Abstract
OBJECTIVE
The purpose of the current study was to determine whether double-stranded adeno-associated virus (dsAAV)-mediated in vivo expression of β-cell growth factors, glucagon-like peptide-1 (GLP-1) and the NK1 fragment of hepatocyte growth factor (HGF/NK1) in β-cells, improves pathology in the db/db mouse model of type 2 diabetes.
RESEARCH DESIGN AND METHODS
The glucoregulatory actions of GLP-1 and full-length HGF are well characterized. Here, we test the ability of HGF/NK1 to induce proliferation of exogenous islets and MIN6 β-cells. In addition, we target both GLP-1 and HGF/NK1 to endogenous β-cells using dsAAV vectors containing the mouse insulin-II promoter. We compare the abilities of these gene products to induce islet proliferation in vitro and in vivo and characterize their abilities to regulate diabetes after AAV-mediated delivery to endogenous islets of db/db mice.
RESULTS
Recombinant HGF/NK1 induces proliferation of isolated islets, and dsAAV-mediated expression of both GLP-1 and HGF/NK1 induces significant β-cell proliferation in vivo. Furthermore, both GLP-1 and HGF/NK1 expressed from dsAAV vectors enhance β-cell mass and insulin secretion in vivo and significantly delay the onset of hyperglycemia in db/db mice.
CONCLUSIONS
A single treatment with dsAAV vectors expressing GLP-1 or HGF/NK1 enhances islet growth and significantly improves pathology in a mouse model of type 2 diabetes. This represents the first example of a successful use of HGF/NK1 for diabetes therapy, providing support for direct AAV-mediated in vivo delivery of β-cell growth factors as a novel therapeutic strategy for the treatment of type 2 diabetes.
Apromising therapeutic for type 2 diabetes is the incretin family of proteins, particularly glucagon-like peptide-1 (GLP-1) (1). GLP-1 has a variety of glucoregulatory actions, which include enhancing insulin synthesis and secretion, improving insulin sensitivity, inhibiting glucagon secretion, and increasing β-cell mass (2). However, GLP-1 is rapidly degraded by the ubiquitous enzyme, dipeptidyl peptidase-IV, and thus has a short in vivo half-life that limits its therapeutic efficacy (3). We have recently shown that adeno-associated virus (AAV) administration of GLP-1 provides long-term, high-level GLP-1 expression, offering an alternative approach to peptide therapy (4).
Another protein that has potential as a therapeutic for diabetes is hepatocyte growth factor (HGF). HGF is involved in the regeneration of multiple organs, including the liver, kidney, and lung (5), and a number of studies illustrate the efficacy of HGF in animal models of diabetes (6–10). Transgenic mice specifically overexpressing HGF in β-cells exhibit increased β-cell proliferation, function, and survival (5), and HGF improves islet transplant outcome in rodent models (6,7). Moreover, HGF has previously been delivered to isolated islets via adenovirus gene transfer, reducing β-cell death, reducing the minimal islet mass required for successful transplant, and improving overall transplant outcome (8,9).
While full-length HGF has beneficial effects in animal models of diabetes, recent research has focused specifically on the N and K1 domains of HGF (HGF/NK1). HGF/NK1 comprises the NH2-terminal 175 amino acids of HGF and is sufficient for binding and partial activation of the HGF receptor, as well as initiation of some mitogenic activity (11–13). HGF/NK1 has not previously been studied in relation to diabetes but may provide several advantages over full-length HGF. HGF/NK1 may improve the safety profile compared with full-length HGF by limiting stimulation of the HGF receptor, Met. Another advantage of using HGF/NK1 instead of full-length HGF is the ability to use double-stranded AAV (dsAAV) vectors for gene delivery. dsAAV vectors provide rapid, efficient, and stable gene expression (14), without the immunogenicity associated with adenovirus vectors. However, dsAAV vectors have limited packaging capacity, thus preventing their use for delivery of full-length HGF.
The majority of studies using gene transfer strategies to enhance islet function or survival have used ex vivo transduction protocols. However, in vivo transduction of β-cells has been achieved by direct targeting of genes to β-cells of pancreatic islets using dsAAV vectors (4,15). There are many benefits of direct in vivo gene transfer compared with transduction of islets for transplantation, as well as compared with existing therapeutics. First of all, the applicability of islet transplantation is reduced by the limited availability of islets. Secondly, while existing antidiabetic agents and incretin drugs have therapeutic efficacy, they are often associated with adverse effects and multiple daily administrations. Direct in vivo gene transfer could be cost-effective and beneficial to patients' quality of life because it may be therapeutic in as little as a single treatment.
Here, we examine whether in vivo delivery of the growth factors GLP-1 and HGF/NK1 via dsAAV-mediated gene transfer can improve pathology in a mouse model of type 2 diabetes. We demonstrate that dsAAV-expressed GLP-1 and HGF/NK1 enhance islet proliferation and delay onset of diabetes in db/db mice, providing the first evidence that HGF/NK1 is a potential therapeutic for diabetes.
RESEARCH DESIGN AND METHODS
Cells, plasmids, and viruses.
The MIN6 β-cell line was a gift from Dr. Jun-ichi Miyazaki of the Osaka University Medical School. MIN6 cells were cultured in high-glucose Dulbecco's modified Eagle's medium supplemented with 10% FBS, 100 units/ml penicillin, and 100 μg/ml streptomycin at 37°C in a 5% CO2 atmosphere.
The plAdeno5 adenovirus helper plasmid, the AAV8 helper plasmid expressing the AAV8 cap and AAV2 rev genes, and the double-stranded AAV8 plasmid expressing enhanced green fluorescent protein (eGFP) flanked by inverted-terminal repeats under the control of the cytomegalovirus (CMV) promoter were gifts of Dr. Hiroyuki Nakai of the University of Pittsburgh. cDNA for full-length murine HGF was a gift from Dr. Andrew Stewart of the University of Pittsburgh. The NK1 fragment of HGF was obtained by PCR using primers 5′-CATCAGACCGGTGGATCCAGCCATGATGTGGGGGACCAAACTTCT and 5′-GCGGCCGCGGATCCCTATTACAACTTGTATGTCAAAATTACTTTGTGTATCC, which introduced AgeI and NotI sites, respectively. The dsAAV–CMV–eGFP expression plasmid was subsequently modified to express our transgenes of interest under the control of the murine preproinsulin-II promoter (MIP). The CMV promoter was excised using restriction enzymes MluI and KpnI. Subsequently, plasmid expressing genes of interest expressed between Adeno-associated virus inverted terminal repeats (pAAV)–MIP–GLP1 was generated by excising eGFP with restriction enzymes AgeI and XbaI, as previously described (4), and pAAV–MIP–HGF/NK1 was generated by excising eGFP with AgeI and NotI.
