Abstract
OBJECTIVE
To describe recent trends in the incidence of nontraumatic amputations among individuals with and without diabetes and estimate the relative risk of amputations among individuals with diabetes in England.
RESEARCH DESIGN AND METHODS
We identified all patients aged >16 years who underwent any nontraumatic amputation in England between 2004 and 2008 using national hospital activity data from all National Health Service hospitals. Age- and sex-specific incidence rates were calculated using the total diabetes population in England every year. To test for time trend, we fitted Poisson regression models.
RESULTS
The absolute number of diabetes-related amputations increased by 14.7%, and the incidence decreased by 9.1%, from 27.5 to 25.0 per 10,000 people with diabetes, during the study period (P > 0.2 for both). The incidence of minor and major amputations did not significantly change (15.7–14.9 and 11.8–10.2 per 10,000 people with diabetes; P = 0.66 and P = 0.29, respectively). Poisson regression analysis showed no statistically significant change in diabetes-related amputation incidence over time (0.98 decrease per year [95% CI 0.93–1.02]; P = 0.12). Nondiabetes-related amputation incidence decreased from 13.6 to 11.9 per 100,000 people without diabetes (0.97 decrease by year [0.93–1.00]; P = 0.059). The relative risk of an individual with diabetes undergoing a lower extremity amputation was 20.3 in 2004 and 21.2 in 2008, compared with that of individuals without diabetes.
CONCLUSIONS
This national study suggests that the overall population burden of amputations increased in people with diabetes at a time when the number and incidence of amputations decreased in the aging nondiabetic population.
Diabetic foot lesions remain a considerable cause of morbidity and a leading cause of hospitalization in people with diabetes (1). Despite intensive interventions, many of these patients require a lower extremity amputation (LEA), with high social impact and poor clinical prognosis for the patients, as well as considerable financial implications for health care systems (2).
The number of people diagnosed as having diabetes has more than doubled over the last 10 years in England (3). As the prevalence of diabetes increases due to an aging population and an increasing rate of obesity, an increase in the number of amputations is to be expected. We have recently reported that whereas the number of type 1 diabetes- and nondiabetes-related LEAs decreased in England between 1996 and 2005, there was a consistent upward trend in type 2 diabetes-related procedures (4). However, because of the lack of accurate information on diabetes prevalence, particularly for the early years of this period, we were unable to calculate diabetes-specific LEA incidence in England.
During the last decade, several initiatives have been undertaken in England to improve diabetes management across primary, community, and secondary care settings and specialist services (5,6). Corresponding with many studies from Europe and the U.S., a series of regional studies and centers highly specialized in diabetic foot care have shown significant decline in the incidence of LEAs after specific interventions were instituted (7–13). Others reported unchanged incidence of amputations in people with diabetes despite increasing vascular intervention rates (14–16). However, most studies report incidence rates from single centers and small geographical areas, and these data are unlikely to reflect national trends. Furthermore, the relative risk of amputations in diabetes has been rarely studied, particularly in larger geographical areas or nationally.
The objective of this study was to assess trends in nontraumatic LEAs among people aged >17 years with and without diabetes between financial years 2004–2005 and 2008–2009 using national hospital admission data from all National Health Service (NHS) hospitals in England. We describe diabetes- and nondiabetes-related incidence rates and assess the relative risk of people with diabetes undergoing a nontraumatic LEA (minor, major, and any) compared with those without diabetes in England.
RESEARCH DESIGN AND METHODS
We examined Hospital Episode Statistics (HES) between the financial years 2004–2005 and 2008–2009 for all NHS hospital trusts in England. The HES dataset covers all inpatient hospital activity and day case admissions to NHS (public) hospitals across England including private patients treated in NHS hospitals. Surgical interventions were defined using the Office of Population Censuses and Surveys' Classification of Surgical Operations (OPCS4) codes that contains up to 12 procedure fields. Data extracted for each hospital admission include patient demographics (age and sex), length of hospital stay, principal diagnosis, and up to 13 secondary diagnoses coded using the ICD-10.
