Abstract
OBJECTIVE
Advanced glycation end products (AGEs) and the renin-angiotensin system (RAS) are both implicated in the development of diabetic retinopathy. How these pathways interact to promote retinal vasculopathy is not fully understood. Glyoxalase-I (GLO-I) is an enzyme critical for the detoxification of AGEs and retinal vascular cell survival. We hypothesized that, in retina, angiotensin II (Ang II) downregulates GLO-I, which leads to an increase in methylglyoxal-AGE formation. The angiotensin type 1 receptor blocker, candesartan, rectifies this imbalance and protects against retinal vasculopathy.
RESEARCH DESIGN AND METHODS
Cultured bovine retinal endothelial cells (BREC) and bovine retinal pericytes (BRP) were incubated with Ang II (100 nmol/l) or Ang II+candesartan (1 μmol/l). Transgenic Ren-2 rats that overexpress the RAS were randomized to be nondiabetic, diabetic, or diabetic+candesartan (5 mg/kg/day) and studied over 20 weeks. Comparisons were made with diabetic Sprague-Dawley rats.
RESULTS
In BREC and BRP, Ang II induced apoptosis and reduced GLO-I activity and mRNA, with a concomitant increase in nitric oxide (NO•), the latter being a known negative regulator of GLO-I in BRP. In BREC and BRP, candesartan restored GLO-I and reduced NO•. Similar events occurred in vivo, with the elevated RAS of the diabetic Ren-2 rat, but not the diabetic Sprague-Dawley rat, reducing retinal GLO-I. In diabetic Ren-2 rats, candesartan reduced retinal acellular capillaries, inflammation, and inducible nitric oxide synthase and NO•, and restored GLO-I.
CONCLUSIONS
We have identified a novel mechanism by which candesartan improves diabetic retinopathy through the restoration of GLO-I.
Chronic hyperglycemia is the major causative factor in the pathogenesis of diabetic retinopathy (1) and may injure retinal vascular cells through a number of pathways including the enhanced production of advanced glycation end products (AGEs) (2,3) and activation of the renin-angiotensin system (RAS) (4). In diabetes, there is an impaired glucose handling and increased glucose flux through the glycolytic pathway resulting in the accumulation of the AGE precursor, methylglyoxal (MGO), which is a source of intracellular and plasma AGEs (5). MGO can modify amine groups (such as lysine and arginine residues) resident on key cellular proteins, generating AGE-modified cellular proteins that have negative effects on protein function and gene regulation (6,7), leading to impaired cell function. In diabetic retinopathy, MGO-derived AGEs are elevated in retina and serum and are viewed to be causative in retinal injury (8,9). The glyoxalase (GLO) system, composed of GLO-I and GLO-II, is critical for controlling MGO levels in vivo and, ultimately, MGO-AGEs. However, in diabetes, GLO-I activity is reduced in some tissues and hence implicated in the accumulation of tissue MGO and AGEs and subsequent pathology (10,11). Relevant to diabetic retinopathy, we reported that, in retinal pericytes grown in hyperglycemic conditions, when GLO-I function is impaired, MGO accumulates and pericyte apoptosis occurs (12).
The RAS is a major regulator of blood pressure and also contributes to retinal pathology by stimulating cell death, inflammation, and angiogenesis [reviewed in ref (4)]. The RAS is initiated by prorenin, and its active form, renin, liberates angiotensin I from angiotensinogen. Angiotensin converting enzyme then converts angiotensin I to angiotensin II (Ang II). Both experimental and clinical evidence indicates that Ang II blockade improves aspects of vascular and neuroglial injury in diabetic retinopathy (13–17). Indeed, the recent findings of the DIRECT program (Diabetic Retinopathy Candesartan Trials) indicate that angiotensin type 1 receptor blockade (AT1-RB) with candesartan reduces the incidence of diabetic retinopathy in type 1 diabetic patients and improves the regression of retinal disease in type 2 diabetic patients (18,19).