Recombinant dsAAV vectors were generated according to the triple transfection protocol as previously described (16). Briefly, HEK293 cells were transfected with the plAdeno5, AAV8 helper, and dsAAV expression plasmids. Virions were purified by double CsCl gradient centrifugation, and viral genomes were quantitated by dot blot analysis. For the remainder of this manuscript, these vectors will be referred to as dsAAV–eGFP, dsAAV–GLP1, and dsAAV–NK1, respectively.
Animal studies.
Female C57BL/6 and db/db mice were obtained from Jackson Laboratories (Bar Harbor, ME). All experiments were approved by the University of Pittsburgh Animal Care and Use Committee. Mice were maintained on a standard 12 h light/dark cycle and received a standard diet. Infections were carried out at a dose of 4 × 1011 viral genomes (vg) per mouse. Viruses were administered intraperitoneally in a total volume of 800 μl of sterile saline solution supplemented with 5% sorbitol. Insulin tolerance tests were performed by intraperitoneal administration of 1 unit/kg of insulin (gift of Dr. Rita Bottino, University of Pittsburgh Diabetes Institute) after a 6-h fast. Blood glucose monitoring was carried out at indicated time points on restrained, unanesthetized animals via tail vein bleeds.
Mouse islet isolation.
Ex vivo islet growth studies were performed using islets freshly isolated from 6-week-old female C57BL/6 mice. Islets were isolated as previously described (17). Briefly, after laparotomy, cold collagenase (type V, 1.75 mg/ml, Sigma Chemical Co., St. Louis, MO) was used to inflate the pancreas via injection into the common bile duct. After inflation, the pancreas was removed and incubated for 20 min at 37°C. Islets were purified by Ficoll density gradient centrifugation and hand-picked under a stereomicroscope, and the purity of the islets was determined by Dithizone staining. Islets were maintained in RPMI-1640 media supplemented with 10% heat inactivated FBS, 2 mmol/l l-glutamine, 100 units/ml penicillin, and 100 μg/ml streptomycin in a humidified 5% CO2 incubator at 37°C.
Tritiated-thymidine proliferation assays.
Recombinant HGF (rHGF) and recombinant HGF/NK1 (rNK1) were gifts of Dr. Donald Bottaro of the National Institutes of Health. Freshly isolated islets were plated at 100 islets/well in six well dishes and treated with 10 μg or 20 μg of rHGF or rNK1, respectively, for a period of 96 h. After incubation with recombinant proteins, islets were washed and incubated at 37°C and 5% CO2 overnight in complete media containing 1 μCi of 3H-thymidine. Islets were subsequently washed and lysed. Lysates were absorbed onto fiberglass filter paper, and counts per min were obtained using a Wallac 1,205 Betaplate liquid scintillation counter (PerkinElmer, Waltham, MA).
ELISAs.
MIN6 β-cells were grown to 80% confluency in a 6-well dish, then infected with dsAAV–eGFP, dsAAV–GLP1, or dsAAV–NK1 in Dulbecco's modified Eagle's medium supplemented with 10% FBS and incubated at 37°C and 5% CO2 for 12–24 h. Media was then removed from the cells, and protein secretion was measured via ELISA. For GLP-1, the GLP-1(7–36) Active ELISA Kit (Linco Research, St. Charles, MO) was used. The anti-sera in this assay cross-react 100% with GLP-1(7–37), GLP-1(7–36), and GLP-1(9–36). The detection limit of this assay is 3 mmol l−1. For HGF, a standard sandwich ELISA was developed using anti-HGFα (N-17) (Santa Cruz Biotechnology, Santa Cruz, CA) as the capture antibody and biotinylated anti-mHGF (R&D Systems, Minneapolis, MN) as the detection antibody. Each of these antibodies recognizes the NH2 terminus of HGF, including the NK1 domain, and rNK1 was used to generate the standard curve. The limit of detection of this assay was ∼0.1 pg/ml.
Circulating insulin concentrations were determined from db/db mouse serum samples at 14 weeks of age (10 weeks post-treatment) using a mouse Insulin Elisa kit (ALPCO, Salem, NH). The sensitivity of this assay is 0.06 ng/ml.
Wounding assays.
MIN6 β-cells were grown to near confluency in 12-well plates. A defined area of the monolayer was disrupted with a sterile instrument, and the size was measured microscopically. Cells were then infected with the eGFP or HGF/NK1 virus or were treated with rHGF or rNK1. Wound size was measured again at 24 and 48 h post-treatment. MetaMorph software (Molecular Devices, Sunnyvale, CA) was used to measure wound size at each time point.
Microscopy.
Immunoflourescence staining was carried out on paraffin-embedded tissue sections. Antigen retrieval was performed prior to incubation with the primary antibodies. For anti-GLP1/insulin double staining, sections were incubated with a mixture of primary antibodies against GLP-1 (mouse monoclonal; Abcam, Cambridge, MA) and insulin (guinea pig polyclonal; Abcam, Cambridge, MA). After incubation with the primary antibodies and three washes, the mixture of secondary antibodies, consisting of Alexa-488-conjugated rabbit anti-mouse IgG (Molecular Probes, Eugene, OR) and Cy3-conjugated donkey anti-guinea pig IgG (Jackson ImmunoResearch, West Grove, PA), were added. Cell nuclei were counterstained with DAPI (Sigma, St. Louis, MO). In addition, multiple antibodies against HGF were unsuccessfully tested for their ability to detect HGF via immunofluorescence, including goat anti-HGFα (N-17) (Santa Cruz Biotechnology, Santa Cruz, CA), rabbit anti-HGFα (H-145) (Santa Cruz Biotechnology, Santa Cruz, CA), and goat anti-mHGF (R&D Systems, Minneapolis, MN). Lack of HGF detection via immunofluorescence is likely due to poor immunoreactivity of the tested antibodies in this protocol.
