Abstract
OBJECTIVE
Neuropathic pain due to small-fiber sensory neuropathy in type 2 diabetes can be diagnosed by skin biopsy with quantification of intra-epidermal nerve fiber (IENF) density. There is, however, a lack of noninvasive physiological assessment. Contact heat–evoked potential (CHEP) is a newly developed approach to record cerebral responses of Aδ fiber–mediated thermonociceptive stimuli. We investigated the diagnostic role of CHEP.
RESEARCH DESIGN AND METHODS
From 2006 to 2009, there were 32 type 2 diabetic patients (20 males and 12 females, aged 51.63 ± 10.93 years) with skin denervation and neuropathic pain. CHEPs were recorded with heat stimulations at the distal leg, where skin biopsy was performed.
RESULTS
CHEP amplitude was reduced in patients compared with age- and sex-matched control subjects (14.8 ± 15.6 vs. 33.7 ± 10.1 μV, P < 0.001). Abnormal CHEP patterns (reduced amplitude or prolonged latency) were noted in 81.3% of these patients. The CHEP amplitude was the most significant parameter correlated with IENF density (P = 0.003) and pain perception to contact heat stimuli (P = 0.019) on multiple linear regression models. An excitability index was derived by calculating the ratio of the CHEP amplitude over the IENF density. This excitability index was higher in diabetic patients than in control subjects (P = 0.023), indicating enhanced brain activities in neuropathic pain. Among different neuropathic pain symptoms, the subgroup with evoked pain had higher CHEP amplitudes than the subgroup without evoked pain (P = 0.011).
CONCLUSIONS
CHEP offers a noninvasive approach to evaluate the degeneration of thermonociceptive nerves in diabetic neuropathy by providing physiological correlates of skin denervation and neuropathic pain.
Type 2 diabetic neuropathy is frequently complicated with neuropathic pain, suggesting the involvement of small-diameter thermonociceptive nerves (1). Two approaches have been developed for the diagnosis of small-fiber sensory neuropathy: psychophysical assessments by measuring thermal thresholds on quantitative sensory testing (2,3) and pathological evaluations by quantifying intra-epidermal nerve fiber (IENF) density in punch skin biopsies (4–6). These examinations provide psychophysical and neuropathological evidence of small-diameter thermonociceptive nerve degeneration and serve as the definition of small-fiber sensory neuropathy (7,8). These two tests are sensitive in detecting the negative symptoms of diabetic neuropathy, for example, the elevation of thermal thresholds (9). However, the neurophysiological correlates of these tests with positive symptoms such as neuropathic pain are limited, and the physiological consequences of thermonociceptive nerve involvements in diabetic neuropathy have rarely been explored.
In recent years, several groups, including our own, have established contact heat–evoked potential (CHEP) as a clinically feasible approach to examine the physiology of thermonociceptive nerves (10,11). CHEP, by activating Aδ fibers, can be recorded at the vertex for clinical use (12). Thus, CHEPs provide a noninvasive technique to objectively evaluate the physiology of thermonociceptive nerve dysfunctions. This approach raises the possibility of whether CHEP can be a noninvasive diagnostic tool complementary to IENF density and thermal thresholds and whether CHEP parameters can reflect the neurophysiological correlates of reduced IENF density in diabetic neuropathy. Additionally, since the CHEP amplitude parallels the perceived intensity of heat pain in normal subjects (11,13), a further critical issue is whether CHEP could demonstrate positive symptoms or signs of neuropathic pain in diabetic neuropathy. These include the spontaneous forms, such as a burning sensation, and the evoked forms, such as hyperalgesia to thermal stimuli.
To address the above issues, our study investigated the following: 1) the changes in CHEP and its diagnostic role in diabetic neuropathy, 2) the correlations of CHEP with the skin innervation and thermal thresholds, and 3) the relationship of CHEP and neuropathic pain in diabetic neuropathy.
