Abstract
The elderly utilize emergency medical services (EMS) at a higher rate than younger patients, yet little is known about the influence of injury on subsequent EMS utilization and costs.
Objective
To assess injury hospitalization as a potential marker for subsequent EMS utilization and costs by Medicare patients.
Methods
This observational study analyzed a retrospective cohort of all Medicare patients (≥67 years) with an ICD-9 injury diagnosis admitted to 125 Oregon and Washington hospitals during 2001-2002 who survived to hospital discharge. The number of EMS transports and total EMS costs were compared one year before and for one year following the index hospitalization.
Results
There were 30,655 injured elders in our cohort. Their mean ICD-9 based injury severity score was 0.97, with 4.1% meeting a definition of severe injury and 37% having hip fractures. The mean (range) number of EMS transports before and after the injury was 0.5 (0-45) and 0.9 (0-56), for an unadjusted incidence rate ratio (IRR) of 1.7 (95% CI 1.7-1.8). The increase in EMS utilization following an injury hospitalization was even greater after adjusting for risk period and other model predictors (IRR 2.4, 95% CI 2.3-2.5). Annual EMS costs rose 74% following the injury hospitalization from $211 to $367 mean dollars per person. The greatest increase was in non-emergent EMS use, accounting for 67% of the increase in the number of uses. Institutionalization in a skilled nursing or rehabilitation facility either before or after injury was strongly associated with the need for EMS care.
Conclusion
An injury hospitalization in the elderly serves as a sentinel marker for an abrupt increase in EMS utilization and costs, even after accounting for confounders. This supports systems planning, research and programs to prevent injuries in elders and alternative, cost-effective modes of transport to accommodate this need.
Keywords: Emergency medical services, geriatrics, elderly, aged, injuries
Introduction
Background
The elderly utilize out-of-hospital emergency medical services (EMS) at a rate far higher than the young.1,2,3,4,5 Prior studies have unanimously found a strong correlation between age and EMS utilization rates. As elders already account for 38% of EMS volume, those over 65 will likely become even more important consumers of EMS as the population ages.6 Injury hospitalization may be a sentinel event for a significant change in the need for EMS, which may increase, decrease, or remain stable. Understanding the patterns of utilization will better enable us to meet the out-of-hospital care needs of the elderly.
Prior studies have shown the importance of injury on the health of the elderly, causing significant morbidity, mortality, and expense.7,8,9,10 However, there is little epidemiologic literature on the role of geriatric injury in EMS utilization. Spaite's 1986 study of injured elders evaluated by Tucson paramedics is one of few studies of the relationship between elder injury and EMS.3 This study described mechanisms and injury patterns in the out-of-hospital phase; however, no studies describe the costs or patterns of EMS use by injured elders. Better understanding the patterns of EMS use by injured elders could prioritize injury prevention, target prevention efforts and inform cost-controlling alternatives. Such prevention strategies could include home safety evaluations, physical therapy, and when necessary, institutionalization of at-risk elders. Other cost-control strategies include identifying high risk individuals or time periods after injury in which unnecessary use could be reduced.
Our specific aim in this study was to quantify the effect of geriatric injury hospitalization on EMS (ambulance) utilization and costs. We compared the number of EMS uses and the costs of those services in the years before and after an injury hospitalization to determine whether such an injury event is a marker of increased EMS utilization and to elucidate the factors associated with utilization. We also sought to identify whether there were high risk time periods or individuals who consumed a disproportionate share of EMS after injury.
Methods
Study Design and Population
This was an observational analysis of a retrospective cohort of all Medicare patients ages 67 years or older admitted to an Oregon or Washington hospital with any injury diagnosis in 2001 or 2002 who survived to hospital discharge.
Medicare patients (≥ 67 years) admitted to 125 Oregon and Washington hospitals from January 1, 2001 through December 31, 2002 were identified by ICD-9 diagnosis injury codes 800-959. We excluded patients who died prior to admission, during their index hospitalization, or within one day of discharge, since these patients would have no post-discharge EMS utilization. Those with ICD-9 codes 905-909 (late effects of injury), 930-939 (foreign bodies), and 958 (complications of injury) were excluded from being considered as markers of our index injury event but not from the counts of EMS use before and after the identified index injury.
All patients had at least one full year of data prior to the index injury hospitalization to determine baseline use of EMS, skilled nursing facility use, and comorbidity burden. Patients were then tracked for 1-year following the date of discharge from the index admission.
