Abstract
OBJECTIVE
The use of alteplase in patients who have had a prior stroke and concomitant diabetes is not approved in Europe. To examine the influence of diabetes and prior stroke on outcomes, we compared data on thrombolysed patients with nonthrombolysed comparators.
RESEARCH DESIGN AND METHODS
We selected patients with ischemic stroke on whom we had data on age, pretreatment baseline National Institutes of Health Stroke Scale (b-NIHSS), and 90-day outcome measures (functional modified Rankin score [mRS]) and neurological measures [NIHSS]) in the Virtual International Stroke Trials Archive. We compared outcomes between thrombolysed patients and nonthrombolysed comparators in those with and without diabetes, those who have had a prior stroke, or both and report findings using the Cochran-Mantel-Haenszel (CMH) test and proportional odds logistic regression analyses. We report an age-adjusted and b-NIHSS–adjusted CMH P value and odds ratio (OR).
RESULTS
Rankin data were available for 5,817 patients: 1,585 thrombolysed patients and 4,232 nonthrombolysed comparators. A total 1,334 (24.1%) patients had diabetes, 1,898 (33.7%) patients have had a prior stroke, and 491 (8%) patients had both. Diabetes and nondiabetes had equal b-NIHSS (median 13; P = 0.3), but patients who have had a prior stroke had higher b-NIHSS than patients who have not had a prior stroke (median 13 vs. 12; P < 0.0001). Functional outcomes were better for thrombolysed patients versus nonthrombolysed comparators among both nondiabetic (P < 0.0001; OR 1.4 [95% CI 1.3–1.6]) and diabetic (P = 0.1; 1.3 [1.05–1.6 ]) subjects. Similarly, outcomes were better for thrombolysed patients versus nonthrombolysed comparators among who have not had a prior stroke (P < 0.0001; 1.4 [1.2–1.6 ]) and those who have (P = 0.02; 1.3 [1.04–1.6 ]). There was no interaction of diabetes and prior stroke with treatment (P = 0.8). Neurological outcomes were consistent with the mRS.
CONCLUSIONS
Outcomes from thrombolysis are better among patients with diabetes and/or those who have had a prior stroke than in control subjects. Withholding thrombolytic treatment from otherwise-eligible patients may not be justified.
Thrombolytic therapy is the only proven therapy known to enhance outcomes in ischemic stroke patients (1,2). Its mechanism involves recanalization and rapid reperfusion of the critically hypoperfused brain tissue, which in turn restores the function of ischemic brain parenchyma (2,3). Reperfusion-induced improvement in outcomes depends on local factors in brain tissue, such as the extent of neuronal damage, cerebral perfusion pressure (systemic blood pressure), oxidative stress, intracellular acidosis, and mitochondrial dysfunction (3,4). Animal studies have shown a conflicting association of hyperglycemia with ischemic stroke (4). Instead, clinical studies (3–5) have largely shown an adverse influence of hyperglycemia on the outcomes of nonlacunar ischemic stroke patients. Poorer response to thrombolysis in these patients is considered to be a result of increased plasminogen activator inhibitor-1 activity, resistance to antithrombotic agents, and higher prevalence of atherosclerosis (3,5). Stroke recurrence is another major problem encountered in clinical practice, and prior stroke in patients is known to reduce the benefits attainable from thrombolytic therapy (6). Because these patients are already on antithrombotic therapy, several clinicians mostly worry about hemorrhagic complications when administering the thrombolytic therapy. An analysis of patients who were treated during 0–6 h of stroke onset (n = 2,184) enrolled in five thrombolysis trials (2,6–9) has shown that a previous stroke and diabetes are the predictors of poor outcome.
Owing to the concerns of poorer outcomes in these patients if given thrombolytic therapy, and two previously unsuccessful Europe-specific thrombolysis trials, trialists agreed to exclude patients with diabetes or a history of stroke when designing the European Cooperative Acute Stroke Study III (ECASS III) (1). As a result, despite encouraging results from the ECASS III (1), the only positive thrombolysis study since the National Institute of Neurological Disorders and Stroke (2), the European drug authorities had to suggest exclusion of these patients from receiving recombinant tissue-type plasminogen activator (rt-PA) therapy when formalizing drug-use labels (10). Use of alteplase in patients having prior stroke and concomitant diabetes is not approved in Europe (10). Regardless, physicians still treat diabetic patients in routine clinical practice or research settings (11).
