Abstract
OBJECTIVE
We explored cognitive impairment in metabolic syndrome in relation to brain magnetic resonance imaging (MRI) findings.
RESEARCH DESIGN AND METHODS
We studied 819 participants free of clinical stroke and dementia of the population-based Austrian Stroke Prevention Study who had undergone brain MRI, neuropsychological testing, and a risk factor assessment relevant to National Cholesterol Education Program Adult Treatment Panel III criteria–defined metabolic syndrome. High-sensitivity C-reactive protein (hs-CRP) was also determined.
RESULTS
Of 819 subjects, 232 (28.3%) had metabolic syndrome. They performed worse than those without metabolic syndrome on cognitive tests assessing memory and executive functioning after adjustment for possible confounders. Stratification by sex demonstrated that metabolic syndrome was related to cognitive dysfunction in men but not in women. Only in men was an increasing number of metabolic syndrome components associated with worse cognitive performance. MRI showed no significant differences in focal ischemic lesions and brain volume between subjects with and without metabolic syndrome, and MRI abnormalities failed to explain impaired cognition. Cognitive performance was most affected in male subjects with metabolic syndrome who also had high hs-CRP levels.
CONCLUSIONS
Metabolic syndrome exerts detrimental effects on memory and executive functioning in community-dwelling subjects who have not had a clinical stroke or do not have dementia. Men are more affected than women, particularly if they have high inflammatory markers. MRI-detected brain abnormalities do not play a crucial role in these relationships.
Metabolic syndrome is a cluster of cardiovascular risk factors, including abdominal obesity, atherogenic dyslipidemia, raised blood pressure, and insulin resistance and glucose intolerance (1). It has been associated with cognitive dysfunction (2,3) and Alzheimer's disease (4), but data are discordant (5–7). Negative associations were reported with memory, processing speed, and fluid intelligence (3). Impaired cognition was linked to high-level inflammation (2).
Although components of the metabolic syndrome have been individually related to cognitive outcomes, the mechanisms affecting cognition in metabolic syndrome are undetermined. Factors related to peripheral hyperinsulinemia are probably highly relevant. Peripheral hyperinsulinemia downregulates blood-brain barrier insulin receptors and subsequently reduces insulin transport to the brain followed by decreased acetylcholine neurotransmission and cerebral blood flow (8). In addition, hyperglycemia itself contributes to neuronal apoptosis via increased generation of free radicals, enhanced glycation end products, and elevated lipid peroxidation (8). Interactive effects between hyperglycemia and components of metabolic syndrome such as arterial hypertension have been reported (9). Another possible mechanism are vascular lesions as a sequela of components of metabolic syndrome including hypertension, impaired glucose tolerance, and dyslipidemia. Previous magnetic resonance imaging (MRI) studies described higher rates of silent brain infarcts (10) and leukoaraiosis (11). A diffusion tensor imaging study found evidence for ultrastructural tissue damage in frontal and temporal lobes (12). These studies did not include cognitive testing and thus cannot imply the higher frequency of brain lesions to be responsible for metabolic syndrome–related cognitive dysfunction.
We evaluated both cognitive function and brain MRI-detected lesions in a large cohort of community-dwelling subjects. We hypothesize that individuals with metabolic syndrome have global and domain-specific cognitive dysfunction, a higher frequency of brain abnormalities, and a cognitive status that relates to brain MRI findings.
RESEARCH DESIGN AND METHODS
The Austrian Stroke Prevention Study (ASPS) is a prospective study on the effects of vascular risk factors on brain structure and function in cognitively normal middle-aged and elderly inhabitants of Graz, Austria; details have been previously described (13,14). Briefly, 2,007 participants were randomly selected from the official community register, and all participants were free of stroke and dementia. The study protocol was approved by the responsible ethics committee.
In a first study panel between 1991 and 1994, 509 subjects randomly selected from the entire cohort underwent an extended diagnostic work-up including brain MRI and cognitive testing. To enlarge the cohort with imaging and neuropsychological assessments, an additional 567 individuals were randomly selected in a second panel between 1999 and 2003. They underwent identical imaging and cognitive test procedures. Participants of the first and second panels were pooled, which resulted in a total of 1,076 individuals with brain MRI and neuropsychological evaluation. The long diagnostic periods resulted from limited research-devoted time slots at the MRI center. All clinical examinations were repeated with MRI scanning and neuropsychological testing. Clinical history, blood tests, MRI, and cognitive assessments were always done in 1 day. A total of 819 subjects had a complete risk factor assessment necessary to determine metabolic syndrome and thus created the current study cohort.
