Abstract
Background Prior to 2003, there was limited capacity for an HIV/AIDS response in China. In early 2003, China launched a 5-year China Comprehensive AIDS Response Programme (China CARES) to contain the spread of HIV infection and reduce its impact. This article describes the China CARES’ practices and experiences.
Methods China CARES covered 83.3 million people in 127 programme sites chosen from 28 provinces based on HIV prevalence. Each China CARES site was required to carry out surveillance and surveys to understand the local HIV/AIDS epidemic, to deliver primary interventions to reduce new HIV infections among and from high-risk groups, to prevent mother-to-child transmission, to treat AIDS patients with antiretroviral medicines and to provide support services to families affected by HIV/AIDS. Data were collected to monitor and evaluate implementation.
Results HIV/AIDS prevention knowledge and awareness improved significantly in China CARES sites from <30% in 2004 to 86% in 2008. The number of persons tested for HIV increased by 67% between 2005 and 2007 from 1.5 to 2.5 million. China CARES enrolled 23 000 patients in anti-retroviral treatment and supported 6007 AIDS orphans. Among pregnant women, 81.8% received counselling and 75.8% received HIV testing during antenatal care, while 92.9% of HIV-infected pregnant women and 85.5% of their newborns received anti-retroviral prophylaxis. During the project period, no known HIV transmissions occurred through blood transfusions.
Conclusion China CARES has facilitated AIDS prevention, treatment and care in resource-poor, rural and ethnic minority areas of China.
Keywords: HIV/AIDS, response, testing, prevention, anti-retroviral treatment, China CARES, AIDS policy
Introduction
The first case of HIV was reported in mainland China in 1985.1 Since then, all 31 provinces have reported HIV-positive cases. By June 2003, the cumulative number of reported HIV cases in China was 45 092, with 3532 AIDS cases and 1800 deaths.2 In central China, HIV cases and deaths were concentrated primarily among rural former plasma donors.3,4 The plasma donors were paid to donate blood, the plasma was removed and the red blood cells were reinfused to prevent anaemia.5 Meanwhile, sexually transmitted HIV infections increased from 5.5% in 1997 to 10.9% by 2002.6–8 Mother-to-child HIV transmission increased rapidly in certain regions.9 Across the country, rapidly expanding commercial sex and injecting drug use, as well population mobility, fuelled the HIV epidemic.10 Estimates from the Ministry of Health indicate that by 2009 around 740 000 people were living with HIV in China and 105 000 people had AIDS.11 The proportion of women infected also doubled in the past decade from 15 to 30%.
In contrast with the rapidly growing epidemic, there was very limited capacity12 for a comprehensive HIV/AIDS intervention response in China, especially in more rural and remote areas of the country where most of the HIV transmission occurred. By October 2002, there were fewer than 10 medical doctors who were sufficiently qualified to provide HIV/AIDS treatment. At that time, there were no more than 100 AIDS patients8,13 known to be receiving anti-retroviral (ARV) treatment in the entire country. Only a few behavioural interventions had been carried out with no nationwide systematic or comprehensive response. Social stigma and discrimination against HIV/AIDS were highly prevalent among the public, including among many health-care professionals.5,14,15
To address this untenable situation, the government launched the China Comprehensive AIDS Response Programme (China CARES) in early 2003 to explore the most appropriate models of a comprehensive HIV/AIDS response that would meet international standards. China CARES was designed to deliver quality HIV care and treatment to AIDS patients, contain the spread of HIV infection and reduce the impact of AIDS on society. The geographic focus was especially on rural, resource-poor and ethnic minority areas with relatively high HIV prevalence. The main activities of China CARES included: (i) strengthening HIV/AIDS surveillance; (ii) distributing comprehensive HIV prevention activities such as information, education and communication (IEC); free voluntary counselling and testing (VCT);16 condom use promotion; sexually transmitted disease (STD) diagnosis and treatment; needle exchange and methadone maintenance treatment (MMT); prevention of mother-to-child transmission (PMTCT); (iii) providing HIV care and treatment such as ARV treatment, care and support to people living with HIV/AIDS and free schooling for children orphaned by AIDS; and (iv) ensuring the safety of the blood supply.
This article describes China CARES practices and experiences between 2003 and 2008.