The relative β-cell area was determined by measuring the areas of insulin-stained islets using MetaMorph software (Molecular Devices, Sunnyvale, CA). β-cell mass was determined using the following formula: β-cell mass (mg) = area of insulin-stained islets/total pancreatic area × total pancreas weight.
Statistical analyses.
Statistical analysis was performed using the Stata 8.2 (STATA, College Station, TX) software package, and the data collected are expressed as mean ± SEM. For most analyses, P values were determined using the Student t test. The percentage of nondiabetic mice was calculated by Kaplan–Meier survival analysis. A P value of <0.05, arrived at using ANOVA and log rank test, was considered to indicate a statistically significant difference.
RESULTS
Recombinant HGF/NK1 enhances islet proliferation ex vivo.
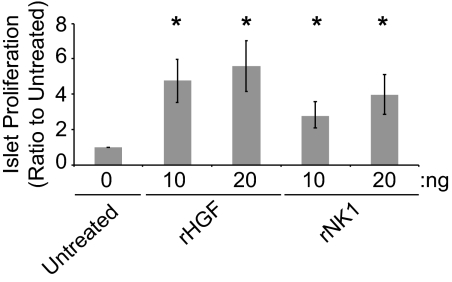
Previous research has shown that both GLP-1 and full-length HGF are capable of enhancing the mass of murine islets (6,18). To use HGF/NK1 for insertion into AAV vectors with limited packaging potential, we examined the ability of rNK1 to stimulate proliferation of islets compared with rHGF. Islets were isolated from 6-week-old female C57BL/6 mice as described in the Research Design and Methods and subsequently treated for 96 h with the indicated concentrations of rHGF or rNK1 (Fig. 1). After 96 h, levels of islet proliferation were measured using a 3H-thymidine proliferation assay. As expected, full-length rHGF provided the maximum observed levels of islet proliferation, at ∼4.5- to 5.5-fold above background. Moreover, rNK1 induced significant increases in islet proliferation at the 10 and 20 ng doses, ∼2.75- and 4-fold above background, respectively. Interestingly, the difference in proliferation induced by rHGF and rNK1 at the 20 ng dose was not statistically significant. This suggests that, at higher doses, the proliferation-inducing potential of HGF/NK1 may be similar to that of full-length HGF in islets.
FIG. 1.
rHGF/rNK1 induces proliferation of islets ex vivo. Freshly isolated islets were treated with 10 or 20 ng of rHGF or rNK1 for a period of 96 h. Islet proliferation was determined by measuring 3H-thymidine incorporation. Data are expressed as the fold change above untreated cells ± SEM for three independent experiments. *P < 0.05 relative to untreated islets.
Expression of GLP1 and HGF/NK1 from dsAAV vectors in MIN6 β-cells.
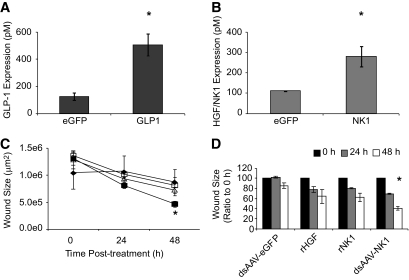
To determine whether local expression of GLP-1 and HGF/NK1 in endogenous β-cells would promote β-cell proliferation and improve diabetes pathology, dsAAV8 vectors were generated expressing GLP-1 (dsAAV–GLP1) or HGF/NK1 (dsAAV–NK1) under the regulation of the MIP, as described in Research Design and Methods. Additionally, dsAAV–eGFP was generated and used as a negative control. To measure expression of the β-cell growth factors from the viruses, MIN6 β-cells were infected at a dose of 5 × 104 vg/cell. At 24 h postinfection, the levels of GLP-1 and HGF/NK1 secreted into the media were determined using ELISA. The levels of GLP-1 secreted from MIN6 cells infected with dsAAV–GLP1 (508 ± 81 pmol/l) were ∼4 times greater than levels detected in cells infected with the dsAAV–eGFP (124 ± 27 pmol/l; Fig. 2A). Similarly, infection with dsAAV–NK1 resulted in a 2.5-fold increase in HGF/NK1 expression (285 ± 51 pmol/l) compared with cells infected with the eGFP control virus (113 ± 1.8 pmol/l; Fig. 2B).
FIG. 2.
Biologically active HGF/NK1 is expressed from a dsAAV8 vector at levels similar to GLP-1. dsAAV vectors express high levels of GLP-1 (A) and HGF/NK1 (B) in MIN6 β-cells. C: Wounding assays were performed using MIN6 β-cells to assess the biological activity of dsAAV-expressed HGF/NK1. dsAAV-NK1 (black squares) induced the greatest wound restitution compared with dsAAV–eGFP (black diamonds), rHGF (open triangles), and rNK1 (open squares). D: dsAAV–NK1 induced an ∼30% reduction in wound size at 24 h postinfection (gray bars) and an ∼60% reduction in wound size at 48 h postinfection (white bars) compared with initial wound size (black bars). Data depict means of three independent experiments ± SEM. *P < 0.05.
It is known that full-length HGF enhances healing of wounded CCL53.1 cell monolayers (19). Thus, to measure the activity of HGF/NK1 expressed from the dsAAV vector, wounding assays were performed using MIN6 cells as described in Research Design and Methods. The effects on wound size at 24 and 48 h post-treatment with rHGF, rNK1, dsAAV–eGFP, and dsAAV–NK1 were calculated as the ratio to the original wound size at 0 h. As shown in Fig. 2C and D, a decrease in wound size at 24 and 48 h was observed after treatment with rHGF, rNK1, and dsAAV–NK1, but not dsAAV–eGFP. The greatest restitution of the wound was observed in dsAAV–NK1-infected samples, improving from a wound size at 0 h of 130 × 104 ± 12 × 104 μm2 to 81 × 104 ± 5.8 × 104 μm2 at 24 h (31% decrease), and 46 × 104 ± 5.2 × 104 μm2 at 48 h (60% decrease). These results demonstrate the biological activity of HGF/NK1 expressed from the AAV-transduced MIN6 cells.
