After years of debate, Le Douarin's elegant work (1) established that pancreatic islet cells differentiate from progenitors emerging from the definitive gut endoderm rather than from neuroectoderm as had been inferred from co-expression of neuronal markers. Although islet cells and the brain do not share a common developmental origin, a fascinating picture has emerged in which they nonetheless share many biochemical pathways and, hence, are characterized by extensive overlap in gene expression. Brain and islet are also tightly linked functionally through neural-entero-islet, brain-islet, and islet-brain axes (2,3). Thus, the secretion of insulin and other islet hormones are clearly regulated by the hypothalamus and other brain areas, while conversely insulin action in the hypothalamus influences both energy balance (4) and glucose metabolism (5). Not surprisingly, therefore, targeted deletion or induction of genes in either tissue can yield mice with overlapping phenotypes where hormone secretion and glucose metabolism are concerned. The report by Wicksteed et al. (6) in this issue of Diabetes sheds welcome light on the extent to which commonly used mouse models for β-cell–specific gene targeting affect gene expression in the brain as well as in the islet.
A commonly employed strategy for gene targeting in vivo employs the Cre/LoxP system of DNA recombination that allows for either deletion or de novo induction of select gene-coding sequences in specific cell types in mice (7–9). Tissue specificity with this method is achieved through the use of cell type-specific promoters to drive expression of Cre recombinase, an enzyme that cleaves DNA sequences between flanking LoxP sites. These promoters can be further modified to incorporate drug-responsive elements, allowing Cre recombinase expression to be switched on at will by drugs such as tamoxifen (CreERT). The Cre/LoxP system has thus emerged as an essential strategy with which to investigate the spatial and temporal function of a given gene (10–13) and has also helped define cell lineage relationships through the induction of reporter genes (14–16).
The capacity to alter islet cell function by directing Cre expression to specific cell populations has been widely and productively employed by diabetes investigators (for a complete list of transgenic mice directing expression of Cre in pancreatic cell populations, refer to http://www.findmice.org/index.jsp and http://www.informatics.jax.org/). Commonly employed mouse models use either the rat insulin2 promoter (RIP) or the Pdx1 promoter to drive Cre recombinase in β-cells. Of three commonly used RIP-Cre mouse lines, Cre is expressed constitutively in two, while expression is tamoxifen-inducible in the third (17–19). Similarly, Cre expression is constitutive in three of four published Pdx1-Cre mouse lines, while it is tamoxifen-inducible in the fourth (20–23).
Because of differences in the timing of Cre-recombinase expression, Pdx1-Cre mouse lines have been labeled “early” or “late” recombinants (e.g., Pdx1-CreEarly [21]) and Pdx1-CreLate [19]). The difference in timing of recombination is important since in addition to other key variables (e.g., tissue distribution and degree of recombination), the age at which altered gene expression occurs can have a dramatic impact on phenotypic outcomes. This effect is illustrated in a study (24) in which the use of Cre-LoxP technology to introduce a stable mutant of β-catenin within the mouse pancreatic epithelium had opposite effects depending on the spatial and temporal pattern of gene induction (25). Thus, when this form of β-catenin was expressed during early organogenesis using Pdx1-CreEarly mice (21), a severe reduction of pancreas mass associated with postnatal lethality was observed (due to the loss of Pdx1 expression in early pancreatic progenitors). By comparison, induction at a later time point using Pdx1-CreLate mice (19) increased cellular proliferation and induced a dramatic increase of pancreas organ size (24). Should Cre recombinase be expressed in other tissues, therefore, the phenotypic consequence may also depend on the age at which recombination occurs.
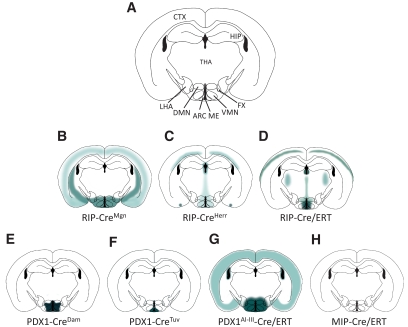
In this issue of Diabetes, Wicksteed et al. (6) compared Cre activity in the brain of commonly used mouse models with that observed using a new mouse line generated using a tamoxifen-inducible mouse insulin1 promoter to drive Cre expression (MIP-Cre/ERT). The investigators report that each of the three commonly used RIP-Cre transgenic lines exhibit Cre-mediated recombination in the brain (Fig. 1). In one of these mouse lines (RIP-CreMgn) (18) (Fig. 1B), 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside (X-gal) staining was detected throughout the brain with the highest intensity in the midbrain and ventral regions, whereas RIP-CreHerr mice displayed a weaker and more punctate central nervous system expression pattern without obvious regionalization (19) (Fig. 1C). The tamoxifen-inducible RIP-Cre/ERT mouse (17) also displayed strong, punctate X-gal staining in the brain but with a more restricted expression pattern (Fig. 1D). Analysis of Pdx1-Cre lines also revealed X-gal staining in the brain, including one (Pdx1-CreEarly) (21) (Fig. 1E) in which Cre activity was detected in distinct hypothalamic neuronal subsets important in metabolic regulation, including both orexin-expressing neurons and neurons shown to be activated by leptin. Since expression of genes targeted using these mouse lines will be altered in the brain as well as in the pancreas, these findings offer a cautionary note to the interpretation of resultant phenotypes.