RESEARCH DESIGN AND METHODS
The study population consisted exclusively of type 2 diabetic patients with neuropathic pain referred to the Department of Neurology, National Taiwan University Hospital, Taipei, Taiwan, from January 2006 to December 2009. The inclusion criteria were 1) symmetrical neuropathic pain symptoms in the feet with a graded stocking pattern of distribution and 2) degeneration of thermonociceptive nerves with reduced IENF density on skin biopsy at the leg. The features of neuropathic pain in the feet and legs were further categorized as evoked pain (thermal hyperalgesia and touch-induced allodynia), tingling (or shooting), lacerating, hot (or burning), cold (or freezing), electric shock, and numbness. Neurological examinations followed routine procedures with detailed assessments of the sensations to heat, cold, pinprick, and vibratory stimuli. Patents with weakness of limbs were excluded. There were 32 diabetic patients (20 males and 12 females) aged 51.6 ± 10.9 years (range 22–65) fulfilling the above criteria, i.e., with symmetric neuropathic pain symptoms and pathological evidence of skin denervation. The duration of diabetes was 8.25 ± 6.60 years (range 0.25–26), and the duration of neuropathic pain was 1.79 ± 1.96 years (range 0.1–7). Data of glycemic control including fasting and 2-h postprandial glucose levels and A1C 3 years before our evaluation were analyzed for patients with diabetes duration longer than 3 years. For those patients with diabetes duration shorter than 3 years, all data before the skin biopsy were collected for analysis.
The Ethics Committee of National Taiwan University Hospital approved this study. Informed consent was obtained from each subject before the procedures.
Each patient had received skin biopsy, CHEP, quantitative sensory testing, and nerve conduction study. All these tests followed established protocols and are detailed in the methods section in the online appendix (available at http://care.diabetesjournals.org/cgi/content/full/dc10-1135/DC1). Results were interpreted according to our previously described normative databases (14,15).
Analysis of CHEP
The analysis of CHEP waveforms was based on an averaged tracing of the first 16 artifact-free tracings (detailed in the online appendix) using the Nicolet EP Vue system (Nicolet Biomedical, Madison, WI). In normal subjects, the control tests showed no recognizable waveforms, and contact heat stimulation of the lateral leg evoked well-defined waveforms at Cz with an initial negative peak (N-wave) followed by a positive peak (P-wave) as described previously (10,15). We measured the N-wave latency as the CHEP latency and the amplitude between the N-wave and P-wave as the CHEP amplitude. Since the reporting of our normative data (15), we have continuously updated normative values of CHEP every year. The normative database now consisted of 92 healthy subjects (40 men and 52 women) aged 40.6 ± 12.0 years (range 22–65). The updated normative values were 448.4 ± 34.4 and 506.4 ms for CHEP latency (mean ± SD and 95th percentile) and 38.6 ± 11.2 and 25.4 μV for CHEP amplitude (mean ± SD and 5th percentile).
The CHEP amplitude and the IENF density assess two different dimensions of neuropathy. Two observations mandate the necessity for an index to integrate these two independent parameters and to investigate the relationship between the CHEP amplitude and IENF density in diabetic painful neuropathy. First, CHEP represents the cerebral responses to thermal pain stimuli and is highly correlated with pain perception (11,13). Second, CHEP is generated through the activation of cutaneous terminals of thermonociceptive small-fiber nerves and therefore is affected by changes in IENF density. IENF represents the nociceptive input and CHEP reflects the output from nociceptive stimuli. To investigate whether there was amplification in signals from the input to the output between control subjects and diabetic patients, we defined an excitability index. The excitability index was calculated by normalizing CHEP amplitude to the IENF density, i.e., the ratio of the CHEP amplitude over the IENF density. Because the IENF density is in the denominator and IENF densities are calculated to the first decimal place, the IENF density was defined as 0.1 fibers/mm if the skin was completely denervated in calculating the excitability index.