All patients who underwent any LEA between financial years 2004–2005 and 2008–2009 were identified through having the procedure code for LEA in any procedure field. Different amputation codes during the same hospitalization on the same limb were assigned as a single procedure on the highest level. A contralateral limb amputation during the same admission was counted as a separate amputation. Side and level of LEA were recorded for each procedure (Z942 indicates the right side and Z943 the left). A minor amputation was defined as any LEA distal to the ankle joint (OPCS4 codes X11.1, X11.2, X11.8, and X11.9); a major amputation was defined as any LEA through or proximal to the ankle joint (OPCS4 codes X09.2–5, X09.9, X10.1–4, and X10.8–9). All traumatic LEAs, defined by any trauma-related code of the lower extremity in any diagnosis field (S70–99, T00–35, Wxx, and Xxx), were excluded from our analysis. Diabetes status was classified as no diabetes or type 1 or type 2 diabetes (ICD-10 code E10–E11) codes recorded in any diagnosis field. Other forms of diabetes (ICD-10 E12–E14) were excluded.
When age-, sex-, and diabetes-specific LEAs were examined in patients with multiple admissions during the same financial year, only first admissions were used to derive patient characteristics. We used a combination of date of birth, sex, and full postcode to distinguish patients, as these were the only identifiers available for all years in this study.
Data on the number of people aged >17 years having a diagnosis of diabetes in England were obtained from the Quality Management and Analysis System (QMAS) for each study year (5). QMAS is the financial database for the Quality and Outcomes Framework (QOF), a national pay for performance scheme for primary care practices introduced in April 2004, and contains diabetes counts and prevalence data for virtually all (>99%) family practices in England (5). For 2004–2005 and 2005–2006, when diabetes figures were available for the total population, we calculated diabetes prevalence for patients aged ≥17 years for both years, using the age- and sex-standardized diabetes prevalence in children and young adults reported by the Royal College of Pediatrics and Child Health (17). Diabetes-specific incidence rates were expressed per 10,000 people with diabetes. Data for the age and sex distribution of individuals with diabetes were obtained from the Health Survey for England 2006 (3). When age- and sex-specific prevalence rates of known diabetes were calculated for the general population of England, we assumed that the age and sex distribution of the diabetic population remained constant between 2004 and 2008. The estimated resident population of England was used to calculate incidence of amputations in individuals without diabetes for each year and incidence rates are expressed per 100,000 people without diabetes.
Ethical approval
We have Section 251 approval from the National Information Governance Board for Health and Social Care (formerly Section 60 approval from the Patient Information Advisory Group) to hold confidential data and analyze them for research purposes. We also have approval from the South East Research Ethics Committee.
Statistical analysis
Statistical analyses were performed using the Stata statistical package. Median lengths of stay were compared by type of LEA and diabetes status with the Brown-Forsythe test (18). To test time trends in LEA rates, we fitted separate Poisson regression models for patients with and without diabetes, using age, sex, and level of amputation as independent variables. We estimated relative risk of an individual with diabetes undergoing a LEA (minor, major, and any) compared with that of an individual without diabetes.
RESULTS
Over the study period between 2004 and 2008, there were 49,487 nontraumatic LEAs performed on 45,424 patients in England. Of all amputations, 51% occurred among people with diabetes (59.6% of minor and 42.6% of major LEAs). There was a considerable male excess of LEAs among people with diabetes with the male-to-female ratio being nearly twice that of people without diabetes (male-to-female ratio diabetes 2.7 [95% CI 1.7–3.7] and nondiabetes 1.4 [0.8–2.1]). Most LEAs occurred in individuals aged >65 years (60.4% of diabetes-related and 68.3% of nondiabetes-related LEAs). Minor amputations were more common than major LEAs in individuals with diabetes, whereas there was a predominance of major LEAs in individuals without diabetes (minor-to-major ratio for diabetes 1.4 [1.2–1.7] and for nondiabetes 0.7 [0.6–0.8]).