Goals and Objectives of China CARES
Goals
The goals of China CARES were to explore and adapt local measures for containing HIV spread in key populations, deliver quality HIV care and treatment to AIDS patients and reduce the societal impact of HIV/AIDS in under-resourced areas of the country.
Objectives
China CARES explored practical methods to conduct prioritized interventions using integrated approaches. The integrated approach included developing a clear annual work plan, monitoring indicators suitable to the local situation, establishing a collaboration network, strengthening staffing, instituting capacity, identifying best practices, documenting lessons learned and replicating successes.
Beginning of China CARES
The China CARES sites were chosen based upon an area’s HIV severity, transmission characteristics, existing response capacity and local government commitment. To address severe geographic and health inequities, ethnic composition of each site was also considered. In 2003, 51 counties and districts were chosen as the first group of programme sites. Counties were selected that had large numbers of reported HIV-positive cases, especially rural communities in Central China with large numbers of HIV-infected former plasma donors.3,4,17,18 A second group of 76 sites was chosen in 2004 in areas with large groups of people engaging in most at-risk behaviours such as injecting drug users and commercial sex workers. These 76 sites were located in a much larger geographic area.19 Overall, 127 counties and districts in 28 provinces participated in China CARES, covering a population of 83.3 million people. In 2004, there were 17 520 reported HIV/AIDS cases in these 127 areas, accounting for 39% of the total reported number of HIV/AIDS cases in the country.20
Project sites were selected using HIV surveillance data, models for the likely spread of HIV, known epicenters of former paid blood collection and local governments’ willingness to participate in the programme. After selection, the leading transmission route(s) for each China CARES site was identified (Table 1). Former paid plasma donation was the main transmission route in 56 (44.1%) sites, injecting drug use in 54 (42.5%) sites, and sexual transmission in 17 (13.4%) sites.23 In 2003, institutional and staff skills in HIV prevention, care and treatment were uniformly week across the sites. There were no HIV screening laboratories in 39 of the 127 sites (31%) and very limited HIV/AIDS prevention and treatment activities had been implemented.21,22 Limited education and HIV testing had previously been carried out in 88 of the 127 sites (69%). There were only a few community-based organizations (CBOs), and very few people living with HIV/AIDS (PLWHA) groups were involved in HIV/AIDS care and support.23
Table 1.
Main HIV transmission route categories in China CARES programme sites, 2003–08
| Main HIV transmission route categories | China CARES programme emphasis | No. of sites (N = 127) |
|---|---|---|
| Injecting drug use and sexual transmission (mixed) | Strengthen harm reduction interventions and balance efforts for preventing HIV transmission through sexual intercourse | 33 |
| Blood and plasma donation with limited commercial sex transmission (no more than 150 HIV cases) | Prioritize high-quality HIV care and treatment roll-out; focus on preventing sexual HIV transmission | 30 |
| Blood and plasma donation (almost exclusive) | Prioritize high-quality HIV care and treatment roll-out | 26 |
| Injecting drug use | Prioritize harm reduction interventions to prevent continued HIV transmission through injecting drug use | 25 |
| Commercial sex transmission | Strengthen education among sex workers and the general public; focus on preventing sexual transmission and implementing a 100% condom use policy | 13 |
Programme Implementation Strategies and Measures
Each China CARES site was required to establish an AIDS working committee to lead the local response, formulate local policies, define roles and responsibilities, mobilize and support of civil society and monitor and evaluate programme implementation. The committee was chaired by a chief government official with members from various government sectors such as Health, Publicity, Education, Civil Affairs, Public Security, Justice, Finance and the Women’s Federation. Non-government organizations (NGOs) and community-based organizations (CBOs) were supported to deliver services to most at-risk populations and people living with HIV/AIDS (PLWHA) in all programme sites.
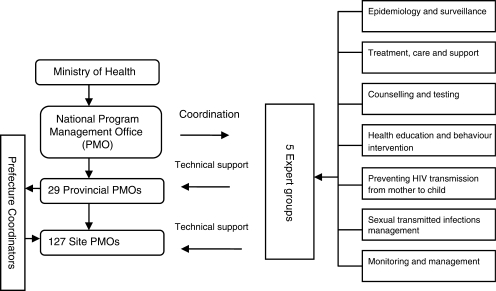
A four-tier programme management system was established at the national, provincial, prefecture and county levels. Corresponding working teams were established at these levels and extended through each county, township and rural village. To ensure a strong programme management system, the National Program Management Office (NPMO) developed the China CARES Program Working Manual 24 and established a resource panel in HIV/AIDS-related technical areas. Each resource group had the responsibility to develop and regularly update the technical guidance, operational manual and training models. Five expert groups were established according to geographic areas to provide specialized technical assistance to the 127 programme sites. Each expert group was responsible for five to six provinces. To respond to diverse needs, a group of professionals with various expertise attended biannual site visits to provide technical support in prevention, treatment, care and management, to ensure the planned activities were running properly and to ensure problems were addressed in a timely manner. Figure 1 provides an overview of the organization of the China CARES programme.
