Abstract
Background
The development of infectious complications after high volume elective surgical procedures imposes a significant clinical burden to the United States population. This study evaluated the association of in-hospital delay of elective procedures and the subsequent impact on infectious complications after coronary artery bypass graft (CABG) surgery, colon resection, and lung resection.
Study Design
The Nationwide Inpatient Sample was queried between 2003–2007 and patients that developed postoperative infectious complications were identified. Time to elective surgery in days from admission was calculated: 0, 1 day, 2–5 days, and 6–10 days. Infectious complications evaluated included pneumonia (PNA), urinary tract infections (UTI), postoperative sepsis, and surgical site infections (SSI). Chi square, multivariable logistic regression analyses, analysis of variance and Cochran-Armitage trend test were utilized.
Results
87,318 CABG procedures, 46,728 colon resections, and 28,960 lung resections were evaluated. Total infection rates significantly increased after elective surgery delays: CABG: 0=5.73%;1=6.68%;2–5=9.33%;6–10=18.24%; Colon Resections:0=8.43 %;1=11.86%;2–5=15.79%;6–10=21.62%; and Lung Resections: 0=10.17%;1=14.53%;2–5=15.53%;6–10=20.56%, p<.0001 for all trends. Trends for increasing infections after delay were significant for PNA and sepsis for all procedures (P<0.0001); UTI and SSI significantly increased after CABG and colon resection. Age 80 years and above, female gender, Black and Hispanic race/ethnicity and comorbidities including congestive heart failure, chronic pulmonary disease and renal failure were associated with delay in surgery. Postoperative hospital mortality after delayed procedures was also greater. Mean cost increased after all procedures with delays: CABG: $36,079 vs. $47,527 (p<.0001), Colon Resections: $20,265 vs. $29,887 (p<.0001), and Lung Resections: $26,323 vs. $30,571 (p=0.0032).
Conclusions
In-hospital delay of elective surgery from the day of admission was associated with a significant increase in infectious complications and mortality. This delay was also associated with a significant increase in hospital cost and utilization. Future policy directed toward preventing in-hospital delay of elective surgery may offer significant cost savings and decrease infectious complications after elective surgery.
Introduction
Infectious complications have a substantial impact on the cost and outcomes for patients after elective surgery.1–2 It has been suggested that infection after surgery continues to be a major source of morbidity and expense despite extensive efforts with educational programs, guidelines, and hospital-based policies and procedures.3 Population analysis of key high-volume index cases allows for the evaluation of these procedures with respect to in-hospital delay of these procedures and allows for the analysis of in-hospital delay on infectious outcomes. Previous studies have suggested that nosocomial infections after elective surgery significantly increased hospital length of stay and reported total hospital cost. 2 A systematic analysis of infectious complications is essential in understanding preventable causes for morbidity and creating management strategies to reduce cost and improve outcomes for elective surgical procedures. Furthermore, as pay for performance becomes more germane, the evaluation of process level opportunities for improvement to reduce infectious complications will become paramount.4
Population analysis represents an ideal methodology for the evaluation of large numbers of index procedures to evaluate factors which may impact infection complications. Little population level data exists evaluating the iatrogenic complication of in-hospital delay prior to elective surgery. The objective of this study was to evaluate the association of in-hospital delay of elective surgical procedures on the rate of infectious complications. Secondary aim of this analysis was to evaluate the association between in-hospital delay of elective surgical procedures and total hospital cost.
Methods
Data Sources
Data for analysis were collected from the HCUP (Healthcare Cost and Utilization Project) Nationwide Inpatient Sample (NIS) for the years 2003–2007. Being the largest publicly available all-payer inpatient care database in the United States and sponsored by the Agency for Healthcare Research and Quality (AHRQ), it contains all inpatient stay records from approximately 20 percent of the U.S. community short-stay hospitals. The most current available 2007 dataset covers 40 states, 1,044 hospitals, and includes more than 8 million observations with 251 data elements. One of these data elements provides information regarding the number of days from hospital admission to principal and all secondary procedures allowing for the identification of a delay of surgical procedure.
