproteins CI, CII, and E to the p13----cen region of human chromosome 19. Hum Genet. 1985;71(2):144–146. doi: 10.1007/BF00283370. [DOI] [PubMed] [Google Scholar]
- Weisgraber KH, Rall SC Jr, Mahley RW. Human E apoprotein heterogeneity. Cysteine-arginine interchanges in the amino acid sequence of the apo-E isoforms. J Biol Chem. 1981;256(17):9077–9083. [PubMed] [Google Scholar]
- Medina-Urrutia AX, Cardoso-Saldana GC, Zamora-Gonzalez J, Liria YK, Posadas-Romero C. Apolipoprotein E polymorphism is related to plasma lipids and apolipoproteins in Mexican adolescents. Hum Biol. 2004;76(4):605–614. doi: 10.1353/hub.2004.0059. [DOI] [PubMed] [Google Scholar]
- Wilson PW, Schaefer EJ, Larson MG, Ordovas JM. Apolipoprotein E alleles and risk of coronary disease. A meta-analysis. Arterioscler Thromb Vasc Biol. 1996;16(10):1250–1255. doi: 10.1161/01.atv.16.10.1250. [DOI] [PubMed] [Google Scholar]
- Laws SM, Hone E, Gandy S, Martins RN. Expanding the association between the APOE gene and the risk of Alzheimer's disease: possible roles for APOE promoter polymorphisms and alterations in APOE transcription. J Neurochem. 2003;84(6):1215–1236. doi: 10.1046/j.1471-4159.2003.01615.x. [DOI] [PubMed] [Google Scholar]
- Bretsky P, Guralnik JM, Launer L, Albert M, Seeman TE. The role of APOE-epsilon4 in longitudinal cognitive decline: MacArthur Studies of Successful Aging. Neurology. 2003;60(7):1077–1081. doi: 10.1212/01.wnl.0000055875.26908.24. [DOI] [PubMed] [Google Scholar]
- Shiraki M, Shiraki Y, Aoki C, Hosoi T, Inoue S, Kaneki M, Ouchi Y. Association of bone mineral density with apolipoprotein E phenotype. J Bone Miner Res. 1997;12(9):1438–1445. doi: 10.1359/jbmr.1997.12.9.1438. [DOI] [PubMed] [Google Scholar]
- Chang SJ, Hou MF, Tsai SM, Kao JT, Wu SH, Hou LA, Tsai LY. Association between the apolipoprotein E genotypes and breast cancer patients in Taiwanese. Breast Cancer Res Treat. 2006;98(1):109–113. doi: 10.1007/s10549-005-9137-0. [DOI] [PubMed] [Google Scholar]
- Hubacek JA, Bloudickova S, Kubinova R, Pikhart H, Viklicky O, Bobak M. Apolipoprotein E polymorphism in hemodialyzed patients and healthy controls. Biochem Genet. 2009;47(9-10):688–693. doi: 10.1007/s10528-009-9266-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Errera FI, Silva ME, Yeh E, Maranduba CM, Folco B, Takahashi W, Pereira AC, Krieger JE, Passos-Bueno MR. Effect of polymorphisms of the MTHFR and APOE genes on susceptibility to diabetes and severity of diabetic retinopathy in Brazilian patients. Braz J Med Biol Res. 2006;39(7):883–888. doi: 10.1590/S0100-879X2006000700005. [DOI] [PubMed] [Google Scholar]
- Reilly M, Rader DJ. Apolipoprotein E and coronary disease: a puzzling paradox. PLoS Med. 2006;3(6):e258. doi: 10.1371/journal.pmed.0030258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailleul S, Couderc R, Landais V, Lefevre G, Raichvarg D, Etienne J. Direct phenotyping of human apolipoprotein E in plasma: application to population frequency distribution in Paris (France) Hum Hered. 1993;43(3):159–165. doi: 10.1159/000154172. [DOI] [PubMed] [Google Scholar]
- The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41(2):105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- Mill JGMM, Silva IO, Marquezine AL, Ferreira AVL, Cunha RS. et al. Epidemiologia da hipertensão arterial na cidade de Vitória, Espírito Santo. Hipertensão. 2004;7(3):109–116. [Google Scholar]
- World Health Organization. Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/index.html
- Freitas SR, Pereira AC, Floriano MS, Mill JG, Krieger JE. Association of alpha1a-adrenergic receptor polymorphism and blood pressure phenotypes in the Brazilian population. BMC Cardiovasc Disord. 2008;8:40. doi: 10.1186/1471-2261-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessa I, Fonseca J. [Race, compliance to treatment and/or consultation and control of arterial hypertension] Arq Bras Cardiol. 1997;68(6):443–449. [PubMed] [Google Scholar]
- 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17(2):151–183. [PubMed] [Google Scholar]