Figure 1.
Overview of the management structure of the China CARES, 2003–08
Given wide disparities and diversity in socio-economic, cultural and ethnic backgrounds, as well as diverse HIV disease burdens and transmission modes, project sites were encouraged to design and develop intervention activities with targeted goals taking the local situation into consideration. For instance, in Yunnan province and Xinjiang Autonomous Region in southwest and northwest of China, project sites particularly focused on intervention for drug users, where as in Henan province in central china, intervention focused on ART and care. Gradually, a set of strategies was formed and classified into five main categories based on the most common transmission routes as listed in Table 1.24 As part of an integrated and comprehensive response, the other transmission modes were also addressed as needed. In total, there were 85 national experts providing regular technical support to the 127 project sites.
Activities implemented in each site were tailored to local circumstances using multi-sectoral collaboration. Each sector was encouraged to contribute and share responsibilities. For instance, Health, Public Security and Food and Drug Administration jointly supported implementation of the MMT programme. Health and other sectors jointly supported condom promotion programmes. Women’s Federation mobilized housewives to conduct face-to-face HIV/AIDS information dissemination. Ministry of Publicity mobilized media outlets to air prime-time public service announcements. Local NGOs helped increase adherence to the ARV treatment and promote support groups. Micro-credit programmes assisted PLWHA to live on their own. Civil affairs sectors helped PLWHA access social security benefits. Youth league, Red Cross Society and Education sectors mobilized student volunteers to participate in HIV prevention information dissemination and promotion of safer sex.
China CARES made use of the available primary health-care system to promote patient follow-up and increase adherence to ARV treatment.4,10,11,25 Village doctors dispensed ARV drugs, provided directly observed therapy (DOT), and reminded patients to routinely have CD4 (and later an annual viral load) tests, which were conducted at facilities at the township, county or provincial level. Since county-level doctors provided technical support to township- and village-level doctors as the treatment team head, the three-tier health system increased patients’ adherence to ART through the DOT programme.4,11
To disseminate programme experiences and lessons learned, a China CARES Newsletter was compiled and published regularly. A China CARES homepage was established on the Chinese Centre for Disease Control and Prevention (China CDC)’s website.25 The Journal of China STD and AIDS issued a special volume about China CARES, as well as four editions of China CARES best practices, to facilitate local and regional experience sharing.26 National dissemination meetings were conducted by the State Council AIDS working committee and Ministry of Health (MOH) twice during the programme period. At the provincial level and below, collections of programme briefings and lessons learned were developed regularly and shared among programme sites to provide updates on progress and experiences to government leaders and related stakeholders.
Project Monitoring and Evaluation
Developing an annual work plan was the primary task for each programme site, with technical assistance provided by the assigned expert group. A monitoring and evaluation (M&E) plan was established to ensure activities were carried out accordingly. Problems identified through M&E were considered in the development of the next annual work plan. A regular reporting system with key M&E indicators, including monthly and quarterly progress reports, was established. Based on data collected from the reporting system, each expert group learned about the project’s progress and provided technical support accordingly. In addition, self-reviews were conducted twice a year at each site. At the provincial level, an overall review was conducted once a year and the review reports were submitted to the NPMO. At the national level, a joint on-site supervision was organized once a year in selected programme sites with participation from the MOH, multiple sectors, international cooperation programmes, NGOs, China CDC and expert groups. Supervisory methods included reviewing programme files and documents, on-site observations, and investigations including key informant and beneficiary interviews, questionnaire surveys and focus group discussions.
In the 2008 programme evaluation, a special survey was administered in a randomly selected sample of 10% of project sites in order to evaluate local facility and staff capacity, intervention effectiveness, general population HIV/AIDS knowledge and awareness, quality of life of people living with HIV/AIDS and total project costs. The evaluation was designed as a special survey and conducted by independent experts at Peking University Social Science and Survey Center, Yunnan Institute for Drug Dependence, China Institute for Health Education and Sichuan University.
