Abstract
Background
It is increasingly recognized that the impact of disease on quality of life should be taken into account when assessing health status. It is likely that tooth loss, in most cases being a consequence of oral diseases, affects Oral Health-Related Quality of Life (OHRQoL). The aim of the present study is to systematically review the literature and to analyse the relationship between the number and location of missing teeth and oral health-related quality of life (OHRQoL). It was hypothesized that tooth loss is associated with an impairment of OHRQoL. Secondly, it was hypothesized that location and distribution of remaining teeth play an important role in this.
Methods
Relevant databases were searched for papers in English, published from 1990 to July 2009 following a broad search strategy. Relevant papers were selected by two independent readers using predefined exclusion criteria, firstly on the basis of abstracts, secondly by assessing full-text papers. Selected studies were grouped on the basis of OHRQoL instruments used and assessed for feasibility for quantitative synthesis. Comparable outcomes were subjected to meta-analysis; remaining outcomes were subjected to a qualitative synthesis only.
Results
From a total of 924 references, 35 were eligible for synthesis (inter-reader agreement abstracts κ = 0.84 ± 0.03; full-texts: κ = 0.68 ± 0.06). Meta-analysis was feasible for 10 studies reporting on 13 different samples, resulting in 6 separate analyses. All studies showed that tooth loss is associated with unfavourable OHRQoL scores, independent of study location and OHRQoL instrument used. Qualitative synthesis showed that all 9 studies investigating a possible relationship between number of occluding pairs of teeth present and OHRQoL reported significant positive correlations. Five studies presented separate data regarding OHRQoL and location of tooth loss (anterior tooth loss vs. posterior tooth loss). Four of these reported highest impact for anterior tooth loss; one study indicated a similar impact for both locations of tooth loss.
Conclusions
This study provides fairly strong evidence that tooth loss is associated with impairment of OHRQoL and location and distribution of tooth loss affect the severity of the impairment. This association seems to be independent from the OHRQoL instrument used and context of the included samples.
Background
It is increasingly recognized that the impact on quality of life (QoL) of disease and treatment of disease and its consequences should be taken into account when assessing health status and evaluating treatment outcomes. Clinical indicators only are not sufficient to describe health status and it has been reported that people with chronic disabling disorders can perceive their quality of life as better than healthy individuals, i.e., poor health or presence of disease does not inevitably mean poor quality of life [1,2]. Adaptive capacity and personal characteristics appear to influence patient's response to chronic disease. This can result in reports which seem counterintuitive, for example, the finding in a large German survey that having fewer than 9 teeth had more impact on health-related QoL than having cancer, hypertension, or allergy [3]. Therefore, clinical indicators only are not sufficient to describe health status. This is also true for oral diseases and its consequences for oral health-related quality of life (OHRQoL). The two most prevalent oral diseases, caries and periodontal disease often do not cause symptoms in early stages. This might explain that clinical indicators of caries or periodontal involvement, such as number of decayed teeth, respectively tooth mobility and pocket depth are not strongly associated with impairment of OHRQoL [4,5]. However, caries and periodontal disease are progressive processes, and lead to tooth loss if not treated adequately. Tooth loss will presumably cause functional impairment, for example, with regard to chewing and esthetics, depending on the location of tooth loss, which might ultimately affect QoL.
Besides generic health related QoL measures, specific oral health-related quality of life models and measures have been developed to assess the impact of oral disease on OHRQoL [6]. For example Locker [7] described a model based on the WHO classification of impairment, disability and handicap. The Oral Health Impact Profile (OHIP), one of the most popular measures, was developed on basis of this model [8].
Although OHRQoL assessment by validated questionnaires is more common nowadays, a recent systematic review of the literature resulted in only sparse information regarding OHRQoL treatment outcomes of reconstructive dentistry for partially edentate patients [9]. However, besides using OHRQoL measures to evaluate treatment outcomes it is in the first place important to know to what extent tooth loss actually affects OHRQoL. This enables development of clinical decision making in public health and to provide appropriate oral health care. Several population surveys include 'number of teeth' in statistical models analyzing impact on OHRQoL, but this parameter appears not always to be the most prominent predictor. For example, in a population of older adults in Sri Lanka, Ekanayake [10] found only a weak association between tooth loss and other clinical parameters on the one hand and oral impacts on the other hand. This suggests that other factors such as age, gender or cultural background of the patient play an important role in the perception of health [10,11]. In contrast, in a large Japanese study Ide et al [12] found a strong correlation between the number of missing teeth and higher OHIP scores suggesting impairment of OHRQoL.
The aim of the present study is to systematically review the literature and to analyse the relationship between the number and location of missing teeth and oral health-related quality of life (OHRQoL). It was hypothesized that tooth loss is associated with an impairment of OHRQoL. Secondly, it was hypothesized that location and distribution of remaining teeth play an important role in this.
Methods
Search strategy
In this study the Cochrane guidelines for the conduct of a systematic review were used [13]. Medline, PubMed, Embase and the Cochrane Library were initially searched for papers published from 1990 to June 2008 to answer the following question: is tooth loss associated with impairment of people's oral health related quality of life and what is the role of location and distribution of tooth loss in this relationship? The search was updated in July 2009. A broad search strategy was pursued to capture as many relevant studies as possible. For this reason not only studies with subject matter 'tooth loss' but also studies with subject matter 'management of tooth loss' were searched for. The following keywords were used: 'quality of life', 'patient satisfaction', 'tooth loss', 'partial edent*', 'partial denture', 'implant' and 'prosthodont*'. MeSH terms were used if the search machine of the database permitted this. The full search strategy for PubMed is presented in Table 1. As in the early nineteen nineties quality of life was not a general used concept in dentistry, patient satisfaction was used as a proxy of quality of life. Although RCT's provide the highest level of evidence, this study design is in most cases not feasible for tooth loss. Therefore, data from observational studies like cross-sectional studies, case series, case-control and cohort studies are included in this review [14]. Only publications in English were selected. Reference lists of the eventually included papers were hand-searched to identify additional relevant studies and possible false exclusions, until no new applicable titles appeared (saturation).
Table 1.