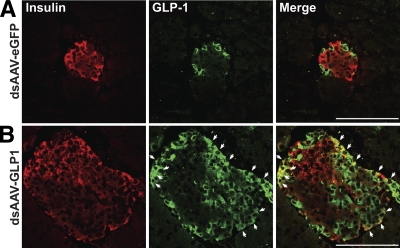
Expression of GLP1 from dsAAV vectors is restricted to islets.
Expression of transgenes under the control of the MIP should restrict expression to insulin-producing β-cells. To examine the tissue-specific expression of GLP-1 and HGF/NK1, pancreas sections from db/db mice at 10 weeks post-treatment with dsAAV-GLP1 and dsAAV-NK1 were stained for GLP-1 and HGF/NK1. Expression was analyzed via immunofluorescence confocal microscopy, as described in Research Design and Methods. We have previously demonstrated that the anti-GLP-1 antisera used in this study cross-reacts with proglucagon, thereby marking all α-cells, as well as cells expressing immunoreactive GLP-1 (4). To identify β-cells expressing viral-encoded GLP-1, sections were costained with insulin. Only mice treated with dsAAV–GLP1 (Fig. 3) contained cells that were immunoreactive for both insulin and GLP-1 (white arrows), with 8.5 ± 1.5% of β-cells expressing GLP-1. However, expression of HGF/NK1 was not observed in islets via immunofluorescence (not shown), due to poor immunoreactivity of the antibodies against the NK1 fragment tested in this method. Furthermore, no GLP-1, HGF/NK1, or eGFP expression was observed in liver or spleen (not shown), indicating that these viruses are specific for insulin-producing β-cells.
FIG. 3.
dsAAV-expressed GLP-1 is localized to insulin-producing β-cells. Expression of GLP-1 in db/db mice treated with dsAAV–eGFP (A) and dsAAV–GLP1 (B) was examined by immunofluorescence at 14 weeks of age, or 10 weeks post-treatment. Islets from mice treated with dsAAV–GLP1 contained examples of β-cells (indicated by white arrows) that were positive for both GLP-1 (green) and insulin (red). Islets from mice treated with dsAAV–eGFP contained no examples of GLP-1 and insulin double-positive cells, indicating that the green staining observed in these samples is glucagon from pancreatic α-cells. Data are representative of at least two sections per mouse, n = 10 mice per group. Scale bar = 100 μm in all images. (A high-quality digital representation of this figure is available in the online issue.)
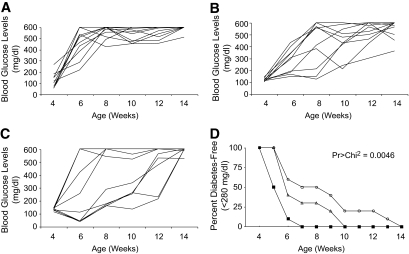
In vivo expression of GLP-1 and HGF/NK1 delays onset of diabetes in db/db mice.
To examine possible therapeutic effects of GLP-1 and HGF/NK1 expression from endogenous β-cells on the course of type 2 diabetes, 4-week-old female db/db mice were treated with a single intraperitoneal injection of dsAAV–eGFP, dsAAV–GLP1, or dsAAV–NK1 and blood glucose levels were monitored weekly until all mice developed diabetes. As shown in Fig. 4A and D, 100% of mice receiving the eGFP control virus developed diabetes by 7 weeks of age. However, treatment with the GLP-1 virus significantly delayed onset of disease, with mice remaining normoglycemic as late as 10 weeks of age (Fig. 4B and D). An even greater effect was observed in animals receiving the HGF/NK1 virus (Fig. 4C and D), with animals remaining normoglycemic as late as 14 weeks of age, twice as long as control mice. These data show that, although the frequency of onset of hyperglycemia was not reduced, a single treatment with AAV expressing β-cell growth factors was sufficient to prolong normoglycemia in db/db mice.
FIG. 4.
GLP-1 and HGF/NK1 gene transfer prolong normoglycemia in db/db mice. Four-week-old female db/db mice were injected intraperitoneally with 4 × 1011 vg of dsAAV–eGFP (A; n = 10), dsAAV–GLP1 (B; n = 10), or dsAAV–NK1 (C; n = 10), and blood glucose levels were monitored weekly until all mice became hyperglycemic. D: The percentage of diabetes-free animals, defined as having blood glucose levels < 280 mg/dl, are plotted against age. Although there was no difference in the incidence of diabetes, there was a significant delay in the onset in mice treated with dsAAV–GLP1 (open triangles) and dsAAV–NK1 (open circles) compared with dsAAV–eGFP-infected control animals (black squares). A P value of <0.005 by log rank test analysis was used to indicate a statistically significant percentage of normoglycemic animals.
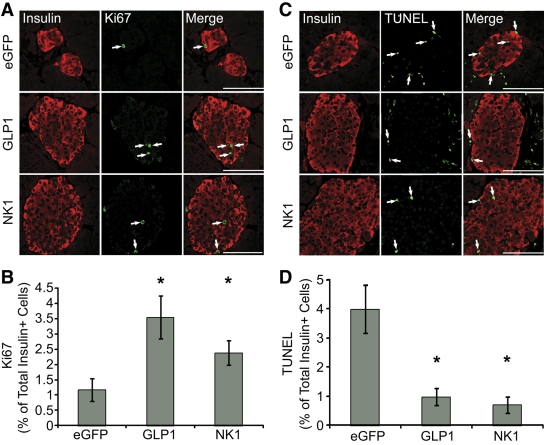
GLP-1 and HGF/NK1 gene transfer enhances β-cell proliferation and survival in db/db mice.
GLP-1 and HGF have previously been shown to promote β-cell proliferation and survival (2,6–10). To determine whether dsAAV-mediated expression of these growth factors has a similar effect in db/db mice, β-cell proliferation was measured in db/db mice at 10 weeks postinfection with dsAAV–eGFP, dsAAV–GLP1, or dsAAV–NK1 by analysis of Ki67+/insulin+ cells in pancreatic sections (Fig. 5A). Figure 5B shows quantification of Ki67 expression, illustrating a significant increase in Ki67+ β-cells after infection with the GLP-1 and NK1 viruses.