Starting the year 2002, the NIS data contains AHRQ comorbidity measures which evaluate comorbid diseases in observed patients. First reported by Elixhauser et al.,5 they are widely used in epidemiological studies with administrative data for risk-adjusted outcome measurement. To perform risk adjustment in our study, we used the following comorbid measures: congestive heart failure, hypertension, chronic pulmonary disease, pulmonary circulation disorders, diabetes, renal failure, solid tumor without metastasis, metastatic cancer, and obesity.
Study population
The study cohort consisted of patients 40 years and older undergoing one of three high volume elective major surgical procedures: coronary artery bypass graft (CABG), lung resection, or colon resection. Patients undergoing CABG were selected with the ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) codes 36.10–36.19 for principal procedure. Patients with open lung resections were identified with the ICD-9-CM codes 162.2–162.9 for principal diagnosis and 32.3, 32.39, 32.4, 32.49 and 32.5, 32.59 for principal procedure. Criteria for selection of patients with open colon resections were ICD-9-CM codes 153.0–153.9 and 154.0–154.8 for principal diagnosis and 45.71–45.79, 45.8 and 48.5 for principal procedure.
To identify postoperative infection, we utilized the following ICD-9-CM diagnosis codes for the secondary diagnoses: 480.x, 481, 482.xx, 483.x, 484.x, 485, 486, 997.31 and 997.39 - for pneumonia; 038.xx, 785.52, 995.91, 995.92, 996.61, 996.62, 998.0, and 999.3x – for sepsis and bloodstream infection; 599.0 and 996.64 – for UTI (urinary tract infection); 998.31, 998.32, 998.5x and 998.83 – for SSI (surgical site infection).
Based on the number of days from hospital admission to procedure performed (time delay to surgery) we categorized all study population in four groups: 0 (same day as admission), 1 day, 2–5 days and 6–10 days. Patients with time delay to surgery more than 10 days represented less than 1 percent of all cases and they were excluded from analysis.
Statistical analysis
All data analysis was performed with SAS 9.2 statistical software (SAS Institute, Cary, NC). Crude rates of infectious complications for each surgical procedure were computed by dividing the number of cases with these complications by the total number of cases with this procedure and multiplying the result by 100 to express as a percentage. With the HCUP Cost-to-Charge ratio files we transformed hospital charges in the NIS data into hospital cost. To evaluate differences between groups, chi-square analysis was used for categorical variables and Student’s t-test for continuous variables. For comparison of the continuous variable “cost” an analysis of variance was utilized. Given the unbalanced design of the data, we used SAS PROC GLM (general linear model) procedure.6 Multivariable stepwise logistic regression analysis with adjustment by age, gender, race, type of surgical procedure, time delay to surgery, and selected comorbidities was employed to identify independent risk factors for postoperative infectious complications and preoperative factors of surgery delay, and to compare hospital mortality after each surgical procedure in association with the time delay to surgery. Results of this analysis were reported as adjusted OR (odds ratio) with 95% CI (confidence interval). To analyze trends of infection rates with increasing time delay to surgery we utilized the Cochran-Armitage trend test.6 The difference between any results were considered statistically significant if the 95% confidence intervals in compared groups were not overlapped or two-sided p-values were <0.05.
Results
A total of 163,006 patients with surgical procedures of interest were identified in the data; patient demographics are displayed in Table 1. Greater than half of these patients (53.6%) underwent CABG, more than a quarter (28.6%) underwent colon resection, and 17.8% had lung resections performed. Approximately three-quarters of study population (73.8%) were at age 60 years and above. Males predominated over females (P<0.0002), and among patients with identified race whites were majority.
Table 1.
