Abstract
Background Before 2003, little was known about the scale of China’s HIV/AIDS epidemic. In 2003, the Chinese government produced national estimates with support from the Joint United Nations Programme on HIV/AIDS, the World Health Organization and the United States Centers for Disease Control and Prevention. Subsequent national estimation exercises were carried out in 2005, 2007 and 2009. We describe these estimation processes and present the results of China’s HIV/AIDS estimation exercises from 2003 to 2009.
Methods The Workbook Method was used to generate national HIV/AIDS estimates. Data from the provincial level were used in 2003, data from the prefecture level were used in 2005 and data from the county level were used in 2007 and 2009. Data at the lowest level of aggregation were used to estimate risk group population size and HIV prevalence. Data from lower levels were combined into national estimates.
Results At the end of 2003, 2005, 2007 and 2009, there were an estimated 0.84, 0.65, 0.70 and 0.74 million people living with HIV/AIDS in China, respectively, with an overall HIV prevalence of 0.05–0.06%. The number of new HIV infections decreased from 70 000 in 2005, to 50 000 in 2007, to 48 000 in 2009. Data quality improvements have increased the precision of China’s HIV estimates.
Conclusion Repeated estimates have improved understanding of the HIV/AIDS epidemic in China. HIV estimates are a valuable tool for guiding national AIDS policies evaluating HIV prevention and control programmes.
Keywords: HIV/AIDS, estimation, Workbook, epidemiologic methods, China
Introduction
How serious is China’s HIV epidemic? This question has generated significant speculation and debate over the past decade. In the 1990s, when HIV began to spread quickly throughout China, little was known about the epidemic. The few data that were available suggested alarming increases in HIV prevalence among drug users (DUs)1,2 and plasma donors.3 In 2002, the United Nations Theme Group on HIV/AIDS in China issued a controversial report citing an estimated 1 million people living with HIV/AIDS (PLWHA) in China in 2001, with a projected 10 million infections by 2010 if countermeasures were not taken.4 Official sources at the time estimated that the number of HIV cases had risen from 300 000 in 1997 to 1 million in 2002.5 China’s HIV epidemic appeared to be escalating out of control, but without good data, it was hard to gauge the true scope of the epidemic.
Beginning in 2003, the Chinese government began conducting systematic, biennial HIV/AIDS estimation exercises to assess the HIV epidemic at the national level. Working together with the Joint United Nations Programme on HIV/AIDS (UNAIDS), the World Health Organization (WHO) and the United States Centers for Disease Control and Prevention (US CDC), the Chinese government estimated that there were 840 000 PLWHA by the end of 2003, among whom 80 000 had developed AIDS.5 This estimation exercise revealed a number of data gaps: limited or absent data at the county level, a small number of epidemiological studies of HIV and sexually transmitted infections (STIs) and limited surveillance data from sites in high-prevalence areas.6 Because of the limited data available in 2003, estimates were prepared at the provincial level (the word ‘province’ in this article refers to all provinces, autonomous regions and municipalities including the Xingjiang Production and Construction Corps), making the precision. Since 2003, the Chinese government has taken measures to improve data availability and data quality. First, the government has expanded the HIV sentinel surveillance system from 148 sites in 2003 to 1029 sites in 2009.6,7 This has expanded geographic coverage and coverage of specific risk groups. For example, 25 surveillance sites assessed HIV trends among men who have sex with men (MSM) in 2009, compared with just 1 site in 2003 and 2005. Secondly, the government has established and expanded the HIV behavioural surveillance system, which provides essential data on risk behaviours in various subpopulations. Thirdly, the government has strengthened the HIV/AIDS case reporting system, including improving laboratory services to support HIV screening and confirmation testing. Finally, the government has conducted a number of special studies, including large-scale HIV screening among former plasma donors in central China.8
As more and more data have become available, China’s HIV/AIDS estimates have become increasingly reliable. In 2005, 2007 and 2009, China conducted three more rounds of HIV/AIDS estimation exercises using the Workbook Method recommended by the WHO and the UNAIDS.9–13 Here, we describe these estimation processes, review the results of these estimation exercises and outline the challenges ahead.