Risk factors and definition of metabolic syndrome
Risk factors were determined based on history and measurements at the examination, as previously described (13). Hypertension was considered a history of hypertension with repeated blood pressure readings ≥140/90 mmHg, treatment for hypertension, or readings at the examination exceeding the limit. Diabetes was coded present if an individual was treated for diabetes at the time of examination or if the fasting blood glucose level at the examination exceeded 126 mg/dl. History of coronary heart disease was determined according to the Rose questionnaire, atrial fibrillation was diagnosed based on electrocardiogram findings, and peripheral artery disease was diagnosed based on history. Study participants were asked whether they were previous and/or current smokers or habitual daily drinkers as well as about their physical activity at leisure time; the amount of activity was graded into none (no physical activity), mild (daily walk), and moderate to intensive (daily sports). Waist circumference was measured to define central obesity. A lipid status was determined with standardized measurements for each study participant after a 12-h fasting. High-sensitivity C-reactive protein (hs-CRP) was measured with a particle-enhanced immunoturbimetric assay, with a detection limit of 0.1 mg/l. We defined a high level of inflammation as hs-CRP levels above the median of hs-CRP distribution (>1.9 mg/l) in our cohort.
Metabolic syndrome was defined according to National Cholesterol Education Program Adult Treatment Panel III criteria and revised American Heart Association/National Heart, Lung, and Blood Institute criteria (1). Participants were considered to have metabolic syndrome if they met three or more of the following criteria: 1) waist circumference >102 cm in men and >88 cm in women, 2) fasting serum triglycerides ≥150 mg/dl or treatment for hypertriglyceridemia, 3) serum HDL cholesterol <40 mg/dl in men and <50 mg/dl in women or treatment for low HDL cholesterol, 4) blood pressure ≥130/85 mmHg or use of antihypertensive drugs, 5) fasting blood glucose levels ≥110 mg/dl or use of antidiabetes drugs.
Neuropsychological testing
A test battery assessing memory and learning abilities, psychomotor skills, and executive functions was administrated as described previously (13,14). To assess learning ability and intermediate memory recall, one test called Bäumler's Lern und Gedächtnistest was used. Psychomotor skills were evaluated by one test called the Purdue's Pegboard Test. Executive functions were assessed by three tests: the Wisconsin Card Sorting Test, part B of the Trail Making Test, and Digit Span Backwards, which is part of the Wechsler Adult Intelligence Scale, revised. We used summary measures of cognitive function by converting individual test results to z-scores and computing the average of the scores within each cognitive domain. Z-scores were not adjusted for age, sex, and education. For assessment of depressive mood we applied the “Eigenschaftswörterliste” of W. Janke, G. Debus (1978) Die Eigenschaftswörterliste (EWL); Handanweisung, Göttingen: Hogrefe, a validated multidimensional tool consisting of a list of given adjectives describing the emotional status of a test person at the time of the interview.
MRI
All scans were obtained on a 1.5-Tesla scanner (Philips Medical Systems, Eindhoven, The Netherlands) with protocols described previously (13). White matter lesion (WML) volume, lacunes, thromboembolic infarcts, and brain volume were determined in each study participant.
WML volume
The scans were analyzed by two experienced investigators (C.E. and R.S.). They first graded WMLs according to our scheme (15), then marked and outlined each WML on a transparency that was overlaid on the proton density scans. They were blinded to clinical data of study participants. Independently from this visual analysis, lesion load measurements were done on proton density–weighted images on an UltraSPARC workstation (Sun Microsystems, Santa Clara, CA) by a trained operator using DISPImage (16). The trained operator used a hardcopy overlaid by the transparency, with all lesions outlined by the experienced readers as reference, and segmented all lesions on the computer image. Lesion areas were then provided by the semiautomated thresholding algorithm implemented in DISPImage. The total lesion volume (cm3) was calculated by multiplying the total lesion area by slice thickness.