Characteristics of the research cohort
| Characteristic | # of cases | % in the group |
|---|---|---|
| Age: | ||
| 40–49 | 10,243 | 6.3 |
| 50–59 | 32,400 | 19.9 |
| 60–69 | 50,586 | 31.0 |
| 70–79 | 50,394 | 30.9 |
| 80+ | 19,383 | 11.9 |
| Gender: | ||
| Males | 102,043 | 62.6* |
| Females | 60,939 | 37.4* |
| Missing | 24 | |
| Race: | ||
| Whites | 108,489 | 84.3* |
| Blacks | 8,379 | 6.5* |
| Hispanics | 6,752 | 5.2* |
| Other | 5,135 | 4.0* |
| Missing | 34,251 | |
| Surgical procedure: | ||
| CABG | 87,318 | 53.6 |
| Colon resection | 46,728 | 28.6 |
| Lung resection | 28,960 | 17.8 |
| TOTAL | 163,006 | 100 |
among observations without missing values
The results in Table 2 show that the majority of patients undergoing lung resection (94.4%) were operated on the same day they were admitted. Almost four-fifths of patients undergoing colon resection (79.2%) were operated on the day of admission. Of the patients undergoing CABG, only 53.0% of population had surgery performed on the day of admission.
Table 2.
Frequency distribution of patients with different surgical procedures and various time delay to surgery
| Type of surgery | Days after admission to surgery |
|||
|---|---|---|---|---|
| 0 | 1 | 2–5 | 6–10 | |
| CABG | 46,244 (53.0%) | 20,099 (23.0%) | 18,239 (20.9%) | 2,736 (3.1%) |
| Colon resection | 37,009 (79.2%) | 5,843 (12.5%) | 3,039 (6.5%) | 837 (1.8%) |
| Lung resection | 27,347 (94.4%) | 826 (2.9%) | 573 (2.0%) | 214 (0.7%) |
percentage represents proportion within group with indicated type of surgery
When surgery occurred on the day of admission, the greatest rate of infectious complications (10.2%) occurred in patients after lung resection. These patients were 1.23 times (95% CI = 1.17–1.30) as likely as patients with colon resection to develop secondary infection. As well, patients after colon resection were 1.51 times (95%CI = 1.43–1.59) as likely as patients after CABG to have any infectious complication when surgery occurred on the day of admission.
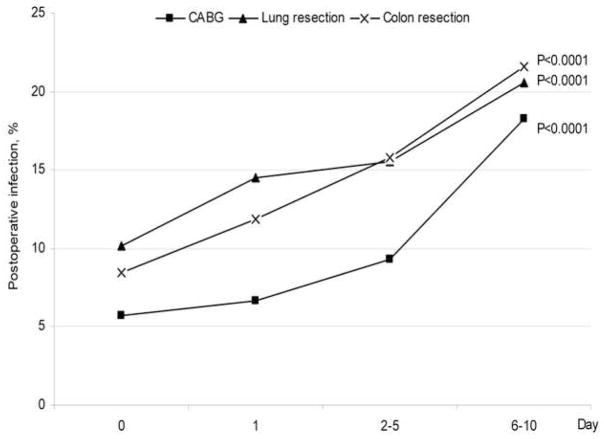
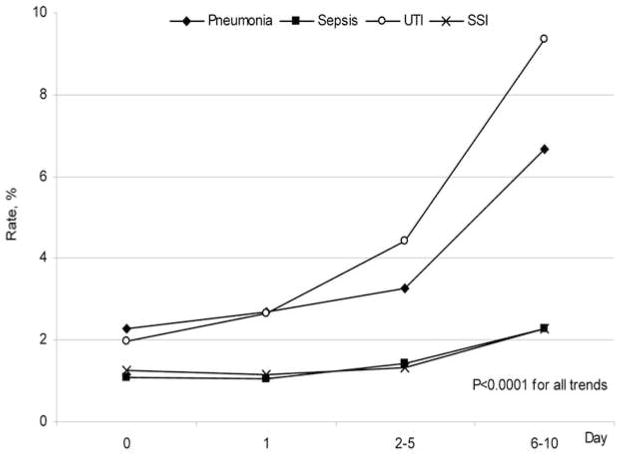
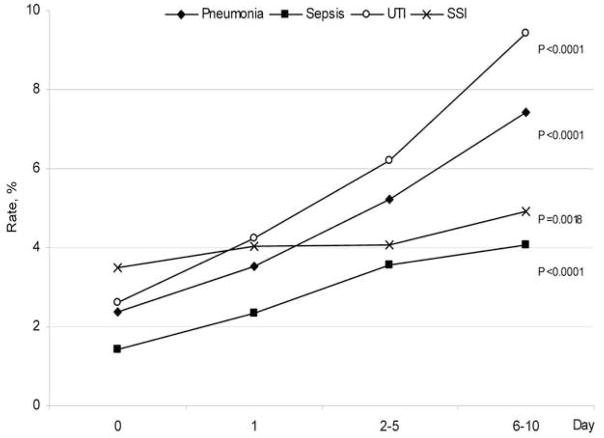