Methods
The estimation process
China’s national HIV estimates have been generated through consultative processes involving key stakeholders. In 2005, the National HIV Epidemic Estimation Working Group was formed to support national HIV/AIDS estimation processes.10 The working group includes domestic experts from the Ministry of Health (MOH) Expert Advisory Committee on HIV/AIDS; the National Center of AIDS/STD Control and Prevention (NCAIDS) within the Chinese Center for Disease Control and Prevention (China CDC); Peking University; Tsinghua University; Fudan University; Peking Union Medical College; Renmin University; and other universities and organizations. The group also includes international experts from the WHO, the UNAIDS, the US CDC and other organizations. Over the course of the estimation processes in 2005, 2007 and 2009,9–11 the group met to review estimation guidelines, to train key provincial level staff, to provide technical support and to oversee estimation analyses.
National guidelines have been established to guide the estimation process. In 2005, NCAIDS staff drafted guidelines to ensure comparability of data across geographical areas, along with an implementation manual.13 The guidelines and implementation manual were pilot tested in one province before being applied nationwide. In 2007, the guidelines and implementation manual were updated to reflect parameter adjustments, standardization of terms and definitions and rules for borrowing estimates across geographical areas in places where data were not available.14,15
Using national guidelines, provinces prepared draft HIV/AIDS estimates. In 2005, provincial estimates were based on prefecture-level Workbook spreadsheets. In 2007 and 2009, when more data were available, county-level Workbook spreadsheets were prepared. In 2005, 2007 and 2009, province-level Workbook spreadsheets were reviewed by regional working groups formed from the National HIV Epidemic Estimation Working Group. After these were reviewed, each provincial health bureau (or health department) and CDC jointly finalized the provincial estimates. NCAIDS staff then prepared national estimates with support from the National HIV Epidemic Estimation Working Group. The national estimates in 2005, 2007 and 2009 were reviewed by representatives from the UNAIDS and the WHO Geneva headquarters, and suggested adjustments were incorporated into the final national estimates.
Prior to each estimation exercise, staff at each level were trained on how to produce HIV estimates using the Workbook Method. At the beginning of the process, senior technical staff from the national and provincial levels attended a training workshop organized by the UNAIDS and the WHO in Bangkok, Thailand. After senior technical staff received the training, a national training workshop was organized with consultants hired by the UNAIDS, and provincial training workshops were organized in each province. By 2009, nearly 75% of the staff workers had already participated in at least one of the previous estimation exercises.
Data sources
Demographic data
Demographic data came primarily from publicly available census data in the previous 2 years, i.e. 2001, 2003, 2005 and 2007, from the National Bureau of Statistics of China, and adjusted by the number of annual reported births and deaths from national health statistics.
HIV prevalence data
HIV prevalence data came primarily from China’s HIV sentinel surveillance system. When possible, data from the previous 12 months were used. When recent data were not available, adjustments were made to previous data as considered necessary by local CDC officials.
To generate HIV estimates for high-risk populations, sentinel surveillance data, behavioural surveillance survey (BSS) data, special epidemiological survey data, public security bureau (PSB) registration data and data from the published literature were used. Between 2003 and 2009, the number of HIV sentinel surveillance sites has grown (Table 1). Coverage of specific populations, such as MSM, has greatly improved (from 1 site in 2003 and 2005 to 25 sites in 2009).
Table 1.
Number of national HIV sentinel surveillance sites that contributed data to China’s national HIV estimates, 2003–09
| Population | 2003 | 2005 | 2007 | 2009 |
|---|---|---|---|---|
| Female SWs | 32 | 49 | 229 | 367 |
| DUs/IDUs | 36 | 62 | 229 | 243 |
| MSM | 1 | 1 | 11 | 25 |
| STD outpatients | 58 | 90 | 267 | 231 |
| Pregnant women | 13 | 26 | 75 | 66 |
| Truck drivers | 8 | 20 | 43 | 46 |
| Othera | – | – | 75 | 51 |
| Total | 148 | 248 | 929 | 1029 |
aOther includes students and tuberculosis patients.
SWs: sex workers, STD: sexually transmitted disease.
