Abstract
OBJECTIVE
To evaluate the effect of a prebreakfast high-protein snack upon postbreakfast hyperglycemia.
RESEARCH DESIGN AND METHODS
We studied 10 men and women with diet- and/or metformin-controlled type 2 diabetes. Metabolic changes after breakfast were compared between 2 days: breakfast taken only and soya-yogurt snack taken prior to breakfast.
RESULTS
There was a significant lower rise in plasma glucose on the snack day. The incremental area under the glucose curve was 450 ± 55 mmol · min/l on the snack day compared with 699 ± 99 mmol · min/l on the control day (P = 0.013). The concentration of plasma free fatty acids immediately before breakfast correlated with the increment in plasma glucose (r = 0.50, P = 0.013).
CONCLUSIONS
Consuming a high-protein prebreakfast snack results in almost 40% reduction of postprandial glucose increment. The second-meal effect can be applied simply and practically to improve postbreakfast hyperglycemia in people with type 2 diabetes.
Previous studies (1,2) have shown a considerable reduction in hyperglycemia after the second meal of the day, provided that breakfast had been taken. The preservation of this effect in type 2 diabetes was not confirmed until recently (3). Postprandial hyperglycemia acts as an independent risk factor for cardiovascular disease (4–6), a major cause of death in subjects with type 2 diabetes (7).
We hypothesized that postbreakfast hyperglycemia in subjects with type 2 diabetes could be improved nonpharmacologically by using a high-protein, low-carbohydrate prebreakfast snack.
RESEARCH DESIGN AND METHODS
Ten subjects (four female, six male) with type 2 diabetes treated by diet and/or metformin were recruited (aged 61 ± 2.3 years, waist-to-hip ratio 0.96 ± 0.01, BMI 28.8 ± 1.0 kg/m2, body fat 33.4 ± 2.6%, and A1C 6.7 ± 0.1%). The Newcastle and North Tyneside Research Ethics Committee No. 2 approved the study. All participants gave written informed consent.
Design and protocol
Every subject was studied on 2 separate days in random order with 2–4 week intervals. On both days, breakfast (51 g carbohydrate; 4.8 g fat; 5.8 g protein) was given at 10:00 a.m. On the snack day only, a snack (30 g soya beans; 75 g yogurt) was given 2 h before the breakfast. The details of metabolic testing, hormone, and metabolites assays were as previously described (3,8).
Statistical analysis
Data are expressed as means ± SEM. Paired Student t test was performed by SPSS (version 17.0; SPSS, Chicago). Incremental area under the curve (IAUC) was computed by the trapezoidal rule.
RESULTS
Plasma glucose
At baseline, 2 h before breakfast, fasting plasma glucose was similar on the 2 study days (6.6 ± 0.3 and 6.6 ± 0.4 mmol/l). The snack induced a small peak in plasma glucose at −60 min (7.3 ± 0.4 mmol/l). The concentrations of plasma glucose immediately before breakfast (t = 0 min) did not differ significantly between the 2 days (6.6 ± 0.3 vs. 6.4 ± 0.3 mmol/l, P = 0.45) (Fig. 1A).
Figure 1.
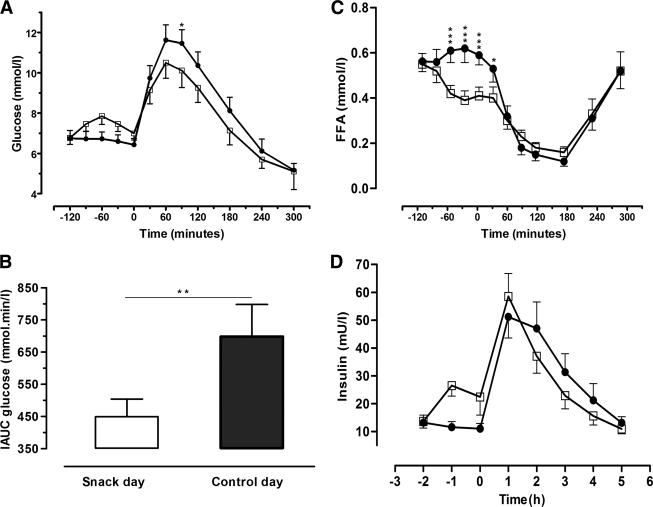
Metabolic changes between the 2 study days in 10 subjects with type 2 diabetes. A: Plasma glucose concentrations. B: Incremental area under the plasma glucose curves during the 5-h postbreakfast period. C and D: Change in FFA and insulin concentrations, respectively. *P < 0.05; **P < 0.02; ***P < 0.01; □, snack day; ●, control day.
