Abstract
AIM: To investigate whether fresh frozen plasma (FFP) transfusion affects outcomes following hepatic resection for hepatocellular carcinoma (HCC) in terms of liver function, postoperative complications and cancer prognosis.
METHODS: We retrospectively compared the incidence of postoperative complications between 204 patients who underwent hepatectomy for HCC with routine FFP transfusion in an early period (1983-1993, Group A) and 293 with necessity for FFP transfusion during a later period (1998-2006, Group B), and also between two subgroups of Group B [22 patients with FFP transfusion (Group B1) and 275 patients without FFP transfusion (Group B2)]. Additionally, only in limited patients in Group B1 and Group B2 with intraoperative blood loss ≥ 2000 mL (Group B1≥ 2000 mL and Group B2≥ 2000 mL), postoperative complications, liver function tests, and cancer prognosis were compared.
RESULTS: No mortality was registered in Group B, compared to 8 patients (3.9%) of Group A. The incidence of morbidity in Group B2 [23.2% (64/275)] was not significantly different from Group B1 [40.9% (9/22)] and Group A [27.0% (55/204)]. The incidence of complications and postoperative liver function tests were comparable between Group B1≥ 2000 mL vs Group B2≥ 2000 mL. Postoperative prognosis did not correlate with administration of FFP, but with tumor-related factors.
CONCLUSION: The outcome of hepatectomy for HCC is not influenced by FFP transfusion. We suggest FFP transfusion be abandoned in patients who undergo hepatectomy for HCC.
Keywords: Fresh frozen plasma, Hepatocellular carcinoma, Surgery, Transfusion
INTRODUCTION
Surgical resection is the established optimal treatment for hepatocellular carcinoma (HCC) associated with hepatitis B virus or hepatitis C virus infection. Since HCC usually develops in patients with liver cirrhosis, most such patients present with bleeding tendencies based on chronic liver dysfunction[1,2]. Accordingly, bleeding is a major problem in liver surgery for HCC, and it also affects postoperative mortality and morbidity[3-5].
Fresh frozen plasma (FFP) is human donor plasma, and contains near normal levels of many plasma proteins, including procoagulants and inhibitory components of the coagulation cascades, acute phase proteins, immunoglobulins and albumin. The clinical use of FFP has increased steadily over the last two decades in many countries[6-8]. Furthermore, in the surgical treatment of HCC, FFP has been frequently administered to supply coagulation factors, maintain serum albumin level and circulating blood volume, and prevent postoperative hepatic failure[9-12]. On the other hand, FFP transfusion is reported to induce adverse effects in some patients: transmission of infection, allergic reactions, hemolysis, anaphylaxis, and transfusion-related acute lung injury (TRALI)[13-15]. Moreover, some studies have reported a relationship between perioperative transfusion and postoperative HCC recurrence[16,17]. In addition to these adverse effects, the amount of FFP is limited because of its source from human donation. Therefore, appropriate use of FFP is needed in terms of application and volume, as stated in the guidelines of the Japanese Ministry of Health, Labour and Welfare[18]. Regarding surgery for HCC, recent advances in both surgical and anesthetic techniques that have led to a reduction in intraoperative blood loss, have resulted indirectly in a gradual decrease in the need for FFP perioperatively[19,20]. Considering the reduction in intraoperative blood loss and the aforementioned potential adverse effects of FFP transfusion, we believe there is no need for FFP in surgery for HCC. In order to discuss this need, we first should investigate whether FFP transfusion affects outcomes following hepatic resection for HCC.
In this study, we retrospectively investigate whether FFP transfusion affects outcomes following hepatic resection for HCC in terms of liver function, postoperative complications and cancer prognosis.
MATERIALS AND METHODS
Trends in transfusion
Until 1993, FFP was routinely administered to patients after hepatectomy for HCC at the Department of Surgery, Osaka University Hospital. In 1994, HCC patients began to donate their blood preoperatively for autologous blood transfusion during or after surgery. Between 1994 and 1997, the use of autologous blood transfusion and FFP transfusion was determined by the surgeon. However, in 1998, the use of autologous blood transfusion was implemented in our institution to cover all HCC patients with hemoglobin of ≥ 11.0 g/dL. FFP was administered only to patients with extensive bleeding intraoperatively and low levels of coagulation factors. After the publication of Guidelines by the Japanese Ministry of Health and Welfare, we adhered to these guidelines in the use of FFP[18].