Study design and data analysis
Data of the 32 patients were compared with data of 32 age- and sex-matched subjects (15 men and 17 women, aged 47.1 ± 15.1 years; P = 0.22 for sex and P = 0.18 for age). All had normal IENF density (8.8 ± 2.4 fibers/mm). Numerical variables are expressed as the mean ± SD and were compared with t tests if the data followed a Gaussian distribution. If the sample size was small, the numerical variables were compared using the nonparametric test (Wilcoxon rank sum test). Correlations between variables were graphically analyzed using the slope of the regression line, including the 95% CI. The correlation was further explored with a multiple linear regression analysis, and the covariance of the model R2 and the standardized correlation coefficient are presented. All analyses were performed using Stata software (StataCorp LP, College Station, TX). Results were considered significant at P < 0.05.
RESULTS
Clinical presentations
The demographic data, diabetic status, and neuropathic pain profiles are summarized in supplementary Table A1 in the online appendix. The symptoms of neuropathic pain were diverse, ranging from evoked pain (10, 31.3%) to numbness (25, 78.1%). Based on neurological examinations, 29 (90.6%) had impaired senses mediated by small fibers (pinprick, heat, and coldness) and 21 (65.6%) patients had dysfunction of large fibers (vibration).
The IENF density was reduced in all these patients: 1.1 ± 1.5 fibers/mm (range 0–5.7 fibers/mm). In total, 27 patients (84.4%) had elevated thermal thresholds on quantitative sensory testing: 26 with elevated warm thresholds and 9 with elevated cold thresholds at the foot dorsum. For large fibers with nerve conduction study, 16 patients (50%) had reduced sensory action potential amplitudes or decreased conduction velocities in the sural nerve, and 21 (65.6%) had reduced CMAP amplitude or decreased conduction velocity in the peroneal nerve.
CHEP in diabetic neuropathy
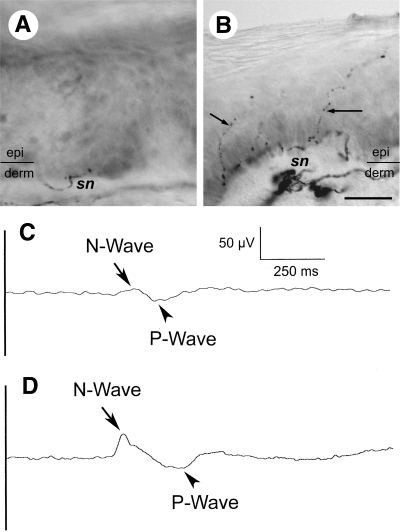
To explore the neurophysiological changes due to thermonociceptive nerve degeneration in type 2 diabetes, we analyzed CHEP parameters in these patients. CHEP amplitudes were reduced in diabetic patients compared with age- and sex-matched control subjects (14.8 ± 15.6 vs. 33.7 ± 10.1 μV, P < 0.001), and 26 patients (81.3%) had abnormal CHEP patterns. Among them, 13 patients had absence of CHEP waveform, and all of them had either complete denervation (in 9 cases) or very low IENF density (in 4 cases with IENF density of 0.2–0.9 fibers/mm); 10 had reduced CHEP amplitude; and 9 had prolonged CHEP latencies. The mean intensity of pain perception on the verbal rating scale was 4.28 ± 1.63, in the range of mild pain. A representative patient with abnormal CHEP is illustrated in Fig. 1A and C. In this 60-year-old female patient with diabetic painful neuropathy and an IENF density of 0.9 fibers/mm, the CHEP latency was mildly prolonged (507 ms) and the CHEP amplitude was reduced (19.3 μV) when compared with the typical N- and P-waves, which could be elicited in an age- and sex-matched healthy subject with an IENF density of 7.9 fibers/mm (Fig. 1B and D).
Figure 1.