To generate HIV estimates for low-risk populations (e.g. the regular sex partners of high-risk individuals), different data sources were used depending on whether an area qualified as a low or high HIV prevalence area (<1 vs >1% antenatal HIV prevalence, respectively). The majority of areas fell into the low-prevalence category. In these places, HIV serodiscordant couple survey data from Xinjiang and Henan provinces were used as a proxy for HIV prevalence among the regular sex partners of high-risk individuals. For high-prevalence areas, antenatal clinic data were used as a proxy for HIV prevalence among the regular sex partners of high-risk individuals.
Population size estimates
High and low estimates were made for the sizes of high-risk populations. As recommended by international guidelines, most population size estimates used indirect multiplier methods.16 To estimate the population size of regular partners of high-risk individuals, data from two sources were collected: (i) proportion of high-risk population such as MSM that engage in heterosexual relationships; and (ii) proportion of HIV-infected plasma blood donors who were married.
Data for population size estimates came primarily from field investigations, behavioural surveillance and registration records from various government agencies, such as the Public Security Bureau. Hospital testing and case reports were also taken into consideration. Data sources and population size estimation methods for the 2005 and 2007 estimation exercises have been described elsewhere.14,17
Missing data
Missing HIV prevalence and population size data for specific areas were imputed using data from areas with similar geographic and socio-economic characteristics. Decisions on how to impute data were made in consultation with experts from the National HIV Epidemic Estimation Working Group and local health officials.
Data quality
In 2007, at the suggestion of the UNAIDS, NCAIDS staff conducted systematic evaluations of data quality, verifying results against other estimation methods.14 Data quality were also assessed in 2009.11
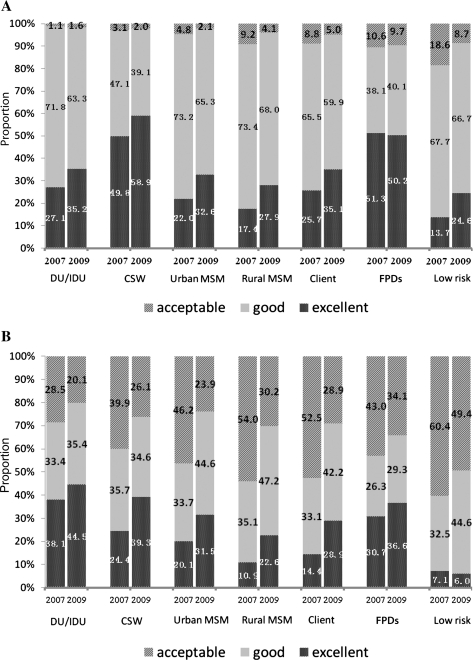
A system for scoring data quality was established in the 2007 National HIV/AIDS Estimation Technical Guidelines.15 In rating the quality of HIV prevalence data, points were given for the following categories: sample quality and sample size (10 points); sampling method (4 points); all subjects belongs to designated specific sentinel group (1 point). A maximum of 17 points was possible; over 13 points was ‘excellent’, 7–12 points was ‘good’ and 0–6 was ‘acceptable’ . If data were not readily available, data from another province or population of a similar HIV/AIDS epidemic situation was used. In these cases, a score of 3 points was given. In rating the quality of population size estimates, points were given as follows based on the data source used for the estimates: population-based survey data (6 points); population statistics plus select survey data (5 points); population statistics plus expert estimates (4 points); adjusted Public Security Bureau registration data for community-based injecting drug users (IDUs; 4 points); similar population statistics and information (4 points); other area data (3 points); unadjusted Public Security Bureau registration data of IDUs (2 points); and expert estimation (1 point). A maximum of 6 points was possible. A score of at least 5 points was ‘excellent’, 3–4 points was ‘good’ and 1–2 points was ‘acceptable’.
Estimation methods
Estimates of HIV prevalence were generated using the Workbook Method recommended by the UNAIDS and the WHO for countries with low level or concentrated epidemics. This method has been described in detail elsewhere.13 Population size estimates for various subpopulations are entered into Workbook spreadsheets. HIV prevalence data are entered and applied to each subpopulation to generate an estimated number of people living with HIV for each subpopulation. High and low estimates for both population size and HIV prevalence are used to reflect uncertainty around estimates, and this gives rise to a range around point estimates.