- Asmar R, Benetos A, Topouchian J, Laurent P, Pannier B, Brisac AM, Target R, Levy BI. Assessment of arterial distensibility by automatic pulse wave velocity measurement. Validation and clinical application studies. Hypertension. 1995;26(3):485–490. doi: 10.1161/01.hyp.26.3.485. [DOI] [PubMed] [Google Scholar]
- Pereira AC, Sposito AC, Mota GF, Cunha RS, Herkenhoff FL, Mill JG, Krieger JE. Endothelial nitric oxide synthase gene variant modulates the relationship between serum cholesterol levels and blood pressure in the general population: new evidence for a direct effect of lipids in arterial blood pressure. Atherosclerosis. 2006;184(1):193–200. doi: 10.1016/j.atherosclerosis.2005.03.035. [DOI] [PubMed] [Google Scholar]
- Santos RD. [III Brazilian Guidelines on Dyslipidemias and Guideline of Atherosclerosis Prevention from Atherosclerosis Department of Sociedade Brasileira de Cardiologia] Arq Bras Cardiol. 2001;77(Suppl 3):1–48. [PubMed] [Google Scholar]
- Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16(3):1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang HK, Fung HC, Hsu WC, Wu YR, Lin JC, Ro LS, Chang KH, Hwu FJ, Hsu Y, Huang SY. et al. Apolipoprotein E, angiotensin-converting enzyme and kallikrein gene polymorphisms and the risk of Alzheimer's disease and vascular dementia. J Neural Transm. 2006;113(10):1499–1509. doi: 10.1007/s00702-005-0424-z. [DOI] [PubMed] [Google Scholar]
- He LN, Recker RR, Deng HW, Dvornyk V. A polymorphism of apolipoprotein E (APOE) gene is associated with age at natural menopause in Caucasian females. Maturitas. 2009;62(1):37–41. doi: 10.1016/j.maturitas.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward H, Mitrou PN, Bowman R, Luben R, Wareham NJ, Khaw KT, Bingham S. APOE genotype, lipids, and coronary heart disease risk: a prospective population study. Arch Intern Med. 2009;169(15):1424–1429. doi: 10.1001/archinternmed.2009.234. [DOI] [PubMed] [Google Scholar]
- Liang S, Pan M, Geng HH, Chen H, Gu LQ, Qin XT, Qian JJ, Zhu JH, Liu CF. Apolipoprotein E polymorphism in normal Han Chinese population: frequency and effect on lipid parameters. Mol Biol Rep. 2009;36(6):1251–1256. doi: 10.1007/s11033-008-9305-5. [DOI] [PubMed] [Google Scholar]
- de-Andrade FM, Larrandaburu M, Callegari-Jacques SM, Gastaldo G, Hutz MH. Association of apolipoprotein E polymorphism with plasma lipids and Alzheimer's disease in a Southern Brazilian population. Braz J Med Biol Res. 2000;33(5):529–537. doi: 10.1590/S0100-879X2000000500007. [DOI] [PubMed] [Google Scholar]
- Mendes-Lana A, Pena GG, Freitas SN, Lima AA, Nicolato RL, Nascimento-Neto RM, Machado-Coelho GL, Freitas RN. Apolipoprotein E polymorphism in Brazilian dyslipidemic individuals: Ouro Preto study. Braz J Med Biol Res. 2007;40(1):49–56. doi: 10.1590/S0100-879X2007000100007. [DOI] [PubMed] [Google Scholar]
- De Franca E, Alves JG, Hutz MH. Apolipoprotein E polymorphism and its association with serum lipid levels in Brazilian children. Hum Biol. 2004;76(2):267–275. doi: 10.1353/hub.2004.0030. [DOI] [PubMed] [Google Scholar]
- Saidi S, Slamia LB, Ammou SB, Mahjoub T, Almawi WY. Association of apolipoprotein E gene polymorphism with ischemic stroke involving large-vessel disease and its relation to serum lipid levels. J Stroke Cerebrovasc Dis. 2007;16(4):160–166. doi: 10.1016/j.jstrokecerebrovasdis.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Kumar P, Luthra K, Dwivedi M, Behl VK, Pandey RM, Misra A. Apolipoprotein E gene polymorphisms in patients with premature myocardial infarction: a case-controlled study in Asian Indians in North India. Ann Clin Biochem. 2003;40(Pt 4):382–387. doi: 10.1258/000456303766477020. [DOI] [PubMed] [Google Scholar]
- Pitsavos C, Choumerianou DM, Skoumas J, Maumus S, Stefanadis C, Dedoussis GV, Visvikis-Siest S. Apolipoprotein E polymorphism is not associated with lipid levels and coronary artery disease in Greek patients with familial hypercholesterolaemia. Clin Exp Med. 2005;5(4):196–201. doi: 10.1007/s10238-005-0086-z. [DOI] [PubMed] [Google Scholar]
- Gottlieb MG, Schwanke CH, Santos AF, Jobim PF, Mussel DP, da Cruz IB. Association among oxidized LDL levels, MnSOD, apolipoprotein E polymorphisms, and cardiovascular risk factors in a south Brazilian region population. Genet Mol Res. 2005;4(4):691–703. [PubMed] [Google Scholar]
