Abstract
AIM: To give an overview of the literature on left-sided acute appendicitis (LSAA) associated with situs inversus totalis (SIT) and midgut malrotation (MM).
METHODS: We present a new case of LSAA with SIT and a literature review of studies published in the English language on LSAA, accessed via PubMed and Google Scholar databases.
RESULTS: Ninety-five published cases of LSAA were evaluated and a 25-year-old female, who presented to our clinic with left lower abdominal pain caused by LSAA, is reported. In the reviewed literature, fifty-seven patients were male and 38 were female with an age range of 8 to 82 years and a median age of 29.1 ± 15.9 years. Sixty-six patients had SIT, 23 had MM, three had cecal malrotation, and two had a previously unnoted congenital abnormality. Fifty-nine patients had presented to the hospital with left lower, 14 with right lower and seven with bilateral lower quadrant pain, and seven subjects complained of left upper quadrant pain. The diagnosis was established preoperatively in 49 patients, intraoperatively in 19, and during the postoperative period in five; 14 patients were aware of having this anomaly. The data of eight patients were not unavailable. Eleven patients underwent laparoscopic appendectomy, which was combined with cholecystectomy in two cases. Histopathological examination of the appendix specimens revealed adenocarcinoma in only two of 95 patients.
CONCLUSION: The diagnosis of left lower quadrant pain is based on well-established clinical symptoms, physical examination and physician’s experience.
Keywords: Diagnostic dilemma, Left lower quadrant pain, Left-sided appendicitis, Midgut malrotation, Situs inversus totalis
INTRODUCTION
Acute appendicitis is probably the most common intraabdominal condition requiring emergency surgery. The diagnosis is based on well-established clinical symptoms, basic radiologic findings and surgeon experience[1,2]. Approximately one third of patients with acute appendicitis have pain localized outside of the right lower quadrant because of the various positions of the appendix vermiformis, i.e. retrocecal, pelvic, subcecal, preileal and postileal, while subhepatic, meso-celiac, mid-inguinal and left-sided are seen more rarely[1,2].
Appendicitis causing pain in the left lower quadrant is extremely rare and can occur with congenital abnormalities that include true left-sided appendix or as an atypical presentation of right-sided, but long appendix, which projects into the left lower quadrant[2]. Left-sided acute appendicitis (LSAA) develops in association with two types of congenital anomalies: situs inversus totalis (SIT) and midgut malrotation (MM)[1-65]. Herein, we report an unusual case of SIT with acute appendicitis presenting as left lower quadrant abdominal pain. We also reviewed 95 published cases of LSAA with congenital anomalies retrieved from the Google Scholar and PubMed databases.
MATERIALS AND METHODS
We report a new case of LSAA with SIT. Additionally, for the review, a search of the English medical language literature in PubMed and Google Scholar was conducted for every case report, series, letter to the editor, original article and literature review relating to left-sided appendicitis. In addition, reference lists of the articles obtained and previous reviews were examined. Key words used were left lower quadrant pain, LSAA, appendicitis with left lower quadrant pain, SIT and appendicitis, acute left-sided appendicitis, and MM and appendicitis. The search included all articles from 1893 to July 2010. The articles containing adequate information such as patient age, sex, localization of the symptoms, time of the diagnosis, type of congenital anomalies, choice of incision and surgery were included in the study, while studies and comment articles with insufficient clinical and demographic data were excluded.
RESULTS
Case report
A 25-year-old female presented to the emergency unit on June 18, 2010 with severe abdominal pain, which started the previous night. The patient stated that the pain has begun first in the epigastric area and later expanded through the left lower quadrant. Besides the pain, she complained of inappetence and mild nausea. Patient history revealed no previous illness or surgery. On physical examination, rebound tenderness was observed in the left lower quadrant. Laboratory tests, including leukocyte count (9100 K/UL), were normal. Based on the patient’s clinical status and our previous experience, we considered LSAA in the differential diagnosis; accordingly, relevant analyses were performed. Chest X-ray revealed dextrocardia (Figure 1) and abdominal ultrasonography (USG) demonstrated SIT and blind intestinal loop consistent with acute appendicitis in the left lower quadrant. The patient was immediately taken to surgery and as the laparoscopic device was out of order, a left McBurney’s incision was performed. She was discharged on the second postoperative day with no complications (Figure 2). Contrast-enhanced thoraco-abdominal computed tomography (CT) in the postoperative period confirmed the diagnosis of SIT (Figure 3).