Patients
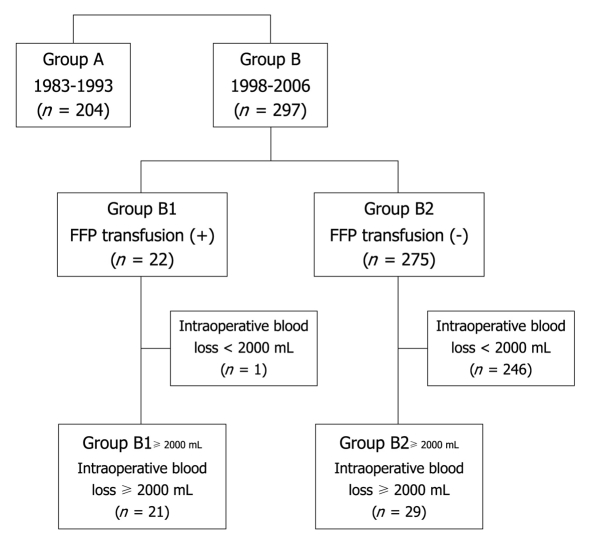
Between 1998 and 2006, 297 patients underwent curative hepatic resection for HCC in our institution. In this study, we retrospectively compared the incidence of postoperative complications and postoperative cancer prognosis in the 297 patients with those of 204 patients with HCC who underwent curative hepatic resection with the routine use of FFP between 1983 and 1993. These 204 patients and 297 patients were categorized into Group A and Group B, respectively. The 297 patients of Group B were also divided into two groups depending on their history regarding perioperative FFP transfusion: 22 patients (7.4%) with FFP transfusion (Group B1) and 275 patients (92.6%) without FFP transfusion (Group B2). The distribution of patients enrolled in this study is illustrated accordingly in Figure 1. In patients of Group B1, FFP transfusion was performed either during the surgery or within 3 d after surgery. The median number of total units of transfused FFP was 10 (range, 4-40). In these groups, the need and validity of routine FFP transfusion were retrospectively evaluated based on the following postoperative complications and cancer prognosis.
Figure 1.
Distribution of the enrolled patients according to the clinical background of hepatectomy for hepatocellular carcinoma. FFP: Fresh frozen plasma.
Surgery and postoperative complications
In our institution, indication for hepatectomy for HCC is based on the value of indocyanine green retention rate at 15 min, and five factors included in the Child-Pugh classification: albumin, prothrombin time (PT), total bilirubin (T-Bil), presence of ascites, and presence of encephalopathy. The selected surgical procedure was based on tumor location and predicted residual liver function, according to the classification system of the Liver Cancer Study Group of Japan[21]. The indication for surgery and selection of surgical procedure were not different between Group A and Group B. Death within 30 d after surgery was considered operative mortality. Morbidities were represented by the following complications that required additional treatment: cardiopulmonary complications, hepatic failure, bleeding, bile leakage, ascites and/or pleural effusion, ileus, and wound infection. PT and T-Bil [preoperative, postoperative day (POD) 1, 3, 5, 7] were used as representative markers of postoperative liver function.
Statistical analysis and ethical considerations
Differences between groups were assessed by the χ2 test, Fisher’s exact test or the Mann-Whitney U test. Survival rates were calculated according to the Kaplan and Meier method and compared using the log-rank test. Statistical analysis was performed using StatView (version 5.0, SAS Institute Inc., Cary, NC). A P value < 0.05 was considered statistically significant. The study was approved by the Human Ethics Review Committee of Osaka University Hospital and a signed consent form was obtained from each patient.
RESULTS
Table 1 lists the differences in perioperative characteristics between Group A and Group B. Patients classified as Child-Pugh A were significantly more common among Group A than Group B (P = 0.0176). Intraoperative blood loss in Group A was significantly greater than in Group B (P < 0.0001). While the postoperative mortality was 3.9% (8/204) in Group A, no mortality was recorded in Group B (P = 0.0007). The incidence of postoperative complications was 27.0% (55/204) in Group A and 24.6% (73/297) in Group B, and the incidence did not significantly differ between the two groups.
Table 1.
Comparison of perioperative characteristics between Group A (1983-1993) and Group B (1998-2006), and between Group B1 and Group B2 n (%)
| Group A (1983-1993) (n = 204) | Group B (1998-2006) (n = 297) | P-value |
Group B |
P-value | ||
| Group B1 (n = 22) | Group B2 (n = 275) | |||||
| Age (yr) | ||||||
| < 60 | 114 (55.9) | 207 (69.7) | 0.0015 | 9 (40.9) | 81 (29.5) | NS |
| ≥ 60 | 90 (44.1) | 90 (30.3) | 13 (59.1) | 194 (70.5) | ||
| Gender | ||||||
| Male | 178 (87.3) | 235 (79.1) | 0.0188 | 20 (90.9) | 215 (78.2) | NS |
| Female | 26 (12.7) | 62 (20.9) | 2 (9.1) | 60 (21.8) | ||
| Child-Pugh | ||||||
| A | 187 (91.7) | 251 (84.5) | 0.0176 | 17 (77.3) | 234 (85.1) | NS |
| B | 17 (8.3) | 46 (15.5) | 5 (22.7) | 41 (14.9) | ||
| Viral infection | ||||||
| HBV (+) | 40/201 (19.9) | 56 (18.9) | NS | 4 (18.2) | 52 (18.9) | NS |
| HCV (+) | 47/78 (60.3) | 177 (59.6) | NS | 11 (40.9) | 166 (61.1) | NS |
| Surgical procedure | ||||||
| ≤ Hr1 | 171 (83.8) | 241 (81.1) | NS | 14 (63.6) | 227 (82.5) | 0.0436 |
| ≥ Hr2 | 33 (16.2) | 56 (18.9) | 8 (36.4) | 48 (17.5) | ||
| Intraoperative blood loss (mL) | ||||||
| < 2000 | 133 (65.2) | 247 (83.2) | < 0.0001 | 1 (4.5) | 246 (89.5) | < 0.0001 |
| ≥ 2000 | 71 (34.8) | 50 (16.8) | 21 (95.5) | 29 (10.5) | ||
| Use of FFP | ||||||
| (-) | 0 (0) | 275 (92.6) | < 0.0001 | |||
| (+) | 204 (100.0) | 22 (7.4) | ||||
| Mortality | 8 (3.9) | 0 (0) | 0.0007 | 0 (0) | 0 (0) | -- |
| Morbidity | 55 (27.0) | 73 (24.6) | NS | 9 (40.9) | 64 (23.2) | NS |
HBV: Hepatitis B virus; HCV: Hepatitis C virus; ≤ Hr1: Partial resection, subsegmentectomy, and segmentectomy of the liver; ≥ Hr2: Bisegmentectomy or more; FFP: Fresh frozen plasma; NS: Not significant.