PubMed search as used
| #1 | ("Quality of Life"[MeSH]) OR ("Patient Satisfaction"[MeSH]) |
|---|---|
| #2 | ("Denture, Partial"[MeSH]) OR ("Denture, Partial, Fixed"[MeSH]) OR ("Dental Implants"[MeSH]) OR ("Dental Implants, Single-Tooth"[MeSH]) OR ("Dental Prosthesis, Implant-Supported"[MeSH]) OR ("Osseointegration"[MeSH]) OR ("Dental Implantation"[MeSH]) |
| #3 | ("Jaw, Edentulous, Partially"[MeSH]) OR ("Tooth Loss"[MeSH]) |
| #4 | (#1 AND #2) |
| #5 | (#1 AND #3) |
| #6 | (#4 OR #5) |
PubMed search using MeSH terms
Study selection
Two readers (NHJC and AEG) independently selected references on the basis of titles and abstracts for the impact of tooth loss or tooth replacement on oral health-related quality of life using predefined exclusion criteria. Excluded were case reports, (narrative) reviews, non-human studies, non-oral implants (hip/knee) studies, studies exclusively dealing with edentulous subjects/full (over)dentures, restorations not replacing teeth, orthodontics, periodontics, tooth wear, and medical compromised patient groups (e.g. irradiated patients and systemic diseases like diabetes). The readers were calibrated by discussion sessions after assessment of every 10 abstracts. If necessary, the list of excluding criteria was revised after a discussion session and those abstracts already screened were re-subjected to the selection process. This procedure was repeated until no new exclusion criteria turned up. Agreement between readers was determined using κ statistics. Disagreements were resolved by discussion and if not resolved a third reader was called in (PFA) and reviewed the manuscript independently. In cases of doubt, the reference was included. This approach was applied in all selection steps.
After abstract selection, full-text copies of the selected papers were made. These full-text papers were assessed independently by the two readers (NHJC and AEG) using a pilot-tested assessment form. Full-text paper exclusion criteria are outlined in Table 2. In this phase of the review process, if considered necessary, authors were contacted to clarify issues of their published research that gave rise to uncertainty.
Table 2.
Exclusion criteria applied for eligibility assessment of full-text papers and number of exclusions
| Reason for exclusion (eligibility) | Number of studies excluded |
|---|---|
| Incomplete sample information | 10 |
| • Sampling method unclear | |
| • Age distribution not stated | |
| • Gender distribution not stated | |
| Insufficient methods (information) | 26 |
| • No clinical examination or validated 'self tooth count' form not used | |
| • Measure for satisfaction or OHRQoL not clearly described | |
| • Details of replacement not explicit | |
| OHRQoL outcomes not related to (management of) tooth loss | 73 |
| Mistakenly included on the basis of abstract | 20 |
| Total | 129 |
Synthesis of data
Studies were grouped on the basis of OHRQoL instruments used: Oral Health Impact Profile (OHIP), Oral Impact on Daily Living (OIDP), Geriatric Oral Health Assessment Index (GOHAI), Dental Impact of Daily Living (DIDL), OHQoL-UK©, and others. The rationale for this grouping was the incompatibility of the various instrument scoring systems. Besides that, the categorizations of number of teeth as used in the original studies should be comparable. Subsequently, for studies presenting continuous outcomes (e.g. mean scores) meta-analysis was deemed possible if a variance estimate was presented such as SD or SE. For studies presenting dichotomized outcomes pooling was considered possible if numbers with or without outcome property (e.g. with or without impact) were presented.
For continuous data Cochran's Q [15] was calculated to test for heterogeneity. Summary effects were calculated with DerSimonian's method [16] in case of heterogeneous data and weighted average was calculated for homogeneous data.
For dichotomized data Woolf's test [17] for heterogeneity was used. Again, summary effects were calculated by DerSimonian's method [16] in case of heterogeneous data, but the Mantel-Haenszel test [18] was used for homogenous data.
All studies, including those not suitable for meta-analyses, were subjected to qualitative analyses. For qualitative analyses study characteristics, main outcomes concerning missing teeth and possible other relevant outcomes were extracted and grouped according to OHRQoL instrument used.
Results
Study selection and study characteristics
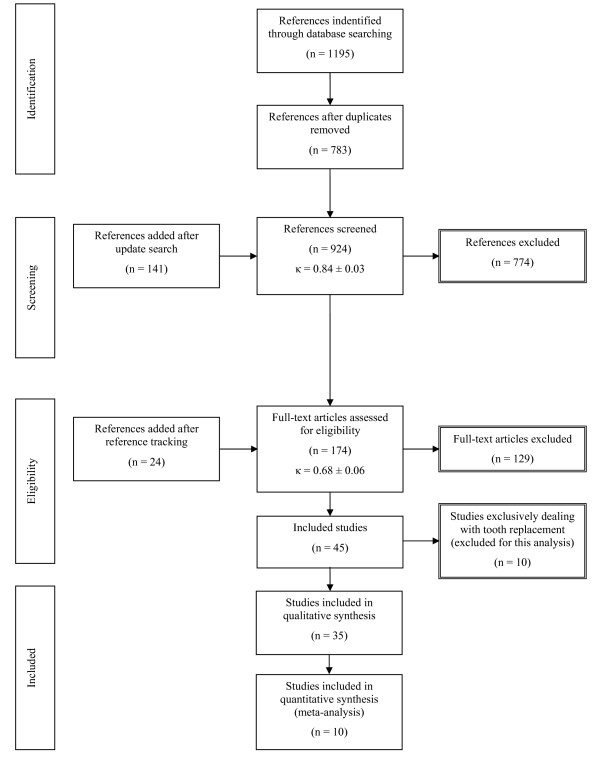
Details of the identification, screening and selection process are presented in Figure 1. A total of 396 references was identified through the searching of Medline, 516 through PubMed, 134 through Embase, and 149 through the Cochrane Library. Duplicate references were removed and eventually 783 references remained. The search update resulted in 141 additional abstracts. For abstract assessment complete agreement was seen for 884 abstracts (inter-reader agreement κ = 0.84; SE = 0.03) and consensus was reached in 40 cases (23 included, 17 excluded). After reviewing the abstracts, 150 studies were included in the study. Reference tracking revealed 24 additional papers adding up to a total of 174 full-text papers for eligibility assessment. Finally, after assessment of full-text articles, 45 papers were included for review (inter-reader agreement κ = 0.68; SE = 0.06). In 5 cases the third reader's judgement was decisive. As the present study is only dealing with tooth loss, and not with management of tooth loss, studies exclusively dealing with the latter were not used for the present analyses. Characteristics and main outcomes of the 35 remaining studies [4,5,10,12,19-49] are presented in Additional file 1, Table S1; a summary of the data and feasibility for meta-analysis are presented in Additional file 2, Table S2.
Figure 1.
Flow chart outlining the search strategy and results along various steps.