Following breakfast, the rise in plasma glucose was lower on the snack day. IAUC was 450 ± 55 mmol · min/l compared with 699 ± 99 mmol · min/l for snack and control day, respectively (P = 0.013) (Fig. 1B). The 2-h postprandial plasma glucose concentration was significantly lower on the snack day compared with the control day (9.8 ± 0.3 vs. 10.8 ± 0.4 mmol/l, P = 0.001). Plasma glucose levels were identical in the two groups 5 h after breakfast.
Plasma free fatty acid
The fasting plasma free fatty acid (FFA) concentrations on both study days were similar (0.57 ± 0.05 and 0.57 ± 0.04 mmol/l, P = 0.9). After ingestion of the snack, plasma FFA concentration declined, falling to 70% of the fasting levels just before breakfast (0.41 ± 0.04 mmol/l). After breakfast, plasma FFA levels in both groups were suppressed (0.16 ± 0.02 vs. 0.14 ± 0.02 mmol/l for snack and control days, respectively) (Fig. 1C). FFA concentration before breakfast was positively correlated with the postprandial IAUC for plasma glucose (r = 0.50, P = 0.013).
Serum insulin and C-peptide
Fasting mean serum insulin levels were similar on the 2 study days (13.4 ± 2.4 and 13.2 ± 2.7 mU/l). On the snack day, insulin concentration rose promptly after ingestion of the snack to 26.5 ± 4.0 mU/l at −60 min and fell before breakfast (Fig. 1D). Following breakfast, insulin levels increased similarly on both days (58.5 ± 7.9 vs. 51.2 ± 7.6 mU/l) at 60 min. The mean insulin-to-C–peptide ratios from the area under the curves (t = 0–5 h) were similar on both days (13.6 ± 3.2 vs. 16. 9 ± 1.4 mU/nmol, P = 0.36) implying similar hepatic insulin extraction.
Substrate oxidation
Fasting glucose oxidation rates were not significantly different on the 2 study days (0.55 ± 0.18 vs. 0.77 ± 0.25 mg/kg · min, P = 0.37). On the snack day, glucose oxidation rate increased to 1.38 ± 0.24 mg/kg · min at 90 min after breakfast compared with 1.09 ± 0.25 mg/kg · min on the control day (P = 0.11). Fasting lipid oxidation rates were similar (0.7 ± 0.1 vs. 0.63 ± 0.12 mg/kg · min) and 90 min after breakfast decreased to 0.39 ± 0.09 vs. 0.51 ± 0.09 mg/kg · min, respectively (P = 0.09).
CONCLUSIONS
This study demonstrated for the first time that the provision of a practical, high-protein, low-carbohydrate snack prior to breakfast reduced by 40% the postprandial plasma glucose increment in people with type 2 diabetes. These findings confirm a potent expression of the second-meal effect in people with type 2 diabetes similar to that resulting from intravenous arginine infusion (3). The importance of the present observation is that a more practical means of improving glucose tolerance could potentially be of therapeutic benefit in people with type 2 diabetes.