CHEP and skin innervation in type 2 diabetic neuropathy. Skin biopsies were stained with anti-protein gene product 9.5 (PGP 9.5) antiserum, and IENF densities were quantified. Skin innervation and CHEP in a representative patient with type 2 diabetic neuropathy (A and C) compared with an age- and sex-matched subject (B and D) are illustrated. A: Skin biopsy from a 60-year-old female patient shows marked depletion of cutaneous nerve terminals in the epidermis (epi) with an IENF density of 0.9 fibers/mm. Only loose and fragmented subepidermal nerve bundles (sn) are recognizable in the dermis (derm). B: Skin biopsy from a 58-year-old healthy woman shows varicose PGP 9.5(+) IENFs (arrows) in the epidermis with an IENF density of 7.9 fibers/mm. C and D: Averaged tracing of the CHEP (C) from the patient in A shows attenuation of N- and P-waves and relatively prolonged N-wave latency comparing with the well-defined complex of N- and P-waves (D) from the control subject in B. (For A and B, bar = 25 μm; for C and D, time base = 250 ms and sensitivity = 50 μV.)
Pathologic and functional correlates of CHEP in diabetic neuropathy
To explore the factors associated with CHEP parameters in type 2 diabetic neuropathy, we analyzed the effects of age, sex, diabetes duration (see the results section in the online appendix), IENF density, and thermal thresholds. On simple linear regression analyses, the CHEP amplitude was linearly correlated with the IENF density (P < 0.001, supplementary Fig. A1) and cold threshold at foot dorsum (P = 0.049). We then analyzed these relationships with a multiple linear regression model. The IENF density was the only independent variable that was still linearly correlated with the CHEP amplitude (P = 0.003) (Table 1).
Table 1.
Correlation among CHEP, IENF density, and thermal thresholds on multiple linear regression models
| CHEP amplitude | IENF density | Verbal rating scale (CHEP amplitude) | Verbal rating scale (IENF density) | |
|---|---|---|---|---|
| Model (R2, P) | 0.49, 0.006* | 0.51, 0.004* | 0.44, 0.017* | 0.39, 0.04* |
| Independent variable (β, P) | ||||
| Age | −0.219, 0.337 | −0.007, 0.751 | 0.022, 0.383 | 0.015, 0.553 |
| Sex | −0.033, 0.995 | −0.343, 0.495 | 0.077, 0.897 | 0.141, 0.823 |
| Duration of diabetes | −0.174, 0.647 | −0.028, 0.421 | −0.044, 0.291 | −0.045, 0.303 |
| IENF density | 6.045, 0.003* | — | — | 0.409, 0.062 |
| CHEP amplitude | — | 0.05, 0.003* | 0.046, 0.019* | — |
| Warm threshold | 0.308, 0.652 | −0.061, 0.322 | −0.05, 0.498 | −0.027, 0.727 |
| Cold threshold | 0.325, 0.286 | −0.00,002, 0.999 | 0.03, 0.373 | 0.042, 0.227 |
β, standardized coefficient with P for each independent variable; CHEP amplitude, N-P amplitude of CHEP; R2, covariance of the given multiple linear regression model with P for the model.
*Statistically significant.
To further investigate the relationship between CHEP amplitude and IENF density and to determine the most important parameters related to skin denervation, we performed simple and multiple linear regression analyses. In the simple linear regression model, the IENF density was correlated with the CHEP amplitude (P < 0.001) and warm thresholds (P = 0.015). On analysis with a multiple linear regression model, only the CHEP amplitude was still correlated with the IENF density (Table 1). Taken together, CHEP amplitude was the most significant neurophysiological correlate of the skin denervation in type 2 diabetic neuropathy.
We then analyzed the association between pain perception to contact heat stimuli and parameters of various examinations. The intensity of pain perception measured by verbal rating scale was correlated with the CHEP amplitude (P = 0.001), IENF density (P = 0.004), warm threshold (P = 0.047), and cold threshold (P = 0.008) in simple linear regression. These relationships were refined with multiple linear regression models, and only the CHEP amplitude was significantly correlated with pain perception (standardized coefficient 0.046, P = 0.019; R2 = 0.44 and P = 0.017 for the model).