In the current scenario, an ideal approach would be to conduct a randomized controlled trial and examine the influence of thrombolytic therapy on outcomes in patients who have diabetes and have had a previous stroke. To our knowledge, there are no plans of any trial group to conduct such a trial; therefore, we planned for an alternative approach. We decided to examine outcomes of patients who received rt-PA against those who did not, from the data of the neuroprotection trials conducted between1998 and 2007 and obtained these data from the Virtual International Stroke Trials Archive (VISTA). Using an analytical approach recommended by the European Medicines Agency (EMEA), we compared outcomes among patients who have diabetes, had previous strokes, and a combination thereof.
RESEARCH DESIGN AND METHODS
Data source and patients
We collated the demographics, clinical data, and measures of functional outcome from neuroprotection trials conducted in the period between 1998 and 2007, held within the VISTA (12). All trials had necessary review board and regulatory approvals, and patients consented to participation; only anonymized data are held by the VISTA (12). We sought data from the VISTA deriving from trials in which the investigational neuroprotection agent was neither vasoactive nor interfered with clotting or from placebo groups. We excluded any patient who had cerebral hemorrhage or stroke of undetermined etiology. To avoid dual publication, we excluded patients who may have been enrolled in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study, as determined from their country and date of enrollment (13). Finally, we excluded patients lacking our chosen outcome measure (90-day modified Rankin score [mRS]) or secondary outcome (90-day National Institutes of Health Stroke Scale [NIHSS] score). Patients who died within 90 days were given an mRS score of 6 and were categorized separately for NIHSS analysis.
Statistical analysis
We compared the outcome between patients who received thrombolysis and nonthrombolysed control subjects among patients who had diabetes, prior stroke, or a combination of both. For each contrast, we compared the overall distribution of all seven categories of day-90 mRS scores of the two groups (i.e., from 0 [asymptomatic] through 5 [bedbound and completely dependent] to 6 [dead]). The EMEA points to consider for reporting trials allow for use of the full distribution of the mRS but suggest that this may be supported by a secondary analysis of a second outcome measure such as the NIHSS (14). For analysis of our supporting end point, NIHSS, we grouped adjacent scores into the following categories: 0 (no measurable deficit), 1–4, 5–8, 9–12, 13–16, 17–20, 21–24, and ≥25 (most severe neurological deficit) or death. The distribution of patients across these categories was then compared between the groups as for mRS.
To test for a significant association of outcome distribution with thrombolysis exposure, we used the Cochran-Mantel-Haenszel [CMH] statistic, adjusting for both age and baseline NIHSS as continuous variables (15). This nonparametric approach avoids invoking an assumption of proportional odds in which there should be a common odds ratio (OR) across all cut points on the ordinal outcome scale, and we consider that the CMH test provides the most conservative estimate of statistical significance (15–17). However, it does not express the extent of the association. For this, we applied logistic regression analysis, also adjusted for age and baseline NIHSS, to estimate the OR under the assumption of proportional odds and its associated 95% CI.
Our choice of baseline factors for adjustment was based on two influences. First, age and baseline severity are the two most powerful prognostic factors for stroke and are usually included in outcome distribution analyses (18). Second, age and NIHSS data were available for our entire sample, whereas other factors of potential interest were incomplete. However, we also undertook a sensitivity analysis by considering the combined effect of the variables that differed significantly at baseline, but if this resulted in excessive diminution of our sample, we did not quote the findings.
Our objective was mainly to undertake ordinal distribution or “shift” analysis, which is an efficient end point analytic technique recommended by the EMEA (19). Shift analysis is considered better than dichotomization of end point measures, although there are differences of opinion (16,17,20–22). Dichotomization is criticized for the statistical information it discards (i.e., loss of power), and shift analysis is especially useful when the treatment effect is mild and/or uniform across all Rankin categories (16,20,23). For comparison with prior randomized trial and registry reports, however, we also present dichotomized analyses of mRS, based on excellent outcome (mRS 0–1), favorable outcome (mRS 0–2), and survival; these analyses are expressed as ORs adjusted for age and b-NIHSS, as for the primary and secondary end points. To remain consistent with the current age criteria of the EMEA, we examined if the interaction of age with t-PA had influence over outcomes. In addition, we estimated CMH p and proportional odds by ordinal logistic regression analysis for patients belonging to age-group ≤80 years.