Quantitative analyses
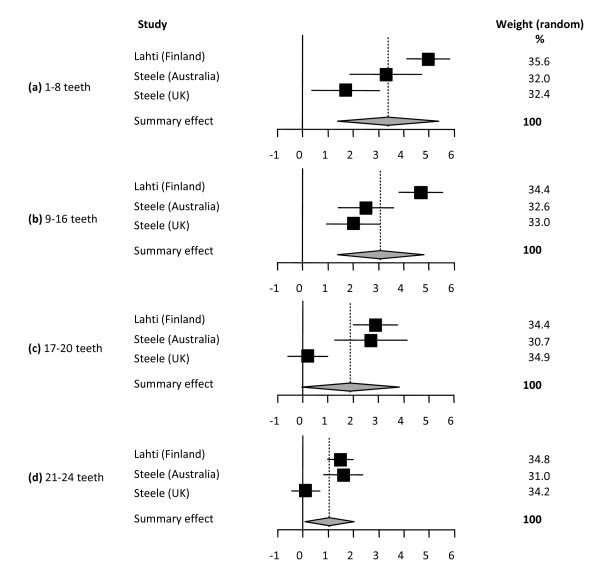
In summary, 10 studies reporting on 13 different samples were eligible for meta-analysis resulting in 6 separate syntheses on the outcomes of 4 OHRQoL instruments (Table 3, Figures 2, 3, 4, 5, 6, 7).
Table 3.
Summary of the 6 meta-analyses
| Comparison | Summary effect | 95% CI | p-value for heterogeneity test | Model used |
|---|---|---|---|---|
|
Meta analysis 1 [25,43] Continuous data (difference in mean OHIP total scores) Total n = 12,965 Reference group: 25-32 teeth | ||||
| 1-8 teeth | 3.37 | 1.37-5.38 | <0.001 | random effect |
| 9-16 teeth | 3.08 | 1.37-4.80 | <0.001 | random effect |
| 17-20 teeth | 1.89 | -0.03-3.82 | <0.001 | random effect |
| 21-24 teeth | 1.05 | 0.07-2.02 | <0.001 | random effect |
|
Meta analysis 2 [25,26] Dichotomized data (Odds ratio for having an OHIP impact) Total n = 6821 Reference group: complete dentition or ≥ 25 teeth | ||||
| Incomplete or < 25 teeth | 3.45 | 2.93-4.05 | 0.975 | fixed effect |
|
Meta analysis 3 [5,24,45] Dichotomized data (Odds ratio for having an OIDP impact) Total n = 2204 Reference group ≥ 21 teeth | ||||
| ≤ 10 teeth | 2.01 | 1.43-2.83 | 0.962 | fixed effect |
| >10 and <21 teeth | 1.63 | 1.23-2.17 | 0.794 | fixed effect |
|
Meta analysis 4 [5,45] Dichotomized data (Odds ratio for having an OIDP impact) Total n = 1184 Reference groups 9-16 NOPs/4-8 POPs/no UAS | ||||
| 0-8 NOPs | 1.99 | 1.39-2.86 | 0.279 | fixed effect |
| 0-3 POPs | 1.66 | 1.16-2.37 | 0.808 | fixed effect |
| UAS | 1.82 | 0.68-4.87 | 0.025 | random effect |
|
Meta analysis 5 [38,46] Continuous data (difference in mean GOHAI total scores) Total n = 435 Reference group: 20-32 teeth | ||||
| 0-19 teeth | 9.78 | 7.38-12.18 | 0.157 | fixed effect |
|
Meta analysis 6 [31,35] Continuous data (difference in mean OHQoL-UK total scores) Total n = 2738 Reference group: 20-32 teeth | ||||
| 0-19 teeth | 4.56 | 3.67-5.44 | 0.912 | fixed effect |
Figure 2.
Synthesis of two studies presenting differences in mean OHIP total scores. Forest plots presenting differences in mean OHIP total scores of categories of number of present teeth for three samples (total n = 12,965) [25,43]. The category 25-32 teeth was used as reference. Relative box size indicates the weight of the study: (a) 1-8 teeth (heterogeneity Q = 16.75; df = 2), (b) 9-16 teeth (heterogeneity Q = 17.80; df = 2), (c) 17-20 teeth (heterogeneity Q = 22.06; df = 2), (d) 21-24 teeth (heterogeneity Q = 15.51; df = 2).
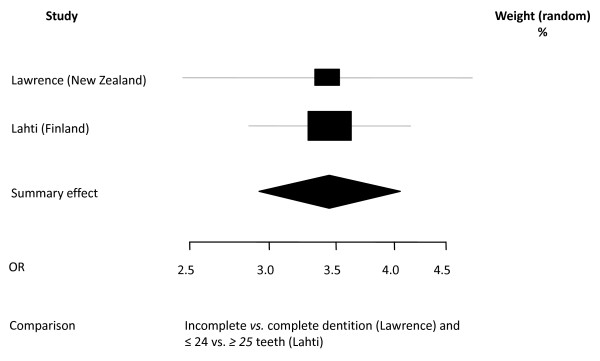
Figure 3.
Synthesis of two OHIP studies presenting Odds Ratio's. Forest plot presenting Odss Ratio's (OR) for having OHIP impacts (fairly/very often) of two categories of number of present teeth (incomplete vs. complete [26] and ≤ 24 vs. ≥ 25 [25]) in two samples (total n = 6821). Relative box size indicates weight of the study (heterogeneity Χ2 = 0,00; df = 1).
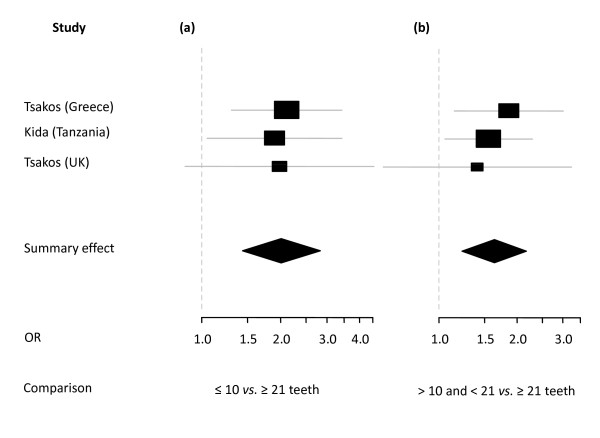
Figure 4.
Synthesis of three OIDP studies presenting Odds Ratio's. Forest plots presenting Odss Ratio's (OR) for having any impact on OIDP of three categories of number of present teeth in three samples (total n = 2204) [5,24,45]. Relative box size indicates weight of the study. (a) ≤ 10 vs. ≥ 21 (heterogeneity Χ2 = 0.08; df = 2), (b) >10 and < 21 vs. ≥ 21 teeth (heterogeneity Χ2 = 0.46; df = 2).
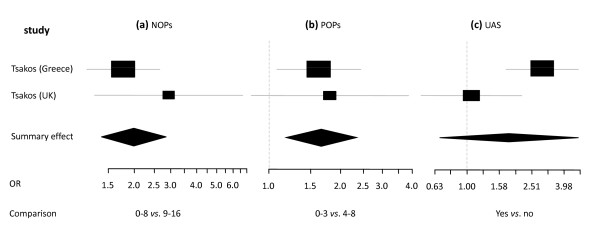
Figure 5.