Project impact was measured by comparing the baseline survey conducted in 2004 with the 2008 evaluation, and by comparing surveys conducted in 2008 in project and non-project sites nationally. In the baseline and 2008 surveys, structured questionnaires were used as well as focus group discussions, individual interviews among key informants and beneficiaries and project monthly and quarterly progress reports. The progress reports covered information on HIV testing, support for AIDS orphans, PMTCT, HIV care and support, STI services and intervention programmes including condom promotion and needle/syringe exchange.
To ensure the quality of data in the reporting system, the national programme officers regularly sampled the forms and reports and validated the information. The survey interviewers and investigators were formally trained before data collection. All respondents provided written informed consent. The respondents could decline to answer any question or leave the survey at any time.
China CARES Outcomes
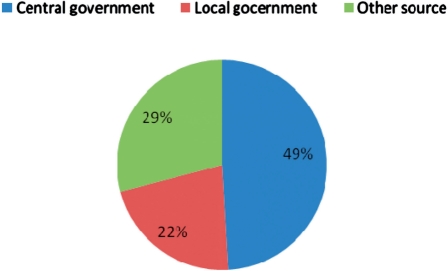
The Government allocated RMB 270 million (USD 39 million) to China CARES over 5 years. Local governments allocated RMB 119 million (USD 17 million), averaging 938 000 RMB (USD 134 000) for each site from 2004 to 2007. China CARES received financial support from other sources such as the Global Fund, the United Nations Population Fund (UNFPA), and the US CDC Global AIDS Program. On average, each site received RMB 4.3 million (614 000 USD) from the central government and an equivalent amount from the local provincial, prefecture and county government, plus other sources.28 Figure 2 lists the average distribution of financial support for the 127 China CARES sites.
Figure 2.
Summary of the financial support provided by central and local government and other sources for China CARES, 2004–07. ‘Other source’ includes: financial support from international institutions and bilateral organizations, foundations and NGOs
The county-level CDCs undertook China CARES implementation and, by 2008, 96% of programme sites had set up HIV/AIDS Prevention and Control offices at local county CDCs. The number of HIV/AIDS professional workers reached 1911, with an average of 15 workers per site (interquartile range = 8–21 workers per site). Based on an external independent assessment, 5 years of programme implementation showed significantly increased human capacity at the local level.26 The assessment team interviewed government leaders and beneficiary representatives as key informants using the indicators listed in Table 2.
Table 2.
China CARES programme satisfaction indicators among key informants and beneficiaries at the end of 5 years of implementation, 2008–09
| Institutional capacity indicators |
Average score (maximum 5.0) |
Standard deviation | |
|---|---|---|---|
| Informants (N = 72) | Beneficiaries (N = 175) | ||
| Financial resources | |||
| Resource mobilization | 4.78 | 4.62 | 0.67 |
| Resource allocation and usage | 4.75 | 4.53 | 0.50 |
| Coordination with multi-sectors | |||
| Joint work with multi-sectors | 4.76 | 4.61 | 0.72 |
| Training | 4.85 | 4.76 | 0.51 |
| Programme design | 4.61 | 4.57 | 0.72 |
| Programme implementation | 4.71 | 4.59 | 0.72 |
| Programme development | |||
| Programme management | 4.85 | 4.75 | 0.51 |
| Programme innovation | 4.43 | 4.54 | 0.73 |
| Overall capacity | 4.78 | 4.77 | 0.54 |
| Laboratory | |||
| Laboratory test | 4.72 | 4.70 | 0.61 |
| Emergency response | 4.76 | 4.70 | 0.58 |
| Information management | 4.71 | 4.75 | 0.55 |
HIV/AIDS prevention knowledge and awareness improved significantly in China CARES sites from <30% in 2004 to 86% in 2008. Eighty-six percent of rural adults, 92% of urban adults, 76% of Grade 7–9 students and 91% of Grade 10–12 students showed high levels of HIV knowledge. This compares with the national average of <70% among the general population 26. Five years after its implementation, sites adopting the China CARES programme performed better overall than non-programme sites in terms of HIV awareness among the general population and intervention effectiveness and coverage, according to the final evaluation report for China CARES (Table 3). An HIV sentinel surveillance system and an extensive laboratory network were established and later improved.16,29,30 By 2008, 23 000 PLWHA from China CARES sites received HIV care and support, and 6007 children orphaned by AIDS received free books, schooling fees and a subsidy for school boarding.31 Quality of life and living circumstances of PLWHA were significantly improved in China CARES sites, according to a comparison study.1,32,33 PLWHA in programme sites scored significantly better in terms of quality of life psychological functioning and social functioning than those in non-programme regions.26 By 2008, there were an average of at least six VCT clinics in each programme site, compared with an average of three in non-programme sites across the country.26 There were 60 MMT clinics in program sites.26 By 2006, PMTCT services covered all 127 programme sites through 1907 midwifery institutions. Among pregnant women, 81.8% received counselling and 75.8% received HIV testing, while 92.9% HIV infected pregnant women and 85.5% of their newborns received ARV prophylaxis.9,26 The mother-to-child transmission rate was reduced to 9.1% from an estimated 33% at baseline (Table 3). HIV transmission through blood was effectively prevented. One hundred per cent of blood used for clinical purposes was collected from voluntary as opposed to paid donors.34
Table 3.