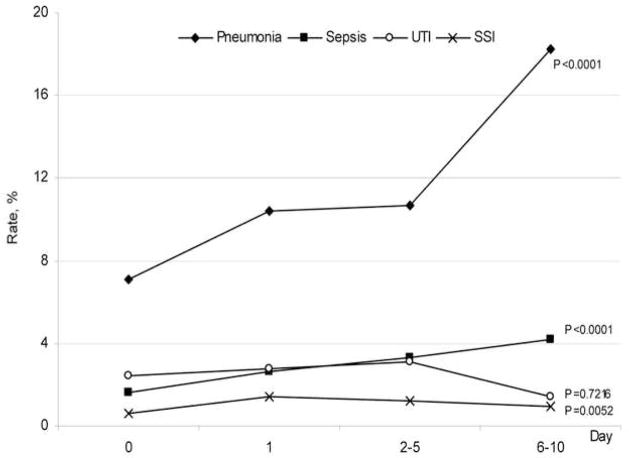
Delay in surgical procedure significantly increased the risk of developing postoperative infection (Fig. 1). Total infection rate after CABG increased from 5.7% when the procedure was performed on the day of admission to 18.2% if the procedure were delayed to 6–10 days. Similar increases were noted after colon resection (from 8.4% to 21.6%) and after lung resection (from 10.2% to 20.6%; P<0.0001 for all trends). Figures 2–4 demonstrates specific post-operative infectious complications associated with each procedure at the time points evaluated in this analysis. Patients undergoing elective CABG or colon procedures had significant increases in the rates of all infectious complications evaluated. For CABG and colon, the greatest increased rates of infections associated with delay were UTI and pneumonia. Lung resections demonstrated significantly increased trends in rates of sepsis and pneumonia associated with delay.
Fig 1.
Rates of all infections after CABG, lung and colon resection when procedure was delayed after hospital admission
Fig. 2.
Rates of specific infections after CABG when procedure was delayed after hospital admission
Fig. 4.
Rates of specific infections after colon resection when procedure was delayed after hospital admission
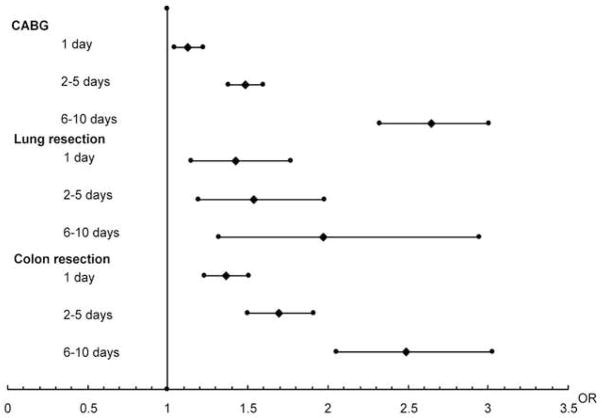
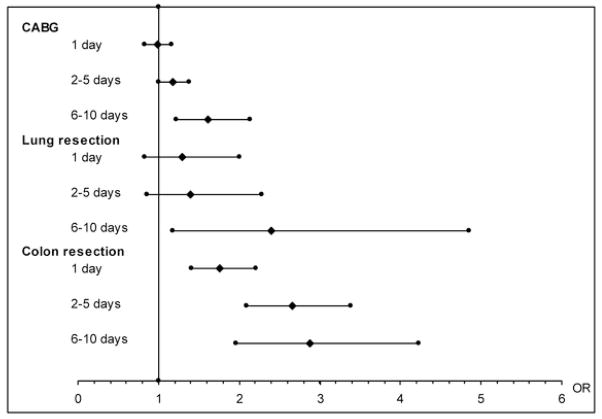
To adjust for age, gender, race and comorbidities, a logistic regression model with infection as an outcome and the above mentioned confounders as independent predictors was created. Fig. 5 displays the odds ratios with 95% confidence intervals of developing postoperative infection after delayed procedures compared to procedures performed at the admission day. After adjustment for age, gender, race and comorbidities, the overall risk of developing infectious complications increased significantly when surgery was delayed. The strongest association between risk of postoperative infection and time delay to surgery was found after CABG. In patients who had colon or lung resection such differences between two adjacent day groups remained significant compared to admission day.