Synthesis of two OIDP studies presenting Odds Ratio's in relation to occluding pairs and location. Forest plots presenting Odss Ratio's (OR) for having any impact on OIDP of two categories of number of natural occluding pairs (NOPs) and posterior occluding pairs (POPs) and unrestored anterior spaces (UAS) in two samples (total n = 1184) [5,45]. Relative box size indicates weight of the study. (a) NOPs 0-8 vs. 9-16 (heterogeneity Χ2 = 1.17; df = 1), (b) POPs 0-3 vs. 4-8 (heterogeneity Χ2 = 0.06; df = 1), (c) UAS yes vs. no (heterogeneity Χ2 = 5.03; df = 1).
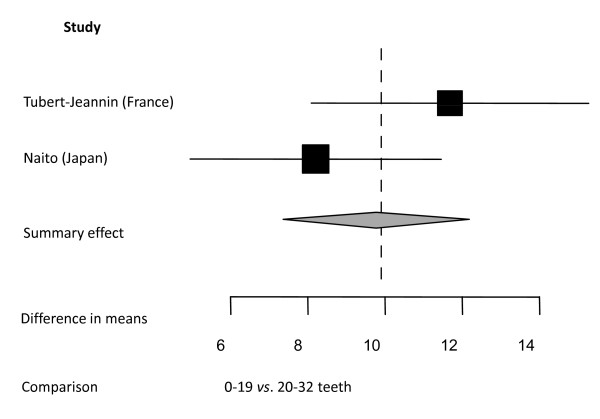
Figure 6.
Synthesis of two studies presenting differences in mean GOHAI total scores. Forest plot presenting differences in mean GOHAI total scores between two categories of number of present teeth: 0-19 teeth vs. 20+ teeth in two samples (total n = 435) [38,46]. Relative box size indicates weight of the study (heterogeneity Q = 2.00; df = 1).
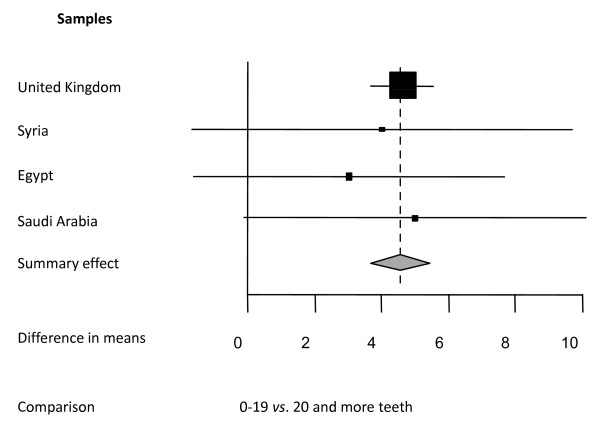
Figure 7.
Synthesis of two studies presenting differences in mean OHQoL-UK© total scores in four samples. Forest plot presenting differences in mean OHQoL-UK© total scores between two categories of numbers of present teeth: 0-19 teeth vs. 20 and more teeth in four samples (total n = 2738) described in two studies [31,35]. Relative box size indicates weight of the study (heterogeneity Q = 0.15; df = 3).
Oral Health Impact Profile (OHIP) studies
Two studies [25,43] reported OHIP data as mean total scores (SD) from three different samples of three cross-sectional surveys from the UK (n = 3662), Australia (n = 3406) and Finland (n = 5987). In this analyses mean OHIP scores of subjects with 25-32 teeth were compared with mean OHIP scores of subjects having 21-24 teeth, 17-20 teeth, 9-16 teeth and 1-8 teeth (Figure 2). Data are presented as differences in mean OHIP scores per group for each sample. This meta-analysis shows that the fewer teeth are present the higher the impact on OHRQoL with a marked deterioration once the number of remaining teeth drops below 17.
Two studies [25,26], including in total 6,821 subjects, reported OHIP data as prevalence of impacts according to dental status (Figure 3). One study categorized dental status as complete dentition vs. one or more missing teeth [26] whereas the other study categorized dental status as 32-25 teeth vs. 0-24 teeth [25]. This pooling was made on the assumption that categories were comparable. Differences in impact scores between the two categories in each study are presented as Odds Ratios. The pooled data indicate that loss of teeth is associated with a threefold likelihood of reporting an impact on OHRQoL.
Oral Impact on Daily Living (OIDP) studies
The three studies [5,24,45], including in total 2204 subjects, that used OIDP scores as an outcome measure for OHRQoL are presented in Figure 4. In all three studies OIPD scores were calculated by multiplying frequency by severity of the impact and summing up the scores of ten areas of daily activities. Three categories of dental status were presented namely 0/1-10, 11-20 and 21-32 teeth present. Differences between the categories were presented as Odds Ratios with having an impact as dependent variable. Subjects with fewer than 10 teeth were twice as likely to report an impact compared with subjects having 21-32 teeth; subject with 11-20 teeth were 1.5 times more likely to report an impact.
Two of the OIDP studies [5,45] (total number of subjects = 1184) presented OHRQoL data in relation to occluding pairs and location of tooth loss: natural occluding pairs (NOPs), posterior occluding pairs (POPs), and presence of 'unrestored anterior spaces' (UAS). Differences between categories are presented as Odds Ratio's with having an impact as dependent variable (Figure 5). Reporting an impact on their daily life was twice as likely for subjects with 0-8 NOPs than for subjects having 9-16 NOPs and 1.6 times more likely for subjects having 0-3 POPs than for subjects having 4-8 POPs. Subjects having one or more unrestored anterior spaces were 1.8 times more likely to report any impact on their daily life.
Geriatric Oral Health Assessment Index (GOHAI) studies
The two GOHAI studies [38,46] (total n = 435) in this meta-analysis used mean total scores as outcome measure (Figure 6). Differences in the mean scores show that GOHAI scores were higher for subjects with 20 or more teeth, indicating better OHRQoL.
Oral Health Quality of Life-UK (OHQoL-UK© )studies
Two studies [31,35] reported mean total scores for OHQoL-UK© for four different samples from the UK, Syria, Egypt and Saudi Arabia with a total of 2783 subjects (Figure 7). Differences between mean total scores of two categories of dental status, namely 0-19 teeth present vs. 20 and more teeth. It should be noted that the UK sample contributes 91% to the summary effect.
Qualitative analyses
The studies that failed the criteria for meta-analysis were only analyzed qualitatively.