Diabetes-related amputations
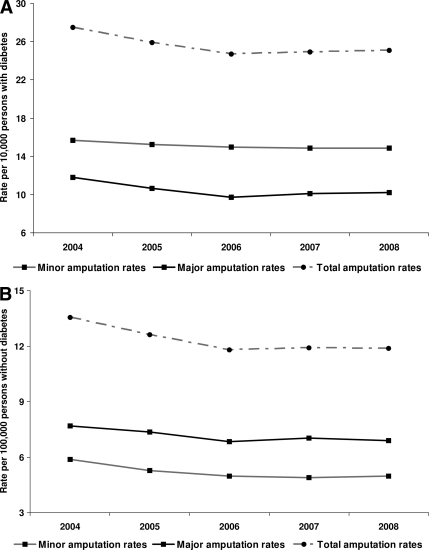
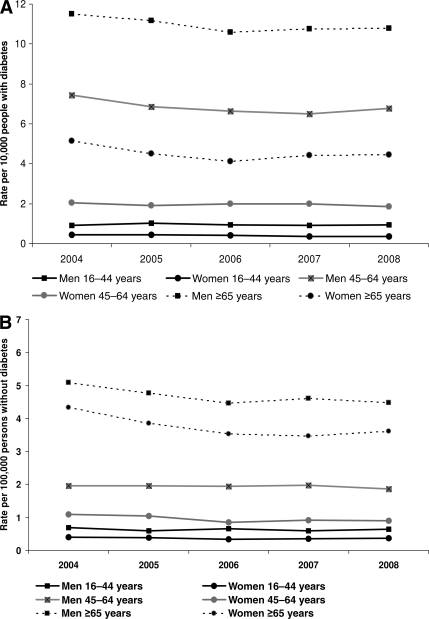
Between 2004 and 2008, the number of patients who underwent an amputation and the number of amputations performed increased significantly among individuals with diabetes in England (Table 1). Overall amputation incidence rates (minor and major combined) decreased by 9.1%, from 27.5 per 10,000 people with diabetes in 2004 to 25.0 per 10,000 people with diabetes in 2008. During the study period, the incidence of minor LEAs (15.7 to 14.9 per 10,000 people with diabetes; P = 0.66) and major LEA rates (11.8 to 10.2 per 10,000 people with diabetes; P = 0.29) decreased slightly, but this decrease did not reach statistical significance (Fig. 1A). Incidence of LEAs was significantly higher among men than among women with diabetes (P < 0.001). However, changes in overall LEA rates did not significantly differ between men and women (19.9 to 18.3 vs. 7.6 to 6.7 per 10,000 people with diabetes; P = 0.81) (Fig. 2). When stratified by age, the incidence was the highest among individuals aged >65 years in both men and women (Fig. 2). Poisson regression analysis showed no significant decrease in incidence of amputations after adjustment for age, sex, year, and level of amputation (0.98 decrease per year [95% CI 0.93–1.02]; P = 0.12).
Table 1.
Characteristics of amputees between the financial years 2004–2005 and 2008–2009 in England
| Diabetes-related LEAs |
P value | Nondiabetes-related LEAs |
P value | |||
|---|---|---|---|---|---|---|
| 2004–2005 | 2008–2009 | 2004–2005 | 2008–2009 | |||
| Minor amputations | — | |||||
| No. of amputations | 2,768 | 3,289 | 2,266 | 1,966 | ||
| Patient-to-amputation ratio | 0.89 (0.88–0.91) | 0.88 (0.86–0.90) | 0.81 | 0.95 (0.94–0.97) | 0.95 (0.93–0.97) | 0.81 |
| Sex, male | 2,044 (73.8) | 2,450 (74.5) | 0.57 | 1,125 (49.6) | 1,064 (54.1) | 0.004 |
| Age-group | ||||||
| 16–44 years | 167 (6.0) | 204 (6.2) | 0.85 | 198 (8.8) | 152 (7.7) | 0.42 |
| 45–64 years | 1,045 (37.8) | 1,248 (37.9) | 524 (23.1) | 481 (24.5) | ||
| ≤65 years | 1,556 (56.2) | 1,837 (55.8) | 1,544 (68.1) | 1,333 (67.7) | ||
| Hospital length of stay (days) | 15 (7–30) | 13 (6–25) | 0.001 | 5 (2–19) | 6 (1–21) | 0.41 |
| Major amputations | ||||||
| No. of amputations | 2,084 | 2,277 | 2,963 | 2,731 | ||
| Patient-to-amputation ratio (95% CI) | 0.88 (0.86–0.90) | 0.88 (0.85–0.9) | 0.98 | 0.95 (0.92–0.97) | 0.94 (0.93–0.96) | 0.81 |
| Sex, male | 1,465 (70.2) | 1,640 (72.0) | 0.21 | 1,860 (62.8) | 1,699 (62.2) | 0.68 |
| Age-group | ||||||
| 16–44 years | 73 (3.5) | 83 (3.6) | 0.48 | 222 (7.5) | 247 (9.0) | 0.48 |
| 45–64 years | 628 (30.1) | 663 (29.1) | 654 (22.1) | 614 (22.5) | ||
| ≤65 years | 1,383 (66.4) | 1,531 (67.2) | 2,087 (70.4) | 1,870 (68.5) | ||
| Hospital length of stay (days) | 38 (22–69) | 34 (20–59) | <0.001 | 32 (17–58) | 28 (15–52) | <0.001 |
Data are ratio (95% CI), n (%), or median (interquartile range).