Data Collection
Data for each patient's index hospitalization were obtained from the Center for Medicare and Medicaid Services Medicare Provider Analysis and Review (MEDPAR) file. Services from independent EMS providers were identified in the carrier standard analytic file by a Berenson-Eggers Type of Service (BETOS) code or an EMS related Healthcare Common Procedure Coding System (HCPCS) code, including aeromedical transport. Hospital-owned ambulance bills were identified in the outpatient standard analytic file by HCPCS codes. The MEDPAR file was also analyzed for EMS rendered during an acute care hospitalization or stay in a SNF.11 The costs of ambulance services were summed from the Medicare covered charges in each of the three databases and were not included with costs from the index hospitalization. We classified EMS uses as emergent or non-emergent based on HCPCS codes, assuming that all aeromedical transport, specialty care transport and advanced life support level-2 services were emergent.12
In defining EMS utilization, we sought to exclude transport services that brought the patient to their index hospitalization or transported them home after discharge. Therefore, we excluded any EMS transport that occurred within one day prior to or following the index hospitalization. We used this cutoff because patients transported in the evening might not be admitted until the following calendar day due to a long emergency department stay or transfer from one emergency department to admission at another facility.
Mortality was taken from the Medicare denominator standard analytic file, which accurately reports the date of death, as it is based on daily reports from the Social Security Administration.
The study was approved with a HIPAA Waiver of Consent by the Oregon Health & Science University (OHSU) Institutional Review Board and the Centers for Medicare and Medicaid Services Privacy Board.
Methods of Measurement
The MEDPARS dataset contained up to 9 diagnosis fields from the index hospitalization which were used to calculate an ICD-9 based injury severity score (ICISS) for each patient.13 This method calculates the likelihood of survival as the product of the probabilities of surviving each of the individual injuries sustained by the patient. We derived these probabilities from the 2002 National Inpatient Sample. An ICISS of 0.9 or less was considered a “serious injury,” a definition used in previous trauma studies.14 While 30% of patients had all nine available diagnosis codes filled and thus might have other injuries which were unreported, previous work has shown that considering more than the one to three most severe injuries is unnecessary for predicting outcomes.15 Using ICD-9 codes, injuries were also categorized as femoral neck (hip) fractures, other extremity injuries, spinal injuries, head injuries, and chest injuries using the method described by Clark.16 Hip fractures were defined by an ICD-9 code of 820. Other extremity injures were defined by ICD-9 codes of 808 (pelvic fractures), 810–819 (upper extremity fractures), 821–829 (other lower extremity fractures), 831–838 (dislocations), 840–845 (sprains and strains), 880–897 (wounds), 912–917 (superficial injuries), 923–924 (contusions), or 927–928 (crush injuries). Spinal injuries were defined by ICD-9 codes 805–806 or 952. Head injuries were defined by ICD-9 codes 800–804 or 850–854. Chest injuries were defined by ICD-9 codes 807, 860–862, 875, or 901. A dichotomous measure of major operative intervention not including orthopedic surgery was also constructed from ICD-9 procedures codes in the MEDPAR file and included any of the following operative procedures: brain, spine, neck, chest, abdominal, or vascular.17,18
Data for medical co-morbidities were obtained from ICD-9 codes included in the Medicare Standard Analytical File for outpatient and emergency department visits, plus inpatient records (MEDPAR file) for one year prior to the injury. Deyo's adaptation of the Charlson comorbidity index was used to convert ICD-9 codes to a weighted comorbidity score.19 This validated system uses weighted scores for 17 diagnoses as well as age to produce a prognostic index for survival.
Skilled nursing facility (SNF) or rehabilitation facility residence prior to injury was defined as present if a SNF bill was recorded in the MEDPAR file within 90 days preceding the index hospitalization. This definition has been used in previous injury studies using Medicare data.20 The total numbers of days spent in acute care hospitals before and after injury were calculated by summing the cumulative lengths of stay in the MEDPAR file. As disposition codes were inconsistently reported, the presence of a SNF bill in the 90 days after discharge was used as a surrogate for discharge to skilled nursing or rehabilitation care.
Outcomes Measures
Our primary outcomes were the counts and costs of EMS in the one year before and after the injury. The count of EMS uses in the years before and after the index injury hospitalization was defined as the number of EMS-related bills in the carrier, MEDPARS, and outpatient datasets. The cost of EMS was the sum of the Medicare covered charges for EMS appearing on those bills.
Analytical Methods
The count of EMS uses and their summed costs were first compared without adjustment in the years before and after injury hospitalization with 95% confidence intervals for the incidence rate ratio generated by a negative binomial regression model.