Figure 1.

Chest X-ray showing dextrocardia.
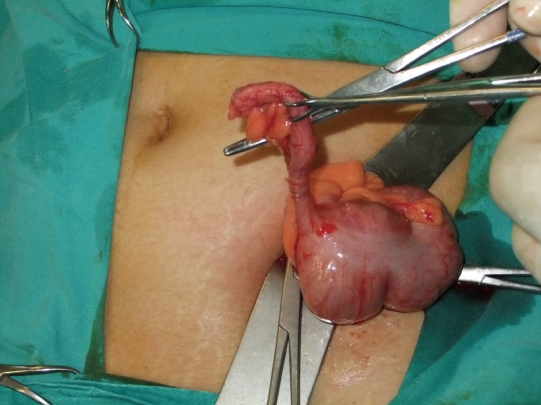
Figure 2.
Intraoperative photograph showing an appendix together with cecum in the left lower quadrant.
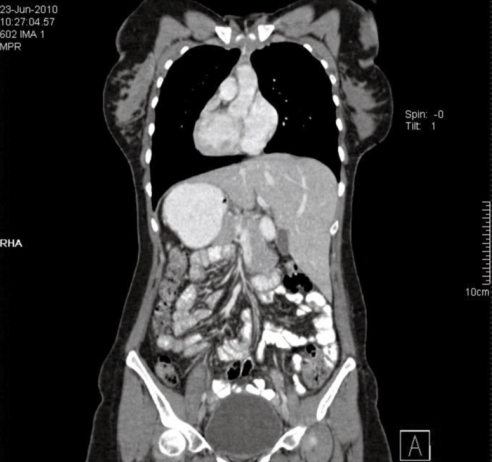
Figure 3.
Coronal contrast-enhanced multidetector computed tomography of the thorax, abdomen and pelvis. Computed tomography showed situs inversus totalis including dextrocardia, right-sided gastric bubble and reversed spleen and liver (postoperative view).
Analysis of literature about left-sided appendicitis
The English medical literature published to July 2010 in PubMed and Google Scholar databases was reviewed, and 64 reports concerning 95 cases of LSAA meeting the above-mentioned criteria were included in this review[1-64]. The article types were as follows: case report - 48, case report and a review of the literature - 7, imaging for surgeon - 5, letter to the editor - 2, and abstract - 2. The clinicopathologic characteristics of the 95 patients are summarized in Table 1. The patients were aged from 8 to 82 years (mean: 29.1 ± 15.9 years). Fifty-seven were male (mean: 30.9 ± 15.2 years, range: 9-82 years) and 38 were female (mean: 26.5 ± 16.4 years, range: 8-76 years). Sixty-six patients had SIT, 23 had MM, 3 had cecal malrotation, in two the anomaly was previously unnoted and in one case, the end of the appendix running along the anterior side of sacrum was found in the left side. According to localization of the symptoms, 59 patients presented with left and 14 with right lower quadrant pain, 7 with bilateral lower quadrant pain, 7 with left upper quadrant pain, 6 with peri-umbilical, and two presented with pelvic pain. With regard to the diagnosis, 49 patients were diagnosed with appendicitis during the pre-operative period, in 19 patients, the diagnosis was established intraoperatively and in 5 postoperatively; 14 patients were previously known to have SIT and/or MM. No information was available in eight patients. Of 95 patients included in this literature review, 13.6% of patients underwent laparoscopic surgery. Laparoscopic appendectomy was performed in eight cases[6,10,12,13,15,21,24,58], and was combined with cholecystectomy in two[3,41] and with ablation of endometriosis implants in one patient[7]. In the remaining two patients, the intervention was switched to laparotomy due to technical reasons[8,25].
Table 1.