Figure 1.
Changes in minor and major amputation incidence rates in (A) individuals with diabetes expressed per 10,000 people with diabetes and (B) individuals without diabetes expressed per 100,000 people without diabetes.
Figure 2.
Changes in amputation incidence rates between 2004–2005 and 2008–2009 in England in (A) individuals with diabetes expressed per 10,000 people with diabetes and (B) individuals without diabetes expressed per 100,000 people without diabetes, by age and sex.
Nondiabetes-related amputations
The number of people without diabetes who underwent a LEA and the number of amputations performed decreased during the study period. Although the percentage of men undergoing minor amputations increased significantly, male predominance was not evident among minor amputees (Table 1). Amputation incidence (minor and major combined) decreased from 13.6 per 100,000 people without diabetes in 2004 to 11.9 per 100,000 people without diabetes in 2008. Incidence of minor LEAs decreased significantly from 5.9 to 5.0 per 100,000 people without diabetes (P = 0.01). There was a nonsignificant reduction in the incidence of major LEAs among individuals without diabetes, from 7.7 to 6.9 per 100,000 people (P = 0.39) (Fig. 1B). The fall in LEA rates was achieved between 2004 and 2006, and incidence rates remained constant afterward for both minor and major procedures. Incidence of LEAs declined among both men and women (Fig. 2). Of all decreases, 76% have been achieved through a reduction in LEAs in people aged >65 years (Fig. 2). Poisson regression analysis showed that the decline in nondiabetes-related LEAs was marginally significant after adjustment for age, sex, level of amputation, and year (0.97 decrease by year [95% CI 0.93–1.00], P = 0.059).
Relative risk of amputations
The risk of an individual with diabetes undergoing a LEA was 20.3 times that of an individual without diabetes in 2004 and did not significantly change by 2008 (P = 0.317) (Table 2).
Table 2.
Relative risk of LEAs in individuals with diabetes compared with those without diabetes between 2004–2005 and 2008–2009 in England
| Minor amputations | Major amputations | All amputations | |
|---|---|---|---|
| 2004–2005 | 27.0 (25.5–28.5) | 15.5 (14.7–16.4) | 20.5 (19.7–21.3) |
| 2005–2006 | 29.3 (27.7–31.0) | 14.6 (13.8–15.5) | 20.7 (19.9–21.6) |
| 2006–2007 | 30.2 (28.5–31.9) | 14.2 (13.4–15.1) | 20.9 (20.1–21.8) |
| 2007–2008 | 30.4 (28.7–32.2) | 14.4 (13.6–15.2) | 21.0 (20.2–21.8) |
| 2008–2009 | 29.9 (28.3–31.7) | 14.9 (14.1–15.7) | 21.2 (20.4–22.1) |
Data are relative risk (95% CI). P < 0.001 for all.