- Miettinen TA, Gylling H, Vanhanen H, Ollus A. Cholesterol absorption, elimination, and synthesis related to LDL kinetics during varying fat intake in men with different apoprotein E phenotypes. Arterioscler Thromb. 1992;12(9):1044–1052. doi: 10.1161/01.atv.12.9.1044. [DOI] [PubMed] [Google Scholar]
- Weintraub MS, Eisenberg S, Breslow JL. Dietary fat clearance in normal subjects is regulated by genetic variation in apolipoprotein E. J Clin Invest. 1987;80(6):1571–1577. doi: 10.1172/JCI113243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaume S, Benetos A, Henry OF, Rudnichi A, Safar ME. Aortic pulse wave velocity predicts cardiovascular mortality in subjects >70 years of age. Arterioscler Thromb Vasc Biol. 2001;21(12):2046–2050. doi: 10.1161/hq1201.100226. [DOI] [PubMed] [Google Scholar]
- Zanchetti A. Hyperlipidemia in the hypertensive patient. Am J Med. 1994;96(6A):3S–8S. doi: 10.1016/0002-9343(94)90225-9. [DOI] [PubMed] [Google Scholar]
- Pannier BM, Cambillau MS, Vellaud V, Atger V, Moatti N, Safar ME. Abnormalities of lipid metabolism and arterial rigidity in young subjects with borderline hypertension. Clin Invest Med. 1994;17(1):42–51. [PubMed] [Google Scholar]
- Fuzikawa AK, Peixoto SV, Taufer M, Moriguchi EH, Lima-Costa MF. Association of ApoE polymorphisms with prevalent hypertension in 1406 older adults: the Bambui Health Aging Study (BHAS) Braz J Med Biol Res. 2008;41(2):89–94. doi: 10.1590/S0100-879X2008000200002. [DOI] [PubMed] [Google Scholar]
- Carmo Martins M, Lima Faleiro L, Rodrigues MO, Albergaria I, Fonseca A. [Influence of the APOE genotypes in some atherosclerotic risk factors] Acta Med Port. 2008;21(5):433–440. [PubMed] [Google Scholar]
- Vogel RA, Corretti MC, Gellman J. Cholesterol, cholesterol lowering, and endothelial function. Prog Cardiovasc Dis. 1998;41(2):117–136. doi: 10.1016/S0033-0620(98)80008-X. [DOI] [PubMed] [Google Scholar]
- Hollister LE, Overall JE, Snow HL. Relationship of obesity to serum triglyceride, cholesterol, and uric acid, and to plasma-glucose levels. Am J Clin Nutr. 1967;20(7):777–782. doi: 10.1093/ajcn/20.7.777. [DOI] [PubMed] [Google Scholar]
- Li NF, Wang HM, Yang J, Zhou L, Yao XG, Hong J. Serum uric acid is associated with metabolic risk factors for cardiovascular disease in the Uygur population. Appl Physiol Nutr Metab. 2009;34(6):1032–1039. doi: 10.1139/H09-101. [DOI] [PubMed] [Google Scholar]
- Liberopoulos EN, Miltiadous GA, Athyros VG, Ganotakis M, Cariolou M, Bairaktari E, Elisaf MS. Effect of apolipoprotein E polymorphism on serum uric acid levels in healthy subjects. J Investig Med. 2005;53(3):116–122. doi: 10.2310/6650.2005.00306. [DOI] [PubMed] [Google Scholar]
- Quinones Galvan A, Natali A, Baldi S, Frascerra S, Sanna G, Ciociaro D, Ferrannini E. Effect of insulin on uric acid excretion in humans. Am J Physiol. 1995;268(1 Pt 1):E1–5. doi: 10.1152/ajpendo.1995.268.1.E1. [DOI] [PubMed] [Google Scholar]
- Kolovou GD, Anagnostopoulou KK, Kostakou P, Giannakopoulou V, Mihas C, Hatzigeorgiou G, Vasiliadis IK, Mikhailidis DP, Cokkinos DV. Apolipoprotein E gene polymorphism and obesity status in middle-aged men with coronary heart disease. In Vivo. 2009;23(1):33–39. [PubMed] [Google Scholar]
- Liberopoulos EN, Miltiadous GA, Cariolou M, Kalaitzidis R, Siamopoulos KC, Elisaf MS. Influence of apolipoprotein E polymorphisms on serum creatinine levels and predicted glomerular filtration rate in healthy subjects. Nephrol Dial Transplant. 2004;19(8):2006–2012. doi: 10.1093/ndt/gfh349. [DOI] [PubMed] [Google Scholar]
- Karagiannides I, Abdou R, Tzortzopoulou A, Voshol PJ, Kypreos KE. Apolipoprotein E predisposes to obesity and related metabolic dysfunctions in mice. FEBS J. 2008;275(19):4796–4809. doi: 10.1111/j.1742-4658.2008.06619.x. [DOI] [PubMed] [Google Scholar]
- Kypreos KE, Li X, van Dijk KW, Havekes LM, Zannis VI. Molecular mechanisms of type III hyperlipoproteinemia: The contribution of the carboxy-terminal domain of ApoE can account for the dyslipidemia that is associated with the E2/E2 phenotype. Biochemistry. 2003;42(33):9841–9853. doi: 10.1021/bi0271796. [DOI] [PubMed] [Google Scholar]