ORs in our analysis express the common odds of an improved distribution of outcome in association with alteplase treatment. CMH and logistic regression analysis were undertaken using SAS 9.2 software and other analyses by StatsDirect software. Reliable information on symptomatic hemorrhage was not available because posttreatment imaging was not routinely applied in neuroprotection trials to patients who had not been treated with alteplase.
RESULTS
Patient sample
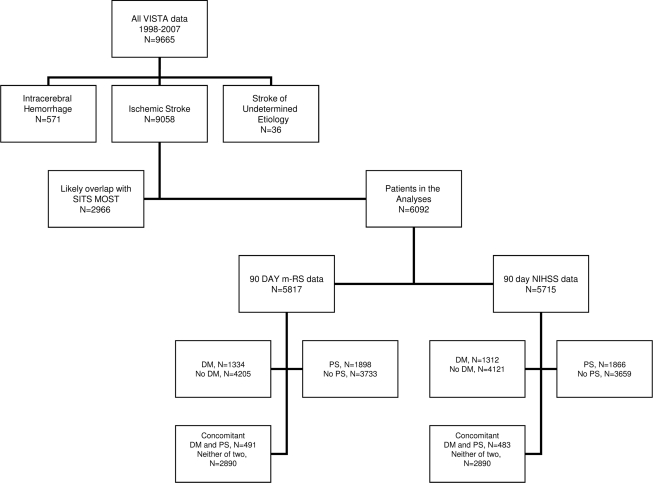
We collated data on 9,665 patients, of whom 5,342 (59%) were enrolled from non-European sites. To avoid dual publication with the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (13), we excluded 2,789 patients (28%) enrolled from European sites between 2002 and 2006 and 177 patients for whom we lacked information on nationality. Complete data were available for analysis of mRS in 5,817 patients and on NIHSS in 5,715 (Fig. 1).
Figure 1.
Baseline description of the data derived from VISTA for the analyses.
All stroke patients were treated as per institutional practice and stroke guidelines acceptable at the point of trial conduct. Monitoring for protocol compliance was undertaken on behalf of sponsors for these trials. This implies that where thrombolysis was administered, this was in accordance with marketing authorization for the relevant country (i.e., that treatment commenced within 3 h of stroke onset); however, the onset to treatment delay is not recorded for thrombolysis in these trials. Our data derived mainly from Northern American (60%), European (16%), and Australasian (13%) centers. Baseline characteristics are shown in Table 1. Of 5,817 patients with mRS outcome data, 1,585 (27.2%) received thrombolysis.
Table 1.
Table shows the baseline characteristics of the patients in the VISTA classified by the presence of diabetes, presence of prior stroke, and presence of prior stroke and concomitant diabetes
| Group of diabetic patients |
Group of prior stroke patients |
Group of concomitant diabetes and prior stroke* |
||||
|---|---|---|---|---|---|---|
| Alteplase | No alteplase | Alteplase | No alteplase | Alteplase | No alteplase | |
| Age** | ||||||