A negative binomial regression model was then used to adjust for reduced periods of risk for EMS use in the years before and after the injury hospitalization. Time periods where a patient was hospitalized (before or after the index injury hospitalization), as well as time after death for those who died within a year of injury were considered periods at which the patient was not at-risk of requiring EMS and were adjusted for. We also included several confounders of a-priori importance to the model. Patient factors that we expected to be predictive of EMS utilization included sex, age, Charlson co-morbidity score, and SNF residence before and after injury. Goodness of model fit was performed by graphically comparing observed versus predicted probabilities for counts of EMS uses. The “countfit” command in Stata was used to test the differences between observed and predicted probabilities.21
To model costs, we used a two-part model, a standard approach from the field of health economics.22 Part one was a logistic regression model where the dependent variable took on values of one for positive expenditures and zero for no EMS use. Part two of the model used the Extended Estimating Equations (EEE) method, a flexible extension of Generalized Linear Models that is useful for modeling the right-skewed distributions that are common in health care expenditures.23,24 Confidence intervals for cost estimates were generated using bootstrapping techniques at 500 iterations. Data management was performed using SAS v.9.1 (SAS Institute, Cary, NC). Statistical analysis was done with STATA 11 (STATACorp, College Station, Texas).
Results
There were 30,655 injured elders admitted to 125 hospitals in Oregon and Washington over the two-year period who survived more than a day after hospital discharge. Characteristics of the patient population and details of their injury hospitalization are described in Table 1. During the year prior to injury, the cohort utilized EMS 16,029 times, for a mean, unadjusted rate of 0.52 rides per person-year (table 2). In the year after discharge from their injury hospitalization, utilization increased 73% to 27,781 uses, a mean of 0.91 rides per person-year. The distribution of EMS utilization among cohort members is shown in Figure 1. After the index hospitalization, 19,386 patients (63%) used no EMS (figure 2). Only 144 patients used greater than 10 EMS rides in the year after injury, accounting for 8% of the total EMS use.
Table 1.
Characteristics of hospitalized injured Medicare patients who survived to hospital discharge in Oregon and Washington
| Total Sample | 30,655 | |
| Sex | ||
| Female | 21,010 | (68.5%) |
| Male | 9,645 | (31.5%) |
| Age at time of injury. Median (IQR) | 82 | (77-88) |
| Age ranges: | ||
| 67-69 | 1,760 | (5.7%) |
| 70-79 | 9,505 | (31.0%) |
| 80-89 | 13,868 | (45.2%) |
| 90-99 | 5,351 | (17.5%) |
| 100-104 | 164 | (0.5%) |
| 105-108 | 7 | (0.0%) |
| White race | 29,558 | (96.4%) |
| Charlson co-morbidity index. Median (IQR) | 1 | (0-2) |
| 0 | 14,554 | (47.5%) |
| 1-2 | 12,013 | (39.2%) |
| ≥3 | 4,088 | (13.3%) |
| SNF resident prior to injury* | 1,323 | (4.3%) |
| SNF resident after discharge** | 3,111 | (10.1%) |
| Details of index injury hospitalization | ||
| Length of stay, days Median (IQR) | 4 | (3-6) |
| Inter-hospital transfer after admission | 840 | (2.7%) |
| ICD-9 based Injury Severity Score (ICISS) Median (IQR) |
0.97 | (0.96-0.98) |
| Serious injury: ICISS ≤0.9 | 1,246 | (4.1%) |
| Major surgery including orthopedic surgery | 17,331 | (56.5%) |
| Major non-orthopedic surgery | 1,334 | (4.4%) |
| Blood transfusion | 4,507 | (14.7%) |
| Diagnoses | ||
| Hip fracture | 11,244 | (36.7%) |
| Other extremity injury | 12,358 | (40.3%) |
| Spine injury | 2,141 | (7.0%) |
| Head injury | 2,030 | (6.6%) |
| Chest injury | 1,791 | (5.8%) |
| One year mortality | 7,642 | (24.9%) |
Defined by the presence of a skilled nursing facility (SNF) or rehabilitation facility bill in the 90 days preceding admission.
Defined by the presence of a SNF or rehabilitation facility bill in the 90 days after discharge.
Table 2.
Rates of EMS utilization in the years before and after injury hospitalization (n=30,655)
| Before injury: Total uses, mean rides/person-yr (range, IQR) |
After injury: Total uses, mean rides/person-yr (range, IQR) |
Unadjusted incidence rate ratio (95% CI) |
Incidence rate ratio adjusted for risk period* (95% CI) |
Incidence rate ratio in full multivariable model** | |
|---|---|---|---|---|---|
| All EMS Uses | 16,029 0.52 (0 - 45, 0 - 1) |
27,781 0.91 (0 - 56, 0 - 1) |
1.7 (1.7 - 1.8) |
3.0 (2.9 - 3.1) |
2.4 (2.3 - 2.5) |
| Emergent EMS Uses† | 6,887 0.22 (0-24, 0-0) |
9,799 0.32 (0-21, 0-0) |
1.4 (1.4-1.5) |
2.0 (2.0 - 2.1) |
1.9 (1.8 - 2.0) |
| Non-Emergent EMS Uses† | 3,732 0.12 (0-24, 0-0) |
9,764 0.32 (0-52, 0-0) |
2.6 (2.5-2.8) |
4.6 (4.2 - 4.9) |
3.2 (3.0 – 3.5) |
Adjusted for time spent in an acute care hospital in the years before and after injury, and for death during the year after injury.