Lacunes and thromboembolic infarcts
Lacunes were defined as focal lesions that involved the basal ganglia, internal capsule, thalamus, or brain stem, not exceeding a maximum diameter of 15 mm. The presence of silent thromboembolic infarcts was also recorded.
Brain volume
Brain volume was calculated from the T2-weighted spin echo sequence using the fully automated structural image evaluation of atrophy (Sienax, part of the FMRIB Software Library; http://www.fmrib.ox.ac.uk/fsl). Brain parenchyma percentage was estimated from the ratio of parenchymal volume to the total volume given by the outer surface of the brain. To determine the measurement errors in our dataset, 20 participants were scanned and rescanned after shortly leaving the scanner. The median relative error for Sienax was 1.2%.
Data analysis
Significant differences in means of normally distributed continuous variables were tested by ANOVA and significant differences of nonnormally distributed variables by the Mann-Whitney U test. Difference in proportions was assessed by χ2 statistics.
Linear regression analysis was performed to estimate the association between metabolic syndrome and the z-scores of the specific cognitive domains. Different models were assessed. Model 1 included age and sex plus subjects' characteristics that were different across the metabolic syndrome, including years of education, leisure physical activity, and coronary heart disease. Although significantly more common in patients with metabolic syndrome, hypertension and diabetes were not used as covariates because all subjects with hypertension and diabetes were included in our definition of metabolic syndrome. Depressive mood was considered as a covariate based on its significant relationship to cognitive functioning. Model 2 investigated to what extent the associations between metabolic syndrome and cognition were mediated by MRI findings and thus included all covariates of model 1 plus presence of lacunes, silent infarcts, WML volume, and brain parenchymal fraction. The relationship between metabolic syndrome and vascular lesions and brain atrophy was determined by multivariate regression analyses using model 1 covariates.
Multicollinearity between MRI variables was assessed using the variance inflation factor (VIF). Usually, VIF values >10 are suggestive of multicollinearity and merit further investigation. The mean VIF for MRI variables in our study was 1.04 (range 1.01–1.08). Because data from the literature suggest possible sex differences in metabolic syndrome (6,17), we also stratified our analyses by sex.
Hs-CRP measurements were available in only a subset of our cohort, thus we did not include this factor in the primary model but performed a subanalysis in 541 subjects with hs-CRP measurement to assess whether inflammation plays a causal role in the association between metabolic syndrome and cognition. This subanalysis was done with and without additional adjustment for nonsteroidal anti-inflammatory drugs or acetylsalicyclic acid use. Interactions of hs-CRP and metabolic syndrome with cognitive functioning were tested by including the respective interaction term in the multivariate linear regression models. All analyses were done using Stata (Stata Statistical Software, release 6; StataCorp, College Station, TX).
RESULTS
A total of 232 (28.3%) study participants had metabolic syndrome. There were 157 (67.6%) subjects with three, 55 (23.7%) with four, and 20 (8.6%) with five components of metabolic syndrome. The characteristics of the study cohort are shown in Table 1. Subjects with metabolic syndrome had lower educational status, less leisure physical activity, more coronary heart disease, higher frequencies of each component of metabolic syndrome, and higher hs-CRP.
Table 1.