Despite the positive findings of DIRECT, AT1-RB did not normalize retinal pathology. This may be due to Ang II's interactions with other pathways such as AGEs to induce organ pathology (20–23). In terms of diabetic retinopathy, the few studies that have evaluated this relationship have focused on extracellular events where Ang II increases AGEs and the receptor for AGEs (RAGE)-induced apoptosis of retinal pericytes (24). However, there is little understanding about how intracellular AGEs, such as those generated from MGO through GLO-I inactivation, are influenced by the RAS in diabetic retinopathy. In the present study, we hypothesized that Ang II stimulates the downregulation of retinal GLO-I with a subsequent increase in MGO formation, leading to increased MGO-AGEs and vascular damage in diabetic retinopathy. We also evaluated whether candesartan's protective effects in diabetic retinopathy involves restoration of retinal GLO-I. Studies were performed in transgenic (mRen-2)27 (Ren-2) rats, which overexpress the RAS in extrarenal tissues, are hypertensive and develop accelerated retinopathy compared with Sprague-Dawley rats when made diabetic with streptozotocin (13,15,25). To more directly evaluate the relationship between Ang II and GLO-I in retinal vascular cells, studies were performed in cultured bovine retinal endothelial cells (BREC) and bovine retinal pericytes (BRP). Furthermore, given that we have identified that nitric oxide (NO•) is a regulator of GLO-I activity in retinal pericytes (12), we determined if Ang II's modulation of retinal GLO-I is associated with changes in retinal NO•.
RESEARCH DESIGN AND METHODS
Tissue culture experiments. Culture of BREC and BRP.
BREC and BRP were cultured as previously described (26). Passage numbers were between 3 and 6 for BREC and 3 and 7 for BRP. See the online appendix available at http://diabetes.diabetesjournals.org/cgi/content/full/db10-0552/DC1 for details regarding treatment of cells with Ang II and candesartan.
BREC and BRP apoptosis.
BRP apoptosis was quantitated by flow cytometry by double staining with annexin-fluorescein isothiocyanate (FITC) and propidium iodide (TACS AnnexinV-FITC Apoptosis Detection kit, R&D Systems, Minneapolis, USA) as previously described (12). BREC apoptosis was not assessed by flow cytometry, as it has been reported that the quantitation of apoptosis in BREC by this method is unreliable (27). BREC apoptosis was conducted in 96-well plates and detected by transferase-mediated dUTP nick-end labeling (TUNEL) staining using an In Situ Cell Death Detection kit (Roche Diagnostics, NSW, Australia) according to the manufacturer's instructions. Cells were counterstained with 300 nmol/l DAPI for 1 min to visualize the nucleus. Three nonoverlapping fields/well were captured using a Nikon Eclipse TE2000-U microscope coupled to a Digital Sight camera (Nikon, Melville, NY, USA) and interfaced with a computer running NIS Elements F2.20 (Nikon).
GLO-I activity and expression in BREC and BRP.
To determine whether Ang II influences GLO-I activity, cell lysates were prepared as previously described and 10 μg of lysate was assayed (12). To measure mRNA levels, 0.5 μg of total RNA from either BREC or BRP was extracted using Trizol (Invitrogen, Vic, Australia) and was DNase treated and reverse transcribed (26). Real-time PCR was conducted to detect mRNA levels of GLO-I using SYBR Green UDG Mater Mix (Invitrogen) and an ABI 7900HT Sequence Detection System (Applied Biosystems, Vic, Australia). Primers are detailed in the online appendix (Table S1).
NO• assay in BREC and BRP.
Cells were harvested and treated with nitrate reductase to reduce nitrates to nitrite as previously described (12). NO• was quantitated in cells using 2,3-diaminonaphthalene (28). See online appendix for further detail.
Animal studies.
Procedures complied with the National Health and Medical Research Council of Australia's (NHMRC) Code of the Care and Use of Animals for Scientific Purposes and were approved by the Alfred Medical Research and Education Precinct's (AMREP) Animal Ethics Committee. Female 8-week-old Ren-2 rats were obtained from AMREP Animal Services Pty. Ltd. Female 8-week-old Sprague-Dawley rats were obtained from the Animal Research Centre (Perth, WA, Australia) and served as age-matched controls for Ren-2 rat studies. All rats had free access to normal rat chow and drinking water. They were housed in a stable environment maintained at 22 ± 1°C (12 h light–dark cycle). Ren-2 rats were randomized to the following groups: 1) nondiabetic control, 2) diabetic control, and 3) diabetic+candesartan (5 mg/kg/day, gavage). To make them diabetic, rats were fasted overnight and given a single tail vein injection of streptozotocin (50 mg/kg, 0.1M citrate buffer; Sigma-Aldrich) (13,15,25). Two to three days later, rats began treatment with candesartan for 4 or 20 weeks. Diabetic rats received insulin (Humulin, Eli Lilly Co., USA, 2 units) every 2 days by subcutaneous injection. Body weight was measured each month. Systolic blood pressure was measured each month using a tail cuff method (AD Instruments, CO Springs, CO, USA) (13,15,25). Blood glucose was determined using Accu-check Advantage II Glucose Meter (Roche, Grenzacherstrasse, Basel, Switzerland). Prior to tissue collection, rats were anesthetized with Nembutal (60 mg/kg, Sigma-Aldrich).