Number of teeth
Most included studies found statistically significant associations between missing teeth and unfavourable OHQoL scores, independent of the instrument used or the country of investigation. However, the results of a few studies were not conclusive: Hassel [23] reported no statistically significant difference in OHIP scores between dentate and edentate institutionalized elderly, but statistically significant higher OHIP scores for subject with 'less teeth in static occlusion'; Mesas [37] reported only statistically significant differences in GOHAI scores between edentulous and dentate subjects for the 'physical' dimension but not for the 'social' and 'worry' dimension; Tsakos [5] and Sheiham [41], reporting on the same sample, found no statistically significant association between number of present teeth and having an OIPD impact in British adults, but lower numbers of anterior occluding pairs and natural occluding pairs were associated with OHRQoL impairment.
Occluding pairs and location of missing teeth
Statistically significant positive correlations between number of occluding pairs and OHRQoL were found in all 10 studies (dealing with 9 different samples) reporting on this subject [5,20,21,23,27,29,36,37,44,45] (Table 4).
Table 4.
Summary of studies reporting on occluding pairs
| First author, year | Population, sample n, (% females) | Subject of the study | Main outcomes regarding occluding pairs |
|---|---|---|---|
| OHIP-49 (Oral Health Impact Profile) | |||
| Baba, 2008aCS [20] Baba, 2008bCS [21] |
Japanese adults with shortened dental arches n = 155 (70) |
Relationship between shortened dental arches and OHRQoL | a: Dose response relationship between number of missing posterior teeth and OHRQoL in subjects with shortened dental arches. Missing posterior units is related to impairment of OHRQoL. b: Patterns of missing occluding units likely to be related to the OHRQoL impairment in shortened dental arch subjects with the presence of first molar contact having a particularly important role. |
| Hassel,2006CS [23] | German institutionalized elderly n = 159 (81) |
Dental and non-dental factors on OHRQoL of institutionalized elderly | Less teeth in static occlusion related to impairment of OHRQoL. |
| Locker, 1994LT [29] | Canadian older adults n = 312 (54) |
Clinical and subjective indicators of oral health status and OHRQoL | Having fewer functional units associated with impairment of OHRQoL. |
| GOHAI (Geriatric Oral Health Assessment Index) | |||
| Mesas, 2008CS [37] | Brazilian urban elderly n = 267 (60) |
Dental and non-dental factors on OHRQoL | Absence of posterior occlusion associated with impairment of OHRQoL but only statistically significant for 'physical' dimension and not for the 'social' and 'worry' dimensions. |
| Swoboda, 2006CS [44] | American low income elderly n = 733 (56) |
Dental and non-dental predictors on OHRQoL | OHRQoL positively related to the total number of occluding pairs, molar pairs occluding, anterior pairs occluding, and premolar pairs occluding. |
| OIDP (Oral Impact on Daily Performance) | |||
| Tsakos, 2006CS [5] | British non-institutionalized elderly (subsample of Sheiham, 2001) n = 736 (48) |
Clinical correlates of OHRQoL | OHRQoL significantly related to the total number of occluding pairs and to the number of anterior occluding pairs but not to the number of posterior occluding pairs. |
| Tsakos, 2004CS [45] | Greek non-institutionalized elderly n = 448 (64) |
Relationship between clinical dental measures and OHRQoL | OHRQoL significantly related to the total number of occluding pairs and to the number of posterior occluding pairs. |
| Ad hoc satisfaction questionnaires | |||
| Leake, 1994CS [27] | American and Canadian older adults n = 338 (55) |
Assessment of relationship between oral function and posterior dental units | Low number of posterior units was associated with embarrassment and dissatisfaction on chewing and appearance, indicating OHRQoL impairment. |
| Meeuwissen, 1995CS [36] | Dutch dentate older adults n = 320 (59) |
Satisfaction with reduced dentitions | Fewer posterior occluding units associated with lower satisfaction scores, indicating OHRQoL impairment. |
CS = cross-sectional study; LT = longitudinal study; CO = cohort study; VA = validation study
Five studies reported on OHRQoL and location of missing teeth, four of them [5,40,45,48] reporting higher impact for missing anterior teeth. One of them [44] indicated comparable impact for missing posterior occluding pairs and anterior occluding pairs (Table 5).
Table 5.
Summary of studies reporting the location of missing teeth
| First author, year | Population, sample n, (% females) | Subject of the study | Main outcomes regarding location of missing teeth |
|---|---|---|---|
| OHIP-49 (Oral Health Impact Profile) | |||
| Walter, 2007CS [48] | Canadian rural adults n = 140 (64) |
Clinical and socio-demographic variables and OHRQoL | One or more natural posterior teeth missing not associated with OHRQoL impairment whereas one or more natural anterior teeth missing was associated with OHRQoL impairment. |
| OHIP-14 (Oral Health Impact Profile short version) | |||
| Pallegedara, 2008CS [40] | Sinhalese non-institutionalized elderly n = 630 (54) |
Tooth loss, denture status and OHRQoL | 'Presence of anterior spaces' more negative impact on the OHRQoL than 'missing posterior teeth'. |
| GOHAI (Geriatric Oral Health Assessment Index) | |||
| Swoboda, 2006CS [44] | American low income elderly n = 733 (56) |
Dental and non-dental predictors on OHRQoL | Comparable impact on OHRQoL of the number of molar pairs occluding, premolar pairs occluding and anterior pairs occluding. |
| OIDP (Oral Impact on Daily Performance) | |||
| Tsakos, 2004CS [45] | Greek non-institutionalized elderly n = 448 (48) |
Relationship between clinical dental measures and OHRQoL | Having 'unfilled anterior spaces' more impact on OHRQoL than having few (0-3) posterior occluding pairs. |
| Tsakos, 2006CS [5] | British non-institutionalized elderly n = 736 (64) |
Clinical correlates of OHRQoL | Having few anterior occluding pairs (0-2) more impact on OHRQoL than having few posterior occluding pairs (0-3). |
CS = cross-sectional study; LT = longitudinal study; CO = cohort study; VA = validation study
Discussion
Chronic diseases such as dental caries are still highly prevalent in older adults, and the risk of tooth loss in old age is high. Oral health care with an intervention led focus is costly, and demand for this care may increase as the proportion of older dentate adults increases. Demand for treatment is not well correlated with objectively determined treatment need, and it has been recognized that objective measures of disease are not good predictors of demand. It would appear that loss of teeth is not as acceptable as in previous generations, and this will potentially influence future demand for treatment [50]. As public resources for dental treatment becomes increasingly scarce, new paradigms for assessment of oral health have been developed. The use of OHRQoL measures has increased significantly over the past 15 years. By incorporating subjective and objective assessment, our understanding of the consequences of oral disease and tooth loss has improved [51]. Subjective assessment has also been advocated as a means of targeting treatment resources provided through publically funded health services [52]. The rationale for this is to prioritise scarce financial resources towards those eligible patients most likely to benefit from a particular therapy. It is known that the impact of disease on quality of life is highly variable, and thus, the impact of a treatment intervention will also vary. An example of this is in the use of dental implants to retain prostheses in edentulous patients. Dental status (in this case, edentate) does not necessarily predict treatment outcome, and edentate patients satisfied with having complete dentures are unlikely to report significant extra benefit from having an expensive intervention (e.g., implant retained dentures) [53]. In this scenario, a health service provider would prefer to target resources towards patients who are dissatisfied with being edentate and have a poor self-reported health status. This is particularly relevant where a cure is not the objective of treatment, and the treatment goal is a reduction in morbidity associated with chronic disease.