Adaptations to the Workbook Method were made to account for the special characteristics of China’s HIV epidemic. The adaptations made in 2005 and 2007 have been described elsewhere.14,17
National-level estimates of HIV prevalence were generated based on provincial Workbook spreadsheets. Provincial data were aggregated to produce national estimates.
In 2005, 2007 and 2009, estimates of new HIV infections and HIV-related deaths were generated using the Estimation and Projection Package (EPP)18 and Spectrum19 software packages developed by the UNAIDS and the WHO. EPP generates a national HIV prevalence curve based on prevalence curves from lower levels of geographical aggregation (e.g. county, prefecture or province curves) and different subpopulations. EPP output is entered into Spectrum to calculate the annual number of new HIV infections and deaths since the start of the epidemic. Details of the application of EPP and Spectrum during the 2005 and 2007 estimation exercises have been described elsewhere.14,17
Results
Estimated HIV/AIDS cases
Key findings from China’s 2003, 2005, 2007 and 2009 HIV/AIDS estimation exercises are presented in Table 2. The estimated number of PLWHA dropped from 840 000 in 2003 to 650 000 in 2005, then rose to 700 000 in 2007 and 740 000 in 2009. The estimated number of AIDS cases fell from 80 000 in 2003 to 75 000 in 2005, then rose to 85 000 in 2007 and 105 000 in 2009. The estimated number of new HIV infections fell from 70 000 in 2005 to 50 000 in 2007 and 48 000 in 2009.
Table 2.
China’s national HIV/AIDS estimates, 2003–09
| Estimated number of people | ||||
|---|---|---|---|---|
| 2003 | 2005 | 2007 | 2009 | |
| PLWHA | ||||
| Point estimate | 840 000 | 650 000 | 700 000 | 740 000 |
| Range | 650 000–1 200 000 | 540 000–760 000 | 550 000–850 000 | 560 000–920 000 |
| AIDS cases | ||||
| Point estimate | 80 000 | 75 000 | 85 000 | 105 000 |
| Range | 65 000–85 000 | 80 000–90 000 | 97 000–112 000 | |
| AIDS deaths | ||||
| Point estimate | 25 000 | 20 000 | 26 000 | |
| Range | 20 000–30 000 | 15 000–25 000 | 22 000–30 000 | |
| New HIV infections | ||||
| Point estimate | 70 000 | 50 000 | 48 000 | |
| Range | 60 000–80 000 | 40 000–60 000 | 41 000–55 000 | |
The estimated number of PLWHA by mode of transmission is presented in Table 3. In 2003, estimates were not stratified by mode of transmission. Between 2005 and 2009, the proportion of estimated cases associated with sexual transmission increased and the proportion of estimated cases associated with injecting drug use transmission decreased.
Table 3.
Estimated number of PLWHA in China, by transmission mode: 2003–09
| 2003 (840 000) | 2005 (650 000) (%) | 2007 (700 000) (%) | 2009 (740 000) (%) | |
|---|---|---|---|---|
| Sexual contact | NA | 43.6 | 51.6 | 59.0 |
| Heterosexual | 36.3 | 40.6 | 44.3 | |
| Homosexual | 7.3 | 11 | 14.7 | |
| Injecting drug use | NA | 44.3 | 38.1 | 32.2 |
| Mother-to-child transmission | NA | 1.4 | 1.0 | 1.0 |
| Plasma/blood | NA | 10.7 | 9.3 | 7.8 |
| Total | 100 | 100 | 100 |
NA: not available.
The estimated number of new HIV infections by mode of transmission is presented in Table 4. Dramatic increases in HIV transmission among MSM have been observed in recent years.
Table 4.
Estimated number of new HIV infections in China, by transmission mode: 2003–09
| 2003 (NA) | 2005 (70 000) (%) | 2007 (50 000) (%) | 2009 (48 000) (%) | |
|---|---|---|---|---|
| Sexual contact | NA | 49.8 | 56.9 | 74.7 |
| Heterosexual | NA | 44.7 | 42.2 | |
| Homosexual | NA | 12.2 | 32.5 | |
| Injecting drug use | NA | 48.6 | 42.0 | 24.3 |
| Mother-to-child transmission | NA | 1.6 | 1.0 | 1.0 |
| Total | 100 | 100 | 100 |
NA: not available.