| Mean | 69.5 (10.9), n = 342 | 70.3 (10.8), n = 992 | 70.6 (12.6), n = 319 | 73.2 (10.9), n = 1,579 | 71.2 (10), n = 86 | 71.8 (9.8), n = 405 |
| Median | 71 (33–98) | 72 (30–96) | 73 (21–98) | 75 (30–101) | 73 (46–98) | 73 (37–90) |
| P = 0.2 | P = 0.0002 | P = 0.6 | ||||
| Sex (male) | 198/342 (57.9%) | 532/992 (53.6%) | 180/319 (56.4%) | 822/1,579 (52.1%) | 54/86 (62.8%) | 212/405 (52.3%) |
| P = 0.17 | P = 0.2 | P = 0.07 | ||||
| Baseline NIHSS | 13 (5–30) | 13 (2–29) | 13 (3–30) | 12 (2–37) | 13.5 (5–30) | 12 (2–29) |
| P = 0.01 | P = 0.02 | P = 0.03 | ||||
| Atrial fibrillation | 82/342 (24%) | 256/992 (34.5%) | 82/312 (26.3%) | 501/1,494 (33.5%) | 18/86 (20.9%) | 105/405 (25.9%) |
| P < 0.05 | P = 0.009 | P = 0.3 | ||||
| Hypertension | 278/342 (81.3%) | 795/992 (80.1%) | 240/312 (76.9%) | 1,162/1,494 (77.8%) | 76/86 (88.4%) | 332/405 (82%) |
| P = 0.6 | P = 0.7 | P = 0.2 | ||||
| Prior use of antiplatelets | 120/241 (49.8%) | 145/348 (41.7%) | 119/186 (64%) | 168/349 (48.1%) | 37/51 (72.5%) | 62/105 (59.0%) |
| P = 0.053 | P = 0.001 | P = 0.09% | ||||
| Prior anticoagulants | 17/241 (7.1%) | 44/348 (12.6%) | 18/186 (9.7%) | 77/349 (22.1%) | 5/51 (9.8%) | 20/105 (19.0%) |
| P = 0.03 | P < 0.05 | P = 0.1 | ||||
| Use of antithrombotics | 129/241 (53.5%) | 173/348 (49.7%) | 128/186 (68.8%) | 225/349 (64.5%) | 38/51 (74.5%) | 72/105 (68.6%) |
| P = 0.04 | P = 0.3 | P = 0.4 | ||||
| Myocardial infarction | 94/342 (27.5%) | 202/992 (20.4%) | 79/312 (25.3%) | 299/1,494 (20%) | 26/86 (30.2%) | 87/405 (21.5%) |
| P = 0.009 | P = 0.047 | P = 0.1 | ||||
| Congestive cardiac failure | 46/272 (16.9%) | 50/374 (13.4%) | 40/197 (20.3%) | 45/359 (12.5%) | 11/53 (20.7%) | 13/110 (11.8%) |
| P = 0.2 | P = 0.02 | P = 0.2 | ||||
P value refers to the comparison between the treated and nontreated group corresponding to each variable.
*The group comprising diabetes and prior stroke was compared specifically against those patients who had neither of the two factors.
**Age is described with mean and SD (above) and median (range) (below).
Analysis of outcomes
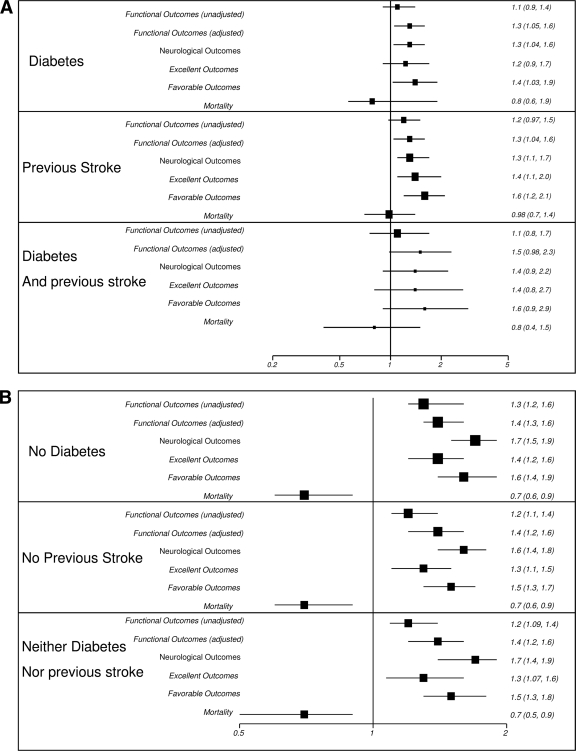
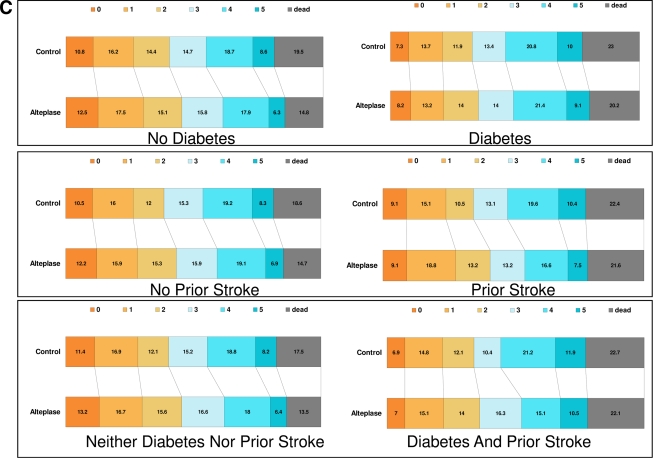
We examined the outcomes in patients with diabetes, those who have had prior strokes, and their combinations. Findings are shown in Fig. 2.
