This article seeks to share the recruitment statistics and experiences for the Assessment of Caregivers for Team Intervention via Videophone Encounters home-based telehealth intervention pilot study. Challenges such as initial inclusion criteria, monitoring and tracking of recruitment statistics, and strategies are presented. Recruitment continues to be an important barrier to home-based telehealth research, and the sharing of recruitment statistics, challenges, and strategies can be beneficial.
Key words: recruitment, hospice, palliative care, intervention research
Abstract
The difficulty in recruiting subjects for home-based telehealth research is well documented. This article shares the recruitment statistics and experiences in the Assessment of Caregivers for Team Intervention via Videophone Encounters pilot study, a home-based telehealth intervention. The study obtained 83% of the desired sample. Challenges included issues with initial inclusion criteria, weather-related problems, timely referrals and follow-up, the enrollment process, the need for multiple visits, and unforeseen cases of multiple caregivers. Detailed monitoring and tracking of recruitment statistics and immediate response to overcome challenges were critical to the eventual recruitment success. Strategies included the reallocation of resources to add a second research site, adjustments in inclusion criteria, process improvement with the hospice admissions process, and strategies to address staff gate-keeping. Recruitment continues to be an important barrier to home-based telehealth research and the sharing of recruitment statistics, challenges, and strategies can be beneficial. Gathering of recruitment data is a critical component of pilot studies, which assists in the development of successful randomized clinical trials for future home-based telehealth research.
Introduction
In 2008, 4,850 U.S. hospice agencies cared for more than 1.45 million terminally ill individuals and their families. Most services (74.1%) are delivered in patients' homes by an informal, unpaid caregiver, with a median hospice stay of 21 days.1 Home-based hospice care provides a unique opportunity to use telehealth technology to overcome the geographic distances between homes and hospice staff, especially in rural areas; yet the domain of hospice remains somewhat unexplored when it comes to the use of telehealth technologies.
The difficulties in recruiting subjects for home-based telehealth research are well documented.2,3 These challenges are increased with telehospice, when equipment must be installed in a home where attention is focused on caring for a dying person.4,5 Although there is much literature on challenges and experiences, only few studies have documented and reported statistics reflecting research recruitment experiences. The documentation of these details offers home-based telehealth researchers valuable information for planning studies and demonstrating the significant investment required in recruitment. The purpose of this article was to share the experiences in one home-based telehealth study. The following questions guide this article: (1) What were the recruitment challenges in this home-based telehealth study? (2) What strategies were helpful to recruitment? (3) What changes were made to facilitate meeting targets?
Methods
This article reports on the recruitment experiences of researchers conducting the Assessment of Caregivers for Team Intervention via Video Encounters pilot study, a home-based telehealth intervention funded by the National Cancer Institute.6 The details of the clinical pilot study results and intervention are outlined elsewhere.7–9 The goal of the pilot study was to measure the feasibility and effectiveness of a home-based telehealth intervention using commercially available plain old telephone-based videophone technology to bring informal caregivers of hospice patients into hospice interdisciplinary team meetings. Documentation was kept on all referrals including those not meeting the inclusion criteria. Data included the number of referrals contacted, the outcome of those contacts, the number of visits necessary to obtain final enrollment, and the reasons why individuals were not enrolled when a visit was made.
The setting for the study was a rural area in a midwestern state. The sample consisted of hospice caregivers recruited during the 2 years of the study. Based on an initial power analysis of outcome measures, the study had a total recruitment goal of 90 caregivers and 90 patients. The original inclusion criteria for patients and family members required: (1) enrollment as a home hospice caregiver/patient, (2) patient diagnosis of terminal cancer, (3) adult, (4) access to a standard phone line, (5) without functional hearing loss, (6) and cognitively able to consent. These criteria were later modified and will be discussed later.
The recruitment protocol directed that upon admission to the hospice, all patients meeting the inclusion criteria would be informed that the hospice was involved in a research study to improve patient/family services and would be asked to consent to a visit by a graduate research assistant (GRA) for further information. The admitting hospice nurse obtained written consent for referral and information on the family was given to a GRA. Once a referral was received, the GRA contacted the caregiver by phone and scheduled a visit.