Retinal pathology.
Acellular capillaries and leukocyte adherence in large retinal vessels were measured as previously described (13,26). See the online appendix for further detail.
Real-time PCR in retina.
Retinal mRNA levels were determined by real-time PCR as previously described (26). One μg of total RNA extracted from retina was DNase-treated and reverse transcribed. mRNA levels of vascular endothelial growth factor (VEGF), intercellular adhesion molecule-1 (ICAM-I), tumor necrosis factor-α (TNF-α), GLO-I, and inducible nitric oxide synthase (iNOS) were measured. See online appendix for descriptions of primers (Table S1).
Retinal GLO-I activity, tissue and plasma MGO-AGE, argpyrimidine and NO• levels.
For GLO-I activity, flash-frozen whole retina was prepared as described in the online appendix and 10 μg of retina was assayed as described for BREC and BRP. Tissue MGO-AGE and argpyrimidine, a specific MGO-AGE, were detected in undialyzed retinal lysates generated for the GLO-I assay by direct ELISA. See online appendix for further detail. Plasma MGO-AGEs and total AGEs (all AGEs including MGO-AGEs) were quantitated by competitive ELISA. See online appendix for further detail. NO• was measured in retinal lysates as described in ref (28). See online appendix for further detail.
Statistics.
For all cell culture studies, experiments were performed in triplicate and then the entire experiment was independently repeated at least three times. Data were analyzed using either SPSS v11 (SPSS Inc., Chicago, IL, USA) or GraphPad Prism five (GraphPad Software Inc, LA Jolla, CA, USA). For animal experiments, at least six rats were required in each group to achieve statistical significance. To determine how many animals per group were required, we compared previous experimental data in diabetic animals with treated groups for each respective end point and then calculated the number of animals required to achieve an expected power of 0.8 (80%) and a P value of 0.05. Both animal and cell culture datasets were assessed for normality, and in the case of >2 treatments, either one-way ANOVA (parametric), followed by appropriate post hoc analyses correcting for the number of comparisons, or Kruskal-Wallis, followed by individual Mann-Whitney U tests (nonparametric), was conducted. When only two treatments were given, either an unpaired t test (parametric) or a Mann-Whitney U test (nonparametric) was conducted. Investigators were masked to the groups. A value of P < 0.05 was considered significant.
RESULTS
Ang II stimulates apoptosis and decreases GLO-I in BRECs and BRPs.
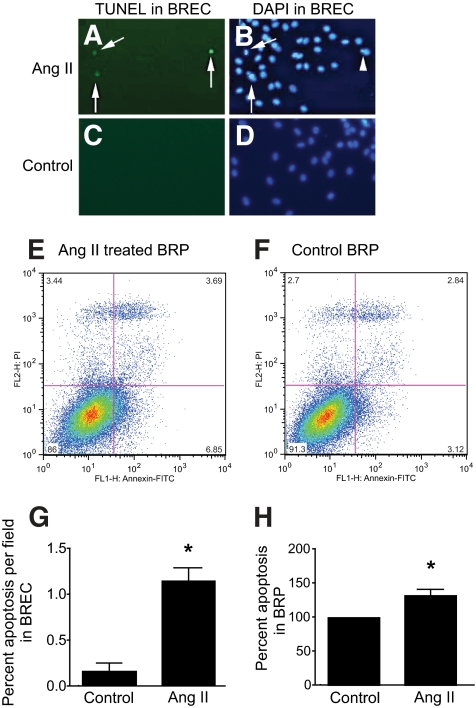
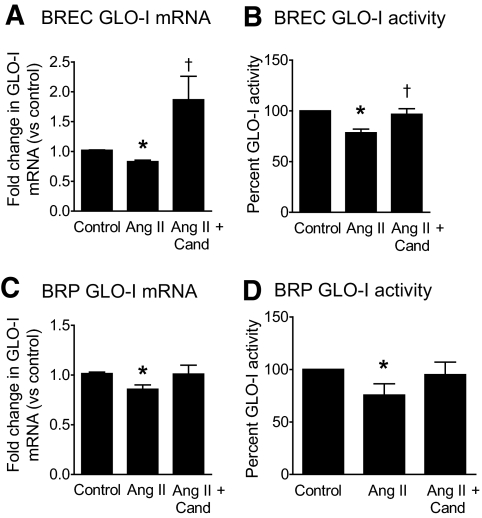