Results of a programme evaluation at the end of 5 years of implementation of the China CARES programme in 127 counties and districts, 2008–09
| Indicator | Evaluation Result | Remarks |
|---|---|---|
| HIV/AIDS awareness among the general population (%) | 86.21 | 75 (planned target) |
| HIV/AIDS awareness among women aged 14–49 years (%) | 85.47 | 85 (planned target) |
| Intervention coverage among sex workers (%) | 88.60 | 39.80 (nationwide) |
| Condom use among sex workers (%) | 85.00 | 70 (planned target) |
| Needle sharing at last injection among IDU (%) | 12.09 | 27.5 (nationwide) |
| Cumulative number of PLWHA receiving ARV treatment | 19 000 | 46.2 of the country |
| Current number of PLWA receiving ARV treatment | 15 000 | 44.7% of the country |
| Percentage of PLWHA receiving ARV treatment for at least 12 months (%) | 87.40 | 84.4 (nationwide) |
| Mother-to-child transmission (%) | 9.13 | 33 (baseline) |
| Number of screening laboratories | 412 | 125 (baseline) |
| Number of sentinel surveillance | 145 | 21 (baseline) |
| Number of VCT clinics | 868 | None (baseline) |
China CARES has made efforts to mobilize NGOs involved in HIV/AIDS prevention and control. The programme helped NGOs increase capacity to deliver HIV services related to education, behaviour change and life care.35 There was a substantial increase in the number of NGOs involved in HIV/AIDS care in the China CARES sites, increasing from zero in 2003 to 756 at the end of the 5-year period.26
Regarding HIV testing, the number of persons who were tested for HIV increased significantly between 2005 and 2007, from 1.5 to 2.5 million, a 67% increase. However, the annual number of HIV-positive cases reported dropped slightly, from 8179 in 2005 to 7702 in 2007, with a corresponding decrease in prevalence from 5.3 to 3.7 per 1000 persons tested.
Discussion
After 5 years of implementation, China CARES has succeeded in disseminating best practices and experiences throughout many disparate areas of the country and has become a prototype for implementing Global Fund-supported HIV/AIDS programmes in many other counties.36 This government-led China CARES comprehensive programme, with multi-sectoral support and strong societal participation,37 was successful in raising awareness of HIV/AIDS in the general population and increasing coverage of preventive interventions along with increasing coverage of HIV care and treatment services. HIV/AIDS policies were formulated and implemented in 127 relatively poor counties and districts covering a population of 83.3 million people. In addition, China CARES promoted the revision and development of national and local laws and regulations such as the revision of AIDS articles in the Law of the Peoples’ Republic of China on the Prevention and Treatment of Infectious Diseases, as well as laws affecting health insurance and regulations concerning HIV/AIDS prevention and treatment.
Using a four-tier programme management system resulted in an effective and rapid response to HIV/AIDS in programme sites. Programme management offices at all levels followed the same guidelines on policies, technical planning, programme management and monitoring and evaluation. Programme sites were encouraged to explore individualized working methods and interventions adapted to the local context. These strategies proved essential for a quick and efficient HIV/AIDS response scale-up in low-capacity areas of the country.