The model adjusted for risk period and included covariates of age, sex, Charlson co-morbidity score, and institutionalization status before and after injury.
31% of EMS uses could not be classified as emergent versus non-emergent and were not included in this part of the analysis.
Figure 1.
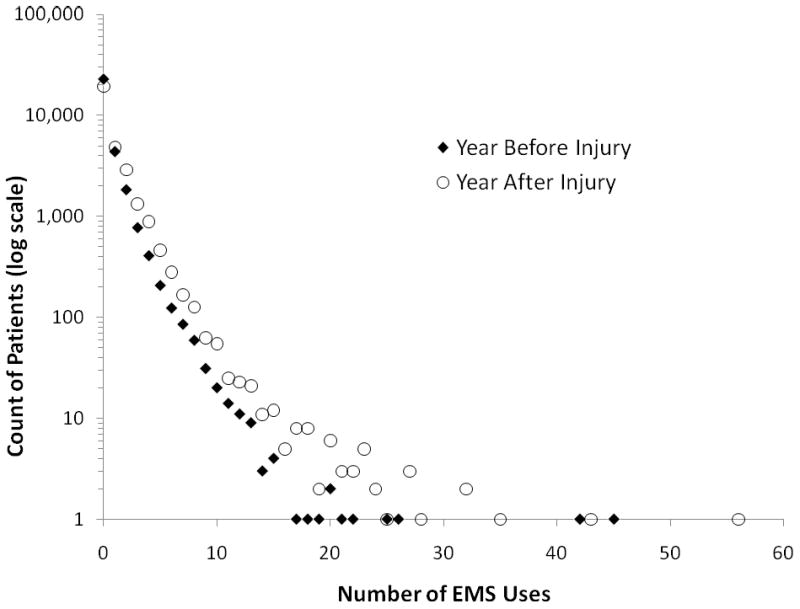
Unadjusted counts of EMS utilization in the years before and after injury hospitalization among elders (n=30,655).
Figure 2.
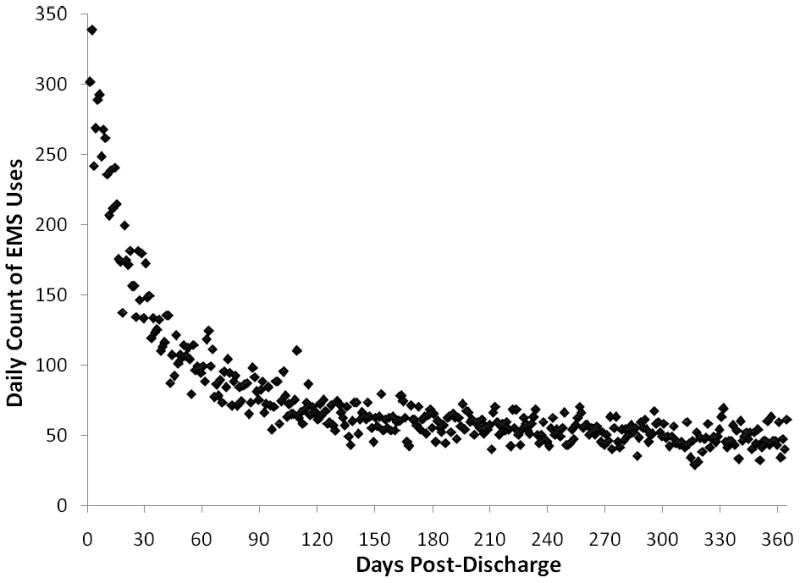
Timing of EMS utilization after discharge from injury hospitalization among elders (n=30,655).
Rides were able to be classified as emergent vs non-emergent in 69% of cases. The greatest increase was seen in non-emergent EMS use, increasing from 35% of classifiable EMS uses before injury to 50% after. Non-emergency use accounted for 67% of the increase in total EMS use after injury.
Adjusting for reduced exposure periods for EMS use in the years before and after hospitalization because of death or hospitalization, the incidence rate ratio (IRR) for EMS use after the injury admission was 3.0 (95% confidence interval [CI] 2.9 to 3.1, table 2). After adding baseline patient characteristics and skilled nursing facility residence before and after injury to the model, the IRR for EMS use after versus before injury admission was 2.4 (95% CI 2.3 to 2.5).