CONCLUSIONS
This nationwide study was undertaken to quantify the incidence and relative risk of nontraumatic amputations in people with and without diabetes between 2004 and 2008 in England. Our results indicate an increasing number of procedures and a nonstatistically significant decline in the incidence of amputations in people with diabetes. Over the study period, the incidence of diabetes-related amputations decreased by 9.1%, from 27.5 to 25.0 per 10,000 people with diabetes. In contrast, the number and incidence of LEAs decreased in individuals without diabetes, and this decline was marginally significant in a regression model. As expected, we found a markedly increased risk of amputations in individuals with diabetes compared with those without diabetes.
In recent years, a series of studies have reported decreasing incidence of amputations from the U.S. and Western Europe (6,7,10–12). Regional studies identified large geographical variations in peripheral vascular disease and amputation incidence. In England, the lowest diabetes-related amputation rates were recorded in centers in Leicester and Ipswich (11.0 and 16.0 per 10,000 people with diabetes, respectively) and considerably higher incidence was identified in Middlesbrough (44.6 per 10, 000 people with diabetes) (13,19). Wide variations in the incidence of diabetes-related LEAs have been reported across nationwide studies from Western Europe. In Germany, incidence was reported as 40.2 and 17.4 per 10,000 people with diabetes in men and women, respectively and in the Netherlands as 36 per 10,000 people with diabetes (7,10). Several factors have been described that might explain these differences, such as differences in study methodology, estimation of the denominator, prevalence of diabetes, case mix, availability of foot clinics, diabetes specialists, treatment programs and resources, the treatment approach of an expert team, and demographic and clinical confounding factors, among others (20). Canavan et al. (9) identified prominently high major LEA incidence (56.4 per 10,000 people with diabetes) in the South Tees area, which was attributed to the gaps in knowledge and incomplete foot care in individuals with diabetes. This rate decreased to 17.6 per 10,000 people with diabetes during a 5-year period as a result of better organized diabetes care. Schofield et al. (6) found decreasing amputation rates in Tayside, Scotland, and suggested that better control for cardiovascular risk factors might partly explain this reduction.
During the last decade, there have been substantial improvements in quality of diabetes management in U.K. primary care in response to a wide range of initiatives such as national treatment standards for the management of major chronic diseases (5,21). Despite these developments, this study found no evidence that the diabetes-related amputation incidence has significantly decreased over the last 5 years. Risk factor intervention studies have failed to demonstrate reduction in peripheral arterial disease-related clinical end points (22). It is possible that interventions to address the surrogate end points measured and rewarded as part of QOF have not been shown to translate into reductions in clinical peripheral arterial disease-related end points.
The relative risk of amputation in people with diabetes compared with those without diabetes did not significantly change over the study period in England (20.5 in 2004 and 21.2 in 2008). Previous reports from small geographic areas showed large variations in relative risk of amputations in England (from 7.7 to 31.6) (9,19). Nationwide studies from other Western European countries also reported varying relative risk of LEAs (20.3 in the Netherlands and 7.4 in Germany) (10,23).
When calculating diabetes-specific incidence rates, we used the total number of people with diabetes in England as denominator, based on data from QMAS (5). During the study period, the prevalence of diabetes increased from 4.4 to 5.2% in people aged ≥17 years in England (5,17). The modest reduction in diabetes-related amputation incidence occurred between 2004 and 2006, and LEA rates remained fairly constant afterward. A clear explanation for this finding is lacking because the rise in the denominator was steady over the study period; therefore, it is not likely to explain this trend. Furthermore, a similar pattern was found in people without diabetes. It is possible that an increased number of subjects with shorter diabetes duration and without complications in the diabetic population might explain this finding (6).
To the best of our knowledge, this is the first study to identify diabetes-related amputation incidence using a national sample that covers the entire population of England. Previous reports have mostly documented center-oriented or regional information (8,9,13,19). The results of these studies may not be generalizable because these centers might be highly specialized in diabetic foot care and have a relatively small number of amputations. Furthermore, the calculation of denominators may be flawed because of the potential overlap between the catchment areas of different institutions and patient referrals from or to other centers. In contrast, denominator data for our survey were derived from a comprehensive national database. These estimates are likely to be robust, given that an estimated 99% of the U.K. population are registered with a family practitioner and nearly 100% of practices participate in the pay for performance scheme that incentivizes completeness of disease registers (5).