Currently, the China CARES model is being promoted throughout the country because of its targeted interventions with integrated approaches adapted to the local situation. HIV/AIDS prevention and control staff capacity building will continue based on the China CARES experience. The strategic information system, including that for project monitoring and evaluation, will be further strengthened. Following the China CARES model, 16 provinces have established an additional 117 provincial sites using their own funds, and, in 2010, an additional 1300 sites will be established using international and central government funds.
One important limitation of the China CARES programme was that men who have sex with men (MSM) were not originally included as a target population. In 2003, few MSM sentinel surveillance sites existed. Since then, HIV prevalence among MSM has increased rapidly along with better testing coverage and an improved surveillance network.38–40
Challenges and Lessons Learned
Though great progress has been made and remarkable accomplishments have been achieved, many lessons have been learned from the implementation of China CARES, and there are still considerable challenges to be faced to improve China CARES in future.
High staff turnover affected the functioning of the project. Although there was constant and repeated training every year in different areas, it was difficult for new staff, especially in management and technical posts, to quickly reach functioning level.
All levels of government need to be included. Early on, an opportunity was missed with the prefecture level. Although coordinators were established at the prefecture level to communicate information between counties and the provincial levels, since the prefecture itself did not receive any funds, coordinators lacked technical training opportunities and the ability to carry out technical supervision. In the second round of China CARES, the prefecture level’s role has been strengthened.
Funds were sometimes delayed in their dispersal from central to county level, and this delay affected the project’s effectiveness.
Local leaders need to be fully aware of the significance of the HIV/AIDS response. In some cases, during episodes of local administration change, new leaders in charge of the health sector might remove HIV from the local priority list. Monitoring these changes in leadership and providing information on HIV at the appropriate time can greatly affect programme implementation.
Local staff need the capacity to do the work. Limited capacity of county level staff was a limiting factor as few staff experienced with the techniques to conduct targeted interventions for most at-risk populations.
Bottlenecks may occur when public health interventions are serial; for example, partner notification, patient follow-up, especially for mobile populations, and targeted health education for ethnic minority populations.
Social stigma and discrimination remains an important barrier in China.5 The new round of China CARES will continue to explore further methods to reduce stigma and discrimination.
Conclusion
China CARES has developed a crucial set of norms and standards for HIV/AIDS prevention and control at the national and local levels, which has played a fundamental role in the HIV/AIDS response in China. After a slow start,5 China has taken bold steps to control the epidemic using evidence-based strategies. China’s ‘Four Frees, and One Care’ (‘Four Frees’ refers to free HIV VCT, free schooling for orphaned children of AIDS patients, ART for pregnant women and free ART for rural HIV patients and poor urban patients; ‘One Care’ refers to financial subsidies for low-income AIDS patients and their families)4 policy was first implemented through China CARES. Programme implementation methods, best practices and lessons learned have been developed, documented and disseminated. Information sharing has been strengthened through the cooperation of international programmes such as the Global Fund and China–UK HIV/AIDS Prevention and Control Project. Wider geographical areas and risk populations have been covered by replicating the programme in other provinces, resulting in the establishment of an additional 117 HIV/AIDS programme sites by the end of the 5-year period. China CARES has made important contributions to expanding the coverage and impact of HIV/AIDS prevention, care and treatment activities in China, particularly among the resource-poor, rural and ethnic minority populations, which are often disproportionately affected by HIV/AIDS. China CARES has helped spearhead the country towards eventually reaching Universal Access as advocated by the United Nations.
Funding
Chinese Ministry of Health National AIDS Programme (131-08-105-02); and partly from the Global Fund, UNFPA and US CDC Global AIDS Program in China.
Acknowledgements
The authors would like to thank Christine Korhonen, Wendy Wei and Liming Wang (US CDC Global AIDS Programme in China) and Adrian Liau for their invaluable comments and editing assistance. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the U.S. Centers for Disease Control and Prevention.
Conflicts of interest: None declared.
KEY MESSAGES.
AIDS knowledge increased significantly, people tested for HIV increased by 67%, 23 000 patients enrolled to ARV treatment and 93% of HIV-infected pregnant women received PMTCT in 127 China CARES sites.
China CARES has facilitated HIV prevention, treatment and care in resource-poor, rural and ethnic minority areas of China.