FIG. 1.
Schematic representation of Cre expression in a coronal section taken through the mid-hypothalamus of mice with pancreas-targeted Cre drivers that were crossed with the R26R β-galactosidase Cre reporter line. Shaded areas depict regions of Cre-mediated recombination based subjectively on findings reported by Wicksteed et al. (6). A: R26Rwt/lacZ without a Cre driver. B: RIP-CreMgn; R26Rwt/lacZ. C: RIP-CreHerr; R26Rwt/lacZ. D: RIP-Cre/ERT; R26Rwt/lacZ. E: PDX1-CreDam; R26Rwt/lacZ. F: PDX1-CreTuv; R26Rwt/lacZ. G: PDX1AI-III-Cre/ERT; R26Rwt/lacZ. H: MIP-Cre/ERT; R26Rwt/lacZ. Until more is known regarding the reproducibility of these expression patterns, this depiction is intended only as a general guide. Investigators using these mice are advised to evaluate central nervous system Cre-mediated recombination on a case-by-case basis. ARC, arcuate nucleus; CTX, cortex; DMN, dorsomedial nucleus; FX, formix; HIP, hippocampus; LHA, lateral hypothalamic area; ME, median area eminence; THA, thalamus; VMN, ventro-medial nucleus.
Compared with the above Cre models, the new MIP-Cre/ERT mice described by Wicksteed et al. display a more β-cell–specific recombination pattern with virtually undetectable Cre activity in any brain regions analyzed (Fig. 1H). As this mouse model also features a tamoxifen-inducible Cre, it offers the potential for both temporal and tissue-specific control of gene deletion (or induction) in pancreatic β-cells and, hence, is a welcome addition to the repertoire of animal models used by the diabetes research community. Whether efficient Cre-mediated recombination in MIP-Cre/ERT mice can be achieved in utero and therefore can be used to target select genes during β-cell development is a question that awaits further study.
Although somewhat tangential to the question at hand, it seems perplexing that the rat insulin2 promoter, but not the mouse insulin1 promoter, is active in the mouse brain. Several factors likely contribute to this discrepancy, including the additional regulatory elements within the larger promoter fragment employed in MIP-Cre/ERT mice, but an important conclusion supported by this finding is that the insulin gene does not appear to be expressed in adult mammalian brain. This finding adds to a literature that strongly supports this conclusion despite papers that appear from time to time implying the opposite (most recently in the Alzheimer disease literature) (26).
It seems likely that the question of whether altered neuronal gene expression influenced the phenotype of various published RIP-Cre or Pdx1-Cre mouse models will soon be answered. In the meantime, however, RIP-Cre and Pdx1-Cre models will continue to be important tools for the study of islet development and function as long as a neural contribution to a particular phenotype can be reliably excluded, and improvements in this technology will undoubtedly continue. As this progress unfolds, we are reminded that the close functional link between brain and islet can be a source of confusion and frustration, as well as one of fascination.
ACKNOWLEDGMENTS
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 3090.
REFERENCES
- 1.Le Douarin NM: On the origin of pancreatic endocrine cells. Cell 1988;53:169–171 [DOI] [PubMed] [Google Scholar]
- 2.Rohner-Jeanrenaud F, Bobbioni E, Ionescu E, Sauter JF, Jeanrenaud B: Central nervous system regulation of insulin secretion. Adv Metab Disord 1983;10:193–220 [DOI] [PubMed] [Google Scholar]
- 3.Atouf F, Czernichow P, Scharfmann R: Expression of neuronal traits in pancreatic beta cells. Implication of neuron-restrictive silencing factor/repressor element silencing transcription factor, a neuron-restrictive silencer. J Biol Chem 1997;272:1929–1934 [DOI] [PubMed] [Google Scholar]
- 4.Schwartz MW, Figlewicz DP, Baskin DG, Woods SC, Porte D, Jr: Insulin in the brain: a hormonal regulator of energy balance. Endocr Rev 1992;13:387–414 [DOI] [PubMed] [Google Scholar]
- 5.Obici S, Zhang BB, Karkanias G, Rossetti L: Hypothalamic insulin signaling is required for inhibition of glucose production. Nat Med 2002;8:1376–1382 [DOI] [PubMed] [Google Scholar]