Figure 2 shows the timing of EMS use after injury. The early post-discharge period was a time of particularly high use, with 7.1% of the year's EMS use occurring in the seven days starting two days after discharge and 22.7% of the year's use occurring in the 30 days starting two days after discharge.
The unadjusted cost of EMS in the year before injury was $211 per cohort member (table 3). Costs increased 74% to $367 per person in the year after hospital discharge. These unadjusted results were similar to the full multivariate model, which estimated costs to be $212 before and $369 after injury, an increase of $157 dollars per person (95% CI $150 to $164). The total cost of ambulance services for our cohort in the year after injury was $11.3 million, an increase of $4.8 million from the year before injury.
Table 3.
Costs of EMS in the years before and after injury hospitalization
| Year before injury. Mean, (IQR) |
Year after injury. Mean, (IQR) |
Unadjusted ratio of EMS costs in years before and after injury | Model predicted costs in year before injury.* (95% CI) |
Model predicted costs in the year after injury.** (95% CI) |
Model predicted increase in costs after injury. (95% CI) |
|
|---|---|---|---|---|---|---|
| Cost of EMS | $211 (0 - 0) |
$367 (0 - 484) |
1.74 | $212 (206 - 218) |
$369 (359 - 379) |
$157 (150 - 164) |
Model included age, sex, Charlson co-morbidity score, and skilled nursing facility residence before and after injury.
Comparison of predicted and observed probabilities indicated that our negative binomial model fit the data well (appendix 1). There was no significant difference between observed and predicted counts (Pearson's chi-squared = 0.06, p<1).
Discussion
In this study, we found markedly elevated EMS utilization and costs by elders in the year following an injury hospitalization. These rates and costs were even more pronounced after accounting for relevant confounding factors and a restricted at-risk period of exposure.
These results are important because elders consume a large share of EMS resources and because of the important role of injury in their overall health and health care utilization. The high utilization rates in this population reflect both increased need for medical care (i.e., a high comorbidity burden and medical fragility), plus possibly the lack of other appropriate means for medical transportation. Injury is an important and often preventable reason for seeking care among the geriatric population. Prior studies have shown the importance of injury on the health of the elderly, causing significant morbidity, mortality, and expense. Medicare spending for injury care in 1999 cost $8 billion, almost 6% of total spending.25 Many of those who survive do so with permanent loss of function, with more than 50% of previously community-dwelling elderly hip fracture patients suffering walking disability one year after injury.26
Despite the importance of both EMS and injury in health care utilization by the elderly, few studies have looked directly at this interaction. Spaite reviewed injuries in those 70 years and older seen by the Tucson fire department in 1986.3 As in other studies, elders used EMS at a much higher rate (84 versus 42 calls per 1,000 person-years) than younger persons. Transport rates for elderly trauma patients were much higher than for younger patients (75% versus 49%). Our study expands on this work by following patients through their hospital course and for one-year post discharge to quantify their subsequent use of EMS.
Our finding of increased EMS utilization and costs after injury raises the question of whether the injury itself was the principal driver of increased utilization or merely a marker of generally declining health status. Our data suggest that injury is not simply a marker of ill health pre-injury, but is independently associated with increased EMS utilization rates and costs. We found that the Charlson medical co-morbidity score was actually a weak (although significant) predictor of EMS utilization in our multivariable model. We also demonstrated that injuries resulting in hospital admission among elders were not trivial: 56% required surgery, 37% had hip fractures, and 4% met an ICD-9 based definition of serious trauma with an ICISS of 0.9 or less. Our interpretation that injury itself significantly impacted the patient's subsequent health status is supported by Tinetti et al's 1997 study of the role of falls in predicting subsequent institutionalization in a cohort of community-dwelling elders.27 They found that elders who sustained significant injury in their falls had more than three times the adjusted relative risk of SNF placement than those who fell without injury. While the outcome used in the Tinetti study (SNF placement) was different from ours (EMS utilization), it supports our hypothesis that injuries in the elderly are a significant contributor to their health care utilization, and not merely a marker of general frailty.
We found that injury particularly resulted in an increased need for non-emergency out-of-hospital care, increasing from 35 to 50% of all EMS use and making up 67% of the increase in EMS use. This increase in non-emergent services did not explain the entire increase in EMS after injury, with emergent services being utilized after injury at a rate 1.4 times that pre-injury. This has important implications for system planners, who may be able to mitigate costs by improving access to less expensive non-emergent transport.