Relationship of the neuropathic pain with CHEP and IENF density
To explore whether CHEP reflected the neuropathic pain in diabetes, we analyzed the excitability indexes by calculating the ratio of CHEP amplitude to IENF density. The excitability index was significantly higher in the diabetic neuropathic group than the age- and sex-matched control group (44.03 ± 97.31 vs. 3.95 ± 1.02; P = 0.023), indicating relatively higher CHEP amplitudes compared with the corresponding IENF densities in diabetic painful neuropathy.
We further examined the relationships between the CHEP amplitude and different neuropathic pain symptoms by analyzing the CHEP amplitude and IENF density between patients with or without a defined symptom (Table 2). Among all symptoms, the CHEP amplitude was higher in patients with evoked pain than in individuals without evoked pain (24.9 ± 14.8 vs. 10.2 ± 14 μV, P = 0.011); the degree of skin innervation between these two subgroups, however, was similar, with IENF densities of 1.1 ± 1.1 versus 1.1 ± 1.6 fibers/mm (P = 0.989). This finding indicated enhanced brain activations relative to the corresponding IENF density in patients with evoked pain.
Table 2.
CHEP amplitude and IENF density according to neuropathic pain symptoms
| n | CHEP amplitude | P | IENF density | P | |
|---|---|---|---|---|---|
| Evoked pain | |||||
| Yes | 10 | 24.9 ± 14.8 | 0.011* | 1.1 ± 1.1 | 0.989 |
| No | 22 | 10.2 ± 14 | 1.1 ± 1.6 | ||
| Tingling or shooting | |||||
| Yes | 25 | 15.4 ± 15.6 | 0.67 | 1.1 ± 1.6 | 0.74 |
| No | 7 | 12.5 ± 16.8 | 0.9 ± 1.0 | ||
| Lacerating† | |||||
| Yes | 2 | 9 ± 12.7 | 0.687 | 2.1 ± 2.9 | 0.687 |
| No | 30 | 15.2 ± 15.9 | 1.0 ± 1.4 | ||
| Hot or burning | |||||
| Yes | 13 | 17.1 ± 18.2 | 0.51 | 1.5 ± 1.8 | 0.139 |
| No | 19 | 13.3 ± 13.9 | 0.7 ± 1.2 | ||
| Cold or freezing† | |||||
| Yes | 4 | 14.9 ± 4.3 | 0.68 | 0.5 ± 0.7 | 0.836 |
| No | 28 | 14.8 ± 16.6 | 1.1 ± 1.5 | ||
| Electric shock | |||||
| Yes | 14 | 18.5 ± 15.9 | 0.242 | 1.5 ± 1.8 | 0.147 |
| No | 18 | 11.9 ± 15.1 | 0.7 ± 1.1 | ||
| Numbness | |||||
| Yes | 25 | 14 ± 13.9 | 0.608 | 0.9 ± 1.3 | 0.255 |
| No | 7 | 17.5 ± 21.8 | 1.6 ± 2 |
Data are means ± SD unless otherwise indicated. P, P value for the t test or nonparametric test.
*Statistically significant.
†Nonparametric test (Wilcoxon rank sum test).
CONCLUSIONS
This study demonstrates the clinical significance of the CHEP in type 2 diabetic neuropathy. Important findings include the following: 1) abnormal CHEP patterns (reduction of CHEP amplitudes or prolongation of CHEP latencies) were noted in most patients (81.3%) of diabetic painful neuropathy with skin denervation, and these findings could be neurophysiological characteristics in diagnosing small-fiber sensory neuropathy; 2) the CHEP amplitude was the most significant parameter correlated with the IENF density and the pain perception to contact heat stimuli and could represent the physiological consequences of thermonociceptive nerve degeneration; and 3) patients with diabetic painful neuropathy had much higher CHEP amplitude relative to their corresponding IENF densities, especially the patients with evoked pain despite a similar degree of skin denervation. These observations suggest that the CHEP amplitude provides a noninvasive test for assessing the degeneration of Aδ thermonociceptive fibers and reflects the physiology of pain in type 2 diabetic neuropathy.