Figure 2.
Forest plots (A and B) and bar diagrams (C) showing outcomes in the approved population (absence of diabetes or prior strokes) and the affected population (presence of diabetes or prior stroke). All outcomes are outcomes on day 90 after the stroke. Excellent outcomes refer to m-RS 0-1 and favorable outcomes to m-RS 0-2. Neurological outcomes refer to the NIHSS scores on day 90. Analyses for neurological outcomes were undertaken using proportional odds logistic regression analyses. NIHSS by day 90 were combined into categories as 0–4, 5–8, 9–12, 13–16, 17–20, 21–24, and ≥25, and distributions were compared in a manner similar to Rankin scores.
In a proportional odds logistic regression analysis adjusting for age and baseline NIHSS, we did not find any interaction of diabetes (P = 0.49), prior stroke (P = 0.72), and diabetes and prior stroke (P = 0.8) with use of rt-PA. For each of the analyses above, we also considered the subgroup of patients aged ≤80 years and also sought evidence of any interaction with age. We failed to find evidence of a differential effect or interaction with age.
CONCLUSIONS
Our analysis reconfirms occurrence of improved outcomes among patients who do not have diabetes and prior stroke, with a significant odds of 1.4. These odds were comparable to the odds obtained from large thrombolysis trials (24), which allowed us to anchor our findings on patients having both diabetes and previous stroke with the trial data. We showed a significant association of improved outcomes with the use of thrombolytic therapy in patients having “diabetes” and “prior stroke” and then also showed that there were no interactions of the diabetes and prior strokes with the use of thrombolytic therapy. However, we failed to confirm statistical significance for a small group of patients who concomitantly had a previous stroke and diabetes (OR 1.5 [95% CI 0.98–2.3]). We attribute this to a type 2 error in this subgroup, namely a smaller sample size (n = 491). Our findings from shift analyses were also supported by similar results from the analyses of dichotomized outcomes.
These findings can be generalized not only because of the comparable odds to those obtained from the large trials data (24) but also because our results were replicated on another analysis involving the comparison of thrombolysed patients (in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study dataset) with the nonthrombolysed control subjects (from the VISTA) (25). In addition, we had supportive findings from analyses of our group (M.K.) for the Helsinki Thrombolysis Register. Here, from 1,200 consecutively treated patients, complete information was available for 1,104 patients, and 51% of patients were treated despite license contraindications. The analysis of 26 patients aged ≤80 years who had both diabetes and previous stroke suggested poorer favorable outcomes (mRS 0–2) in univariate analysis when compared with those treated according to the European license of alteplase but not in multivariate analysis. These patients had more symptomatic intracerebral hemorrhages than those treated on label in univariate analysis, but 95% CI was not significant and in a multivariate analysis there was no trend for symptomatic hemorrhage. We could not however examine the symptomatic brain hemorrhages in our VISTA patients, as our data were derived from neuroprotection trials, which had not routinely obtained imaging information of the untreated patients.
We based our conclusions on adjusted analyses, adjusting for age and baseline NIHSS, because prognostic variables differed at baseline, and age and baseline severity have an established influence on stroke outcomes (18). However, we could not adjust for all variables, as data were incomplete. Despite robust analyses and adjustment for important variables, we acknowledge that a randomized study would have the best design. But there are no such studies conducted yet or any that are ongoing. Ours is the only analyses available that is based on the largest dataset on thrombolysed patients available to date. It uses an analytic approach recommended by the EMEA and replicates findings of functional outcomes on neurological outcomes.