FIG. 5.
Gene transfer of GLP-1 and HGF/NK1 increase β-cell proliferation in db/db mice. A: Pancreatic sections from db/db mice infected with dsAAV–eGFP, dsAAV–GLP, or dsAAV–NK1 were stained for insulin (red) and the proliferation marker, Ki67 (green). Arrowheads indicate cells that are double-positive for insulin and Ki67. B: Quantification of Ki67-positive β-cells, expressed as the mean percentage of Ki67-positive, insulin-positive cells in 20–40 individual islets from each group. *P < 0.05. C: Pancreatic sections from db/db mice infected with dsAAV–eGFP, dsAAV–GLP, or dsAAV–NK1 were stained for insulin (red) and subjected to TUNEL staining (green). Arrowheads indicate cells that are double-positive for insulin and TUNEL. D: Quantification of TUNEL-positive β-cells, expressed as the mean percentage of TUNEL-positive, insulin-positive cells in 20–40 individual islets from each treatment group. *P < 0.002. For all images, magnification = ×40, scale bars = 100 μm. (A high-quality digital representation of this figure is available in the online issue.)
Transferase-mediated dUTP nick-end labeling (TUNEL) staining was performed on pancreatic sections from db/db mice at 10 weeks post-treatment to measure β-cell survival. As shown in Fig. 5C and D, there was a significant decrease in the percentage of TUNEL+/insulin+ cells after infection with dsAAV–GLP1 and dsAAV–NK1, compared with the control virus. Taken together, these results suggest that dsAAV-mediated expression of GLP-1 and HGF/NK1 promotes β-cell proliferation and survival in db/db mice.
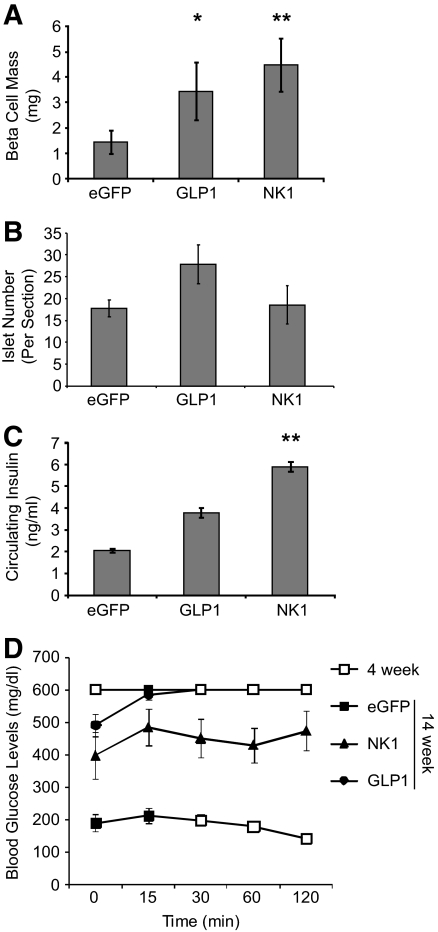
dsAAV-mediated expression of GLP-1 and HGF/NK1 increases β-cell mass in db/db mice.
Enhanced β-cell proliferation and survival after infection with dsAAV-expressing GLP-1 and HGF/NK1 suggests an increase in β-cell mass in response to these growth factors. Therefore, β-cell mass was analyzed at 14 weeks of age. There was a significant increase in β-cell mass in db/db mice (Fig. 6A) treated with dsAAV–GLP1 (3.4 ± 1.1 mg) and dsAAV–NK1 (4.5 ± 1.0 mg), compared with control mice (1.5 ± 0.5 mg).
FIG. 6.
GLP-1 and HGF/NK1 gene transfer increases β-cell mass and insulin secretion in db/db mice. A: β-Cell mass was evaluated as described in Research Design and Methods. B: The average numbers of islets in db/db mice did not differ significantly among any of the three treatments. Data are presented as the mean ± SEM of at least two sections per mouse, n = 10 mice per group. C: ELISAs performed on serum from treated mice revealed a significant increase in circulating insulin levels in db/db mice treated with dsAAV–NK1. The increased insulin after dsAAV–GLP1 administration was not statistically significant (P = 0.054). D: Intraperitoneal insulin tolerance tests performed at the time of treatment (4 weeks of age) and 10 weeks post-treatment (14 weeks of age), as described in Research Design and Methods, indicate insulin resistance at each time point. *P < 0.05; **P < 0.01.
In addition to larger islets, GLP-1 and HGF have been indicated to promote β-cell neogenesis. When combined with the suppression of β-cell apoptosis (Fig. 5), this may lead to increased numbers of islets (2,6). To determine whether dsAAV–GLP1 and dsAAV–NK1 increase overall numbers of islets, tissue sections from treated mice were analyzed for numbers of islets and compared with control mice. As shown in Fig. 6B, there was a modest, but not significant, increase in numbers of islets in mice treated with dsAAV–GLP1 but not dsAAV–NK1, compared with mice receiving dsAAV–eGFP. Taken together, data in Figures 4 and 5 indicate that the observed increase in β-cell mass is due to enhanced proliferation of β-cells in existing islets, not β-cell neogenesis.
β-Cell-specific expression of GLP-1 and HGF/NK1 increases insulin secretion, but not insulin sensitivity, in db/db mice.
Previous research has shown that GLP-1 and HGF are capable of increasing insulin synthesis and secretion, as well as enhancing insulin sensitivity (2,5). Serum insulin levels were evaluated in 14-week-old db/db mice (Fig. 6C). There was a significant increase in basal circulating insulin levels in mice treated with dsAAV–NK1 compared with dsAAV–eGFP. In addition, there was a modest, but not significant (P = 0.054), increase in basal circulating insulin in mice treated with dsAAV–GLP1.
To evaluate insulin sensitivity, intraperitoneal insulin tolerance tests were performed as described in Research Design and Methods. At the time of treatment (4 weeks of age, open symbols), db/db mice were already insulin-resistant (Fig. 6D). Furthermore, by 14 weeks of age (closed symbols), infection with dsAAV vectors expressing eGFP, GLP-1, and HGF/NK1 was not able to overcome the severe insulin resistance.