Data quality assessments
In 2007 and 2009, we assessed the quality of HIV prevalence and population size data. A comparison of the quality of population size data used for the 2007 and 2009 estimates is presented in Figure 1A. Subpopulations included DUs (DUs and IDUs), sex workers (SWs), clients of SWs, urban MSM, rural MSM, former plasma donors and low-risk populations. From 2007 to 2009, the proportion of data classified as ‘excellent’ increased for all subpopulations. The proportion of data classified as ‘excellent’ or ‘good’ also increased for all subpopulations, with the exception of a slight decrease for DUs/IDUs (from 98.9% in 2007 to 98.4% in 2009).
Figure 1.
Data quality evaluation for data being used in estimation of HIV/AIDS in China in 2007 and 2009. (A) Population size data and (B) HIV prevalence data. FPD: Former plasma donors
A comparison of the quality of HIV prevalence data used for the 2007 and 2009 estimates is presented in Figure 1B. The quality of data sources categorized as ‘excellent’ or ‘good’ increased for all subpopulations. The proportion of data sources categorized as ‘excellent’ increased from 2007 to 2009 for all subpopulations except for low-risk populations (decreased from 7.1% in 2007 to 6.0% in 2009).
Discussion
Multiple rounds of national estimation exercises have improved the accuracy of China’s HIV/AIDS estimates. Early estimates were based on limited data from high-prevalence areas and high-risk populations, and were hence higher than subsequent estimates based on more complete data from an expanded HIV surveillance system. Between 2003 and 2005, for example, national estimates of the number of PLWHA fell from 840 000 in 2003 to 650 000 in 2005. Two factors were primarily responsible for this drop.10 First, estimates in 2003 were most likely overestimated the epidemic but estimates in 2005 reflected the epidemic better since a wider range of data had became available, including data from a 2004 mass HIV screening of former plasma donors in central China and data from a greatly expanded HIV sentinel surveillance system. Secondly, more precise geographical units were used in preparing the estimates. In 2003, estimates were done at the provincial level, and the estimates were done at the prefecture level in 2005.
Between 2005 and 2009, HIV data availability continued to improve. First, the number of national and provincial HIV sentinel surveillance sites contributing data to China’s national HIV estimates increased from 929 sites in 2007 to 1029 sites in 2009. The largest increases were in the number of sites contributing data for female SWs (2007: 229 sites; 2009: 367 sites) and MSM (2007: 11 sites; 2009: 25 sites). This increase in number of sites reflects the growing importance of sexual transmission, which in 2005 overtook injecting drug use as the leading mode of HIV transmission. Secondly, more data are now available from expanded surveillance and special surveys. For example, three rounds of national surveys of MSM in 61 cities have provided more accurate assessments of HIV prevalence and risk behaviours within MSM communities around the country.
The quality of HIV data has also continued to improve. From 2007 to 2009, there was marked improvement in the proportion of HIV prevalence data classified as ‘excellent’ or ‘good’ across all populations. The quality of data used for population size estimates has also improved over time.
The increase of number of PLWHA may be influenced by two factors. First, with rapid scale-up of the national free antiretroviral treatment programme, PLWHA live longer.20 Secondly, even if a reduction of new HIV infections were observed, there are still a considerable number of people infected with HIV each year.
The rapid increase in HIV prevalence among MSM in recent years is a major cause for concern. Among both urban and rural MSM, estimated HIV prevalence has increased during each round of estimation since 2005. In 2009, MSM accounted for nearly one-third of new HIV infections in China.
For future HIV/AIDS estimation exercises, improvements still need to be made. There are still many data gaps to be filled. For example, further attention must be paid to HIV among the male clients of SWs and rural MSM. HIV surveillance sites need to be further expanded to cover smaller and medium-sized cities. Methodological limitations must also be addressed. The Workbook Method provides a good starting point for generating national HIV/AIDS estimates, but it may not accurately reflect the large regional differences in China’s HIV/AIDS epidemic. The Workbook Method also currently does not have the ability to generate estimates for a number of populations, including MSM >50-year-old, migrant wives, those infected via blood and or/blood products, mother-to-child transmission, sailors and foreigners.