This study is the first to demonstrate the feasibility of CHEP as a clinical examination for diabetic neuropathy. A negative-positive waveform of CHEP mediated by Aδ fibers can be recorded in normal subjects by suprathreshold and fixed-intensity thermal stimuli (10,15). Because CHEPs record the brain activities to heat pain stimuli conveyed by thermonociceptive nerves, they could detect the dysfunctions due to small-diameter sensory nerve degeneration. In patients with skin denervation, the CHEP amplitudes were reduced and the latencies became prolonged (12,16). The present study explores the clinical applications of CHEP for the diagnosis of small-fiber thermonociceptive nerve involvement in diabetic neuropathy. In our diabetic patients with neuropathic pain and skin denervation, 81.3% of patients had reduced CHEP amplitudes or prolonged CHEP latencies. These findings demonstrate that CHEP can detect physiological consequences of thermonociceptive nerve degeneration and provide an objective, sensitive, and noninvasive assessment for thermonociceptive nerves in diabetes.
In the present study, the CHEP amplitude, IENF density, and thermal thresholds were associated with one another, and the only and most significant correlation existed between the CHEP amplitude and IENF density on multiple regression models. The generation of CHEP begins at the cutaneous nociceptors, and the signal is transmitted through Aδ afferents to the central nerve system. Aδ fibers lose their myelin sheath before entering the epidermis and become indistinguishable from C-fiber terminals (17), and the IENF density represents the pathology of these small-diameter sensory nerves terminating in the skin. Diabetic neuropathy is associated with axonal degeneration of C and Aδ fibers and skin denervation (9,18). Therefore, reduced IENF density might reflect pathological changes in Aδ afferents of peripheral nerves and result in decreased input of contact heat stimuli. In this study, CHEP has the highest correlation with the IENF density compared with other parameters of sensory nerve functions such as thermal thresholds in quantitative sensory testing. This finding suggests that the CHEP amplitude may serve as an alternative examination of thermonociceptive nerves for diabetic patients in whom the skin biopsy is contraindicated.
Neuropathic pain is common in diabetic neuropathy (1), but the relationship between skin denervation and neuropathic pain is not consistent (19). The observation of higher CHEP amplitude relative to the corresponding IENF density in patients with diabetic painful neuropathy provides new insights about mechanisms of neuropathic pain. Previous and the present studies documented the positive correlation between the CHEP amplitude and IENF density in small-fiber neuropathy (16). Pain- or laser-evoked potential also showed delayed and reduced late responses in HIV-associated neuropathy (20) and postherpetic neuralgia (21). All these studies showing attenuated or delayed responses of pain-related potentials indicated deafferentation of peripheral Aδ fiber nerves (22). CHEPs represent the brain activities that are affected not only by peripheral deafferentation but also by the changes in central processing through the spinal cord and brain. In this study, we designed an excitability index to assess the significance of CHEP amplitude in relation to the corresponding IENF density. Patients with diabetic painful neuropathy and skin denervation had higher excitability indexes than control subjects. Furthermore, the analysis of subgroups with different features of neuropathic pain demonstrated higher CHEP amplitudes in the subgroup with evoked pain than the group without this symptom, despite a similar degree of cutaneous nerve degeneration. These findings indicate that patients with diabetic painful neuropathy had relatively enhanced brain activities of CHEP, even with corresponding reduction of IENF densities, and suggest that the CHEP amplitude could serve as a physiological hallmark of evoked pain in diabetic painful neuropathy. The possible mechanisms underlying such changes in CHEP include both peripheral sensitization at the level of the peripheral nerve and dorsal root ganglia and central sensitization at the spinal and supraspinal levels during the progression of diabetic neuropathy. For example, upregulation and enhanced activities of voltage-gated sodium channels, or transient receptor potential vanilloid 1 receptor, increased noradrenergic sensitivity of human nociceptors and plasticity in the spinal cord involving GABA receptors, NMDA receptors, or nitric oxide synthase–nitric oxide cascade. Additional supraspinal influences also contribute to the development and maintenance of thermal hyperalgesia (23,24). The present study demonstrates the opportunity of applying CHEP as a tool to follow the progression of neuropathy and to investigate whether such changes parallel the progression of symptoms and disability. This study specifically focused on diabetic painful neuropathy. The extension of this approach to nonpainful neuropathy will provide further insights on the relations between CHEP and clinical symptoms.