We know that patients with premorbid mRS >1 were excluded from the VISTA trials, but the prestroke functional status of individual patients were not recorded in VISTA. Hence, it is likely that any effect of prestroke disability in the patients having prior stroke(s) would only lead to an underestimation treatment effect in this analyses.
We agree that there could be differences on outcomes owing to center specific effects on treatment of patients. This would, however, occur if the patients were part of routine clinical care and not enrolled in rigorously controlled clinical trials. Because our patients were enrolled in neuroprotection clinical trials during 1998–2007, we assume that they all received the best standard of care at each participating center. A total of 60% of our patients were from American centers where the thrombolytic therapy was approved soon after the NINDS results were published in 1995 (2). During next years, even other centers (including European centers [16% patients]) practiced thrombolytic therapy based on clinicians' choice (13). In 2002, the alteplase was approved in Europe as well. This would imply that all those stroke patients who were eligible for thrombolysis in physician's opinion received therapy. However, we could not adjust for centers, as center-specific information was missing in our dataset.
Finally, one must consider that analyses like these are based on probabilistic models where level of significance is arbitrarily chosen (and conventionally set at 5%), and the decision to thrombolyse is left to the clinicians who determine their own limits regarding taking chances while offering the therapy. The group of patients having concomitant diabetes and previous strokes missed statistical significance but had a favorable point estimate of 1.5. Had we considered a higher level of significance, our results would have been significant for outcomes among all subgroups of patients.
In summary, our analysis shows improved outcomes among patients with diabetes, those who have had a prior stroke, and those with diabetes and/or prior stroke, though marginally failed to show a statistically significant improvement in the patients who had both diabetes and a prior stroke together. We however believe that a potential benefit might exist for the combined group too, and withholding a proven therapy among these patients would not be justified. Treatment may be offered to a carefully selected patient, and trialists should now be encouraged to consider examining these patients by conducting a randomized controlled trial. We recommend that withholding treatment from these patients is unjustified.
Acknowledgments
VISTA has received financial support from the European Stroke Organisation in the form of an unrestricted grant as well as contributions toward data extraction and capacity building from the Universities of Glasgow; California, San Diego; Nottingham; Edmonton; Calgary; Texas; Massachusetts; from commercial groups including Brainsgate, Novartis, Boehringer Ingelheim, and the Vertical Group; and from grant agencies and charities including the U.K. Stroke Association.
N.K.M. is supported by a British ORS Scholarship and the University of Glasgow Scholarship. M.K. has received honoraria (modest) from Boehringer Ingelheim, Forest Laboratories, Lundbeck, and Paion. S.M.D. has received support from Boehringer Ingelhiem, Ebewe, and sanofi-aventis. K.R.L. has received honoraria (modest) from Boehringer Ingelheim, Lundbeck, Thrombogenics, and Talecris. No other potential conflicts of interest relevant to this article were reported.
The analyses reported in this article were based on a research proposal approved by the VISTA Steering Committee and were undertaken by N.K.M. at the University of Glasgow. N.K.M. and K.R.L. designed and interpreted the analyses and drafted the manuscript; both had access to the VISTA data. M.K. and S.M.D. contributed data, reviewed the outline proposal, commented on the manuscript, and approved the final version. The manuscript was reviewed and approved by the VISTA Steering Committee. No commercial organization was involved in the origination, execution, or reporting of this work.
Parts of this article were presented in abstract form at the European Stroke Conference, Barcelona, Spain, 25–28 May 2010.