Individual studies that have reported OHRQoL outcomes have indentified predictors of poor OHRQoL. These included disease severity, dental status, social class and cultural background. Unfortunately, there has been a lack of uniformity in methods used to collect these data, and this has created some difficulty in generalizing the results of individual studies. A variety of OHRQoL measures have been used, ranging from ad hoc, non-validated questionnaires (mostly used in the early nineteen nineties when quality of life was not a general used concept in dentistry yet), to comprehensive measures based on conceptual models and validated for use in particular populations. In the case of the latter measures, scoring systems have varied and been reported variously as prevalence, severity, and combinations of negative and positive perceptions of health. Finally, population studies have for the most part used shortened versions of validated measures such as the OHIP and this may lead to under-reporting of impacts.
Given these concerns, this review of the literature aimed to assimilate all of the available information on the relationship between tooth loss and OHRQoL in a systematic way using existing guidelines for conducting a systematic review. There were some limitations common to most systematic reviews, primarily difficulty in accessing literature not published in English. In order to minimize the possibility of publication bias, authors with acknowledged expertise in the field were contacted to determine if they had relevant data, which had not yet been published. They were also asked to clarify issues in their published research, which gave rise to uncertainty during the data extraction phase of the review. Accordingly, we believe that we have minimized the impact of reporting and publication bias.
Quality assessment of included studies was restricted to the use of exclusion criteria. These included minimal criteria of sample description (age and gender distribution) but not for example Socio Economic Status (SES). Other criteria indicating the quality of surveys, such as the number of observers, observer agreements, representativeness for larger samples, and the use of validated instruments were not always described, but were not used in the exclusion process. For instance, nine of the included studies were validation studies and these studies - presenting relevant data - would have been excluded in case the use of a validated instrument were an inclusion criterion. Although these studies were designed for another purpose, i.e. to test the psychometric properties of newly developed OHRQoL instruments, it was considered to be appropriate to use data on the number of missing teeth from these studies.
As far as we are aware of, this is the first systematic review and meta-analysis of the relationship between OHRQoL and tooth loss. Data from our systematic review and meta-analyses of observational studies provide fairly strong evidence that tooth loss is, on the whole, viewed negatively. This is a consistent finding, and appears to be independent of the OHRQoL measure used to assess subjective impact and context (e.g., country of residence). However, the severity of impairment of OHRQoL is probably context dependent [43]. Moreover, the severity of impairment might be associated with location and distribution of missing teeth, as suggested by the outcome of the meta-analysis of data of a Greek and a British population (Figure 5). Although associated, the correlation between number of missing teeth and number of occluding pairs (which is a derivative of the distribution of missing teeth) is not linear [54]. Therefore, the impact of cultural background, and location and distribution of missing teeth remains subject for further exploration.
It should be acknowledged that all studies are reported at population level, and this may mask heterogeneity of scores at an individual level. The latter is reflected by the wide variation in outcome scores in the meta-analyses as presented in Figures 2, 3, 4, 5, 6 and 7. Despite this, it seems that the negative view of tooth loss may ultimately result in demand for treatment to replace missing teeth. This will include a demand for dental implant retained restorations and other costly forms of treatment with a high burden of maintenance. Acceptance of dental extraction and replacement of teeth with conventional removable dentures, either partial or complete, has diminished [50]; furthermore, ability to adapt to complete replacement dentures in old age is also uncertain and best avoided if possible. This poses a considerable challenge for oral health care policy makers, and it is unlikely that all demand for high cost treatment interventions can be met solely by publicly funded healthcare.
The shortened dental arch concept has been described as means of providing sub-optimal, but acceptable level of oral function [55]. In limiting treatment goals to providing a shortened dental arch, costs of care can be minimized. The results of the review suggest that the number of occluding pairs of teeth is an important predictor of OHRQoL, and that the prevalence of negative impacts increases sharply once the number of teeth present drops below 20. It seems reasonable to suggest that application of the shortened dental arch approach is acceptable, particularly to older adults, and this may help inform public policy for oral health care in older age groups. The data also suggest that preventive strategies aimed at reducing tooth loss need to be reinforced. As reported by Petersen and Yamamoto [56], most oral diseases and chronic disease share common risk factors, and national health programs should incorporate disease prevention and health promotion using a common risk factor approach. Given the rising burden of chronic disease in an aging population, coupled with its negative impact on quality of life, this should receive urgent attention from policy makers.
Conclusions
This study provides fairly strong evidence that tooth loss is associated with impairment in OHRQoL. This association appeared to be independent from the OHRQoL instrument used and context (e.g., cultural background) of the included samples. However, the extent and severity of impairment seems to be context dependent. Moreover, this study indicates that not only number, but also location and distribution of missing teeth affect the severity of OHQoL impairment. Given the negative consequences of tooth loss on OHRQoL, it is important that disease prevention measures are promoted when formulating health policy for older adults. It is likely that there will be greater demand from patients for treatment aimed at preserving teeth. The effectiveness of preventive strategies will require further research, and further economic analysis of tooth replacement strategies is also required.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AEG designed the study, assessed all included publications for eligibility and drafted the manuscript. EMB performed the statistical analyses and assisted in the interpretation of the data and helped to draft the manuscript, PFA participated in the design of the study and assessment of the included papers and helped to draft the manuscript, DJW helped to draft the manuscript, NHJC participated in the design of the study, assessed all included publications for eligibility and helped to draft the manuscript. All authors read and approved the final manuscript.
Supplementary Material
Table S1: Summary of primary and additional outcomes of all included studies
Summary of data of all included studies and feasibility for meta-analysis.
Contributor Information
Anneloes E Gerritsen, Email: a.gerritsen@dent.umcn.nl.
P Finbarr Allen, Email: f.allen@ucc.ie.
Dick J Witter, Email: d.witter@dent.umcn.nl.
Ewald M Bronkhorst, Email: e.bronkhorst@dent.umcn.nl.
Nico HJ Creugers, Email: n.creugers@dent.umcn.nl.