Summary of 95 reported cases of left-sided acute appendicitis with situs inversus totalis and midgut malrotation n (%)
| Patient characteristics | Results |
| Mean age (yr, range) | 29.1 ± 15.9 (8-82) |
| Sex | |
| Male | 57 (60) |
| Female | 38 (40) |
| Pain location | |
| Left-lower quadrant | 59 (62.1) |
| Right-lower quadrant | 14 (14.7) |
| Bilateral lower quadrant | 7 (7.3) |
| Pelvic | 2 (2) |
| Left-upper quadrant | 7 (7.3) |
| Peri-umbilical | 6 (6.3) |
| Congenital anomaly | |
| Situs inversus totalis | 66 (69.4) |
| Midgut malrotation | 23 (24.2) |
| Cecal malrotation | 3 (3) |
| Unnoted | 2 (2) |
| Other | 1 (1) |
| Time of diagnosis | |
| Preoperative | 49 (51.5) |
| Intraoperative | 19 (20) |
| Known | 14 (14.7) |
| Postop | 5 (5.2) |
| Unnoted | 8 (8.4) |
DISCUSSION
There are two anatomic abnormalities which result in LSAA - the first being SI, and the second, less common abnormality, is MM[6,7]. MM is the term used to describe a spectrum of congenital positional anomalies of the intestine caused by nonrotation or incomplete rotation of the primitive loop around the axis of the superior mesenteric artery (SMA) during fetal life. Although about 80% of cases are diagnosed in patients younger than 1 mo, malrotation has also been reported in older children and adults[8]. The incidence of MM cited in the literature varies from 0.03% to 0.5% in live births[1,3,9,10]. SI is an uncommon condition, which is caused by a single autosomal recessive gene with incomplete penetrance and occurs in 1 per 5000 to 1 per 10 000 live births[7]. This condition may be complete (SIT), when both thoracic and abdominal organs are transposed, or partial, when only one of those cavities is affected[1]. The incidence of SIT reported in the literature varies from 0.001% to 0.01% in the general population[12-14], whereas the incidence of acute appendicitis associated with SIT is reported to be between 0.016% and 0.024%[5,13,14].
According to published reports in the literature, LSAA occurs between the age of 8 and 63 years and is 1.5-fold more frequent in men than in women[3,13]. In our review, we determined the mean age of the patients as 29.3 ± 16.1 (range: 8-82) years and the male/female sex ratio as 3/2[1].
The differential diagnosis of left lower quadrant abdominal pain includes: diverticulitis, renal colic, ruptured ovarian cyst, Meckel’s diverticulitis, epididymitis, incarcerated or strangulated hernia, bowel obstruction, regional enteritis, psoas abscess, and right- and left-sided appendicitis (LSAA)[1,4].
LSAA is a diagnostic dilemma, because the appendix is located in an abnormal position. The differential diagnosis of LSAA may not be promptly established in the emergency setting and is often delayed due to lack of uniformity in the clinical signs[11,58]. It is assumed that even though the viscera are transposed, the nervous system may not show the corresponding transposition, which may result in confusing symptoms and signs. In about 18.4%-31% of patients with SIT and MM, the pain caused by LSAA has been reported in the right lower quadrant[1,5,11-13]. In this literature review, it was observed that 14.7% of patients had pain localized in the right lower quadrant, which indicates the importance of accurate preoperative diagnosis in order to avoid incorrect incision.
The diagnosis of acute appendicitis in patients with SIT or MM can be based on physical examination, electrocardiogram, chest X-ray, barium studies, USG, CT scan and diagnostic laparoscopy[1,2].
Plain radiographs are usually not helpful for establishing the diagnosis of appendicitis. However, the detection of dextrocardia on chest X-ray and right-sided gastric bubble on abdominal plane X-ray is of considerable value in establishing the diagnosis of SIT. Barium enema with gastrografin can reveal MM or SIT, when there are difficulties in making the diagnosis of acute left lower quadrant pain[11]. Over the last two decades, there has been an increasing use of imaging modalities, such as USG and CT, in the diagnosis of acute appendicitis. USG is widely used in cases of appendicitis, however, it has significant limitations: it is operator-dependent, and examination of the lower quadrant can be compromised in patients with large body habitus or by overlying bowel gas. The value of CT in the diagnosis of acute appendicitis has been well-documented, with a reported accuracy of 90%-98%[2,13]. USG and CT may also be helpful in the detection of SIT and MM. Of the patients included in this literature review, CT has been used in the diagnosis of 28 patients and USG in 22 patients since 2000[1,6,8,17-24,26,27].