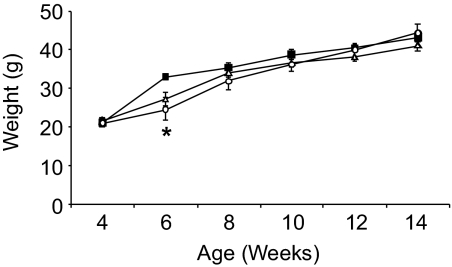
In vivo expression of GLP-1 and HGF/NK1 does not affect weight of obese db/db mice.
GLP-1 inhibits gastric emptying and gastric acid secretion in humans and rodent models, leading to decreased food intake and reduced body weight (18,20). To assess the effects of dsAAV-expressed GLP-1 and HGF/NK1 on body weight, the weights of db/db mice treated at 4 weeks of age were monitored weekly (Fig. 7). At 6 weeks of age, there was a modest, but statistically significant, difference in body weights, with dsAAV–GLP1- and dsAAV–NK1-infected mice weighing ∼7–10 g less than mice treated with dsAAV–eGFP. However, there was no difference in body weight at any other time point.
FIG. 7.
dsAAV-mediated expression of GLP-1 and HGF/NK1 does not affect the weight of obese db/db mice. The weights of female db/db mice treated with dsAAV–eGFP (black squares; n = 10), dsAAV–GLP1 (open triangles; n = 10), and dsAAV–NK1 (open circles; n = 10) were monitored weekly. A significant difference in weights of dsAAV–GLP1 and dsAAV–NK1 infected mice was observed at 6 weeks of age but at no other time points. *P < 0.05.
DISCUSSION
We demonstrated previously that dsAAV8 vectors provide long-term, stable gene transfer and expression in pancreatic β-cells in C57BL/6 and BALB/c mice (15). Expression of transgenes can be restricted to β-cells by coupling transgene expression to the MIP. Moreover, our dsAAV8 vector expressing GLP-1, driven by the MIP, provides local production and secretion of GLP-1 in pancreatic β-cells and prevents diabetes after multiple low-dose streptozotocin administrations in a mouse model of type 1 diabetes (4).
Here, we examined the efficacy of the GLP-1–expressing dsAAV8 vector as well as a dsAAV8 vector expressing HGF/NK1 in a mouse model for type 2 diabetes. Full-length HGF is a large protein, encoded by an ∼2.2 kb gene. The packaging capacity of dsAAV vectors is restricted to ∼2.5 kb, including gene and promoter, thus preventing expression of the full-length HGF gene. HGF/NK1 possesses about 50% of the mitogenic activity of full-length HGF in hepatocytes (11), but its effects in β-cells have not been examined. Here, we demonstrate that dsAAV8 vectors provide high levels of GLP-1 and HGF/NK1 expression in vitro, and that this expression is specific to β-cells. In addition, while we have previously shown that dsAAV-GLP1 induces β-cell proliferation (4), here we demonstrate that rNK1 and HGF/NK1 expressed from a dsAAV8 vector are capable of inducing β-cell proliferation. Moreover, expression of GLP-1 and HGF/NK1 by endogenous β-cells after dsAAV8 gene transfer enhances β-cell mass in vivo and significantly delays the onset of diabetes in db/db mice.
Gene therapy provides a potentially very useful method of targeted expression of GLP-1 and HGF to β-cells. A number of studies have examined the potential of endogenous expression of GLP-1 and HGF to mitigate diabetes in animal models. Previous studies using GLP-1 gene therapy for type 2 diabetes have primarily used constitutive promoters, such as CMV, chicken β-actin, or ubiquitin promoters, to drive unregulated expression of GLP-1. Although these studies have yielded promising results, with improved insulin sensitivity and lowered blood glucose levels, these treatments have also resulted in high levels of circulating GLP-1, which may promote GLP-1 receptor desensitization over time. The vector used in our study provides the advantage of local GLP-1 expression by using the MIP to restrict expression to β-cells, the primary target of GLP-1 for glucoregulatory activity, and limiting levels of circulating GLP-1 (4).
Diabetes gene therapy also has been attempted using vectors expressing HGF, mostly in ex vivo studies to facilitate islet transplantation. HGF expression has been restricted to islets by using adenovirus vectors driven by the rat insulin promoter, demonstrating that targeted HGF gene transfer reduces β-cell death, reduces the minimal islet mass required for successful transplant, and improves overall transplant outcome (8,9). HGF also can regulate diabetes in a type 2 diabetes mouse model, and HGF gene transfer slows the progression of diabetic nephropathy in db/db mice. Each of these studies has used full-length HGF as a therapeutic gene. Here, we provide the first evidence that HGF/NK1 has therapeutic efficacy in an animal model of diabetes. HGF/NK1 may provide several advantages over full-length HGF. The receptor for HGF is Met, which is encoded by the proto-oncogene, c-Met. Although the HGF-Met pathway is known to play a role in tumorigenesis, little is known about the possible role of HGF/NK1 in this pathway. Several studies indicate that HGF/NK1 is antagonistic, suggesting a role for HGF/NK1 as a potential cancer therapy (21,22). Other studies, including work presented here, suggest that HGF/NK1 is a partial agonist, capable of inducing >50% of mitogenic activity of full-length HGF (11–13). The partial agonist effect of HGF/NK1 may have a role in improving its safety profile compared with full-length HGF. Indeed, while transgenic mice that systemically overexpress HGF/NK1 developed complications similar to those seen in full-length HGF transgenic mice, including increased susceptibility to some cancers, the HGF/NK1 phenotypes were significantly less severe than those seen in full-length HGF transgenic mice (13). Moreover, transgenic mice overexpressing HGF specifically in β-cells have not been associated with increased risk of tumorigenesis (A.F. Stewart, personal communication), suggesting that localized expression of HGF and HGF/NK1 may further enhance their safety.