Various perioperative parameters were compared between Group B1 and Group B2 (Table 1). The preoperative factors were similar in the two groups. The incidence of hepatectomy equal to or more than Hr 2 was significantly higher in Group B1 than in Group B2 (P = 0.0436), and a significantly greater intraoperative blood loss was recorded in Group B1 than in Group B2 (P < 0.0001). There was no operative mortality in either of the two groups. The incidence of postoperative complications was 40.9% (9/22) in Group B1 and 23.2% (64/275) in Group B2, and the incidence did not significantly differ between the two groups. No adverse events related to FFP transfusion were found in Group B1. Postoperative complications and liver function were compared between Group B1 and Group B2 only in patients with intraoperative blood loss of ≥ 2000 mL (Group B1≥ 2000 mL: n = 21, Group B2≥ 2000 mL: n = 29). Comparison of clinical features of patients in these two groups is summarized in Table 2. There were no significant differences in the preoperative factors. Intraoperative blood loss and the frequency of administration of red cell concentrates (RCC) in Group B1≥ 2000 mL were significantly more than those in Group B2≥ 2000 mL (P < 0.0001 and P = 0.0004, respectively). Operative mortality was not encountered in the two groups. The incidence of postoperative complications was 42.9% (9/21) in Group B1≥ 2000 mL and 31.0% (9/29) in Group B2≥ 2000 mL. Table 3 lists the types of complications. Neither postoperative hepatic failure nor postoperative bleeding occurred in the two groups.
Table 2.
Comparison of perioperative characteristics between Group B1≥ 2000 mL and Group B2≥ 2000 mL n (%)
| Group B1≥ 2000 mL (n = 21) | Group B2≥ 2000 mL (n = 29) | P-value | |
| Age (yr) | |||
| < 60 | 9 (42.9) | 11 (37.9) | NS |
| ≥ 60 | 12 (57.1) | 18 (62.1) | |
| Gender | |||
| Male | 20 (95.2) | 23 (79.3) | NS |
| Female | 1 (4.8) | 6 (20.7) | |
| Child-Pugh | |||
| A | 17 (81.0) | 21 (72.4) | NS |
| B | 4 (19.0) | 8 (27.6) | |
| Viral infection | |||
| HBV (+) | 5 (23.8) | 3 (10.3) | NS |
| HCV (+) | 9 (42.9) | 19 (65.5) | NS |
| Maximum size of tumor(s) (cm) | 8.3 ± 6.3 | 6.9 ± 4.6 | NS |
| Intrahepatic metastasis | |||
| (-) | 9 (26.8) | 17 (58.6) | NS |
| (+) | 12 (63.2) | 12 (41.4) | |
| Vascular involvement | |||
| (-) | 8 (38.1) | 17 (58.6) | NS |
| (+) | 13 (61.9) | 12 (41.4) | |
| Operative time (min) | 426 ± 154 | 391 ± 130 | NS |
| Intraoperative blood loss (mL) | 5364 ± 1651 | 2854 ± 1056 | < 0.0001 |
| Use of RCC | |||
| (-) | 3 (14.3) | 19 (65.5) | 0.0004 |
| (+) | 18 (85.7) | 10 (34.5) | |
| Surgical procedure | |||
| ≤ Hr1 | 14 (66.7) | 17 (58.6) | NS |
| ≥ Hr2 | 7 (33.3) | 12 (41.4) |
HBV: Hepatitis B virus; HCV: Hepatitis C virus; ≤ Hr1: Partial resection, subsegmentectomy, and segmentectomy of the liver; ≥ Hr2: Bisegmentectomy or more; RCC: Red cell concentrate; NS: Not significant.
Table 3.