After establishing the diagnosis of SIT or MM, the surgical options are the same as for normal patients[1]. According to the reviewed literature, we observed that many open and a few laparoscopic procedures have been performed[1,6,8,15]. Laparoscopic appendectomy was first carried out in 1998 by Contini et al[58] in a 34-year-old male patient with SIT. Since then, laparoscopic appendectomy has been performed in a total of 20 cases (12 with MM and 8 with SIT), of which two have undergone cholecystectomy at the same surgical session[3,6,7,10,12,13,15,21,24,41,58,65]. We believe that laparoscopy may be very useful both in establishing the differential diagnosis and in performing the definitive surgery[1].
As in patients with normally localized appendix, appendectomy specimens in LSAA should be sent for pathological evaluation. To our knowledge, in the literature, only two of 95 patients (59 male, 76 female), who underwent appendectomy due to LSAA, were pathologically diagnosed with malignancy. Ascendent hemicolectomy was performed in both patients after pathological evaluation, which revealed mucinous adenocarcinoma and mucinous cystadenocarcinoma[19,26].
In conclusion, LSAA should be considered in the differential diagnosis of young patients presenting with pain localized in the left lower quadrant. Chest X-ray, abdominal USG and CT provide quite useful information. Diagnostic laparoscopy is the gold standard in cases with complicated differential diagnosis.
COMMENTS
Background
Acute appendicitis is a surgical condition, which manifests itself as pain usually localized in the lower right quadrant and can be diagnosed easily due to its clinical findings. Besides the surgeon experience, blood tests, radiological investigations, and in some circumstances, diagnostic laparoscopic techniques, should be used in the diagnosis of atypically localized appendicitis.
Research frontiers
Left-sided appendix is a rarely seen condition, which is frequently associated with situs inversus totalis (SIT) and midgut malrotation (MM). In this study, the authors performed an overall evaluation of management approaches and diagnostic processes in cases of left-sided acute appendicitis (LSAA) related to SIT and MM published in the English language literature to date, and presented the experience.
Innovations and breakthroughs
This study is the largest literature screening on LSAA to date.
Applications
This brief literature review demonstrates the importance of radiologic assessment and diagnostic laparoscopy along with surgical experience in the differential diagnosis of LSAA.
Peer review
The authors described a case of left sided appendicitis in the setting of situs inversus and a corresponding literature review. Over all, this paper is well written, concise and information.
Footnotes
Peer reviewer: Eric S Hungness, MD, FACS, Assistant Professor, Division of Gastrointestinal and Oncologic Surgery, Northwestern University Feinberg School of Medicine, 676 N. St. Clair St., Suite 650, Chicago, IL 60611-2908, United States
S- Editor Wang YR L- Editor Webster JR E- Editor Zheng XM
References
- 1.Akbulut S, Caliskan A, Ekin A, Yagmur Y. Left-sided acute appendicitis with situs inversus totalis: review of 63 published cases and report of two cases. J Gastrointest Surg. 2010;14:1422–1428. doi: 10.1007/s11605-010-1210-2. [DOI] [PubMed] [Google Scholar]
- 2.Hou SK, Chern CH, How CK, Kao WF, Chen JD, Wang LM, Huang CI. Diagnosis of appendicitis with left lower quadrant pain. J Chin Med Assoc. 2005;68:599–603. doi: 10.1016/S1726-4901(09)70101-7. [DOI] [PubMed] [Google Scholar]
- 3.Franklin ME Jr, Almeida JA, Pérez ER, Michaelson RLP, Majarrez A. Cholecystectomy and appendectomy by laparoscopy in a patient with situs inversus totalis: A case report and review of the literature. Asoc Mex Cir Endoscopica. 2001;2:150–153. [Google Scholar]