Another advantage of using HGF/NK1 instead of full-length HGF is the ability to use dsAAV vectors for gene delivery. All of the GLP-1 and HGF gene transfer studies cited above have used adenovirus vectors. Whereas adenovirus vectors provide rapid and efficient gene transfer, their immunogenicity limits their therapeutic potential. Although the packaging capacity of dsAAV vectors is limited, a variety of factors contribute to the attractiveness of these vectors for gene transfer. First of all, AAV has not been associated with any disease or pathology. Furthermore, unlike adenovirus, there is a lack of a significant immune response directed against the AAV vector, contributing to the ability of the vectors to persist in vivo (23,24). AAV vectors also provide long-term transgene expression, primarily via the formation of double-stranded extrachromosomal (episomal) genomes (25,26). This suggests that dsAAV-mediated production of GLP-1 and HGF/NK1 in β-cells may abrogate the need for repeat administrations, which are required with current therapies.
Our results demonstrate that dsAAV gene transfer of the growth factors, GLP-1 and HGF/NK1, significantly improves pathology in db/db mice. Although the frequency of onset of hyperglycemia was not reduced, a single treatment with dsAAV expressing GLP-1 and HGF/NK1 was sufficient to increase β-cell mass and insulin secretion and prolong normoglycemia. These phenotypes were observed despite suboptimal in vivo expression of GLP-1 and presumably HGF/NK1. This is probably due to the nature of GLP-1 and HGF/NK1, which are secreted paracrine factors that likely influence neighboring islets and untransduced β-cells within each islet. There are a number of methods by which this technique may be optimized to improve expression, thereby possibly improving efficacy. First of all, the dose of 4 × 1011 vg/mouse was chosen to test a low dose of vector expressing a therapeutic transgene. However, we have previously demonstrated that doses as high as 1012 vg of dsAAV8 expressing eGFP were unable to achieve complete transduction of islets, with a gradient of expression observed with higher efficiency in the peripheral zone than in the central zone (15), similar to the GLP-1 expression patterns observed here. Therefore, higher doses of virus may provide enhanced transduction of β-cells. This may be particularly true in obese mice, as additional virus may be necessary to compensate for substantially increased body weight. Furthermore, intraperitoneal injection of virus was chosen for ease of administration. However, we have previously demonstrated that retrograde pancreatic intraductal delivery, which is similar to the commonly used clinical technique of endoscopic retrograde cholangiopancreatography, provides enhanced transduction of β-cells within islets (15). Therefore, this approach, while more complicated in a mouse model, may be superior and more clinically relevant than the more commonly used intraperitoneal injection.
Previous studies indicate that GLP-1 and HGF are capable of enhancing insulin sensitivity (5), and that GLP-1 is capable of regulating food intake, thereby reducing body weight in obese patients (18,27). This was not the case in the studies presented here, as neither GLP-1 nor HGF/NK1 reversed insulin resistance at the tested time points or prevented weight gain in db/db mice. In regard to insulin sensitivity, it is possible that the severity of insulin resistance observed at the time of treatment precluded compensation by the observed functional increase in β-cell mass. It also may be possible that insulin sensitivity was increased sufficiently at earlier times post-treatment to allow the increased levels of circulating insulin to delay the onset of hyperglycemia. Alternatively, the localized expression of these growth factors to the pancreas may prevent their interaction with other tissues, such as lipocytes, muscle, and liver, that are important for controlling insulin sensitivity, thereby preventing the reversal of insulin resistance. Along these same lines, GLP-1 is normally produced in and secreted from intestinal endocrine l-cells, which are located mainly in the distal ileum and colon. GLP-1 then acts locally in the gut to inhibit gastric emptying and gastric acid secretion, leading to decreased food intake and reduced body weight (18,20,28,29). However, restriction of exogenous GLP-1 expression to β-cells likely prevents its gastrointestinal effects, as our previous studies with this vector demonstrate that GLP-1 expressed in β-cells from dsAAV vectors does not increase levels of GLP-1 in circulation (4). Therefore, although more work is necessary to elucidate the complete mechanism, the data presented here demonstrate that dsAAV vectors expressing the growth factors, GLP-1 and HGF/NK1, have potential as novel therapies for type 2 diabetes.
ACKNOWLEDGMENTS
This work was supported by a program grant from the Juvenile Diabetes Research Foundation (JDRF) to P.D.R., and D.F.G. was supported by a fellowship from the JDRF. M.J.R. was supported by the Michael Smith Foundation for Health Research (MSFHR), the Canadian Diabetes Association, the Stem Cell Network, and the JDRF. T.J.K. is a MSFHR senior scholar. S.P.G. was supported by a fellowship from the SASS Foundation for Medical Research. No potential conflicts of interest relevant to this article were reported.
D.F.G. researched data and wrote the manuscript. M.J.R. and S.P.G. reviewed/edited the manuscript and researched data. T.J.K. reviewed/edited the manuscript. P.D.R. wrote the manuscript.