Results
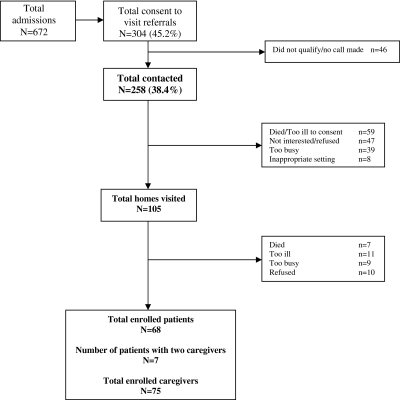
After 20 months of data collection, 2 months longer than planned, the project had enrolled 75 caregivers (83.3% of the goal). Nearly half (45.2%) of admitted individuals consented to be contacted by GRAs for further information about the study. Families that did not meet the inclusion criteria were omitted from consideration, leaving 258 families. This represented 38.4% of all hospice admissions and 84.9% of all families that provided consent to be contacted. GRAs contacted the 258 remaining families by phone and offered a visit to further explain the project. Of the 258 families, 105 (40.7%) agreed to an informational visit; 153 families refused to participate.
The most common reason (38.6%) for visit refusal was because the patient had died or become too ill between the time of the patient's admission to hospice and the initial phone call from the GRA. Another third (30.7%) changed their mind about accepting an informational visit but did not state a reason. Finally, upon follow-up call, a quarter (25.5%) of the caregivers declined stating they were no longer interested or were too busy.
Visits were made to 105 potential subjects, and the majority (64.8%) of the caregivers enrolled in the study. The primary reasons for nonenrollment were patient death (7 individuals) or patient illness (11 individuals). The study was explained to 10 persons who refused to participate without specifying a reason and 9 who stated they were too busy to participate. In summary, caregivers for 68 patients were enrolled from 672 hospice admissions (10.1%). Figure 1 summarizes the recruitment data. It is also noteworthy that seven patients had more than one caregiver who enrolled in the study, bringing total enrollment to 75 of the targeted 90.
Fig. 1.
Recruitment results.
Attrition is always a concern in an intervention study. The average length of stay in hospices was 80.5 days, with a range of 10–565 days. The average time in the study was 64.5 days, with a range of 3–510 days. The researchers collected baseline measures upon enrollment, patient follow-up measures every 2 weeks, and a caregiver follow-up every month. Complete baseline measures were obtained from 66.2% of patients upon enrollment. Two weeks later, 36.8% of patients with baseline measures were able to complete the first follow-up; after 8 weeks, 29.4% of patients were healthy enough to provide a third set of follow-up measures. Although nearly all caregivers completed baseline measures, a significant number were ineligible for follow-up after 30 days because of the death of their patient. Sixty-one percent of caregivers were still caring for hospice patients at 30 days after their enrollment in the study; the number dropped to 33.3% at 60 days postenrollment. Ninety days into the study, 20% of caregivers were still caring for their hospice patient and able to provide follow-up data. Only three caregivers refused follow-up measures; attrition was almost exclusively due to the death of the patient. One of the most important findings involved the effect of the timing for follow-up measures had upon attrition. If follow-up measures with the caregivers had been done at 14 days rather than 30 days, we would have had second measures on 92% of caregivers, cutting the attrition rate from 39% to 8%.
Discussion
Although recruitment targets for this study were successful, they were achieved as a result of good monitoring and modifications. The challenges and strategies learned from this experience included changes made to the study inclusion criteria, weather-related problems, delays in the referral and enrollment process, multiple visits and multiple caregivers, and gate-keeping by the staff.
Recruitment challenges were identified from the beginning of the project. After 6 weeks of active recruitment, and only four enrollees, the inclusion criteria were reviewed. The decision was made to add cancer as a variable to the study, rather than an inclusion criterion, to open the sampling to noncancer patients. Cancer was tracked as both a terminal diagnosis and a secondary diagnosis.