- 4.Lee MR, Kim JH, Hwang Y, Kim YK. A left-sided periappendiceal abscess in an adult with intestinal malrotation. World J Gastroenterol. 2006;12:5399–5400. doi: 10.3748/wjg.v12.i33.5399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Steensel CJ, Wereldsma JC. Acute appendicitis in complete situs inversus. Neth J Surg. 1985;37:117–118. [PubMed] [Google Scholar]
- 6.Bedoui R, Ali Ouaer M, Nouira R, Dziri C. Acute left-sided appendicitis. Tunis Med. 2009;87:873–874. [PubMed] [Google Scholar]
- 7.Song JY, Rana N, Rotman CA. Laparoscopic appendectomy in a female patient with situs inversus: case report and literature review. JSLS. 2004;8:175–177. [PMC free article] [PubMed] [Google Scholar]
- 8.Nicholas JM, Rozycki GS. Special feature: image of the month. Diagnosis: acute left-sided appendicitis. Arch Surg. 2001;136:705–706. doi: 10.1001/archsurg.136.6.705. [DOI] [PubMed] [Google Scholar]
- 9.Israelit S, Brook OR, Nira BR, Guralnik L, Hershko D. Left-sided perforated acute appendicitis in an adult with midgut malrotation: the role of computed tomography. Emerg Radiol. 2009;16:217–218. doi: 10.1007/s10140-008-0746-x. [DOI] [PubMed] [Google Scholar]
- 10.Welte FJ, Grosso M. Left-sided appendicitis in a patient with congenital gastrointestinal malrotation: a case report. J Med Case Reports. 2007;1:92. doi: 10.1186/1752-1947-1-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed JU, Hossain GMZ, Karim MM, Hossain ASMI, Ahmed M, Bhuya MSA. Left sided acute appendicitis with situs inversus in an elderly - an unusual case. JCMCTA. 2007;18:29–31. [Google Scholar]
- 12.Golash V. Laparoscopic management of acute appendicitis in situs inversus. J Min Access Surg. 2006;2:220–221. doi: 10.4103/0972-9941.28184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perera WR, Hennessy OF. Clinical Images. An unusual case of appendicitis. Am J Surg. 2010;199:e79–e81. doi: 10.1016/j.amjsurg.2009.08.047. [DOI] [PubMed] [Google Scholar]
- 14.Huang SM, Yao CC, Tsai TP, Hsu GW. Acute appendicitis in situs inversus totalis. J Am Coll Surg. 2008;207:954. doi: 10.1016/j.jamcollsurg.2008.03.030. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz JH, Manco LG. Left-sided appendicitis. J Am Coll Surg. 2008;206:590. doi: 10.1016/j.jamcollsurg.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 16.Seifmanesh H, Jamshidi K, Kordjamshidi A, Delpisheh A, Peyman H, Yasemi M. Acute left-sided appendicitis with situs inversus totalis: a case report. Am J Emerg Med. 2010;28:1058.e5–1058.e7. doi: 10.1016/j.ajem.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 17.Pillow MT, Valle C. Appendicitis in an uncommon location. West J Emerg Med. 2010;11:115. [PMC free article] [PubMed] [Google Scholar]
- 18.Cissé M, Touré AO, Konaté I, Dieng M, Ka O, Touré FB, Dia A, Touré CT. Appendicular peritonitis in situs inversus totalis: a case report. J Med Case Reports. 2010;4:134. doi: 10.1186/1752-1947-4-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Petrou A, Papalambros A, Katsoulas N, Bramis K, Evangelou K, Felekouras E. Primary appendiceal mucinous adenocarcinoma alongside with situs inversus totalis: a unique clinical case. World J Surg Oncol. 2010;8:49. doi: 10.1186/1477-7819-8-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abboud B, Daher R. An exceptional cause of left lower quadrant abdominal pain. World J Gastroenterol. 2009;15:3451. doi: 10.3748/wjg.15.3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hassan AA, El Sabagh A, Helmy AH. Laparoscopic management of acute appendicitis in situs inversus totalis. Egypt J Surg. 2008;27:213–215. [Google Scholar]