References
- 1.Zheng X. A report on AIDS surveillance report from 1985 to 1988 in China. Chin J Epidemiol. 1989;10:65–67. (Chinese) [PubMed] [Google Scholar]
- 2.State Council AIDS Working Committee Office UN Theme Group on AIDS in China. A Joint Assessment of HIV/AIDS Prevention, Treatment and Care in China (2007) Beijing: Ministry of Health; 2007. p. 49. [Google Scholar]
- 3.Mastro TD, Yip R. The legacy of unhygienic plasma collection in China. AIDS. 2006;20:1451–52. doi: 10.1097/01.aids.0000233580.56844.c1. [DOI] [PubMed] [Google Scholar]
- 4.Bulterys M, Vermund SH, Chen RY, et al. A public health approach to rapid scale-up of free antiretroviral treatment in China: an ounce of prevention is worth a pound of cure. Chin Med J. 2009;122:1352–55. [PubMed] [Google Scholar]
- 5.Wu Z, Sullivan SG, Wang Y, et al. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369:679–90. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan J, Zheng X, Zhang X, et al. A survey of prevalence of HIV infection among paid blood donors in one county in China. Chin J Epidemiol. 2000;21:10–13. (Chinese) [PubMed] [Google Scholar]
- 7.Wu Z, Rou K, Detels R, et al. A survey of prevalence of HIV infection among paid blood donors in one county in China. Health Policy and Planning. 2001;1:41–46. doi: 10.1093/heapol/16.1.41. [DOI] [PubMed] [Google Scholar]
- 8.Department of Disease Control of the Ministry of Health of China. Establishment of the HIV sentinel surveillance system in China and the report of surveillance in 1995. Chin J STD AIDS Prev Control. 1996;2:193–97. [Google Scholar]
- 9.Wang L, Fang L, Wang Q, et al. The changing trend in mother-to-child transmission of HIV-1 during 2005-2007 in certain areas of China. Zhonghua Yu Fang Yi Xue Za Zhi. 2009;43:984–87. (Chinese) [PubMed] [Google Scholar]
- 10.Zheng X, Tian C, Choi KH, et al. Injecting drug use and HIV infection in Southwest China. AIDS. 1994;8:1141–47. doi: 10.1097/00002030-199408000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Zhang F, Dou Z, Ma Y, et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Ann Intern Med. 2009;151:241–51. doi: 10.7326/0003-4819-151-4-200908180-00006. [DOI] [PubMed] [Google Scholar]
- 12.Wang X, Wu Z. Factors associated with adherence to antiretroviral therapy among HIV/AIDS patients in rural China. AIDS. 2007;21(Suppl. 8):S149–55. doi: 10.1097/01.aids.0000304711.87164.99. [DOI] [PubMed] [Google Scholar]
- 13.Cao YZ, Lu HZ. Care of HIV-infected patients in China. Cell Res. 2005;15:883–90. doi: 10.1038/sj.cr.7290363. [DOI] [PubMed] [Google Scholar]
- 14.Sullivan SG, Xu J, Feng Y, et al. Stigmatizing attitudes and behaviors toward PLHA in rural China. AIDS Care. 2010;22:104–11. doi: 10.1080/09540120903012528. [DOI] [PubMed] [Google Scholar]
- 15.Cao X, Pang L, Wu Z. Cause, expression and elimination strategy of AIDS-related discrimination. Chin J AIDS STD. 2005;11:235–36. [Google Scholar]
- 16.Ma W, Wu Z, Qin Y, et al. A comparison of voluntary counseling and testing uptake between a China CARES county and a county not designated for the China CARES program. AIDS Patient Care STD. 2008;22:521–33. doi: 10.1089/apc.2007.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng X. HIV response work measures and insight observation in Zoucheng city. Chinese J Pub Health Manag. 2008;3:282–84. [Google Scholar]
- 18. Ministry of Health (MOH). Circular on guidance of China CARES project by the Office of MOH and Disease Control Department of MOH. Beijing (China): No 12, 2003.
- 19. Ministry of Health. Circular on second batch of China CARES project sites by Office of MOH. Beijing (China): No 133, 2003.