We were particularly interested in the relationship between institutionalization and EMS use. As institutionalization is a marker of ill health, one could hypothesize that nursing home residents would be high users of EMS. Alternatively, one could posit that as a SNF is already a step toward an acute care facility, usually with nurses, pharmacy services, and physicians, residents of this level of care might have a decreased need for EMS trips to acute care facilities. Our data suggested the former to be true. In our full regression model, those who lived in a SNF in the 90 days prior to injury utilized EMS at a rate 2.6 times that of their community dwelling counterparts. While our observation of high utilization among the institutionalized elders cannot prove causation, it would suggest that more widespread institutionalization of the elderly who are at-risk of requiring EMS would not be an effective means of curbing their utilization.
We also questioned whether most of the increased need for EMS could be explained by the transition of some patients from community living to institutionalization after injury, as most institutionalized elders will require medical transport for most needs. As injury often results in decreased independence or the need for rehabilitation care, we saw institutionalization increase from 4.3 before to 10.1% after injury. This did not remove the effect of injury itself on EMS use, as adding post-injury institutionalization to our model already containing pre-injury institutionalization decreased the incidence rate ratio for EMS use only slightly, from 3.1 to 2.4. Therefore, institutionalization after injury was a significant predictor of the need for EMS, but only explained a small part of this result.
Previous studies have shown that rates of repeat EMS use are high not only for injured elders. In a recent study by Shah et al., only 70% of EMS calls over a 16 month period for community dwelling elders were for unique individuals.28 Compared with other studies of EMS use by the elderly, our study found that our trauma patients had a higher rate of repeat EMS use within a year of their index visit (37%) than a sample of elders presenting to the emergency department by EMS for all causes studied by Weiss et al (23%).29 While this might suggest that injury results in a higher need for subsequent EMS care, Weiss et al's study included patients who were sent home from the emergency department and were therefore less sick than our cohort of admitted patients.
Our findings have practical applications by both policy-makers and system planners. Once an injury has occurred, the most effective targets should be identified for curbing subsequent costs. We found that the burden placed on the system by the “frequent flyers”, who we defined as those who used EMS more than ten times in the year after injury, was relatively modest, accounting for only 8% of all uses. Therefore, strategies to identify this high risk group would likely have only a small impact on the overall system burden. We were also interested in whether there was a high risk time period that would be a reasonable target for intervention. Our finding that greater than 22% of the subsequent year's services occurred in the first 30 days suggests that this early time period might be a fruitful interval for intervention. One method would be to pro-actively enroll all elders discharged from the hospital with injuries into alternative medical transportation programs for 30 days in order to decrease their use of 911 services for non-emergencies.
We observed a large difference in the incidence rate ratios for EMS use after injury depending on whether or not we adjusted for reduced risk period (3.0 vs 1.7). This large difference was due to the fact that while the average risk period after injury was only modestly shorter than that before injury, high utilization was concentrated in those who died soon after injury. Which estimate is applicable depends on the intended purpose and assumptions regarding the population of interest. If one is interested in examining the role of injury on EMS utilization on the individual, our risk-period adjusted estimate of a tripling in the need for EMS after injury would be appropriate. If one were an EMS manager or systems planner predicting the need for services after injury in a closed cohort of patients such as a community, our unadjusted estimate of a 70% increase is more relevant. Even this lesser estimate makes a strong argument for increased funding for injury prevention and cost-reduction strategies: in these two states, injury hospitalization was associated with an increase of $4.8 million per year in EMS spending alone. Other studies have shown it to be feasible EMS personnel to aid in injury prevention efforts by identifying factors contributing to injury and making social service referrals.30,31
Limitations
This cohort consisted of elders hospitalized with an injury diagnosis. Therefore, injured elders that did not survive to hospital discharge or who were discharged home from the emergency department or clinic were not included in the sample. Inclusion of these patients (particularly those from outpatient settings) may have changed our findings.
A limitation of quantifying out-of-hospital care services from billing data is that EMS calls that did not result in a transport were not captured. Therefore, our findings underestimated the actual burden on EMS systems. Spaite's study showed a 25% non-transport rate for geriatric injury calls. Another weakness of using Medicare data is the lack of information about the injury mechanism. While the dataset did contain ICD-9 mechanism of injury codes (e-codes), these were incompletely reported.
Comparing EMS utilization rates and costs in the years before and after injury raises the problem of unobserved confounders. Our regression models attempted to control for these patient level predictors, but the adjustment for confounding may have been incomplete. While we were able to use the Charlson co-morbidity score and prior nursing home residence as surrogates for general health status in the year preceding the injury admission, we could not measure the acute health events occurring immediately prior to the injury. Comparing our injured population to a similar cohort of patients admitted to the hospital for medical diagnoses would have been a further way of isolating the role of injury in subsequent EMS use; however, our dataset containing only injury patients prevented this additional analysis.
Our methods for assessing the important confounder of institutionalization versus community dwelling status was imperfect, as Medicare only pays for skilled nursing and rehabilitation facilities but not other types of care such as assisted living or adult foster homes. Also, emergent versus non-emergent EMS uses could only be classified in 69% of cases.