Fig 5.
Odds ratio of having postoperative infection when procedure was delayed compared to procedure at the day of admission
Using a similar model with death as the hospital as the outcome, we evaluated hospital mortality after each procedure in association with time delay to surgery. As displayed in Fig. 6, hospital mortality after delay for colon resection was significantly greater for any period of delay encountered. For CABG and lung resections, mortality was significantly greater when these procedures were postponed greater than 5 days.
Figure 6.
Odds ratio of hospital mortality when procedure was delayed compared to procedure at the day of admission.
We also evaluated the association of patient factors (age, gender, race, and comorbidities) with the development of in-hospital delay (Table 3). Octogenarians and women were more likely to undergo delayed CABG or colon resections compared to younger patients. As well, Blacks and Hispanics were mole likely compared to Whites to experience delay in all procedures evaluated. Comorbidities that were more frequently associated with delay were congestive heart failure, chronic pulmonary disease and renal failure.
Table 3.
Preoperative factors of surgery delay
| Parameters | Surgical procedures |
||
|---|---|---|---|
| CABG | Lung resection | Colon resection | |
| Age: | |||
| 80+ | 1.26 (1.16–1.37) | NS | 2.24 (1.97–2.54) |
| Gender: | |||
| Female | 1.24 (1.19–1.28) | 0.84 (0.75–0.94) | 1.11 (1.05–1.17) |
| Race/Ethnicity: | |||
| Black | 1.13 (1.05–1.21) | 1.47 (1.20–1.81) | 1.37 (1.26–1.49) |
| Hispanic | 1.69 (1.58–1.80) | 1.73 (1.30–2,29) | 1.37 (1.22–1.54) |
| Comorbidities: | |||
| Congestive heart failure | NS | 1.40 (1.12–1.75) | 1.85 (1.69–2.02) |
| Chronic pulmonary disease | 1.13 (1.09–1.18) | 1.21 (1.08–1.36) | 1.16 (1.08–1.24) |
| Renal failure | 1.40 (1.31–1.50) | 1.49 (1.10–2.03) | 1.40 (1.21–1.63) |
References: Age: 40–49 years; Gender: male; Race: White. NS: results non significant. Odds ratios with 95% confidence intervals.
The total hospital cost of procedures with various time delays to surgery was evaluated. The significance was tested utilizing trend analysis across the increase in time delay to surgery. The results are displayed in Table 4. For each surgical procedure delay in surgery from time of admission significantly increased total hospital cost and this increase was greater if delay was longer.
Table 4.
Total hospital cost ($$, mean ± standard deviation) in different surgical groups with various time delay to surgery
| Time delay to surgery, days | Surgical procedure |
||
|---|---|---|---|
| CABG | Colon resection | Lung resection | |
| 0 | 25,164 ± 16,777 | 13,660 ± 12,268 | 18,519 ± 16,662 |
| 1 | 28,962 ± 17,439 | 17,431 ± 17,387 | 22,169 ± 21,869 |
| 2–5 | 38,873 ± 19,163 | 21,018 ± 16,182 | 22,696 ± 17,922 |
| 6–10 | 42,055 ± 24,779 | 25,307 ± 19,869 | 25,054 ± 16,049 |
| P for trend | < 0.0001 | < 0.0001 | < 0.0001 |
Discussion
This analysis has demonstrated that patients, after adjustment for age, gender, race and comorbidities, had increased infectious complications after in-hospital delay for all elective high volume procedures evaluated. An in-hospital delay of as few as two days is associated with increase infectious complications, particularly of pneumonia and UTI for elective CABG. For elective thoracic procedures, pneumonia was seen to dramatically increase if patients were delayed greater than six days. Factors associated with in-hospital delay included advanced age, female gender, minority status, and comorbidities including congestive heart failure, chronic pulmonary disease and renal failure. The development of complications may be multifactorial, yet in-hospital delay was significantly associated with the development of infectious complications and increased hospital resource utilization.