Comparison of postoperative complications between Group B1≥ 2000 mL and Group B2≥ 2000 mL n (%)
| Group B1≥ 2000 mL (n = 21) | Group B2≥ 2000 mL (n = 29) | P-value | |
| Mortality | 0 (0) | 0 (0) | -- |
| Morbidity | 9 (42.9) | 9 (31.0) | NS |
| Cardiopulmonary | 2 (9.5) | 0 (0) | |
| Renal dysfunction | 0 (0) | 0 (0) | |
| Hepatic failure | 0 (0) | 0 (0) | |
| Bleeding | 1 (4.8) | 1 (3.4) | |
| Bile leakage | 1 (4.8) | 2 (6.9) | |
| Ascites and/or pleural effusion | 0 (0) | 3 (10.3) | |
| Ileus | 2 (9.5) | 0 (0) | |
| Wound infection | 3 (14.3) | 3 (10.3) |
NS: Not significant.
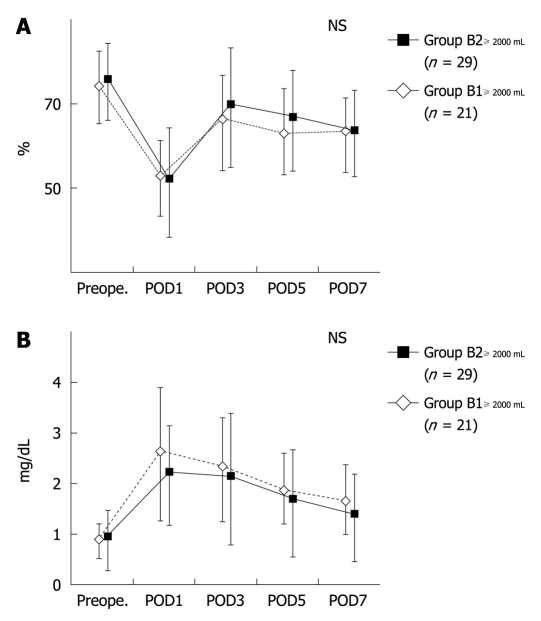
Figure 2 demonstrates the perioperative changes in PT and T-Bil in patients with intraoperative blood loss of ≥ 2000 mL. The levels of PT and T-Bil were not significantly different between the two groups, irrespective of the POD.
Figure 2.
Perioperative changes in (A) serum prothrombin time, and (B) total bilirubin levels in Group B1≥ 2000 mL and Group B2≥ 2000 mL. NS: Not significant; Preope.: Preoperative; POD: Postoperative day.
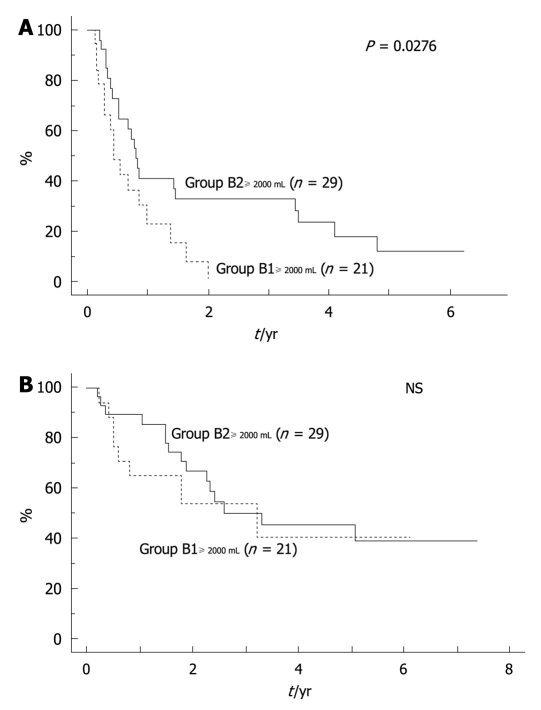
Long-term postoperative outcomes, including disease-free survival (DFS) and overall survival (OS) after hepatic resection, were also examined in patients with intraoperative blood loss of ≥ 2000 mL (Table 4). Vascular invasion (absent/present), FFP transfusion (transfused/non-transfused), tumor size (< 5 cm/≥ 5 cm), RCC transfusion (transfused/non-transfused) were significant factors in univariate analysis of DFS among the clinicopathological factors tested (P = 0.0101, 0.0276, 0.0288, and 0.0343, respectively). Multivariate analysis for DFS using the four factors identified vascular invasion as the only significant independent factor (P = 0.0299). The DFS in Group B2≥ 2000 mL was significantly better than in Group B1≥ 2000 mL (P = 0.0276), though the factor was not significant on multivariate analysis (Figure 3A). Next, univariate analysis for OS using various clinicopathological factors demonstrated that vascular invasion (absent/present) and number of nodules (single/multiple) were significant factors (P = 0.0024 and P = 0.0150, respectively). Multivariate analysis for OS using the two factors, identified vascular invasion as the only significant independent factor (P = 0.0185). There was no significant difference in OS between Group B2≥ 2000 mL and Group B1≥ 2000 mL (P = not significant) (Figure 3B).
Table 4.