Four months into the project, the research site was hit by a record ice storm, resulting in the designation of the study region as a federal disaster area. The ice storm led to power outage for 7 days in some areas, and hospice patients could not be contacted as they were moved to hospitals and shelters. The loss of power made the technology unusable. Additionally, hospice staff members were unable to safely drive to the office or navigate to most rural patient homes. As a result, admissions came to a standstill and so did the study. There were no referrals for 19 days. One year later, the area was hit by yet another ice storm, not as severe but again impacting referrals because the staff and the community focused on managing without power for 3 days and the videophones were not useable. Following the first ice storm, a decision was made to add an additional site so that data collection was not solely dependent on one location.
Early in the study, the number of days that transpired between a patient's admission into hospice and the receipt of the consent to be contacted by GRAs averaged 9 days. The lack of an electronic medical record meant that referral forms were not received in a timely manner. This delay resulted in lost intervention days and, although improved, was never totally resolved. This is reflected in the discrepancy between the average length of stay in hospice (80.5 days) and the average time in the study (64.5 days). Throughout the duration of the study these delays resulted in 59 patients dying between the time they had agreed to be contacted and the time the referral was received. In addition to the patients who died before referrals were received, caregivers for 22 patients refused informational visits because the patient for whom they provided care either was too ill or could no longer consent to participate in the study. It is possible that these patients could have been involved in the project if the referral had been received earlier or if an electronic medical record or communications system had been available.
It was also discovered that in some cases more than one visit was necessary to present the study and obtain all consents. In several instances after explaining the study, patients and caregivers would want to discuss and decide whether they wanted to enroll. Although this is expected in research, given the short length of stay and delicate condition of hospice patients, these delays are more problematic in hospice care than in other research settings. In addition to requiring multiple visits, researchers also needed to consider situations in which multiple caregivers were involved. Seven patients in the study were actively cared for by multiple individuals who took turns and were assigned various caring roles. To capture the experiences of all involved caregivers, a decision was made to allow multiple individuals to enroll in the study as patient caregivers. Both the lack of immediate enrollment decisions and the involvement of more than one caregiver resulted in multiple visits by research staff to complete enrollment, more delays, increasing cost of research staff time and unanticipated mileage costs, and decreased number of days enrolled in the study.
Research in telehealth has found gate-keeping by staff to be a barrier to referral10; this project had that as a concern as well. To assist, a letter of support signed by each hospice medical director was given to all patients and caregivers upon admission to hospice. The physicians in both hospices were very supportive of the research project and consistently encouraged staff to refer patients and caregivers to the study. The medical director's letter of support provided credibility for the project with patients, family, and staff. The letter was presented with a brochure in a plastic sleeve in the hospice admission packet when requesting patient and caregiver consent for a follow-up visit.
Also, hospice researchers have noted the importance of involving and communicating with staff while doing research in their environment.11 To remind staff of the study, colorful attractive posters were hung on the wall in a common staff area. Additionally, in an equally visible place, a sign was put on the wall each month reporting the total number of persons who had enrolled in the study. Finally, research staff were visible in the offices with scheduled times and expected activities. The research staff completed the hospice volunteer training, making them official hospice volunteers. This not only gave the research staff an understanding of hospice, but also brought them into the “inside” world of hospice. Staff saw them as hospice volunteers who were doing research. After a few months the researchers became an accepted part of the team and were included in nonstudy-related activities such as birthday parties, building important relationships, and providing opportunities for answering questions. Continuous appreciation and recognition of the staff by the research team were very important. The initial phase or recruitment did not provide for formal recognition of referrals with any type of payment and so informal recognition and appreciation were critically important. At the end of the first year, a celebration breakfast was hosted for the staff. During this informal gathering, the recruitment statistics from the first phase of the study were shared. During the intervention phase, resources were available to recognize referrals and the hospices were presented with a check representing a small payment for each referral for the extra amount of time required to participate in the study.