- 22.Pinto A, Di Raimondo D, Tuttolomondo A, Fernandez P, Caronia A, Lagalla R, Arnao V, Law RL, Licata G. An atypical clinical presentation of acute appendicitis in a young man with midgut malrotation. Radiography. 2007;13:164–168. [Google Scholar]
- 23.Lin CJ, Tiu CM, Chou YH, Chen JD, Liang WY, Chang CY. CT presentation of ruptured appendicitis in an adult with incomplete intestinal malrotation. Emerg Radiol. 2004;10:210–212. doi: 10.1007/s10140-003-0316-1. [DOI] [PubMed] [Google Scholar]
- 24.Tsumura H, Ichikawa T, Kagawa T, Nishihara M. Successful laparoscopic Ladd's procedure and appendectomy for intestinal malrotation with appendicitis. Surg Endosc. 2003;17:657–658. doi: 10.1007/s00464-002-4516-7. [DOI] [PubMed] [Google Scholar]
- 25.Keith JC, Thoma JJ, Bugay SJ, Price PD, Smear J. Asymptomatic midgut rotational anomalies in adults: 2 case reports and review of the literature. Contemp Surg. 2003;59:322–325. [Google Scholar]
- 26.Sato H, Fujisaki M, Takahashi T, Maruta M, Maeda K, Kuroda M. Mucinous cystadenocarcinoma in the appendix in a patient with nonrotation: report of a case. Surg Today. 2001;31:1012–1015. doi: 10.1007/s005950170014. [DOI] [PubMed] [Google Scholar]
- 27.Zissin R, Kots E, Shpindel T, Shapiro-Feinberg M. Acute appendicitis with intestinal non-rotation presenting with partial small bowel obstruction diagnosed on CT. Br J Radiol. 2000;73:557–559. doi: 10.1259/bjr.73.869.10884757. [DOI] [PubMed] [Google Scholar]
- 28.Carmichael KA, Gayle WE Jr. Situs inversus and appendicitis. South Med J. 1979;72:1147–1150. doi: 10.1097/00007611-197909000-00020. [DOI] [PubMed] [Google Scholar]
- 29.Shapiro NM, Michels LM, Hurwıtz S. Appendicitis with typical symptoms but ectopic appendix due to malrotation of colon. Calif Med. 1963;98:158–159. [PMC free article] [PubMed] [Google Scholar]
- 30.Price EA, Kane G. Non-rotation of gut; with report of case of left-sided appendiceal abscess. S Afr Med J. 1955;29:655–658. [PubMed] [Google Scholar]
- 31.Thomas DW. Left-sided appendicitis. Br Med J. 1952;2:43. [Google Scholar]
- 32.Hershman M. Left-sided appendicitis. Br Med J. 1952;1:1357. [Google Scholar]
- 33.Roche DA. Left-sided appendicitis. Br Med J. 1952;2:43. [Google Scholar]
- 34.Rowling JT. Left-sided appendicitis. Br Med J. 1952;2:43. [Google Scholar]
- 35.Strother-Stewart CR, McVey F. Points from letters: left-sided appendicitis. Br Med J. 1952;2:165. [Google Scholar]
- 36.Cannon DJ. Points from letters: left-sided appendicitis. Br Med J. 1952;2:165. [Google Scholar]
- 37.Haddon JWL. A case of left-sided appendicitis. Br Med J. 1945;2:569. doi: 10.1136/bmj.2.4425.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grook JL. Left-sided appendicitis. South Med J. 1918;11:311, 318. [Google Scholar]
- 39.Craig HL, Millar DM. Acute appendicitis in situs inversus. Br Med J. 1962;1:563. [Google Scholar]
- 40.Marks C, Pokroy M. Situs inversus totalis; a report of a case presenting with an acute abdomen. S Afr Med J. 1955;29:526–527. [PubMed] [Google Scholar]
- 41.Djohan RS, Rodriguez HE, Wiesman IM, Unti JA, Podbielski FJ. Laparoscopic cholecystectomy and appendectomy in situs inversus totalis. JSLS. 2000;4:251–254. [PMC free article] [PubMed] [Google Scholar]
- 42.Uludag M, Citgez B, Ozkurt H. Delayed small bowel perforation due to blunt abdominal trauma and periappendicitis in a patient with situs inversus totalis: a report of a case. Acta Chir Belg. 2009;109:234–237. doi: 10.1080/00015458.2009.11680412. [DOI] [PubMed] [Google Scholar]
- 43.Ucar AE, Ergul E, Aydin R, Ozgun YM, Korukluoglu B. Left-sided acute appendicitis with situs inversus totalis. Internet J Surg. 2007;12:5. [Google Scholar]
- 44.Kamiyama T, Fujiyoshi F, Hamada H, Nakajo M, Harada O, Haraguchi Y. Left-sided acute appendicitis with intestinal malrotation. Radiat Med. 2005;23:125–127. [PubMed] [Google Scholar]