Using a regional dataset limits generalizability to other regions. Elders in the Pacific Northwest are racially homogenous and may not be comparable to elder populations in other regions of the US. Another limitation is the lack of data from the 19% of the Medicare entitled population covered by Medicare managed care organizations, a percentage that is even higher in the West.32 These patients may have different baseline characteristics than our fee-for-service Medicare population.
Conclusions
In summary, an injury hospitalization is a strong marker of increased EMS utilization and EMS-related costs in a cohort of Medicare patients. Injury in the elderly is not merely a marker of declining health status, but an independent predictor of subsequent out-of-hospital care needs and costs.
Supplementary Material
Acknowledgments
This publication was made possible with support from the Oregon Clinical and Translational Research Institute (OCTRI), grant number UL1 RR024140 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
Presentations: An abstract of this project was presented at the 2009 Society for Academic Emergency Medicine Annual Meeting in New Orleans, LA (May 2009).
References
- 1.Wofford JL, Moran WP, Heuser MD, Schwartz E, Velez R, Mittelmark MB. Emergency Medical Transport of the Elderly: A Population-Based Study. American Journal of Emergency Medicine. 1995;13(3):297–300. doi: 10.1016/0735-6757(95)90203-1. [DOI] [PubMed] [Google Scholar]
- 2.McConnel CE, Wilson RW. The Demand for Prehospital Emergency Services in an Aging Society. Social Science Medicine. 1998;46(8):1027–31. doi: 10.1016/s0277-9536(97)10029-6. [DOI] [PubMed] [Google Scholar]
- 3.Spaite DW, Criss EA, Valenzuela TD, Meislin HW, Ross J. Geriatric Injury: An Analysis of Prehospital Demographics, Mechanisms, and Patterns. Annals of Emergency Medicine. 1990;19(12):1418–1421. doi: 10.1016/s0196-0644(05)82611-3. [DOI] [PubMed] [Google Scholar]
- 4.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 Emergency Department Summary. [April 19, 2009]; Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr007.pdf. [PubMed]
- 5.Dickinson ET, Verdile VP, Kostyun CT, Salluzzo RF. Geriatric Use of Emergency Medical Services. Annals of Emergency Medicine. 1996 February;27(2):199–203. doi: 10.1016/s0196-0644(96)70323-2. [DOI] [PubMed] [Google Scholar]
- 6.Shah MN, Bazarian JJ, Lerner EB, et al. The Epidemiology of Emergency Medical Services Use by Older Adults: An Analysis of the National Hospital Ambulatory Medical Care Survey. Academic Emergency Medicine. 2007;14(5):441–448. doi: 10.1197/j.aem.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 7.Stevens JA, Hasbrouck LM, Durant TM, et al. Surveillance for injuries and violence among older adults. MMWR CDC Surveillance Summary. 1999;48:27–50. [PubMed] [Google Scholar]
- 8.Zuckerman JD. Hip fracture. New England Journal of Medicine. 1996;334(23):1519–25. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 9.Parker MJ, Anand JK. What is the True Mortality of Hip Fractures? Public Health. 1991;105(6):443–6. doi: 10.1016/s0033-3506(05)80614-6. [DOI] [PubMed] [Google Scholar]
- 10.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Survival Experience of Aged Hip Fracture Patients. American Journal of Public Health. 1989;79(3):274–8. doi: 10.2105/ajph.79.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Technical Brief, ResDAC Publication Number TN-002. Research Data Assistance Center, University of Minnesota; [April 1, 2009]. How to Find Ambulance Services in the Medicare Claims Data. Available at: http://www.resdac.umn.edu. [Google Scholar]
- 12.Baltimore(MD): Center for Medicare and Medicade Services; 2009. Mar 6, Medicare Claims Processing Manual. Chapter 15-Ambulance [Internet] cited 2009 April 15. Available from: http://www.cms.hhs.gov/Manuals/IOM/list.asp. [Google Scholar]
- 13.Osler T, Rutledge R, Deis J, Bedrick E. ICISS: An International Classification of Disease-9 Based Injury Severity Score. Journal of Trauma. 1996;41(3):380–8. doi: 10.1097/00005373-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Diggs BS, Mullins RJ, Hedges JR, Arthur M, Newgard CD. Proportion of Seriously Injured Patients Admitted to Hospitals in the US With a High Annual Injured Patient Volume: A Metric of Regionalized Trauma Care. Journal of the American College of Surgeons. 2008;206(2):212–219. doi: 10.1016/j.jamcollsurg.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 15.Kilgo PD, Osler TM, Meredithg W. The Worst Injury Predicts Mortality Outcome the Best: Rethinking the Role of Multiple Injuries in Trauma Outcome Scoring. J Trauma. 2003;55(4):599–607. doi: 10.1097/01.TA.0000085721.47738.BD. [DOI] [PubMed] [Google Scholar]