The concept that surgical infections are increased with in-hospital delay has been described, yet few population level data exist. 1, 7–8 It has been reported from single center series that increased overall length of stay in the postoperative period is associated with increased nosocomial infections. Cruse et al. described that advanced age of the patient, prolonged preoperative hospitalization, and long operations were associated with an increase in the rate of infection of surgical wounds.7 Saez-Castillo et al. also demonstrated utilizing an asymmetric logit that length of stay, the existence of a preoperative stay, and obesity were the main risk factors for a nosocomial infections.1 As well, a single center study performed almost two decades ago evaluated 449 patients undergoing a variety of surgical procedures. They suggested that lengthening the preoperative stay may increase wound infections and they found the strongest association between preoperative stay and nosocomial infection.8
Multiple authors have elucidated the significant cost of infection and that health care-associated infections impose substantial clinical and economic costs.9–10 This analysis has demonstrated that for all index procedures evaluated, delay was associated with significant cost increases. These increased costs were greater than would be expected from the increased room charges alone. Sparling et al. used a matched cohort design to compare costs and demonstrated that length of stay was increased by 10.6 days and costs were increased by $27,288 for each patient with a potentially preventable surgical site infection.10 Healthcare-associated infections also have a relevant socioeconomic impact. In a European study, the overall estimated yearly costs vary between 3.5 billion Euros in the United States to 1.3 billion Euros in England. Surgical site and bloodstream infections were found to be the most costly types of infections, followed by lower respiratory tract and urinary tract infections.11
Suggested methods to prevent these complications have been compliance to best practices and structural process of care within hospitals. 12–16 Fry et al. has stated that infection after surgery continues to be a major source of morbidity and expense despite efforts with educational programs, guidelines, and hospital-based policies and procedures. This study concluded that the adoption of a culture dedicated to quality control through better information technology and data-driven initiatives to achieve improved clinical outcomes from infectious complications in surgery.3 From this analysis, only 53% of elective CABG procedures were performed on the day of admission. It is plausible that future data driven methodologies implementing guidelines to decrease in-hospital delay prior to elective procedures may improve outcomes and may decrease overall rates of infection.
This study has several limitations. Administrative data originally were intended primarily for reimbursement, although validation of the use of administrative data for research purposes has been performed.17–18 In addition, the potential for inclusion bias based on limited coding schemes for the many clinical entities cannot be entirely excluded. Due to the large number of hospitals reporting data and the even larger number of coders entering data it is difficult to account for potential coding errors. As well, the NIS does not include patients in military hospitals or VA medical centers. It has been suggested that length of preoperative stay is a surrogate for severity of illness and co-morbid conditions19, although this was adjusted for in the analysis. As well, the use of coding present-on-admission coding would be useful to discern procedures occurring before elective surgeries, but these codes are not currently available. Furthermore, this study contains only elective procedures and no information regarding infections present on admission is available, yet there is the possibility that elective admissions developed an emergency procedure during their hospitalization and this cannot be discerned from the current dataset. The use of smaller cohorts may offer further refined clinical information regarding infectious complications, although these data are generalizable to the nation and offer insight into national rates of infectious complications after in-hospital delay of elective index surgeries.
In conclusion, this analysis has shown on a population level that in-hospital delay is significantly associated with a negative impact on patients with regard to infectious complications and mortality. The rates of all nosocomial infections after CABG, lung and colon resection increased significantly when a procedure encountered in-hospital delay after admission. In-hospital delay before elective surgery evokes a significant increase in infectious complications for high volume cases and subsequently adds significantly to the cost of healthcare. After adjustment for age, gender, race and comorbidities a delay of as little as one day increased rates of infection for all index cases evaluated, and this association had greater impact as the delay continued. Future systems approaches to decreasing in-hospital delay are warranted and would likely reduce infection while also reducing total hospital utilization.