Characteristics of the study cohort (n = 819) by the absence or presence of metabolic syndrome
| Variable | No metabolic syndrome | Metabolic syndrome | P |
|---|---|---|---|
| n | 587 | 232 | |
| Demographic characteristics | |||
| Age (years) | 64.8 ± 8.1 | 65.1 ± 7.2 | 0.64* |
| Women | 318 (54.1) | 138 (59.5) | 0.16† |
| Years of education | 10 (9–13) | 10 (9–10) | <0.002‡ |
| Risk factors | |||
| Smoking status | 0.44† | ||
| Never | 361 (61.5) | 133 (57.3) | |
| Former | 163 (27.8) | 68 (29.3) | |
| Current | 63 (10.7) | 31 (13.4) | |
| Daily alcohol consumption | 75 (16.4) | 36 (19.8) | 0.30† |
| Physical activity at leisure time | 0.008† | ||
| None | 31 (5.3) | 26 (11.2) | |
| Mild | 189 (32.2) | 76 (32.7) | |
| Moderate to intensive | 367 (62.5) | 130 (56.1) | |
| Hypertension | 391 (66.6) | 202 (87.1) | <0.001† |
| History of coronary heart disease | 183 (31.2) | 89 (38.9) | 0.051† |
| Diabetes | 15 (2.6) | 56 (24.2) | <0.001† |
| Atrial fibrillation | 12 (2.0) | 4 (1.7) | 0.77† |
| Peripheral arterial disease | 5 (0.9) | 5 (2.3) | 0.13† |
| Depressive mood | 1 (0–2) | 1 (0–2) | 0.92‡ |
| hs-CRP (mg/l)§ | 1.7 (0.8–3.2) | 2.5 (1.4–5.1) | <0.001‡ |
| Components of metabolic syndrome | |||
| Abdominal obesity | 149 (25.3) | 176 (75.8) | <0.001‡ |
| Triglycerides ≥150 mg/dl | 76 (12.9) | 172 (74.1) | <0.001† |
| Low HDL cholesterol | 64 (10.9) | 133 (57.3) | <0.001† |
| Fasting glucose ≥110 mg/dl | 25 (4.2) | 84 (36.2) | <0.001† |
| Blood pressure ≥130/85 mmHg | 467 (79.5) | 226 (97.4) | <0.001† |
Data are means ± SD, n (%), or median (interquartile range).
*ANOVA test.
†χ2 test.
‡Mann-Whitney U test.
§Measurement of hs-CRP only available in 541 subjects.
Table 2 shows that subjects with metabolic syndrome performed worse on all cognitive tests, with significant differences in memory and executive functions, but there existed no significant differences in MRI findings between subjects with and without metabolic syndrome. Metabolic syndrome and MRI findings were also not significantly associated in multivariate regression analyses (data not shown).
Table 2.
Cognitive performance and brain MRI findings in the sample (n = 819) by the absence or presence of metabolic syndrome
| Variable | No metabolic syndrome | Metabolic syndrome | P |
|---|---|---|---|
| n | 587 | 232 | |
| Neuropsychological test results | |||
| Mini Mental State Examination | 27.5 ± 1.5 (22–30) | 27.4 ± 1.5 (22–30) | 0.58* |
| Memory | 0.06 ± 1.0 (−1.91 to 4.38) | −0.17 ± 0.9 (−1.98 to 3.32) | <0.001* |
| Psychomotor skills | 0.06 ± 0.8 (−3.00 to 2.56) | 0.01 ± 0.9 (−2.17 to 2.93) | 0.46* |
| Executive functions | 0.49 ± 3.0 (−18.23 to 5.44) | −0.32 ± 3.1 (−16.04 to 5.21) | <0.001* |
| Brain MRI findings | |||
| WML volume in cm3 | 0.9 (0.2–3.1) | 0.9 (0.2–2.4) | 0.89† |
| Lacunes | 32 (5.4) | 15 (6.4) | 0.56‡ |
| Silent infarcts | 16 (2.7) | 10 (4.3) | 0.24‡ |
| Normalized brain percentage | 0.78 ± 0.03 (0.67–0.87) | 0.78 ± 0.04 (0.68–0.86) | 0.38* |
Data are means ± SD (range), n (%), or median (interquartile range).
*ANOVA test.
†Mann-Whitney U test.
‡χ2 test.
When using linear regression analysis with adjustment for age, sex, years of education, depressive mood, coronary heart disease, and physical activity at leisure time (Table 3, model 1), the inverse associations between metabolic syndrome and memory, as well as executive functions, remained significant. The results were virtually unchanged following adjustment for MRI findings (Table 3, model 2). Stratification by sex demonstrated that the significant relationship between metabolic syndrome and impaired memory and executive functioning existed only in men but not in women (Table 3).
Table 3.