- 20.National Office of China CARES. Final Evaluation Report for 1st round of China CARES Project. Beijing (China): 2009. p. 2. [Google Scholar]
- 21.Office of China CARES project. Situation Analysis for China CARES Project. Beijing (China): 2003. p. 4. [Google Scholar]
- 22.Yu Z, Kan Q, He Y, et al. A comparison of the effects of three kinds of antiretroviral therapy on patients with human immunodeficiency virus infection. Chin J Infect Dis. 2007;12:726–30. [Google Scholar]
- 23.Wang M, Liu Q. The development of NGO in HIV/AIDS area and its relevant policy recommendation. Jiangsu Soc Sci. 2006;4:130–34. (Chinese) [Google Scholar]
- 24.National Office of China CARES project. Working manual for China CARES Project. Beijing (China): 2004. p. 6. [Google Scholar]
- 25.Zhao Y, Sun X, He Y, et al. Progress of the National Pediatric Free Antiretroviral Therapy program in China. AIDS Care. 2010;26:1–7. doi: 10.1080/09540121003615129. [DOI] [PubMed] [Google Scholar]
- 26. Chinaids.org [Internet]. Beijing: Chinese Centers for Disease Control and Prevention. China CARES. Available from: http://www.chinaids.org.cn/n16/n1193/n4073/442811.html (Chinese with English abstract). (date last acccessed September 27, 2010)
- 27. China CARES Program Office. Best practices and experiences of China CARES programme. Chin J AIDS STD 2007;13(Suppl.):1–125.
- 28. Unaids.org/en/ [Internet]. Geneva: UNAIDS. UNGASS reporting 2010. Available from: http://data.unaids.org/pub/Report/2010/china_2010_country_progress_report_en.pdf (date last accessed September 27, 2010)
- 29.Sun X, Wang N, Li D, et al. The development of HIV/AIDS surveillance in China. AIDS. 2007;21(Suppl 8):S33–38. doi: 10.1097/01.aids.0000304694.54884.06. [DOI] [PubMed] [Google Scholar]
- 30.Jia Y, Lu F, Sun X, et al. Sources of data for improved surveillance of HIV/AIDS in China. Southeast Asian J Trop Med Public Health. 2007;38:1041–52. [PMC free article] [PubMed] [Google Scholar]
- 31.Wang H, He G, Li X, et al. Self-Reported adherence to antiretroviral treatment among HIV-infected people in Central China. AIDS Patient Care STD. 2008;22:71–80. doi: 10.1089/apc.2007.0047. [DOI] [PubMed] [Google Scholar]
- 32.Ho C, Twinn S, Cheng K, et al. Quality of life constructs of Chinese people living with HIV/AIDS. Psychol Health Med. 2010;15:210–19. doi: 10.1080/13548501003623948. [DOI] [PubMed] [Google Scholar]
- 33.Xu T, Wu Z, Rou K, et al. Quality of life of children living in HIV/AIDS-affected families in rural areas in Yunnan, China. J Child Fam Stud. 2009;18:93–101. [Google Scholar]
- 34.State Council Working Committee office on AIDS. Mid-term Review Report for Action Plan for HIV Prevention and Treatment in China (2005–2010) Beijing (China): 2009. [Google Scholar]
- 35.Wang N. China HIV epidemic situation and its response. China Soc Welfare. 2005;10:29–31. [Google Scholar]
- 36.Cheng X. HIV response work meansures and insight observation in Zoucheng city. Chinese J Pub Health Manag. 2008;3:282–84. [Google Scholar]
- 37.Wang L. Overview of the HIV/AIDS epidemic, scientific research and government responses in China. AIDS. 2007;21(Suppl. 8):S3–7. doi: 10.1097/01.aids.0000304690.24390.c2. [DOI] [PubMed] [Google Scholar]
- 38.Wang L, Wang N, Wang LY, et al. The 2007 estimates for people at risk for and living with HIV in China: progress and challenges. J AIDS. 2009;4:414–18. doi: 10.1097/QAI.0b013e3181958530. [DOI] [PubMed] [Google Scholar]
- 39.Wei C, Guadamuz T, Stall R, et al. STD prevalence, risky behaviors and sex with women in a national sample of Chinese men who have sex with men. Am J Public Health. 2009;11:1978–81. doi: 10.2105/AJPH.2008.150037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu H, Yang H, Li X, et al. Men who have sex with men and human immunodeficiency virus/sexually transmitted disease control in China. Sex Transm Dis. 2006;33:68–76. doi: 10.1097/01.olq.0000187266.29927.11. [DOI] [PubMed] [Google Scholar]