Multivariate analysis of disease-free survival and overall survival after hepatectomy for hepatocellular carcinoma in patients with intraoperative blood loss of ≥ 2000 mL
| n |
DFS |
OS |
|||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | ||
| Maximum size of tumor (cm) | 1.553 | 0.755-3.191 | NS | ||||
| ≤ 5 | 16 | ||||||
| > 5 | 31 | ||||||
| Tumor number | 2.280 | 0.874-5.591 | NS | ||||
| Single | 24 | ||||||
| Multiple | 26 | ||||||
| Vascular invasion | 2.445 | 1.091-5.464 | 0.0299 | 3.203 | 1.216-8.439 | 0.0185 | |
| (-) | 25 | ||||||
| (+) | 25 | ||||||
| RCC transfusion | 1.695 | 0.674-4.261 | NS | ||||
| (-) | 22 | ||||||
| (+) | 28 | ||||||
| FFP transfusion | 1.340 | 0.512-3.005 | NS | ||||
| (-) | 29 | ||||||
| (+) | 21 | ||||||
DFS: Disease-free survival; OS: Overall survival; OR: Odds ratio; 95% CI: 95% confidence interval; RCC: Red cell concentrate; FFP: Fresh frozen plasma; NS: Not significant.
Figure 3.
Disease-free survival (A) and overall survival (B) in Group B1≥ 2000 mL and Group B2≥ 2000 mL. NS: Not significant.
DISCUSSION
The present study was designed to investigate whether the outcomes of hepatectomy for HCC are influenced by FFP transfusion. Firstly, we compared the incidence of mortality and morbidity between Group A and Group B, indicating no significant difference in the incidence between the two groups. However, the comparison is considered to be difficult because of differences in the background of each period such as surgical and anesthetic techniques. For example, there were significant differences in liver function evaluated by Child-Pugh classification, and in intraoperative blood loss, between the two groups. Therefore, for more justified analysis, we next compared the outcomes between Group B1 and Group B2. The result showed the incidence of mortality and morbidity to be comparable between Group B1 and Group B2. However, since there were significant differences in the surgical procedure and intraoperative blood loss between the two groups, we also compared the postoperative complications between Group B1≥ 2000 mL vs Group B2≥ 2000 mL. The results showed equal rates of postoperative complications in the two groups. In particular, hepatic failure (prevention of which is one of the purposes of FFP administration) was not identified in the two groups. Postoperative residual liver function, represented by PT and T-Bil, was also equal in the two groups. Furthermore, the incidences of postoperative mortality and morbidity in Group B1 and Group B2 were similar to those reported in other studies[5,22-24]. For example, Imamura et al[5] reported the surgical result of 1056 hepatic resections including 532 HCC cases, with incidences of postoperative mortality and morbidity of 0% and 39.0%, respectively. However, they did not report the number of patients who received FFP. FFP was reported to be administered at a rate that exceeded the amount of blood loss by 10% to 20% during surgery; it substituted the amount of protein lost so as to maintain serum total protein level at 6.0 g/dL in that study. Based on our results and those of early studies, it cannot be concluded that FFP administration would contribute to the incidences of postoperative mortality and morbidity, including hepatic failure.
Although some previous studies have reported postoperative complications after hepatectomy for HCC, there are no reports comparing postoperative complications between patients with FFP transfusion and those without FFP transfusion. Martin et al[25] reported the use of FFP after hepatic resection and suggested criteria for FFP transfusion to deal with postoperative complications after treatment of liver metastasis from colorectal cancer, but not for HCC with liver cirrhosis. Accordingly, their criteria should not be necessarily generalized to the use of FFP in hepatectomy for HCC. Therefore, this study is the first report in which the incidence of postoperative complications in HCC patients was compared between patients who received FFP and those who did not receive FFP transfusion.
To date, FFP has been traditionally used at hepatectomy for the purpose of hemostatic effect by correction of deficiency of coagulation factors and maintenance of circulating blood volume by supplementation of albumin, which is mainly responsible for the colloid osmotic pressure of plasma; in addition to the aforementioned purpose of prevention of hepatic failure[6-8]. Firstly, with regard to the hemostatic effect, recent improvements in surgical techniques allow hepatectomy to be performed with minimal bleeding[19,20]. Moreover, coagulopathy requiring FFP transfusion is generally reported to occur at a PT value of more than 2.0 times the control, whereas the mean PT level of patients of Group B1≥ 2000 mL and Group B2≥ 2000 mL in the present study did not drop to the applicable level, even though it was measured after hepatectomy[26-28]. Furthermore, the incidence of postoperative bleeding was low and was not different in the two groups. Taking these results into consideration, routine administration of FFP is not necessary in terms of the hemostatic effect. Secondly, the maintenance of appropriate circulating blood volume is important in order to prevent certain complications such as pulmonary edema and pre-renal type of renal dysfunction. However, albumin products, which can be administered safely compared to FFP, can be substitutes for FFP in terms of maintenance of circulating blood volume. In fact, albumin products were administered perioperatively instead of FFP in this study, especially in the non-transfused group, and the incidence of these complications was not different between Group B1≥ 2000 mL and Group B2≥ 2000 mL. In this context, routine FFP administration is also suggested not to be necessary in terms of maintenance of the circulating blood volume. Thus, we suggest that the routine administration of FFP for the purpose of prevention of hepatic failure, hemostatic effect, and maintenance of circulating blood volume is not necessary.