Relationship between metabolic syndrome and cognition: multivariate regression analysis
| Model 1* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total sample (n = 819)† |
Men (n = 363) |
Women (n = 456) |
|||||||
| β | P | 95% CI | β | P | 95% CI | β | P | 95% CI | |
| Memory | −0.14 | 0.034 | −0.27 to −0.01 | −0.27 | 0.013 | −0.49 to −0.05 | −0.06 | 0.444 | −0.22 to 0.09 |
| Psychomotor skills | −0.03 | 0.593 | −0.14 to 0.08 | −0.09 | 0.280 | −0.26 to 0.07 | 0.03 | 0.670 | −0.11 to 0.17 |
| Executive functions | −0.58 | 0.010 | −1.02 to −0.14 | −0.80 | 0.033 | −1.54 to −0.06 | −0.39 | 0.162 | −0.94 to 0.15 |
| Model 2* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total sample (n = 819)† |
Men (n = 363) |
Women (n = 456) |
|||||||
| β | P | 95% CI | β | P | 95% CI | β | P | 95% CI | |
| Memory | −0.12 | 0.090 | −0.27 to 0.02 | −0.25 | 0.050 | −0.51 to 0.00 | −0.04 | 0.645 | −0.23 to 0.14 |
| Psychomotor skills | −0.006 | 0.920 | −0.13 to 0.11 | 0.02 | 0.842 | −0.18 to 0.22 | −0.003 | 0.961 | −0.16 to 0.15 |
| Executive functions | −0.65 | 0.010 | −1.14 to −0.15 | −0.94 | 0.023 | −1.74 to −0.13 | −0.44 | 0.165 | −1.07 to 0.18 |
*Model 1: adjusted for age, years of education, depressive mood, coronary heart disease, and physical activity at leisure time. Model 2: model 1 plus adjustment for WML volume, presence of lacunes, silent infarcts, and brain parenchymal fraction.
†Total sample: additionally adjusted for sex.
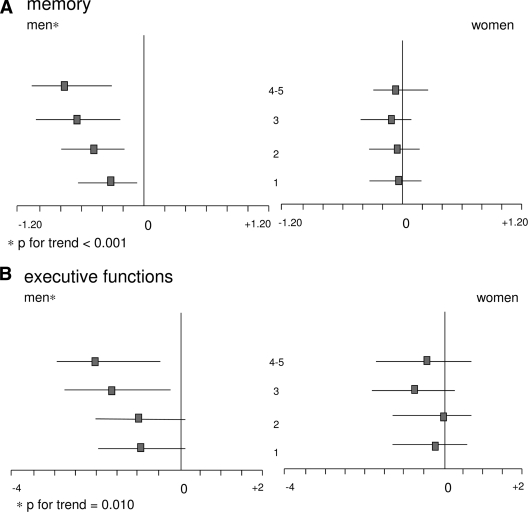
Figure 1 displays the relationship between the number of components of metabolic syndrome and performance on tests of memory and executive functioning. In men, with more components of metabolic syndrome present, memory (one component: β = −0.38; two components: β = −0.52; three components: β = −0.64; more than three components: β = −0.71; P for trend <0.001) and executive functions (one component: β = −0.99; two components: β = −1.02; three components: β = −1.55; more than three components: β = −1.90; P for trend = 0.010) were more impaired. No such relationship existed in women.
Figure 1.
Relationship between memory performance (upper panel), executive functions (lower panel), and number of metabolic syndrome components (indicated on the y-axis in the middle). Multivariate regression analysis stratified by sex and adjusted for age, years of education, depressive mood, physical activity at leisure time, and coronary heart disease. The squares on the x-axis indicate β-coefficients, and the bars indicate 95% CIs. An increasing number of metabolic syndrome components was associated with worse function in these domains in men only.
A multivariate regression analysis adjusted for model 1 and 2 covariates showed that men, but not women, with metabolic syndrome who had high hs-CRP levels (i.e., >1.9 mg/l) performed significantly worse on tests of memory (β = −0.44; 95% CI [−0.94 to 0.04]; P = 0.074) and executive functions (β = −2.21; 95% CI [−3.81 to −0.62]; P = 0.007) than their male counterparts with low hs-CRP (memory: β = −0.05; 95% CI [−0.45 to 0.33]; P = 0.774; executive functions: β = 0.48; 95% CI [−0.74 to 1.7]; P = 0.437). After adjustment for nonsteroidal anti-inflammatory drugs or aspirin usage in the model, the results remained almost identical (data not shown). The interaction between hs-CRP and metabolic syndrome was significant for executive functions (β = −2.79; 95% CI [−4.67 to −0.92]; P = 0.004) and showed a nonsignificant trend for memory (β = −0.56; 95% CI [−1.17 to 0.04]; P = 0.068).