- 6.Wicksteed B, Brissova M, Yan W, Opland DM, Plank JL, Reinert RB, Dickson LM, Tamarina NA, Philipson LH, Shostak A, Bernal-Mizrachi E, Elghazi L, Row MW, Labosky PA, Myers MM, Jr, Gannon M, Powers AC, Dempsey PJ: Conditional gene targeting in mouse pancreatic β-cells: analysis of ectopic Cre transgene expression in the brain. Diabetes 2010;59:3090–3098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sauer B: Manipulation of transgenes by site-specific recombination: use of Cre recombinase. Methods Enzymol 1993;225:890–900 [DOI] [PubMed] [Google Scholar]
- 8.Marth JD: Recent advances in gene mutagenesis by site-directed recombination. J Clin Invest 1996;97:1999–2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajewsky K, Gu H, Kühn R, Betz UA, Müller W, Roes J, Schwenk F: Conditional gene targeting. J Clin Invest 1996;98:600–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metzger D, Clifford J, Chiba H, Chambon P: Conditional site-specific recombination in mammalian cells using a ligand-dependent chimeric Cre recombinase. Proc Natl Acad Sci U S A 1995;92:6991–6995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feil R, Brocard J, Mascrez B, LeMeur M, Metzger D, Chambon P: Ligand-activated site-specific recombination in mice. Proc Natl Acad Sci U S A 1996;93:10887–10890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li M, Indra AK, Warot X, Brocard J, Messaddeq N, Kato S, Metzger D, Chambon P: Skin abnormalities generated by temporally controlled RXRalpha mutations in mouse epidermis. Nature 2000;407:633–636 [DOI] [PubMed] [Google Scholar]
- 13.Vasioukhin V, Degenstein L, Wise B, Fuchs E: The magical touch: genome targeting in epidermal stem cells induced by tamoxifen application to mouse skin. Proc Natl Acad Sci U S A 1999;96:8551–8556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herrera PL: Defining the cell lineages of the islets of Langerhans using transgenic mice. Int J Dev Biol 2002;46:97–103 [PubMed] [Google Scholar]
- 15.Seymour PA, Freude KK, Dubois CL, Shih HP, Patel NA, Sander M: A dosage-dependent requirement for Sox9 in pancreatic endocrine cell formation. Dev Biol 2008;323:19–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thorel F, Népote V, Avril I, Kohno K, Desgraz R, Chera S, Herrera PL: Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature 2010;464:1149–1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dor Y, Brown J, Martinez OI, Melton DA: Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature 2004;429:41–46 [DOI] [PubMed] [Google Scholar]
- 18.Postic C, Shiota M, Niswender KD, Jetton TL, Chen Y, Moates JM, Shelton KD, Lindner J, Cherrington AD, Magnuson MA: Dual roles for glucokinase in glucose homeostasis as determined by liver and pancreatic beta cell-specific gene knock-outs using Cre recombinase. J Biol Chem 1999;274:305–315 [DOI] [PubMed] [Google Scholar]
- 19.Herrera PL: Adult insulin- and glucagon-producing cells differentiate from two independent cell lineages. Development 2000;127:2317–2322 [DOI] [PubMed] [Google Scholar]
- 20.Offield MF, Jetton TL, Labosky PA, Ray M, Stein RW, Magnuson MA, Hogan BL, Wright CV: PDX-1 is required for pancreatic outgrowth and differentiation of the rostral duodenum. Development 1996;122:983–995 [DOI] [PubMed] [Google Scholar]
- 21.Gu G, Dubauskaite J, Melton DA: Direct evidence for the pancreatic lineage: NGN3+ cells are islet progenitors and are distinct from duct progenitors. Development 2002;129:2447–2457 [DOI] [PubMed] [Google Scholar]
- 22.Hingorani SR, Petricoin EF, Maitra A, Rajapakse V, King C, Jacobetz MA, Ross S, Conrads TP, Veenstra TD, Hitt BA, Kawaguchi Y, Johann D, Liotta LA, Crawford HC, Putt ME, Jacks T, Wright CV, Hruban RH, Lowy AM, Tuveson DA: Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell 2003;4:437–450 [DOI] [PubMed] [Google Scholar]
- 23.Zhang H, Fujitani Y, Wright CV, Gannon M: Efficient recombination in pancreatic islets by a tamoxifen-inducible Cre-recombinase. Genesis 2005;42:210–217 [DOI] [PubMed] [Google Scholar]
- 24.Heiser PW, Lau J, Taketo MM, Herrera PL, Hebrok M: Stabilization of beta-catenin impacts pancreas growth. Development 2006;133:2023–2032 [DOI] [PubMed] [Google Scholar]
- 25.Harada N, Tamai Y, Ishikawa T, Sauer B, Takaku K, Oshima M, Taketo MM: Intestinal polyposis in mice with a dominant stable mutation of the beta-catenin gene. EMBO J 1999;18:5931–5942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rivera EJ, Goldin A, Fulmer N, Tavares R, Wands JR, de la Monte SM: Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer's disease: link to brain reductions in acetylcholine. J Alzheimers Dis 2005;8:247–268 [DOI] [PubMed] [Google Scholar]