Many adverse effects related to FFP transfusion have been identified, such as infection, allergic reactions, hemolysis, anaphylaxis, and TRALI[13-15]. In particular, TRALI, which is a rare and serious complication characterized by sudden onset of respiratory distress due to non-cardiogenic pulmonary edema during or following transfusion, can be life-threatening. Fortunately, none of these transfusion-related complications occurred in our patients. However, since some of the reported adverse events can be life-threatening, one should refrain from inappropriate use of FFP.
Since an initial report by Foster et al[29] about survival advantages in patients undergoing colectomy for colon cancer, several other reports have shown that perioperative homologous blood transfusion to be an independent prognostic factor in many kinds of cancers[16,17,30-33]. However, a few suggested that homologous blood transfusion has no significant effect on the prognosis of cancer patients[34,35]. Thus, the association between transfusion and postoperative prognosis is still under debate. In the present study, postoperative prognosis did not correlate with FFP administration, but rather with tumor-related factors. Although the result was not powerful evidence to resolve the controversy, we can at least confirm that FFP administration does not improve prognosis of patients undergoing hepatectomy for HCC.
In fact, the guidelines of the Japanese Ministry of Health, Labour and Welfare state that administration of FFP should be limited only to supplement coagulation factors in those patients with a PT of more than 2.0 times normal or coagulation factor activity of ≤ 30%, and that the use of FFP for supplementation of circulation blood volume is inappropriate[18]. The guidelines do not mention administration of FFP for the prevention of hepatic failure. Thus, our suggestion is to obey the guidelines. Recently, Kaibori et al[36] reported the clinical value of FFP in surgery for HCC. They suggested that FFP transfusion was useful and recommended on the grounds of the results obtained from their analysis that the incidence of postoperative complications in patients with FFP transfusions was lower than that of patients with FFP and RCC transfusions, and was equal to that of non-transfused patients; long-term survival in patients with FFP transfusions was almost equal to that in non-transfused patients. However, their suggestion is perceived as groundless for the following reasons. To begin with, although there were some significant differences in many factors such as liver function and tumor progression among the groups in their study, they simply suggested that the difference in postoperative complications and long-term outcome resulted from the RCC and FFP transfusions. Secondly, since details of postoperative complications were not shown, especially for hepatic failure, postoperative bleeding, pulmonary edema and renal dysfunction, the examination of correlations between complications and FFP transfusions was insufficient. In addition, their suggestion completely ignored the recent guidelines of Japan.
The present analysis did not include HCC patients who underwent liver transplantation for treatment of liver cirrhosis. Therefore, the result of this study is not applicable to liver transplantation surgery. Considering that transfusion is performed for concomitant liver dysfunction at almost all liver transplantation surgery, it seems to be still too early to discuss the necessity of transfusion in such surgery.
In summary, FFP transfusion did not affect outcomes following hepatic resection for HCC in terms of liver function, postoperative complications and cancer prognosis. Considering the previously reported FFP transfusion-related adverse effects in addition to the results of the present study, we suggest that FFP transfusion be abandoned in patients who undergo hepatectomy for HCC.
COMMENTS
Background
Fresh frozen plasma (FFP) has been frequently administered in the surgical treatment for hepatocellular carcinoma (HCC). Today, appropriate use of FFP is needed in terms of application and FFP transfusion-related potential adverse events. However, to our knowledge, there have been few reports investigating whether FFP transfusion affects outcomes following hepatic resection for HCC or any discussion of the need for FFP in surgery for HCC.
Research frontiers
The incidence of mortality and morbidity, postoperative liver function, and postoperative cancer prognosis were comparable between patients with intraoperative blood loss ≥ 2000 mL who had FFP transfusion and who did not have FFP transfusion.
Innovations and breakthroughs
This study showed that FFP transfusion did not affect outcomes following hepatic resection for HCC in terms of liver function, postoperative complications and cancer prognosis.
Applications
Considering the results of the present study, there is a suggestion that FFP transfusion should be abandoned in patients who undergo hepatectomy for HCC.
Peer review
The manuscript is a well-written paper that is adequately discussed with a reasonable number of literature references. Moreover, the topic is a current and popular one. Conclusions are well supplied by the results and literature.