CONCLUSIONS
Middle-aged and elderly community-dwelling subjects with metabolic syndrome performed worse on tasks assessing memory and executive functions than their counterparts without metabolic syndrome. This was seen in men but not in women, and the more components of metabolic syndrome were present, the more impaired was cognitive functioning. Focal and diffuse brain lesions failed to explain the association between metabolic syndrome and cognition. Men with metabolic syndrome and high inflammatory markers had more severe cognitive deficits.
Previous studies (2,3) described cognitive dysfunction in patients with metabolic syndrome. Most used gross measures of cognition for patients' assessment (2). The Longitudinal Aging Study Amsterdam also applied comprehensive neuropsychological testing and, similar to us, also found memory and processing speed deficits in metabolic syndrome patients (3). This pattern favors both cortical and subcortical brain damage as the underlying cause (18). Our finding that metabolic syndrome affects cognition, particularly in men, is novel. So far, only few studies stratified their analyses by sex, and they yielded conflicting results. Vanhanen et al (4) found more Alzheimer's disease in metabolic syndrome patients, and, after stratification by sex, this association existed predominantly in women. By contrast, Laudisio et al. (6) reported that female patients performed cognitively better than male patients. So far, sex-specific differences in risk factor–related biological mechanisms leading to cognitive decline remained widely unexplored. We can only speculate on the causes for more pronounced cognitive deficits in men than in women with metabolic syndrome. Central nervous insulin resistance may play a role. It is assumed to be a common denominator of metabolic disorders and cognitive dysfunctions by exerting detrimental effects on cholinergic and glutamatergic pathways which establish neuronal plasticity (19).
Women have less insulin resistance than men and may thus be less amenable to metabolic syndrome–related cognitive dysfunction. Several mechanisms have been reported, leading to a more insulin-sensitive environment in women. These include sex differences in adipose tissue distribution, estrogen effects on insulin and glucose homeostasis and proinflammatory markers, as well as higher levels of the insulin-sensitizing hormone adiponectin in women (20).
We saw no significant differences in ischemic brain lesions or brain atrophy between subjects with and without metabolic syndrome. Our MRI results were unexpected, as previous investigations described associations of metabolic syndrome with increasing grades of white matter abnormalities (11) and brain infarctions (10), and several studies indicated more pronounced brain atrophy in individuals with single components of metabolic syndrome such as diabetes (21) and hypertension (22). We probably recruited healthier participants than previous hospital- or population-based cohorts not excluding clinically overt cerebral disease (10,11). It remains to be determined whether ultrastructural tissue changes in subcortical or cortical tissue compartments not seen in conventional but new MRI techniques, such as diffusion tensor imaging (12), occur with metabolic syndrome and whether they correlate with cognitive decline.
Our analyses on the associations between metabolic syndrome, hs-CRP levels, and cognitive functioning suggest that inflammation interacts in the relationship between metabolic syndrome and cognitive impairment. This finding is corroborated by investigations by Dik et al. (3) and Yaffe et al. (2,23) that described the detrimental effect of metabolic syndrome on cognition mainly in metabolic syndrome subjects with high levels of proinflammatory markers. The association between hs-CRP and cognitive impairment in metabolic syndrome patients may at first seem to indicate that subjects with ongoing generalized atherosclerosis are at greater risk of concurrent and subsequent cerebrovascular damage and neurodegeneration, both of which cause cognitive decline. This, however, is unlikely based on our findings that the frequency of focal ischemic lesions and brain atrophy was similar in subjects with and without metabolic syndrome, and MRI abnormalities were not related to cognitive test performance. These findings rather favor inflammatory processes being directly related to both metabolic syndrome and cognitive functioning irrespectively of their possible role in the etiology of vascular and primary degeneration. Increased hs-CRP levels may well reflect lifetime overreactivity of the innate immune system to various exogenous and endogenous stimuli. This overreactivity may be genetically determined and confer the increased risk for developing both metabolic syndrome and cognitive impairment in later life. Consequently, the interactive association observed here of metabolic syndrome and hs-CRP with cognitive functions is of particular interest. In this context it is also noteworthy that elevated levels of inflammatory markers have been repeatedly linked to an increased risk of dementia (23). Intriguingly, the Honolulu Asia Aging Study reported increased hs-CRP levels 25 years prior to the occurrence of dementia (24). Similar data come from the Rotterdam Study (25).