Conclusion
Repeated rounds of national HIV/AIDS estimate exercises in 2003, 2005, 2007 and 2009 have generated data that more accurately reflect China’s heterogeneous epidemic. Improvements in data quality and data availability have improved the precision of HIV/AIDS estimates, providing information that is critical to public health priority setting and policymaking.
In the coming years, the government should continue to improve the quality and amount of data available for HIV/AIDS estimation exercises. Accurate estimates based on high-quality data will help the Chinese government, international organizations and civil society better target HIV testing, prevention, treatment and care programmes to curtail the Chinese HIV/AIDS epidemic.
Funding
This work was supported by the Chinese Government AIDS Programme (131-08-105-02); partly supported by China National Science and Technology Major Project on AIDS (2008ZX10001-003, 2008ZX10001-016); and partly supported by the Multidisciplinary HIV and TB Implementation Sciences Training in China funded by the US National Institutes of Health, Fogarty International Center and the National Institute on Drug Abuse (5U2RTW06918-07).
Acknowledgements
The authors thank Susan Chan for providing editing assistance. Authors are also grateful to staff from Epidemiology Division of National Centre for AIDS/STD Control and Prevention at China CDC: Shuquan Qu, Lan Wang, Dongmin Li, Liyan Wang, Qianqian Qin, Guowei Ding, Zhengwei Ding, Yanhe Wang and Xing Gao for their contributions in estimation in 2003–09.
The National Expert Group on HIV/AIDS Estimation includes scientists from the Ministry of Health AIDS Expert Advisory Committee (Yi Zeng, Zhicheng Dai, Konglai Zhang, Yude Chen, Xiwen Zheng, Ruotao Wang, Laiyi Kang, Beichuang Zhang, Qingwu Jiang, Suiming Pan, Dun Li, Lin Lu, Manhong Jia, Peng Lin, Wei Liu, Xi Chen, Yanshen Yan, Xiong He, Qichao Pan, Xiaoke Zhu); China CDC (Yu Wang); NCAIDS (Zunyou Wu, Ning Wang, Kangmai Liu, Yiming Shao, Lu Wang, Fan Lv, Fujie Zhang), Peking University (Yonghua Hu, Weihua Cao, Min Liu); Tsinghua University (Jun Jing); Peking Union Medical College (Zhenglai Wu); Fudan University (Na He); Nanjing University (Rongbin Yu); Anhui University (Hongbo Zhang); UNAIDS (Jinglin He, Zhondan Chen, Elisabeth Pisani, Joel Rehnstrom, Salil Panakadan, Rob Lyerla, Bernhard Schwartlander); WHO (Hong Chen, Wiwat Rojanapithayakorn, Pengfei Zhao, Katharine Poundstone, Connie Osborne), US CDC GAP (Ray Yip, Jinkou Zhao, Zhijun Li, Marc Bulterys); from local provinces (Minjian Ni, Guoping Ji, Bo Tao, Haitao Yang, Ming Fan, Peng Qu, Jihua Fu, Limei Shen, Qiya He, Faxian Zhan, Xianbin Ding, Xiaohong Pan, Hongyan Lu).
Conflict of interest: None declared.
KEY MESSAGES.
Repeated estimates HIV/AIDS in China in 2003, 2005, 2007 and 2009 have improved data quality, accuracy and reliability.
Repeated estimates have improved understanding of the HIV/AIDS epidemic in China.