Footnotes
Peer reviewers: Itaru Endo, MD, PhD, Professor and Chairman, Department of Gastroenterological Surgery, Yokohama City University, Graduate School of Medicine, 3-9 Fukuura, Kanazawa-ku, Yokohama, 2360004, Japan; Ingmar Königsrainer, MD, Department of General, Visceral and Transplant Surgery, Hoppe Seyler Str. 3, 72076 Tübingen, Germany; Dr. Selin Kapan, Associate Professor of General Surgery, Dr. Sadi Konuk Training and Research Hospital, Department of General Surgery, Kucukcekmece, Istanbul 34150, Turkey
S- Editor Tian L L- Editor Logan S E- Editor Zheng XM
References
- 1.Farges O, Malassagne B, Flejou JF, Balzan S, Sauvanet A, Belghiti J. Risk of major liver resection in patients with underlying chronic liver disease: a reappraisal. Ann Surg. 1999;229:210–215. doi: 10.1097/00000658-199902000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsia CY, Lui WY, Chau GY, King KL, Loong CC, Wu CW. Perioperative safety and prognosis in hepatocellular carcinoma patients with impaired liver function. J Am Coll Surg. 2000;190:574–579. doi: 10.1016/s1072-7515(00)00259-3. [DOI] [PubMed] [Google Scholar]
- 3.Nagao T, Inoue S, Goto S, Mizuta T, Omori Y, Kawano N, Morioka Y. Hepatic resection for hepatocellular carcinoma. Clinical features and long-term prognosis. Ann Surg. 1987;205:33–40. doi: 10.1097/00000658-198701000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–406; discussion 406-407. doi: 10.1097/01.SLA.0000029003.66466.B3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, Takayama T, Makuuchi M. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003;138:1198–1206; discussion 1206. doi: 10.1001/archsurg.138.11.1198. [DOI] [PubMed] [Google Scholar]
- 6.Wallace EL. Monitoring the nation's blood supply. Transfusion. 2003;43:299–301. doi: 10.1046/j.1537-2995.2003.00371.x. [DOI] [PubMed] [Google Scholar]
- 7.Stanworth SJ, Brunskill SJ, Hyde CJ, McClelland DB, Murphy MF. Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials. Br J Haematol. 2004;126:139–152. doi: 10.1111/j.1365-2141.2004.04973.x. [DOI] [PubMed] [Google Scholar]
- 8.Stanworth SJ, Hyde CJ, Murphy MF. Evidence for indications of fresh frozen plasma. Transfus Clin Biol. 2007;14:551–556. doi: 10.1016/j.tracli.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Franco D, Smadja C, Kahwaji F, Grange D, Kemeny F, Traynor O. Segmentectomies in the management of liver tumors. Arch Surg. 1988;123:519–522. doi: 10.1001/archsurg.1988.01400280133027. [DOI] [PubMed] [Google Scholar]
- 10.Makuuchi M, Takayama T, Gunvén P, Kosuge T, Yamazaki S, Hasegawa H. Restrictive versus liberal blood transfusion policy for hepatectomies in cirrhotic patients. World J Surg. 1989;13:644–648. doi: 10.1007/BF01658893. [DOI] [PubMed] [Google Scholar]
- 11.Makuuchi M, Kosuge T, Takayama T, Yamazaki S, Kakazu T, Miyagawa S, Kawasaki S. Surgery for small liver cancers. Semin Surg Oncol. 1993;9:298–304. doi: 10.1002/ssu.2980090404. [DOI] [PubMed] [Google Scholar]
- 12.Melendez JA, Arslan V, Fischer ME, Wuest D, Jarnagin WR, Fong Y, Blumgart LH. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg. 1998;187:620–625. doi: 10.1016/s1072-7515(98)00240-3. [DOI] [PubMed] [Google Scholar]
- 13.Isbister JP. Adverse reactions to plasma and plasma components. Anaesth Intensive Care. 1993;21:31–38. doi: 10.1177/0310057X9302100110. [DOI] [PubMed] [Google Scholar]
- 14.MacLennan S, Barbara JA. Risks and side effects of therapy with plasma and plasma fractions. Best Pract Res Clin Haematol. 2006;19:169–189. doi: 10.1016/j.beha.2005.01.033. [DOI] [PubMed] [Google Scholar]
- 15.Bux J, Sachs UJ. The pathogenesis of transfusion-related acute lung injury (TRALI) Br J Haematol. 2007;136:788–799. doi: 10.1111/j.1365-2141.2007.06492.x. [DOI] [PubMed] [Google Scholar]
- 16.Yamamoto J, Kosuge T, Takayama T, Shimada K, Yamasaki S, Ozaki H, Yamaguchi N, Mizuno S, Makuuchi M. Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery. 1994;115:303–309. [PubMed] [Google Scholar]
- 17.Hanazaki K, Kajikawa S, Shimozawa N, Matsushita A, Machida T, Shimada K, Yazawa K, Koide N, Adachi W, Amano J. Perioperative blood transfusion and survival following curative hepatic resection for hepatocellular carcinoma. Hepatogastroenterology. 2005;52:524–529. [PubMed] [Google Scholar]
- 18.Japanese Ministry of Health, Labour and Welfare. Blood transfusion guideline. 3rd ed. Tokyo: Jiho Co; 2005. [Google Scholar]