VISTA Steering Committee members: K.R. Lees (Chair) (Division of Cardiovascular and Medical Sciences, University of Glasgow, U.K.), L. Claesson (AstraZeneca, Södertälje, Sweden), E. Bluhmki (Boehringer Ingelheim, Biberach, Germany), B. Gregson (Department of Neurosurgery, Newcastle University, Newcastle General Hospital, U.K.), G. Donnan (Department of Neurology, University of Melbourne, Australia), H.C. Diener (Department of Neurology, University Duisburg-Essen, Hufelandstrasse, Essen, Germany), J. Grotta (Department of Neurology, University of Texas, Houston Medical School, TX), J. Marler and P. Teal (University of British Columbia, Vancouver, BC, Canada), M.G. Hennerici (Department of Neurology, Universitätsklinikum Mannheim, University of Heidelberg, Germany), N.G. Wahlgren (Karolinska Hospital, Stockholm, Sweden), P. Lyden (Cedars-Sinai Medical Center, Los Angeles, CA), P.W. Bath (Institute of Neuroscience, University of Nottingham, U.K.), R. Sacco (Miller School of Medicine, University of Miami, FL), S.M. Davis (Department of Neurology, Royal Melbourne Hospital, University of Melbourne, Australia), W. Hacke (Department of Neurology, University of Heidelberg, Germany), S. Warach (National Institute of Neurological Disorders and Stroke, Bethesda, MD), M. Fisher (Department of Neurology, University of Massachusetts Medical School, MA), M. Hommel (Joseph Fourier University, Grenoble, France), M.K. (Department of Neurology, Helsinki University Central Hospital, University of Helsinki, Finland), K. Muir (Division of Clinical Neurosciences University of Glasgow Glasgow, U.K.), A. Shuaib (Stroke Program, University of Alberta, Canada), C. Weimar (Department of Neurology, University Hospital Essen, University of Duisburg-Essen, Essen, Germany), A. Alexandrov (University of Alabama Hospital, Birmingham, AL). VISTA is a collaborative group based at the University of Glasgow, U.K.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D: ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359(13):1317–1329 [DOI] [PubMed] [Google Scholar]
- 2.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333(24):1581–1587 [DOI] [PubMed] [Google Scholar]
- 3.Martini SR, Kent TA: Hyperglycemia in acute ischemic stroke: a vascular perspective. J Cereb Blood Flow Metab 2007;27(3):435–451 [DOI] [PubMed] [Google Scholar]
- 4.Schurr A: Bench-to-bedside review: a possible resolution of the glucose paradox of cerebral ischemia. Crit Care 2002;6(4):330–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kruyt ND, Biessels GJ, Devries JH, Roos YB: Hyperglycemia in acute ischemic stroke: pathophysiology and clinical management. Nat Rev Neurol 2010;6(3):145–155 [DOI] [PubMed] [Google Scholar]
- 6.Kent DM, Selker HP, Ruthazer R, Bluhmki E, Hacke W: The stroke-thrombolytic predictive instrument: a predictive instrument for intravenous thrombolysis in acute ischemic stroke. Stroke 2006;37(12):2957–2962 [DOI] [PubMed] [Google Scholar]
- 7.Clark WM, Albers GW, Madden KP, Hamilton S: The rtPA (alteplase) 0- to 6-hour acute stroke trial, part A (A0276g): results of a double-blind, placebo-controlled, multicenter study. Thromblytic Therapy in Acute Ischemic Stroke Study Investigators. Stroke 2000;31(4):811–816 [DOI] [PubMed] [Google Scholar]
- 8.Clark WM, Wissman S, Albers GW, Jhamandas JH, Madden KP, Hamilton S: Recombinant tissue-type plasminogen activator (Alteplase) for ischemic stroke 3 to 5 hours after symptom onset: the ATLANTIS study: a randomized controlled trial. Alteplase Thrombolysis for Acute Noninterventional Therapy in Ischemic Stroke. JAMA 1999;282(21):2019–2026 [DOI] [PubMed] [Google Scholar]
- 9.Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, Larrue V, Bluhmki E, Davis S, Donnan G, Schneider D, Diez-Tejedor E, Trouillas P: Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II): Second European-Australasian Acute Stroke Study Investigators. Lancet 1998;352(9136):1245–1251 [DOI] [PubMed] [Google Scholar]