References
- 1.Ma Y, Li Z, Zhang K, et al. Identification of HIV infection among drug users in China. Chin J Epidemiol. 1990;11:184–85. [Google Scholar]
- 2.Wu Z, Rou K, Cui H. The HIV/AIDS epidemic in China: history, current strategies and future challenges. AIDS Educ Prev. 2004;16:7–17. doi: 10.1521/aeap.16.3.5.7.35521. [DOI] [PubMed] [Google Scholar]
- 3.Wu Z, Rou K, Detels R. Prevalence of HIV infection among former commercial plasma donors in rural eastern China. Health Policy Plan. 2001;16:41–6. doi: 10.1093/heapol/16.1.41. [DOI] [PubMed] [Google Scholar]
- 4.The UN Theme Group on HIV/AIDS in China. China's Titanic Peril: 2001 Update of the AIDS Situation and Needs Assessment Report. Beijing: UNAIDS; 2002. [Google Scholar]
- 5.State Council AIDS Working Committee Office, UN Theme Group on HIV/AIDS in China. A Joint Assessment of HIV/AIDS Prevention, Treatment and Care in China (2003) Beijing: China Ministry of Health; 2003. [Google Scholar]
- 6.Sun X, Wang N, Li D, et al. The development of HIV/AIDS surveillance in China. AIDS. 2007;21(Suppl)( 8):S33–38. doi: 10.1097/01.aids.0000304694.54884.06. [DOI] [PubMed] [Google Scholar]
- 7.National Center for AIDS/STD Control and Prevention/Chinese Center for Disease Control and Prevention. 2009 HIV/AIDS Surveillance Report in China. Beijing: Chinese Center for Disease Control and Prevention; 2010. [Google Scholar]
- 8.Wu Z, Sun X, Sullivan SG, Detels R. Public health. HIV testing in China. Science. 2006;312:1475–76. doi: 10.1126/science.1120682. [DOI] [PubMed] [Google Scholar]
- 9.State Council AIDS Working Committee Office, UN Theme Group on AIDS in China. A Joint Assessment of HIV/AIDS Prevention, Treatment and Care in China (2007) Beijing: China Ministry of Health; 2007. [Google Scholar]
- 10.Ministry of Health of China, UNAIDS, WHO. 2005 Update on the HIV/AIDS Epidemic and Response in China. Beijing: Ministry of Health; 2006. [Google Scholar]
- 11.Ministry of Health of China, UNAIDS, WHO. The Estimation of HIV/AIDS in China in 2009. Beijing: Ministry of Health; 2010. [Google Scholar]
- 12.The UNAIDS Reference Group on Estimates, Modelling, and Projections. Improved methods and assumptions for estimation of the HIV/AIDS epidemic and its impact: Recommendations of the UNAIDS Reference Group on Estimates, Modelling and Projections. AIDS. 2002;16:W1–14. doi: 10.1097/00002030-200206140-00024. [DOI] [PubMed] [Google Scholar]
- 13.Walker N, Stover J, Stanecki K, et al. The workbook approach to making estimates and projecting future scenarios of HIV/AIDS in countries with low level and concentrated epidemics. Sex Transm Infect. 2004;80(Suppl 1):i10–13. doi: 10.1136/sti.2004.010207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang L, Wang N, Li D, et al. The 2007 estimates for people at risk for and living with HIV in China: progress and challenges. J Acquir Immune Defic Syndr. 2009;50:414–18. doi: 10.1097/QAI.0b013e3181958530. [DOI] [PubMed] [Google Scholar]
- 15.National Center for AIDS/STD Control and Prevention/China CDC. 2007 National HIV/AIDS Estimation Technical Guidance Protocol. http://www.chinaids.org.cn/n435777/n436916/n436920/540339.html (23 September 2010, date last accessed) [Google Scholar]
- 16.Family Health International. Estimating the Size of Populations at Risk for HIV: Issues and Methods. A Joint UNAIDS/IMPACT/FHI Workshop: Report and Conclusions. Arlington: Family Health International, Institute for HIV/AIDS; 2002. [Google Scholar]
- 17.Lu F, Wang N, Wu Z, et al. Estimating the number of people at risk for and living with HIV in China in 2005: methods and results. Sex Transm Infect. 2006;82(Suppl 3):iii87–91. doi: 10.1136/sti.2006.020404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown T, Salomon JA, Alkema L, Raftery AE, Gouws E. Progress and challenges in modelling country-level HIV/AIDS epidemics: the UNAIDS Estimation and Projection Package 2007. Sex Transm Infect. 2008;84(Suppl 1):i5–10. doi: 10.1136/sti.2008.030437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stover J, Johnson P, Zaba B, Zwahlen M, Dabis F, Ekpini RE. The Spectrum projection package: improvements in estimating mortality, ART needs, PMTCT impact and uncertainty bounds. Sex Transm Infect. 2008;84(Suppl 1):i24–30. doi: 10.1136/sti.2008.029868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang F, Dou Z, Ma Y, et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Ann Intern Med. 2009;151:241–51. doi: 10.7326/0003-4819-151-4-200908180-00006. [DOI] [PubMed] [Google Scholar]