In conclusion, CHEP provides a noninvasive and sensitive approach to assess the involvement of thermonociceptive nerves in diabetic patients and also provides physiological evidence of evoked pain.
Supplementary Material
Acknowledgments
The work was supported by the National Science Council, Taiwan (NSC97-2320-B-002-042-MY3, NCS98-2314-B002-102-MY3, NSC98-2321-B-002-035).
No potential conflicts of interest relevant to this article were reported.
C.-C.C. researched data, contributed to discussion, and wrote the manuscript. M.-T.T. researched data and contributed to discussion. Y.-J.L. researched data and contributed to discussion. W.-S.Y. researched data and reviewed/edited the manuscript. S.-C.H. contributed to discussion and reviewed/edited the manuscript. M.-J.C. reviewed/edited the manuscript. Y.-H.L. researched the data. Y.-C.C. reviewed/edited the manuscript. S.-T.H. researched data, contributed to discussion, and wrote and reviewed/edited the manuscript.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Davies M, Brophy S, Williams R, Taylor A: The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care 2006;29:1518–1522 [DOI] [PubMed] [Google Scholar]
- 2.Zaslansky R, Yarnitsky D: Clinical applications of quantitative sensory testing (QST). J Neurol Sci 1998;153:215–238 [DOI] [PubMed] [Google Scholar]
- 3.Dyck PJ, Zimmerman IR, Johnson DM, Gillen D, Hokanson JL, Karnes JL, Gruener G, O'Brien PC: A standard test of heat-pain responses using CASE IV. J Neurol Sci 1996;136:54–63 [DOI] [PubMed] [Google Scholar]
- 4.McCarthy BG, Hsieh ST, Stocks A, Hauer P, Macko C, Cornblath DR, Griffin JW, McArthur JC: Cutaneous innervation in sensory neuropathies: evaluation by skin biopsy. Neurology 1995;45:1848–1855 [DOI] [PubMed] [Google Scholar]
- 5.McArthur JC, Stocks EA, Hauer P, Cornblath DR, Griffin JW: Epidermal nerve fiber density: normative reference range and diagnostic efficiency. Arch Neurol 1998;55:1513–1520 [DOI] [PubMed] [Google Scholar]
- 6.Boucek P, Havrdova T, Voska L, Lodererova A, He L, Saudek F, Lipar K, Adamec M, Sommer C: Epidermal innervation in type 1 diabetic patients: a 2.5-year prospective study after simultaneous pancreas/kidney transplantation. Diabetes Care 2008;31:1611–1612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dyck PJ, O'Brien PC: Quantitative sensation testing in small-diameter sensory fiber neuropathy. Muscle Nerve 2002;26:595–596 [DOI] [PubMed] [Google Scholar]
- 8.Devigili G, Tugnoli V, Penza P, Camozzi F, Lombardi R, Melli G, Broglio L, Granieri E, Lauria G: The diagnostic criteria for small fibre neuropathy: from symptoms to neuropathology. Brain 2008;131:1912–1925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shun CT, Chang YC, Wu HP, Hsieh SC, Lin WM, Lin YH, Tai TY, Hsieh ST: Skin denervation in type 2 diabetes: correlations with diabetic duration and functional impairments. Brain 2004;127:1593–1605 [DOI] [PubMed] [Google Scholar]
- 10.Granovsky Y, Matre D, Sokolik A, Lorenz J, Casey KL: Thermoreceptive innervation of human glabrous and hairy skin: a contact heat evoked potential analysis. Pain 2005;115:238–247 [DOI] [PubMed] [Google Scholar]