- 10.Committee for Proprietary Medicinal Products for the European Agency for the Evaluation of Medicinal Products Summary information on a referral opinion following an arbitration persuant to article 29 of directive 2001/83/EC for Actilyse [article online], 2002. Available at http://www.ema.europa.eu/docs/en_GB/document_library/referrals_ document/actilyse_29/WC500010327.pdf Accessed on 14 May 2010
- 11.Rubiera M, Ribo M, Santamarina E, Maisterra O, Delgado-Mederos R, Delgado P, Ortega G, Alvarez-Sabin J, Molina CA: Is it time to reassess the SITS-MOST criteria for thrombolysis? A comparison of patients with and without SITS-MOST exclusion criteria. Stroke 2009;40(7):2568–2571 [DOI] [PubMed] [Google Scholar]
- 12.Ali M, Bath PM, Curram J, Davis SM, Diener HC, Donnan GA, Fisher M, Gregson BA, Grotta J, Hacke W, Hennerici MG, Hommel M, Kaste M, Marler JR, Sacco RL, Teal P, Wahlgren NG, Warach S, Weir CJ, Lees KR: The Virtual International Stroke Trials Archive. Stroke 2007;38(6):1905–1910 [DOI] [PubMed] [Google Scholar]
- 13.Wahlgren N, Ahmed N, Davalos A, Ford GA, Grond M, Hacke W, Hennerici MG, Kaste M, Kuelkens S, Larrue V, Lees KR, Roine RO, Soinne L, Toni D, Vanhooren G: the SITS-MOST Investigators Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet 2007;369(9558):275–282 [DOI] [PubMed] [Google Scholar]
- 14.Committee for Proprietary Medicinal Products Points to consider on clinical investigation of medicinal products for the treatment of acute stroke [article online], 2001. Available at http://www.tga.gov.au/docs/pdf/euguide/ewp/056098en.pdf Accessed 28 August 2010
- 15.Lees KR, Davalos A, Davis SM, Diener HC, Grotta J, Lyden P, Shuaib A, Ashwood T, Hardemark HG, Wasiewski W, Emeribe U, Zivin JA: the SAINT I Investigators Additional outcomes and subgroup analyses of NXY-059 for acute ischemic stroke in the SAINT I trial. Stroke 2006;37(12):2970–2978 [DOI] [PubMed] [Google Scholar]
- 16.Saver JL, Gornbein J: Treatment effects for which shift or binary analyses are advantageous in acute stroke trials. Neurology 2009;72(15):1310–1315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Savitz SI, Lew R, Bluhmki E, Hacke W, Fisher M: Shift analysis versus dichotomization of the modified Rankin scale outcome scores in the NINDS and ECASS-II trials. Stroke 2007;38(12):3205–3212 [DOI] [PubMed] [Google Scholar]
- 18.Weimar C, Konig IR, Kraywinkel K, Ziegler A, Diener HC: Age and National Institutes of Health Stroke Scale Score within 6 hours after onset are accurate predictors of outcome after cerebral ischemia: development and external validation of prognostic models. Stroke 2004;35(1):158–162 [DOI] [PubMed] [Google Scholar]
- 19.Pandhi N, Smith MA, Kind AJ, Frytak JR, Finch MD: The quality of diabetes care following hospitalization for ischemic stroke. Cerebrovasc Dis 2009;27(3):235–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fedorov V, Mannino F, Zhang R: Consequences of dichotomization. Pharm Stat 2009;8(1):50–61 [DOI] [PubMed] [Google Scholar]
- 21.Bluhmki E, Windeler J, Hacke W: [Neurological scales as endpoints in stroke studies. Aspects of statistical evaluation]. Nervenarzt 2000;71(10):797–801[article in German] [DOI] [PubMed] [Google Scholar]
- 22.Saver JL: Novel end point analytic techniques and interpreting shifts across the entire range of outcome scales in acute stroke trials. Stroke 2007;38(11):3055–3062 [DOI] [PubMed] [Google Scholar]
- 23.Senn S, Julious S: Measurement in clinical trials: a neglected issue for statisticians?. Stat Med 2009;28(26):3189–209 [DOI] [PubMed] [Google Scholar]
- 24.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, Albers GW, Kaste M, Marler JR, Hamilton SA, Tilley BC, Davis SM, Donnan GA, Hacke W: the ECASS, ATLANTIS, NINDS and EPITHET rt-PA Study Group Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010;375(9727):1695–1703 [DOI] [PubMed] [Google Scholar]
- 25.Mishra NK, Ahmed N, Davalos A, Iversen HK, Soinne L, Wahlgren N, Lees KR: Post thrombolysis outcomes amongst patients with prior stroke and diabetes: controlled comparison of SITS international registry (SITS-ISTR) versus Virtual International Stroke Trials Archive (VISTA). Cerebrovasc Dis 2010;29(2):160 [Google Scholar]