A strength of our study is the simultaneous assessment of cognitive function and brain MRI in a large cohort of community-dwelling subjects who were prospectively examined using a standardized protocol. An important limitation of this study is its cross-sectional design, which does not permit to deduce a cause-and-effect relationship. Other limitations include missing measurements of hippocampal volume due to lack of coronal MRI sequences and missing information on duration of metabolic syndrome. The cognitive deficits observed in our study are subtle and clinically covert. Their predictive implications require long-term longitudinal evaluation. Sex-specific effects associated with proinflammatory markers and the lack of significant associations with MRI abnormalities ought to be considered in future studies on mechanisms of cognitive impairment in metabolic syndrome.
Acknowledgments
Salary support for M.C. was provided by the “O. Arlotti Trust,” Ferrara, Italy. No other potential conflicts of interest relevant to this article were reported.
M.C. contributed to study design, statistical methods and analysis, interpretation of results, drafting of the manuscript, and critical review of the manuscript. R.S. contributed to study design, study management, statistical methods and analysis, interpretation of results, drafting of the manuscript, and critical review of the manuscript. S.R. contributed to study management and critical review of the manuscript. K.P. contributed to study management, subject recruitment, interpretation of results, and critical review of the manuscript. N.H. contributed to subject recruitment and critical review of the manuscript. A.G. contributed to study recruitment and critical review of the manuscript. P.K. contributed to subject recruitment and critical review of the manuscript. P.S. contributed to subject recruitment and critical review of the manuscript. A.B. contributed to statistical methods and analysis and critical review of the manuscript. C.E. contributed to interpretation of results, drafting of the manuscript, and critical review of the manuscript. A.P.F. contributed to drafting of the manuscript and critical review of the manuscript.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C: Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004;109(3):433–438 [DOI] [PubMed] [Google Scholar]
- 2.Yaffe K, Kanaya A, Lindquist K, Simonsick EM, Harris T, Shorr RI, Tylavsky FA, Newman AB: The metabolic syndrome, inflammation, and risk of cognitive decline. JAMA 2004;292(18):2237–2242 [DOI] [PubMed] [Google Scholar]
- 3.Dik MG, Jonker C, Comijs HC, Deeg DJ, Kok A, Yaffe K, Penninx BW: Contribution of metabolic syndrome components to cognition in older individuals. Diabetes Care 2007;30(10):2655–2660 [DOI] [PubMed] [Google Scholar]
- 4.Vanhanen M, Koivisto K, Moilanen L, Helkala EL, Hanninen T, Soininen H, Kervinen K, Kesaniemi YA, Laakso M, Kuusisto J: Association of metabolic syndrome with Alzheimer disease: a population-based study. Neurology 2006;67(5):843–847 [DOI] [PubMed] [Google Scholar]
- 5.van den Berg E, Biessels GJ, de Craen AJ, Gussekloo J, Westendorp RG: The metabolic syndrome is associated with decelerated cognitive decline in the oldest old. Neurology 2007; 69(10):979–985 [DOI] [PubMed] [Google Scholar]
- 6.Laudisio A, Marzetti E, Pagano F, Cocchi A, Franceschi C, Bernabei R, Zuccala G: Association of metabolic syndrome with cognitive function: the role of sex and age. Clin Nutr 2008;27(5):747–754 [DOI] [PubMed] [Google Scholar]
- 7.Raffaitin C, Gin H, Empana JP, Helmer C, Berr C, Tzourio C, Portet F, Dartigues JF, Alperovitch A, Barberger-Gateau P: Metabolic syndrome and risk for incident Alzheimer's disease or vascular dementia: the Three-City Study. Diabetes Care 2009;32(1):169–174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Craft S, Watson GS: Insulin and neurodegenerative disease: shared and specific mechanisms. Lancet Neurology 2004;3:169–178 [DOI] [PubMed] [Google Scholar]