We were able to distinguish individual patients and therefore multiple hospitalizations using information on date of birth, sex, and full postcode. Information on laterality of amputations was also available in this study with very high completeness, enabling identification of LEAs on different limbs during the same admission, and these procedures could be counted separately. Furthermore, we examined both minor and major amputations and reported LEA incidence separately by level of procedure and also included a nondiabetes comparator (11,24).
Limitations have to be considered in interpretation of our results. Because of the lack of accurate data on the age- and sex-specific prevalence of diabetes, we used the stratum-specific prevalence data from 2006, the mid-term of our study period and had to assume that this information remained constant between 2004 and 2008 (3). The increase in prevalence of diabetes during the study period might be partly explained by better ascertainment and recording of diabetes after the implementation of pay for performance in 2004. However, the increase was consistent during the study period and most of the improved ascertainment is likely to have occurred immediately before the study period as practices responded to the incentives in QOF. We did not distinguish between type 1 and type 2 diabetes because separate data on national prevalence of different types were not available. Furthermore, we could not evaluate misclassification due to undiagnosed and unrecorded cases of diabetes.
Although concerns about the accuracy of routinely collected datasets has been raised, these data are continuously audited and the quality and validity of this dataset has been assessed and proved useful for health research (25).
In summary, in this study we found no evidence that the incidence of amputations has significantly decreased over the last 5 years among people with diabetes in England. In contrast to the results from regional studies in England, the population burden of amputations increased in people with diabetes at a time when both the number and incidence of amputations decreased in the aging general population. There is strong evidence to support the fact that much of this burden is preventable through existing interventions, and our findings highlight the need to further improve foot care for people with diabetes.
Acknowledgments
The research leading to these results has received funding from the European Community Seventh Framework Programme FP7/2007-11 under grant agreement 236336. A.B. and the Dr Foster Unit at Imperial College London are largely funded by Dr Foster Intelligence, an independent health care information company. C.M. is funded by the Higher Education Funding Council for England and the National Institute for Health Research. The Department of Primary Care and Public Health at Imperial College London acknowledges support from the National Institute for Health Research Biomedical Research Centre Scheme and the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care Scheme.
No potential conflicts of interest relevant to this article were reported.
E.P.V. conceived the idea for the study, researched data, and wrote the manuscript. A.B. researched data and reviewed/edited the manuscript. M.E.E., J.V., and A.M. contributed to discussion and reviewed/edited manuscript. C.M. conceived the idea for the study and wrote the manuscript.
Parts of this study were presented in abstract form at the 46th annual meeting of the European Association for the Study of Diabetes, Stockholm, Sweden, 20–24 September 2010.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J: The global burden of diabetic foot disease. Lancet 2005;366:1719–1724 [DOI] [PubMed] [Google Scholar]
- 2.Reiber GE, Lipsky BA, Gibbons GW: The burden of diabetic foot ulcers. Am J Surg 1998;176:5S–10S [DOI] [PubMed] [Google Scholar]
- 3.Department of Health Health survey for England [article online], 2007. Available from http://www.dh.gov.uk/en/Publicationsand statistics/PublishedSurvey/HealthSurvey ForEngland/Healthsurveyresults/index.htm Accessed 16 April 2010