- 11.Chen AC, Niddam DM, Arendt-Nielsen L: Contact heat evoked potentials as a valid means to study nociceptive pathways in human subjects. Neurosci Lett 2001;316:79–82 [DOI] [PubMed] [Google Scholar]
- 12.Truini A, Galeotti F, Pennisi E, Casa F, Biasiotta A, Cruccu G: Trigeminal small-fibre function assessed with contact heat evoked potentials in humans. Pain 2007;132:102–107 [DOI] [PubMed] [Google Scholar]
- 13.Granovsky Y, Granot M, Nir RR, Yarnitsky D: Objective correlate of subjective pain perception by contact heat-evoked potentials. J Pain 2008;9:53–63 [DOI] [PubMed] [Google Scholar]
- 14.Pan CL, Tseng TJ, Lin YH, Chiang MC, Lin WM, Hsieh ST: Cutaneous innervation in Guillain-Barre syndrome: pathology and clinical correlations. Brain 2003;126:386–397 [DOI] [PubMed] [Google Scholar]
- 15.Chao CC, Hsieh ST, Chiu MJ, Tseng MT, Chang YC: Effects of aging on contact heat-evoked potentials: the physiological assessment of thermal perception. Muscle Nerve 2007;36:30–38 [DOI] [PubMed] [Google Scholar]
- 16.Atherton DD, Facer P, Roberts KM, Misra VP, Chizh BA, Bountra C, Anand P: Use of the novel contact heat evoked potential stimulator (CHEPS) for the assessment of small fibre neuropathy: correlations with skin flare responses and intra-epidermal nerve fibre counts. BMC Neurol 2007;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Provitera V, Nolano M, Pagano A, Caporaso G, Stancanelli A, Santoro L: Myelinated nerve endings in human skin. Muscle Nerve 2007;35:767–775 [DOI] [PubMed] [Google Scholar]
- 18.Llewelyn JG, Gilbey SG, Thomas PK, King RH, Muddle JR, Watkins PJ: Sural nerve morphometry in diabetic autonomic and painful sensory neuropathy: a clinicopathological study Brain 1991;114:867–892 [DOI] [PubMed] [Google Scholar]
- 19.Sorensen L, Molyneaux L, Yue DK: The relationship among pain, sensory loss, and small nerve fibers in diabetes. Diabetes Care 2006;29:883–887 [DOI] [PubMed] [Google Scholar]
- 20.Obermann M, Katsarava Z, Esser S, Sommer C, He L, Selter L, Yoon MS, Kaube H, Diener HC, Maschke M: Correlation of epidermal nerve fiber density with pain-related evoked potentials in HIV neuropathy. Pain 2008;138:79–86 [DOI] [PubMed] [Google Scholar]
- 21.Truini A, Haanpaa M, Zucchi R, Galeotti F, Iannetti GD, Romaniello A, Cruccu G: Laser-evoked potentials in post-herpetic neuralgia. Clin Neurophysiol 2003;114:702–709 [DOI] [PubMed] [Google Scholar]
- 22.Kakigi R, Shibasaki H, Tanaka K, Ikeda T, Oda K, Endo C, Ikeda A, Neshige R, Kuroda Y, Miyata K: CO2 laser-induced pain-related somatosensory evoked potentials in peripheral neuropathies: correlation between electrophysiological and histopathological findings. Muscle Nerve 1991;14:441–450 [DOI] [PubMed] [Google Scholar]
- 23.Zhuo M: Neuronal mechanism for neuropathic pain. Mol Pain 2007;3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell JN, Meyer RA: Mechanisms of neuropathic pain. Neuron 2006;52:77–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.