We thank Dr. Maliha Zahid (University of Pittsburgh) for assistance with statistical analysis and Joan Nash (University of Pittsburgh) for assistance with microscopy analysis.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Wideman RD, Kieffer TJ: Mining incretin hormone pathways for novel therapies. Trends Endocrinol Metab 2009;20:280–286 [DOI] [PubMed] [Google Scholar]
- 2.De León DD, Deng S, Madani R, Ahima RS, Drucker DJ, Stoffers DA: Role of endogenous glucagon-like peptide-1 in islet regeneration after partial pancreatectomy. Diabetes 2003;52:365–371 [DOI] [PubMed] [Google Scholar]
- 3.Kieffer TJ, McIntosh CH, Pederson RA: Degradation of glucose-dependent insulinotropic polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase IV. Endocrinology 1995;136:3585–3596 [DOI] [PubMed] [Google Scholar]
- 4.Riedel MJ, Gaddy DF, Asadi A, Robbins PD, Kieffer TJ: DsAAV8-mediated expression of glucagon-like peptide-1 in pancreatic beta-cells ameliorates streptozotocin-induced diabetes. Gene Ther 2010;17:171–180 [DOI] [PubMed] [Google Scholar]
- 5.Matsumoto K, Nakamura T: HGF: its organotrophic role and therapeutic potential. Ciba Found Symp 1997;212:198–211; discussion 211–4 [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Ocaña A, Takane KK, Syed MA, Philbrick WM, Vasavada RC, Stewart AF: Hepatocyte growth factor overexpression in the islet of transgenic mice increases beta cell proliferation, enhances islet mass, and induces mild hypoglycemia. J Biol Chem 2000;275:1226–1232 [DOI] [PubMed] [Google Scholar]
- 7.García-Ocaña A, Vasavada RC, Cebrian A, Reddy V, Takane KK, López-Talavera JC, Stewart AF: Transgenic overexpression of hepatocyte growth factor in the beta-cell markedly improves islet function and islet transplant outcomes in mice. Diabetes 2001;50:2752–2762 [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Talavera JC, Garcia-Ocaña A, Sipula I, Takane KK, Cozar-Castellano I, Stewart AF: Hepatocyte growth factor gene therapy for pancreatic islets in diabetes: reducing the minimal islet transplant mass required in a glucocorticoid-free rat model of allogeneic portal vein islet transplantation. Endocrinology 2004;145:467–474 [DOI] [PubMed] [Google Scholar]
- 9.Rao P, Cozar-Castellano I, Roccisana J, Vasavada RC, Garcia-Ocaña A: Hepatocyte growth factor gene therapy for islet transplantation. Expert opinion on biological therapy 2004;4:507–518 [DOI] [PubMed] [Google Scholar]
- 10.Dai C, Li Y, Yang J, Liu Y: Hepatocyte growth factor preserves beta cell mass and mitigates hyperglycemia in streptozotocin-induced diabetic mice. J Biol Chem 2003;278:27080–27087 [DOI] [PubMed] [Google Scholar]
- 11.Pediaditakis P, Monga SP, Mars WM, Michalopoulos GK: Differential mitogenic effects of single chain hepatocyte growth factor (HGF)/scatter factor and HGF/NK1 following cleavage by factor Xa. J Biol Chem 2002;277:14109–14115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cioce V, Csaky KG, Chan AM, Bottaro DP, Taylor WG, Jensen R, Aaronson SA, Rubin JS: Hepatocyte growth factor (HGF)/NK1 is a naturally occurring HGF/scatter factor variant with partial agonist/antagonist activity. J Biol Chem 1996;271:13110–13115 [DOI] [PubMed] [Google Scholar]
- 13.Jakubczak JL, LaRochelle WJ, Merlino G: NK1, a natural splice variant of hepatocyte growth factor/scatter factor, is a partial agonist in vivo. Mol Cell Biol 1998;18:1275–1283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCarty DM, Fu H, Monahan PE, Toulson CE, Naik P, Samulski RJ: Adeno-associated virus terminal repeat (TR) mutant generates self-complementary vectors to overcome the rate-limiting step to transduction in vivo. Gene Ther 2003;10:2112–2118 [DOI] [PubMed] [Google Scholar]
- 15.Wang Z, Zhu T, Rehman KK, Bertera S, Zhang J, Chen C, Papworth G, Watkins S, Trucco M, Robbins PD, Li J, Xiao X: Widespread and stable pancreatic gene transfer by adeno-associated virus vectors via different routes. Diabetes 2006;55:875–884 [DOI] [PubMed] [Google Scholar]
- 16.Xiao X, Li J, Samulski RJ: Production of high-titer recombinant adeno-associated virus vectors in the absence of helper adenovirus. J Virol 1998;72:2224–2232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bertera S, Crawford ML, Alexander AM, Papworth GD, Watkins SC, Robbins PD, Trucco M: Gene transfer of manganese superoxide dismutase extends islet graft function in a mouse model of autoimmune diabetes. Diabetes 2003;52:387–393 [DOI] [PubMed] [Google Scholar]
- 18.Kieffer TJ, Habener JF: The glucagon-like peptides. Endocr Rev 1999;20:876–913 [DOI] [PubMed] [Google Scholar]
- 19.Nayeri F, Holmgren-Pettersson K, Perskvist N, Forsberg P, Peterson C, Sundqvist T: An in vitro model for assessment of the biological activity of hepatocyte growth factor. Growth Factors 2007;25:33–40 [DOI] [PubMed] [Google Scholar]
- 20.Zander M, Madsbad S, Madsen JL, Holst JJ: Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and beta-cell function in type 2 diabetes: a parallel-group study. Lancet 2002;359:824–830 [DOI] [PubMed] [Google Scholar]
- 21.Youles M, Holmes O, Petoukhov MV, Nessen MA, Stivala S, Svergun DI, Gherardi E: Engineering the NK1 fragment of hepatocyte growth factor/scatter factor as a MET receptor antagonist. J Mol Biol 2008;377:616–622 [DOI] [PubMed] [Google Scholar]
- 22.Lokker NA, Godowski PJ: Generation and characterization of a competitive antagonist of human hepatocyte growth factor, HGF/NK1. J Biol Chem 1993;268:17145–17150 [PubMed] [Google Scholar]
- 23.Dudus L, Anand V, Acland GM, Chen SJ, Wilson JM, Fisher KJ, Maguire AM, Bennett J: Persistent transgene product in retina, optic nerve and brain after intraocular injection of rAAV. Vision Res 1999;39:2545–2553 [DOI] [PubMed] [Google Scholar]
- 24.Xiao X, Li J, Samulski RJ: Efficient long-term gene transfer into muscle tissue of immunocompetent mice by adeno-associated virus vector. J Virol 1996;70:8098–8108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duan D, Sharma P, Yang J, Yue Y, Dudus L, Zhang Y, Fisher KJ, Engelhardt JF: Circular intermediates of recombinant adeno-associated virus have defined structural characteristics responsible for long-term episomal persistence in muscle tissue. J Virol 1998;72:8568–8577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakai H, Yant SR, Storm TA, Fuess S, Meuse L, Kay MA: Extrachromosomal recombinant adeno-associated virus vector genomes are primarily responsible for stable liver transduction in vivo. J Virol 2001;75:6969–6976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baggio LL, Drucker DJ: Biology of incretins: GLP-1 and GIP. Gastroenterology 2007;132:2131–2157 [DOI] [PubMed] [Google Scholar]
- 28.Wettergren A, Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ: Truncated GLP-1 (proglucagon 78–107-amide) inhibits gastric and pancreatic functions in man. Dig Dis Sci 1993;38:665–673 [DOI] [PubMed] [Google Scholar]
- 29.Flint A, Raben A, Astrup A, Holst JJ: Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest 1998;101:515–520 [DOI] [PMC free article] [PubMed] [Google Scholar]