- 16.Clark DE, DeLorenzo MA, Lucas FL, Wennberg DE. Epidemiology and Short-Term Outcomes of Injured Medicare Patients. Journal of the American Geriatrics Society. 2004;53(12):2023–30. doi: 10.1111/j.1532-5415.2004.52560.x. [DOI] [PubMed] [Google Scholar]
- 17.Newgard CD, Hedges JR, Adams A, Mullins RJ. Secondary Triage: Early Identification Of High-Risk Trauma Patients Presenting to Non-Tertiary Hospitals. Prehospital Emergency Care. 2007;11(2):154–163. doi: 10.1080/10903120701205778. [DOI] [PubMed] [Google Scholar]
- 18.Newgard CD, Hedges JR, Diggs B, Mullins RJ. Establishing The Need For Trauma Center Care: Anatomic Injury Or Resource Use? Prehospital Emergency Care. 2008;12(4):451–458. doi: 10.1080/10903120802290737. [DOI] [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a Clinical Co-morbidity Index For Use With ICD-9-CM Administrative Databases. Journal of Clinical Epidemiology. 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen-Oghalai TU, Kuo YF, Zhang DD, Graham JE, Goodwin JS, Ottenbacher KJ. Discharge Setting for Patients with Hip Fracture: Trends from 2001 to 2005. Journal of the American Geriatrics Society. 2008;56(6):1063–8. doi: 10.1111/j.1532-5415.2008.01688.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Long JS, Freese J. Regression Models for Categorical Dependent Variables Using Stata. 2nd. College Station, Texas: Stata Press; 2006. [Google Scholar]
- 22.Duan N, Manning W, Morris C, Newhouse J. A Comparison of Alternative Models for the Demand for Medical Care. Journal of Business Economics and Statistics. 1983;1:115–26. [Google Scholar]
- 23.Basu A. Extended Generalized Linear Models: Simultaneous Estimation of Flexible Link and Variance Functions. The Stata Journal. 2005;5(4):501–16. [Google Scholar]
- 24.Basu A, Rathouz PJ. Estimating Marginal and Incremental Effects on Health Outcomes Using Flexible Link and Variance Function Models. Biostatistics. 2005;6(1):93–109. doi: 10.1093/biostatistics/kxh020. [DOI] [PubMed] [Google Scholar]
- 25.Bishop CE, Gilden D, Blom J, Kubisiak J, Hakim R, Lee A, Garnick DW. Medicare Spending for Injured Elders: Are There Opportunities for Savings? Health Affairs. 2002;21(6):215–223. doi: 10.1377/hlthaff.21.6.215. [DOI] [PubMed] [Google Scholar]
- 26.Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL, Wehren L. Changes in Functional Status Attributable to Hip Fracture: A Comparison of Hip Fracture Patients to Community-Dwelling Aged. American Journal of Epidemiology. 2003;157(11):1023–31. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 27.Tinetti ME, Williams CS. Falls, Injuries Due to Falls, and the Risk of Admission to a Nursing Home. New England Journal of Medicine. 1997;337(18):1297–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 28.Shah MN, Swanson P, Rajasekaran K, Dozier A. Repeat Emergency Medical Services Use by Older Adults in a Rurual Community: Impact on Research Methods and Study Length. Prehospital Emergency Care. 2009;13(2):173–178. doi: 10.1080/10903120802706211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weiss SH, Ernst AA, Miller P, Russell S. Repeat EMS Transports Among Elderly Emergency Department Patients. Prehospital Emergency Care. 2002;6(1):6–10. doi: 10.1080/10903120290938698. [DOI] [PubMed] [Google Scholar]
- 30.Weiss SJ, Chong R, Ong M, Ernst AA, Balash M. Emergency Medical Services Screening of Elderly Falls in the Home. Prehospital Emergency Care. 2003;7(1):79–84. doi: 10.1080/10903120390937148. [DOI] [PubMed] [Google Scholar]
- 31.Kue R, Ramstrom E, Weisberg S, Restuccia M. Evaluation of an Emergency Medical Services-Based Social Services Referral Program for Elderly Patients. Prehospital Emergency Care. 2009;13(3):273–279. doi: 10.1080/10903120802706179. [DOI] [PubMed] [Google Scholar]
- 32.Clark DE, DeLorenzo MA, Lucas FL, Wennberg DE. Injuries Among Older Americans With and Without Medicare. American Journal of Public Health. 2005;95(2):273–8. doi: 10.2105/AJPH.2003.036871. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