We observed no effect of the prior snack on insulin secretion after breakfast. The mechanism underlying the second-meal effect has been shown to be due to suppression of plasma FFA, allowing greater storage of glucose as muscle glycogen (2). We previously demonstrated a strong negative correlation between the decrease of preprandial plasma FFA levels and the postmeal glucose increment. In the present study, a significant positive correlation was found between prebreakfast plasma FFA and the rise in postprandial plasma glucose concentration. This observation is analogous to the acute effect of the antilipolytic nicotinic acid analog acipimox (9).
The snack used in the present study was empirically designed. It will be important to optimize both the composition of the snack and the interval before breakfast to maximize the benefit of this approach. In everyday life, the gap between snack and breakfast would have to be accommodated, for instance, by delaying breakfast until mid-morning. Although the snack induced a small increase in plasma glucose, it was minimal and unlikely to contribute to the hyperglycemic burden. The sample size was dictated by prior power calculation (80% power with 10 subjects).
We have demonstrated that a high-protein, low-carbohydrate snack before breakfast attenuates postbreakfast hyperglycemia, and further studies must determine whether long-term use is associated with improvement in A1C.
Acknowledgments
This work was supported by Wellcome Trust Grant 073561 and the Newcastle National Institute for Health Research Biomedical Research Centre in Ageing.
No potential conflicts of interest relevant to this article were reported.
M.J.C. conducted the study, researched the data, and drafted the manuscript. A.J. designed the study and revised the manuscript. R.T. conceived the overall research question, researched the data, and revised the manuscript.
We thank Heather Cook of the Institute of Cellular Medicine, Newcastle University, for laboratory expertise; Jean Gerrard and Dr. Ee Lin Lim, both of the Institute of Cellular Medicine, Newcastle University, for clinical research support; and the volunteers for their time and cooperation.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
See accompanying editorial, p. 2709.
References
- 1.Carey PE, Halliday J, Snaar JE, Morris PG, Taylor R: Direct assessment of muscle glycogen storage after mixed meals in normal and type 2 diabetic subjects. Am J Physiol Endocrinol Metab 2003;284:E688–E694 [DOI] [PubMed] [Google Scholar]
- 2.Jovanovic A, Leverton E, Solanky B, Ravikumar B, Snaar JE, Morris PG, Taylor R: The second-meal phenomenon is associated with enhanced muscle glycogen storage in humans. Clin Sci 2009;117:119–127 [DOI] [PubMed] [Google Scholar]
- 3.Jovanovic A, Gerrard J, Taylor R: The second-meal phenomenon in type 2 diabetes. Diabetes Care 2009;32:1199–1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Vegt F, Dekker JM, Ruhé HG, Stehouwer CD, Nijpels G, Bouter LM, Heine RJ: Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia 1999;42:926–931 [DOI] [PubMed] [Google Scholar]
- 5.The DECODE Study Group on behalf of the European Diabetes Epidemiology Group Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet 1999;354:617–621 [PubMed] [Google Scholar]
- 6.Meigs JB, Nathan DM, D'Agostino RB, Sr, Wilson PW: Framingham Offspring Study Fasting and postchallenge glycemia and cardiovascular disease risk: the Framingham Offspring Study. Diabetes Care 2002;25:1845–1850 [DOI] [PubMed] [Google Scholar]
- 7.Laakso M: Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes 1999;48:937–942 [DOI] [PubMed] [Google Scholar]
- 8.Carey PE, Gerrard J, Cline GW, Dalla Man C, English PT, Firbank MJ, Cobelli C, Taylor R: Acute inhibition of lipolysis does not affect postprandial suppression of endogenous glucose production. Am J Physiol Endocrinol Metab 2005;289:E941–E947 [DOI] [PubMed] [Google Scholar]
- 9.Vaag A, Skött P, Damsbo P, Gall MA, Richter EA, Beck-Nielsen H: Effect of the antilipolytic nicotinic acid analogue acipimox on whole-body and skeletal muscle glucose metabolism in patients with non-insulin-dependent diabetes mellitus. J Clin Invest 1991;88:1282–1290 [DOI] [PMC free article] [PubMed] [Google Scholar]