The research team monitored recruitment statistics closely, making adjustments and evaluating recruitment strategies throughout the duration of the project. Adjustments were possible given the exploratory nature of the project, affirming the importance of exploratory work for the development of recruitment protocols. Although adjustments may limit the ability to generalize findings, the purpose of the pilot project was to test the feasibility of the intervention and outcomes rather than build findings for generalization. The recruitment analysis is limited as the dates for all changes were not always documented, preventing the assessment of some of the changes. It is recommended that researchers track the implementation date for changes and decisions in a more definite way in future pilot work.
Conclusions
The experiences with this project demonstrate the importance of testing recruitment and sampling protocols with pilot studies. The telehealth equipment was not perceived a barrier to recruitment by potential subjects, and even though hospice providers may have been concerned about the use of equipment, this was not cited as a reason to decline participation. To meet recruitment targets in a hospice setting, it is important to build a process that facilitates a successful outcome. Successful strategies have included the review of recruitment statistics on a monthly basis, the opening of inclusion criteria, the continuous review of related hospice processes, visible support from the medical director, and the constant and visible communication, recognition, and appreciation of the hospice staff. The value of pilot work to develop and refine recruitment strategies and their financial impact has important implications for larger follow-up study development. Defining successful recruitment, planning for expected attrition, and timing measures and interventions are critical. Finally, telehealth researchers are encouraged to maintain detailed recruitment information and share recruitment experiences to assist in the designing of future telehealth studies.
Acknowledgment
This project was funded by the National Cancer Institute R21 CA120179: Patient and Family Participation in Hospice Interdisciplinary Teams, Debra Parker Oliver, PI.
Disclosure Statement
No competing financial interests exist.
References
- 1.National Hospice and Palliative Care Organization. NHPCO facts and figures: hospice care in America 2008. Washington, DC: NHPCO; 2009. [Google Scholar]
- 2.Palmas W, et al. Recruitment and enrollment of rural and urban medically underserved elderly into a randomized trial of telemedicine case management for diabetes care. Telemed J E Health. 2006;12:601–607. doi: 10.1089/tmj.2006.12.601. [DOI] [PubMed] [Google Scholar]
- 3.Subramanian U, et al. Research in home-care telemedicine: Challenges in patient recruitment. Telemed J E Health. 2004;10:155–161. doi: 10.1089/tmj.2004.10.155. [DOI] [PubMed] [Google Scholar]
- 4.Whitten PS. Rowe-Adjibogoun J. Researching health communication technology intervention projects: The challenge of achieving utilization levels sufficient for evalution. J Technol Hum Serv. 2003;22:1–16. [Google Scholar]
- 5.Day M. Demiris G. Parker Oliver D. Exploring underutilization of videophones in hospice settings. Telemed J E Health. 2007;13:25–31. doi: 10.1089/tmj.2006.0023. [DOI] [PubMed] [Google Scholar]
- 6.Parker Oliver D, et al. Patient and family participation in hospice interdisciplinary teams, 2006–08, National Cancer Institute. Grant no. R21 CA120179.
- 7.Parker Oliver D, et al. Caregiver participation in hospice interdisciplinary team meetings via videophone technology: A pilot study to improve pain management. Am J Hosp Palliat Med. Mar. 2010. NIHMSID #170390. E-pub. [DOI] [PMC free article] [PubMed]
- 8.Parker Oliver D, et al. The use of videophones for patient and family participation in hospice interdisciplinary team meetings: A promising approach. Eur J Cancer Care. Sept. 2009. NIHMSID #107662. E-pub. [DOI] [PMC free article] [PubMed]
- 9.Parker Oliver D, et al. “They're part of the team”: Participant evaluation of the ACTive intervention. Palliat Med. 2009;23:549–555. doi: 10.1177/0269216309105725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitten PS. Dolittle G. Mackert M. Providers' acceptance of telehospice. J Palliat Med. 2005;8:730–735. doi: 10.1089/jpm.2005.8.730. [DOI] [PubMed] [Google Scholar]
- 11.McMillan SC. Weitzner MA. Methodologic issues in collecting data from debilitated patients with cancer near the end of life. Oncol Nurs Forum. 2003;30:123–129. doi: 10.1188/03.ONF.123-129. [DOI] [PubMed] [Google Scholar]