Fig. 3.
Rates of specific infections after lung resection when procedure was delayed after hospital admission
Acknowledgments
The authors would like to thank Donald E Fry, MD for his critical review of the manuscript and helpful comments.
Footnotes
Disclosure Information: Nothing to disclose.
Presented at the Annual Meeting of the Surgical Infection Society, Las Vegas, NV, April, 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Saez-Castillo AJ, Olmo-Jimenez MJ, Perez Sanchez JM, et al. Bayesian Analysis of Nosocomial Infection Risk and Length of Stay in a Department of General and Digestive Surgery. Value Health. 2010 doi: 10.1111/j.1524-4733.2009.00680.x. [DOI] [PubMed] [Google Scholar]
- 2.Vogel TR, Dombrovskiy VY, Carson JL, et al. Infectious complications after elective vascular surgical procedures. J Vasc Surg. 2010;51:122–9. doi: 10.1016/j.jvs.2009.08.006. discussion 129–130. [DOI] [PubMed] [Google Scholar]
- 3.Fry DE. A systems approach to the prevention of surgical infections. Surg Clin North Am. 2009;89:521–537. x. doi: 10.1016/j.suc.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 5.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Cody RP, Smith JK. Applied statistics and the SAS programming language. 5. Upper Saddle River, N.J: Pearson Prentice Hall; 2006. [Google Scholar]
- 7.Cruse P. Wound infection surveillance. Rev Infect Dis. 1981;3:734–737. doi: 10.1093/clinids/3.4.734. [DOI] [PubMed] [Google Scholar]
- 8.Bueno Cavanillas A, Rodriguez-Contreras R, Delgado Rodriguez M, et al. Preoperative stay as a risk factor for nosocomial infection. Eur J Epidemiol. 1991;7:670–676. doi: 10.1007/BF00218680. [DOI] [PubMed] [Google Scholar]
- 9.Daschner F. Cost-effectiveness in hospital infection control--lessons for the 1990s. J Hosp Infect. 1989;13:325–336. doi: 10.1016/0195-6701(89)90052-2. [DOI] [PubMed] [Google Scholar]
- 10.Sparling KW, Ryckman FC, Schoettker PJ, et al. Financial impact of failing to prevent surgical site infections. Qual Manag Health Care. 2007;16:219–225. doi: 10.1097/01.QMH.0000281058.99929.ea. [DOI] [PubMed] [Google Scholar]
- 11.Agozzino E, Di Palma MA, Gimigliano A, Piro A. Economic impact of healthcare-associated infections. Ig Sanita Pubbl. 2008;64:655–670. [PubMed] [Google Scholar]
- 12.Humphreys H. Preventing surgical site infection. Where now? J Hosp Infect. 2009;73:316–322. doi: 10.1016/j.jhin.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 13.Travis J, Carr JB, Saylor D, et al. Coronary artery bypass graft surgery: surgical site infection prevention. J Healthc Qual. 2009;31:16–23. doi: 10.1111/j.1945-1474.2009.00033.x. [DOI] [PubMed] [Google Scholar]
- 14.Mawji Z, Stillman P, Laskowski R, et al. First do no harm: integrating patient safety and quality improvement. Jt Comm J Qual Improv. 2002;28:373–386. doi: 10.1016/s1070-3241(02)28037-2. [DOI] [PubMed] [Google Scholar]
- 15.Griffin FA. Best-practice protocols: Preventing surgical site infection. Nurs Manage. 2005;36:20, 2–6. doi: 10.1097/00006247-200511000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Campbell DA, Jr, Henderson WG, Englesbe MJ, et al. Surgical site infection prevention: the importance of operative duration and blood transfusion--results of the first American College of Surgeons-National Surgical Quality Improvement Program Best Practices Initiative. J Am Coll Surg. 2008;207:810–80. doi: 10.1016/j.jamcollsurg.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 17.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–16. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 18.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–15. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 19.Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–258. doi: 10.1086/501620. quiz 259–280. [DOI] [PubMed] [Google Scholar]