References
- Decker SD, Schultz R, Wood D. Determinants of well-being in primary caregivers of spinal cord injured persons. Rehabil Nurs. 1989;14:6–8. doi: 10.1002/j.2048-7940.1989.tb00664.x. [DOI] [PubMed] [Google Scholar]
- Sprangers MA, Aaronson NK. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease: a review. J Clin Epidemiol. 1992;45:743–760. doi: 10.1016/0895-4356(92)90052-O. [DOI] [PubMed] [Google Scholar]
- Mack F, Schwahn C, Feine JS, Mundt T, Bernhardt O, John U, Kocher PT, Biffar R. The impact of tooth loss on general health related to quality of life among elderly Pomeranians: results from the study of health in Pomerania (SHIP-O) Int J Prosthodont. 2005;18:414–419. [PubMed] [Google Scholar]
- Marino R, Schofield M, Wright C, Calache H, Minichiello V. Self-reported and clinically determined oral health status predictors for quality of life in dentate older migrant adults. Community Dent Oral Epidemiol. 2008;36:85–94. doi: 10.1111/j.1600-0528.2007.00378.x. [DOI] [PubMed] [Google Scholar]
- Tsakos G, Steele JG, Marcenes W, Walls AW, Sheiham A. Clinical correlates of oral health-related quality of life: evidence from a national sample of British older people. Eur J Oral Sci. 2006;114:391–395. doi: 10.1111/j.1600-0722.2006.00398.x. [DOI] [PubMed] [Google Scholar]
- Allen PF. Assessment of oral health related quality of life. Health Qual Life Outcomes. 2003;1:40. doi: 10.1186/1477-7525-1-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- Thomason JM, Heydecke G, Feine JS, Ellis JS. How do patients perceive the benefit of reconstructive dentistry with regard to oral health-related quality of life and patient satisfaction? A systematic review. Clin Oral Implants Res. 2007;18(Suppl 3):168–188. doi: 10.1111/j.1600-0501.2007.01461.x. [DOI] [PubMed] [Google Scholar]
- Ekanayake L, Perera I. The association between clinical oral health status and oral impacts experienced by older individuals in Sri Lanka. J Oral Rehabil. 2004;31:831–836. doi: 10.1111/j.1365-2842.2004.01311.x. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa KT, Tejero JS, Kim J, Padilla GV, Hellemann G. Examining predictive models of HRQOL in a population-based, multiethnic sample of women with breast carcinoma. Qual Life Res. 2007;16:413–428. doi: 10.1007/s11136-006-9138-4. [DOI] [PubMed] [Google Scholar]
- Ide R, Yamamoto R, Mizoue T. The Japanese version of the Oral Health Impact Profile (OHIP)--validation among young and middle-aged adults. Community Dent Health. 2006;23:158–163. [PubMed] [Google Scholar]
- Higgings JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Library; 2009. http://www.cochrane-handbook.org Version 5.0.2. [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. doi: 10.2307/3001666. [DOI] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Woolf B. On estimating the relation between blood group and disease. Ann Hum Genet. 1955;19:251–253. doi: 10.1111/j.1469-1809.1955.tb01348.x. [DOI] [PubMed] [Google Scholar]
- Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- Atchison KA, Dolan TA. Development of the Geriatric Oral Health Assessment Index. J Dent Educ. 1990;54:680–687. [PubMed] [Google Scholar]
- Baba K, Igarashi Y, Nishiyama A, John MT, Akagawa Y, Ikebe K, Ishigami T, Kobayashi H, Yamashita S. The relationship between missing occlusal units and oral health-related quality of life in patients with shortened dental arches. Int J Prosthodont. 2008;21:72–74. [PubMed] [Google Scholar]
- Baba K, Igarashi Y, Nishiyama A, John MT, Akagawa Y, Ikebe K, Ishigami T, Kobayashi H, Yamashita S. Patterns of missing occlusal units and oral health-related quality of life in SDA patients. J Oral Rehabil. 2008;35:621–628. doi: 10.1111/j.1365-2842.2007.01803.x. [DOI] [PubMed] [Google Scholar]
- Bae KH, Kim HD, Jung SH, Park DY, Kim JB, Paik DI, Chung SC. Validation of the Korean version of the oral health impact profile among the Korean elderly. Community Dent Oral Epidemiol. 2007;35:73–79. doi: 10.1111/j.1600-0528.2007.00331.x. [DOI] [PubMed] [Google Scholar]
- Hassel AJ, Koke U, Schmitter M, Rammelsberg P. Factors associated with oral health-related quality of life in institutionalized elderly. Acta Odontol Scand. 2006;64:9–15. doi: 10.1080/00016350500326211. [DOI] [PubMed] [Google Scholar]
- Kida IA, Astrom AN, Strand GV, Masalu JR, Tsakos G. Psychometric properties and the prevalence, intensity and causes of oral impacts on daily performance (OIDP) in a population of older Tanzanians. Health Qual Life Outcomes. 2006;4:56. doi: 10.1186/1477-7525-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahti S, Suominen-Taipale L, Hausen H. Oral health impacts among adults in Finland: competing effects of age, number of teeth, and removable dentures. Eur J Oral Sci. 2008;116:260–266. doi: 10.1111/j.1600-0722.2008.00540.x. [DOI] [PubMed] [Google Scholar]
- Lawrence HP, Thomson WM, Broadbent JM, Poulton R. Oral health-related quality of life in a birth cohort of 32-year olds. Community Dent Oral Epidemiol. 2008;36:305–316. doi: 10.1111/j.1600-0528.2007.00395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leake JL, Hawkins R, Locker D. Social and functional impact of reduced posterior dental units in older adults. J Oral Rehabil. 1994;21:1–10. doi: 10.1111/j.1365-2842.1994.tb01119.x. [DOI] [PubMed] [Google Scholar]
- Leao A, Sheiham A. Relation between clinical dental status and subjective impacts on daily living. J Dent Res. 1995;74:1408–1413. doi: 10.1177/00220345950740071301. [DOI] [PubMed] [Google Scholar]
- Locker D, Slade G. Association between clinical and subjective indicators of oral health status in an older adult population. Gerodontology. 1994;11:108–114. doi: 10.1111/j.1741-2358.1994.tb00116.x. [DOI] [PubMed] [Google Scholar]
- Mason J, Pearce MS, Walls AW, Parker L, Steele JG. How do factors at different stages of the lifecourse contribute to oral-health-related quality of life in middle age for men and women? J Dent Res. 2006;85:257–261. doi: 10.1177/154405910608500310. [DOI] [PubMed] [Google Scholar]