- 9.Schmidt R, Launer LJ, Nilson L-G, Pajak A, Sans S, Berger K, Breteler M, de Ridder M, Dufouil C, Fuhrer R, Giampaoli S, Hofman A: the CASCADE Consortium Magnetic resonance imaging of the brain in diabetes: the Cardiovascular Determinants of Dementia (CASCADE) study. Diabetes 2004;53:687–692 [DOI] [PubMed] [Google Scholar]
- 10.Kwon HM, Kim BJ, Lee SH, Choi SH, Oh BH, Yoon BW: Metabolic syndrome as an independent risk factor of silent brain infarction in healthy people. Stroke 2006;37(2):466–470 [DOI] [PubMed] [Google Scholar]
- 11.Park K, Yasuda N, Toyonaga S, Yamada SM, Nakabayashi H, Nakasato M, Nakagomi T, Tsubosaki E, Shimizu K: Significant association between leukoaraiosis and metabolic syndrome in healthy subjects. Neurology 2007;69(10):974–978 [DOI] [PubMed] [Google Scholar]
- 12.Segura B, Jurado MA, Freixenet N, Falcon C, Junque C, Arboix A: Microstructural white matter changes in metabolic syndrome: a diffusion tensor imaging study. Neurology 2009;73(6):438–444 [DOI] [PubMed] [Google Scholar]
- 13.Schmidt R, Fazekas F, Kapeller P, Schmidt H, Hartung H: MRI white matter hyperintensities: three-year follow-up of the Austrian Stroke Prevention Study. Neurology 1999;53:132–139 [DOI] [PubMed] [Google Scholar]
- 14.Schmidt R, Lechner H, Fazekas F, Niederkorn K, Reinhart B, Grieshofer P, Horner S, Offenbacher H, Koch M, Eber B, Schumacher M, Kapeller P, Freidl W, Dusek T: Assessment of cerebrovascular risk profiles in healthy persons: definition of research goals and the Austrian Stroke Prevention Study (ASPS). Neuroepidemiology 1994;13(6):308–313 [DOI] [PubMed] [Google Scholar]
- 15.Fazekas F, Niederkorn K, Schmidt R, Offenbacher H, Horner S, Bertha G, Lechner H: White matter signal abnormalities in normal individuals: correlation with carotid ultrasonography, cerebral blood flow measurements, and cerebrovascular risk factors. Stroke 1988;19:1285–1288 [DOI] [PubMed] [Google Scholar]
- 16.Plummer D: DispImage: a display and analysis tool for medical images. Revista di Neuroradiologica 1992;5:489–495 [Google Scholar]
- 17.Regitz-Zagrosek V, Lehmkuhl E, Weickert MO: Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin Res Cardiol 2006;95(3):136–147 [DOI] [PubMed] [Google Scholar]
- 18.Desmond DW: The neuropsychology of vascular cognitive impairment: is there a specific cognitive deficit? J Neurol Sci 2004;226(1–2):3–7 [DOI] [PubMed] [Google Scholar]
- 19.Kodl CT, Seaquist ER: Cognitive Dysfunction and Diabetes Mellitus. Endocrine Reviews 2008;29(4):494–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geer EB, Wei Shen: Gender Differences in Insulin Resistance, Body Composition, and Energy Balance. Gend Med 2009;6(Suppl. 1):60–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Harten B, de Leeuw FE, Weinstein HC, Scheltens P, Biessels GJ: Brain imaging in patients with diabetes: a systematic review. Diabetes Care 2006;29(11):2539–2548 [DOI] [PubMed] [Google Scholar]
- 22.Manolio TA, Olson J, Longstreth WT: Hypertension and cognitive function: pathophysiologic effects of hypertension on the brain. Curr Hypertens Rep 2003;5(3):255–261 [DOI] [PubMed] [Google Scholar]
- 23.Yaffe K: Metabolic syndrome and cognitive disorders: is the sum greater than its parts? Alzheimer Dis Assoc Disord 2007;21(2):167–171 [DOI] [PubMed] [Google Scholar]
- 24.Schmidt R, Schmidt H, Curb D, Masaki K, White L, Launer L: Early inflammation and dementia: a 25-year follow-up of the Honululu-Asia Aging Study. Ann Neurol 2002;52:168–174 [DOI] [PubMed] [Google Scholar]
- 25.Engelhart MJ, Geerlings MI, Meijer J, Kiliaan A, Ruitenberg A, van Swieten JC, Stijnen T, Hofman A, Witteman JC, Breteler MM: Inflammatory proteins in plasma and the risk of dementia: the Rotterdam Study. Arch Neurol 2004;61(5):668–672 [DOI] [PubMed] [Google Scholar]