- 45.Hollander SC, Springer SA. The diagnosis of acute left-sided appendicitis with computed tomography. Pediatr Radiol. 2003;33:70–71. doi: 10.1007/s00247-002-0829-x. [DOI] [PubMed] [Google Scholar]
- 46.du Toit DF, Greeff M. Acute abdomen in a patient with situs inversus. A case report. S Afr Med J. 1986;69:201–202. [PubMed] [Google Scholar]
- 47.Winter B, Dyk M. Left-sided acute appendicitis. Can Med Assoc J. 1953;68:278–279. [PMC free article] [PubMed] [Google Scholar]
- 48.Block FB, Michael MA. Acute appendicitis in complete transposition of viscera: report of case with symptoms referable to right side mechanism of pain in visceral disease. Ann Surg. 1938;107:511–516. doi: 10.1097/00000658-193804000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Willis BC. Appendicitis and transposition of the viscera. Ann Surg. 1925;82:256–259. doi: 10.1097/00000658-192508000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Blegen HM. Surgery in Situs Inversus. Ann Surg. 1949;129:244–259. doi: 10.1097/00000658-194902000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nelson MJ, Pesola GR. Left lower quadrant pain of unusual cause. J Emerg Med. 2001;20:241–245. doi: 10.1016/s0736-4679(00)00316-4. [DOI] [PubMed] [Google Scholar]
- 52.Ratani RS, Haller JO, Wang WY, Yang DC. Role of CT in left-sided acute appendicitis: case report. Abdom Imaging. 2002;27:18–19. doi: 10.1007/s00261-001-0039-2. [DOI] [PubMed] [Google Scholar]
- 53.Bider K, Kaim A, Wiesner W, Bongartz G. Acute appendicitis in a young adult with midgut malrotation: a case report. Eur Radiol. 2001;11:1171–1174. doi: 10.1007/s003300000734. [DOI] [PubMed] [Google Scholar]
- 54.Garg P, Singh M, Marya SK. Intestinal malrotation in adults. Indian J Gastroenterol. 1991;10:103–104. [PubMed] [Google Scholar]
- 55.Rodriguez O, Avilés A, Aquino E, Pérez Arzola M, Cortés F, Monasterio J. Acute abdominal symptoms as the first presentation of a patient with mirror-image dextrocardia with situs inverus. Bol Asoc Med P R. 2006;98:244–248. [PubMed] [Google Scholar]
- 56.Bielecki K, Gregorczyk M, Baczuk L. Visceral situs inversus in three patients. Wiad Lek. 2006;59:707–709. [PubMed] [Google Scholar]
- 57.Tiwari A, MacMull S, Fox S, Jacob SA. Left sided abdominal pain in a patient with situs inversus. Clin Anat. 2006;19:154–155. doi: 10.1002/ca.20201. [DOI] [PubMed] [Google Scholar]
- 58.Contini S, Dalla Valle R, Zinicola R. Suspected appendicitis in situs inversus totalis: an indication for a laparoscopic approach. Surg Laparosc Endosc. 1998;8:393–394. [PubMed] [Google Scholar]
- 59.Prasad V. Left sided appendicitis and situs inversus. Indian J Gastroenterol. 1992;11:44–45. [PubMed] [Google Scholar]
- 60.Pillay SP. Perforated appendix in situs inversus viscerum. A case report. S Afr Med J. 1976;50:141–143. [PubMed] [Google Scholar]
- 61.Holgersen LO, Kuehner CR, Stanley-Brown EG. Acute appendicitis in a child with complete situs inversus. J Pediatr Surg. 1970;5:379–380. doi: 10.1016/0022-3468(70)90198-3. [DOI] [PubMed] [Google Scholar]
- 62.Abel WG 3rd. Acute appendicitis with concomitant situs inversus; report of a case. N Engl J Med. 1949;241:97. doi: 10.1056/NEJM194907212410304. [DOI] [PubMed] [Google Scholar]
- 63.Çelik F, Güleç S, Gökçora İH. A case of acute appendicitis with situs inversus totalis simulating ureteral colic. Turk J Med Sci. 1986;4:147–148. [Google Scholar]
- 64.Chang KS. Acute appendicitis in situs inversus. Ultrasound Med Biol. 2009;35 Suppl:S163. [Google Scholar]
- 65.Palanivelu C, Rangarajan M, John SJ, Senthilkumar R, Madhankumar MV. Laparoscopic appendectomy for appendicitis in uncommon situations: the advantages of a tailored approach. Singapore Med J. 2007;48:737–740. [PubMed] [Google Scholar]