- 4.Vamos EP, Bottle A, Majeed A, Millett C: Trends in lower extremity amputations in people with and without diabetes in England, 1996–2005. Diabetes Res Clin Pract 2010;87:275–282 [DOI] [PubMed] [Google Scholar]
- 5.The NHS Information Centre The quality and outcomes framework: audits and performance [article online], 2009. Available from http://www.ic.nhs.uk/statistics-and- data-collections/audits-and-performance/ the-quality-and-outcomes-framework Accessed 16 April 2010
- 6.Schofield CJ, Yu N, Jain AS, Leese GP: Decreasing amputation rates in patients with diabetes-a population-based study. Diabet Med 2009;26:773–777 [DOI] [PubMed] [Google Scholar]
- 7.van Houtum WH, Rauwerda JA, Ruwaard D, Schaper NC, Bakker K: Reduction in diabetes-related lower-extremity amputations in The Netherlands: 1991–2000. Diabetes Care 2004;27:1042–1046 [DOI] [PubMed] [Google Scholar]
- 8.Edmonds ME, Blundell MP, Morris ME, Thomas EM, Cotton LT, Watkins PJ: Improved survival of the diabetic foot: the role of a specialized foot clinic. Q J Med 1986;60:763–771 [PubMed] [Google Scholar]
- 9.Canavan RJ, Unwin NC, Kelly WF, Connolly VM: Diabetes- and nondiabetes-related lower extremity amputation incidence before and after the introduction of better organized diabetes foot care: continuous longitudinal monitoring using a standard method. Diabetes Care 2008;31:459–463 [DOI] [PubMed] [Google Scholar]
- 10.Icks A, Haastert B, Trautner C, Giani G, Glaeske G, Hoffmann F: Incidence of lower-limb amputations in the diabetic compared to the non-diabetic population. Findings from nationwide insurance data, Germany, 2005–2007. Exp Clin Endocrinol Diabetes 2009;117:500–504 [DOI] [PubMed] [Google Scholar]
- 11.Holstein P, Ellitsgaard N, Olsen BB, Ellitsgaard V: Decreasing incidence of major amputations in people with diabetes. Diabetologia 2000;43:844–847 [DOI] [PubMed] [Google Scholar]
- 12.Wang J, Imai K, Engelgau MM, Geiss LS, Wen C, Zhang P: Secular trends in diabetes-related preventable hospitalizations in the United States, 1998–2006. Diabetes Care 2009;32:1213–1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krishnan S, Nash F, Baker N, Fowler D, Rayman G: Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care 2008;31:99–101 [DOI] [PubMed] [Google Scholar]
- 14.Tunis SR, Bass EB, Steinberg EP: The use of angioplasty, bypass surgery, and amputation in the management of peripheral vascular disease. N Engl J Med 1991;325:556–562 [DOI] [PubMed] [Google Scholar]
- 15.McCaslin JE, Hafez HM, Stansby G: Lower-limb revascularization and major amputation rates in England. Br J Surg 2007;94:835–839 [DOI] [PubMed] [Google Scholar]
- 16.Trautner C, Haastert B, Spraul M, Giani G, Berger M: Unchanged incidence of lower-limb amputations in a German City, 1990–1998. Diabetes Care 2001;24:855–859 [DOI] [PubMed] [Google Scholar]
- 17.Royal College of Paediatrics and Child Health Growing up with diabetes: children and young people with diabetes in England [article online], 2009. Available from http://www.diabetes.org.uk/Documents/Reports/CYP_Diabetes_Survey_ Report.pdf Accessed 16 April 2010
- 18.Brown MB, Forsythe AB: Robust tests for equality of variances. J Am Stat Assoc 1974;69:364–367 [Google Scholar]
- 19.Canavan RJ, Connolly VM, McIntosh J, Airey M, Burden F, Unwin NC: Geographic variations in lower extremity amputation rates. Diabetic Foot 2003;6:82–89 [Google Scholar]
- 20.Jeffcoate WJ, van Houtum WH: Amputation as a marker of the quality of foot care in diabetes. Diabetologia 2004;47:2051–2058 [DOI] [PubMed] [Google Scholar]
- 21.Department of Health Six years on: delivering the Diabetes National service Framework [article online], 2010. Available from http://www.dh.gov.uk/publications Accessed: 19 May 2010
- 22.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 23.van Houtum WH, Lavery LA, Harkless LB: The impact of diabetes-related lower-extremity amputations in The Netherlands. J Diabetes Complications 1996;10:325–330 [DOI] [PubMed] [Google Scholar]
- 24.Ebskov B, Ebskov L: Major lower limb amputation in diabetic patients: development during 1982 to 1993. Diabetologia 1996;39:1607–1610 [DOI] [PubMed] [Google Scholar]
- 25.Campbell SE, Campbell MK, Grimshaw JM, Walker AE: A systematic review of discharge coding accuracy. J Public Health Med 2001;23:205–211 [DOI] [PubMed] [Google Scholar]