- 19.Poon RT. Recent advances in techniques of liver resection. Surg Technol Int. 2004;13:71–77. [PubMed] [Google Scholar]
- 20.Makuuchi M, Imamura H, Sugawara Y, Takayama T. Progress in surgical treatment of hepatocellular carcinoma. Oncology. 2002;62 Suppl 1:74–81. doi: 10.1159/000048280. [DOI] [PubMed] [Google Scholar]
- 21.Liver Cancer Study Group of Japan. General rules for the clinical and pathological study of primary liver cancer (in Japanese), 5th ed. Tokyo: Kanehara; 2008. [Google Scholar]
- 22.Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, Kubota K, Zucchi A. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg. 1999;134:984–992. doi: 10.1001/archsurg.134.9.984. [DOI] [PubMed] [Google Scholar]
- 23.Wei AC, Tung-Ping Poon R, Fan ST, Wong J. Risk factors for perioperative morbidity and mortality after extended hepatectomy for hepatocellular carcinoma. Br J Surg. 2003;90:33–41. doi: 10.1002/bjs.4018. [DOI] [PubMed] [Google Scholar]
- 24.Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg. 2004;240:698–708; discussion 708-710. doi: 10.1097/01.sla.0000141195.66155.0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin RC 2nd, Jarnagin WR, Fong Y, Biernacki P, Blumgart LH, DeMatteo RP. The use of fresh frozen plasma after major hepatic resection for colorectal metastasis: is there a standard for transfusion? J Am Coll Surg. 2003;196:402–409. doi: 10.1016/S1072-7515(02)01752-0. [DOI] [PubMed] [Google Scholar]
- 26.Hellstern P, Haubelt H. Indications for plasma in massive transfusion. Thromb Res. 2002;107 Suppl 1:S19–S22. doi: 10.1016/s0049-3848(02)00147-0. [DOI] [PubMed] [Google Scholar]
- 27.O'Shaughnessy DF, Atterbury C, Bolton Maggs P, Murphy M, Thomas D, Yates S, Williamson LM. Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol. 2004;126:11–28. doi: 10.1111/j.1365-2141.2004.04972.x. [DOI] [PubMed] [Google Scholar]
- 28.Holland LL, Foster TM, Marlar RA, Brooks JP. Fresh frozen plasma is ineffective for correcting minimally elevated international normalized ratios. Transfusion. 2005;45:1234–1235. doi: 10.1111/j.1537-2995.2005.00184.x. [DOI] [PubMed] [Google Scholar]
- 29.Foster RS Jr, Costanza MC, Foster JC, Wanner MC, Foster CB. Adverse relationship between blood transfusions and survival after colectomy for colon cancer. Cancer. 1985;55:1195–1201. doi: 10.1002/1097-0142(19850315)55:6<1195::aid-cncr2820550610>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 30.Crowe JP, Gordon NH, Fry DE, Shuck JM, Hubay CA. Breast cancer survival and perioperative blood transfusion. Surgery. 1989;106:836–841. [PubMed] [Google Scholar]
- 31.Little AG, Wu HS, Ferguson MK, Ho CH, Bowers VD, Segalin A, Staszek VM. Perioperative blood transfusion adversely affects prognosis of patients with stage I non-small-cell lung cancer. Am J Surg. 1990;160:630–632; discussion 633. doi: 10.1016/s0002-9610(05)80762-7. [DOI] [PubMed] [Google Scholar]
- 32.Tartter PI. The association of perioperative blood transfusion with colorectal cancer recurrence. Ann Surg. 1992;216:633–638. doi: 10.1097/00000658-199212000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Motoyama S, Saito R, Kamata S, Kitamura M, Okuyama M, Imano H, Nakamura M, Suzuki H, Omokawa S, Motohashi Y, et al. Survival advantage of using autologous blood transfusion during surgery for esophageal cancer. Surg Today. 2002;32:951–958. doi: 10.1007/s005950200191. [DOI] [PubMed] [Google Scholar]
- 34.Voogt PJ, van de Velde CJ, Brand A, Hermans J, Stijnen T, Bloem R, Leer JW, Zwaveling A, van Rood JJ. Perioperative blood transfusion and cancer prognosis. Different effects of blood transfusion on prognosis of colon and breast cancer patients. Cancer. 1987;59:836–843. doi: 10.1002/1097-0142(19870215)59:4<836::aid-cncr2820590430>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 35.Donohue JH, Williams S, Cha S, Windschitl HE, Witzig TE, Nelson H, Fitzgibbons RJ Jr, Wieand HS, Moertel CG. Perioperative blood transfusions do not affect disease recurrence of patients undergoing curative resection of colorectal carcinoma: a Mayo/North Central Cancer Treatment Group study. J Clin Oncol. 1995;13:1671–1678. doi: 10.1200/JCO.1995.13.7.1671. [DOI] [PubMed] [Google Scholar]
- 36.Kaibori M, Saito T, Matsui K, Yamaoka M, Kamiyama Y. Impact of fresh frozen plasma on hepatectomy for hepatocellular carcinoma. Anticancer Res. 2008;28:1749–1755. [PubMed] [Google Scholar]