- McGrath C, Alkhatib MN, Al-Munif M, Bedi R, Zaki AS. Translation and validation of an Arabic version of the UK oral health related quality of life measure (OHQoL-UK) in Syria, Egypt and Saudi Arabia. Community Dent Health. 2003;20:241–245. [PubMed] [Google Scholar]
- McGrath C, Bedi R. Can dentures improve the quality of life of those who have experienced considerable tooth loss? J Dent. 2001;29:243–246. doi: 10.1016/S0300-5712(00)00063-4. [DOI] [PubMed] [Google Scholar]
- McGrath C, Bedi R. An evaluation of a new measure of oral health related quality of life--OHQoL-UK(W) Community Dent Health. 2001;18:138–143. [PubMed] [Google Scholar]
- McGrath C, Bedi R. Population based norming of the UK oral health related quality of life measure (OHQoL-UK) Br Dent J. 2002;193:521–524. doi: 10.1038/sj.bdj.4801616. discussion 517. [DOI] [PubMed] [Google Scholar]
- McGrath C, Bedi R. Why are we "weighting"? An assessment of a self-weighting approach to measuring oral health-related quality of life. Community Dent Oral Epidemiol. 2004;32:19–24. doi: 10.1046/j.0301-5661.2003.00110.x. [DOI] [PubMed] [Google Scholar]
- Meeuwissen JH, van Waas MA, Meeuwissen R, Kayser AF, van 't Hof MA, Kalk W. Satisfaction with reduced dentitions in elderly people. J Oral Rehabil. 1995;22:397–401. doi: 10.1111/j.1365-2842.1995.tb00791.x. [DOI] [PubMed] [Google Scholar]
- Mesas AE, de Andrade SM, Cabrera MA. Factors associated with negative self-perception of oral health among elderly people in a Brazilian community. Gerodontology. 2008;25:49–56. doi: 10.1111/j.1741-2358.2007.00196.x. [DOI] [PubMed] [Google Scholar]
- Naito M, Suzukamo Y, Nakayama T, Hamajima N, Fukuhara S. Linguistic adaptation and validation of the General Oral Health Assessment Index (GOHAI) in an elderly Japanese population. J Public Health Dent. 2006;66:273–275. doi: 10.1111/j.1752-7325.2006.tb04081.x. [DOI] [PubMed] [Google Scholar]
- Oliveira BH, Nadanovsky P. Psychometric properties of the Brazilian version of the Oral Health Impact Profile-short form. Community Dent Oral Epidemiol. 2005;33:307–314. doi: 10.1111/j.1600-0528.2005.00225.x. [DOI] [PubMed] [Google Scholar]
- Pallegedara C, Ekanayake L. Effect of tooth loss and denture status on oral health-related quality of life of older individuals from Sri Lanka. Community Dent Health. 2008;25:196–200. [PubMed] [Google Scholar]
- Sheiham A, Steele JG, Marcenes W, Tsakos G, Finch S, Walls AW. Prevalence of impacts of dental and oral disorders and their effects on eating among older people; a national survey in Great Britain. Community Dent Oral Epidemiol. 2001;29:195–203. doi: 10.1034/j.1600-0528.2001.290305.x. [DOI] [PubMed] [Google Scholar]
- Steele JG, Ayatollahi SM, Walls AW, Murray JJ. Clinical factors related to reported satisfaction with oral function amongst dentate older adults in England. Community Dent Oral Epidemiol. 1997;25:143–149. doi: 10.1111/j.1600-0528.1997.tb00912.x. [DOI] [PubMed] [Google Scholar]
- Steele JG, Sanders AE, Slade GD, Allen PF, Lahti S, Nuttall N, Spencer AJ. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two national samples. Community Dent Oral Epidemiol. 2004;32:107–114. doi: 10.1111/j.0301-5661.2004.00131.x. [DOI] [PubMed] [Google Scholar]
- Swoboda J, Kiyak HA, Persson RE, Persson GR, Yamaguchi DK, MacEntee MI, Wyatt CC. Predictors of oral health quality of life in older adults. Spec Care Dentist. 2006;26:137–144. doi: 10.1111/j.1754-4505.2006.tb01714.x. [DOI] [PubMed] [Google Scholar]
- Tsakos G, Marcenes W, Sheiham A. The relationship between clinical dental status and oral impacts in an elderly population. Oral Health Prev Dent. 2004;2:211–220. [PubMed] [Google Scholar]
- Tubert-Jeannin S, Riordan PJ, Morel-Papernot A, Porcheray S, Saby-Collet S. Validation of an oral health quality of life index (GOHAI) in France. Community Dent Oral Epidemiol. 2003;31:275–284. doi: 10.1034/j.1600-0528.2003.t01-1-00006.x. [DOI] [PubMed] [Google Scholar]
- Tubert-Jeannin S, Riordan PJ, Morel-Papernot A, Roland M. Dental status and oral health quality of life in economically disadvantaged French adults. Spec Care Dentist. 2004;24:264–269. doi: 10.1111/j.1754-4505.2004.tb01704.x. [DOI] [PubMed] [Google Scholar]
- Walter MH, Woronuk JI, Tan HK, Lenz U, Koch R, Boening KW, Pinchbeck YJ. Oral health related quality of life and its association with sociodemographic and clinical findings in 3 northern outreach clinics. J Can Dent Assoc. 2007;73:153. [PubMed] [Google Scholar]
- Wong MC, McMillan AS. Tooth loss, denture wearing and oral health-related quality of life in elderly Chinese people. Community Dent Health. 2005;22:156–161. [PubMed] [Google Scholar]
- Cronin M, Meaney S, Jepson NJ, Allen PF. A qualitative study of trends in patient preferences for the management of the partially dentate state. Gerodontology. 2009;26:137–142. doi: 10.1111/j.1741-2358.2008.00239.x. [DOI] [PubMed] [Google Scholar]
- Locker D. Applications of self-reported assessments of oral health outcomes. J Dent Educ. 1996;60:494–500. [PubMed] [Google Scholar]
- Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2:1–74. i-iv. [PubMed] [Google Scholar]
- Allen PF, Thomason JM, Jepson NJ, Nohl F, Smith DG, Ellis J. A randomized controlled trial of implant-retained mandibular overdentures. J Dent Res. 2006;85:547–551. doi: 10.1177/154405910608500613. [DOI] [PubMed] [Google Scholar]
- Nguyen TC, Witter DJ, Bronkhorst EM, Pham L, Creugers N. Dental functional status in a Southern Vietnamese adult population - an analysis by a combined quantitative and qualitative classification system. Int J Prosthodont, in press. [PubMed]
- Gotfredsen K, Walls AW. What dentition assures oral function? Clin Oral Implants Res. 2007;18(Suppl 3):34–45. doi: 10.1111/j.1600-0501.2007.01436.x. [DOI] [PubMed] [Google Scholar]
- Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33:81–92. doi: 10.1111/j.1600-0528.2004.00219.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Summary of primary and additional outcomes of all included studies
Summary of data of all included studies and feasibility for meta-analysis.