To determine whether Ang II induces apoptosis in retinal vascular cells, BREC and BRP were incubated with 100 nmol/l Ang II for 24 h. In BREC and BRP, Ang II treatment resulted in a 500 and 30% increase in either TUNEL or Annexin-positive cells, respectively, compared with control (Fig. 1). Given this finding, we next evaluated GLO-I in BREC and BRP and found that, in both cell types, Ang II decreased GLO-I activity and mRNA by 20% compared with controls (Fig. 2). To confirm the involvement of Ang II in the downregulation of GLO-I, we next measured GLO-I after treatment with the AT1-RB, candesartan. In both BREC and BRP, candesartan restored both GLO-I activity and mRNA to control levels in Ang II-treated cells (Fig. 2), and in the case of BREC, GLO-I mRNA was elevated above control levels (Fig. 2). Overall, BREC was more responsive to the actions of candesartan in terms of restoration of GLO-I function. Candesartan in the absence of Ang II, in almost all instances, did not influence GLO-I levels (see supplementary Fig. 1, available in the online appendix).
FIG. 1.
BREC and BRP apoptosis as detected by TUNEL staining and flow cytometry, respectively, after treatment with Ang II. In BREC, TUNEL staining is increased after treatment with 100 nmol/l Ang II for 24 h (A) compared with control (C). DAPI nuclear staining of Ang II-treated (B) and control (D) BREC. Arrows denote TUNEL-positive BREC, and arrowhead denotes cellular blebbing, a common feature of apoptosis. Magnification ×200. Representative example of Annexin V-FITC (x-axis) and propidium iodide (PI) staining (y-axis) to detect apoptotic cells after treatment of BRP with 100 nmol/l Ang II (E) or control (F) for 24 h. Increases were observed in the Annexin V positive, or early apoptotic phase (bottom right-hand quadrant), and Annexin V positive/PI positive (top right-hand quadrant), or late apoptotic phase (E). Bottom left quadrant, viable cells; Top left quadrant, necrotic cells (PI staining only). G: Graphical representation of BREC apoptosis detected by TUNEL staining; *P < 0.01 versus control. N = 3 samples and is a representative dataset of three independent experiments. H: Graphical representation of BRP apoptosis detected by Annexin/PI staining; *P < 0.03 versus control. All data were analyzed by unpaired t tests. N = 3 independent experiments. Values are mean ± SEM. (A high-quality color representation of this figure is available in the online issue.)
FIG. 2.
GLO-I mRNA and activity levels in BREC and BRP after treatment with Ang II and candesartan (Cand). In BREC (A and B) and BRP (C and D), GLO-I mRNA (A and C) and activity (B and D) is decreased after treatment with Ang II (100 nmol/l) for 24 h compared with control. Cand (1 μmol/l) restored GLO-I activity and mRNA in BREC and BRP co-incubated with Ang II. A, B: *P < 0.05 versus control, †P < 0.05 versus Ang II. C and D: *P < 0.03 versus control. All data were analyzed by Kruskal-Wallis test, followed by Mann-Whitney U tests. Values are the mean of N = 3–4 independent experiments with triplicate samples within each experiment.
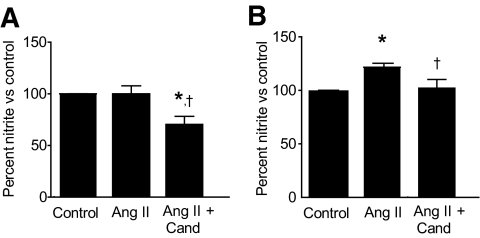
Ang II's reduction of GLO-I and in BRP is accompanied by an increase in NO•.
To determine whether Ang II's downregulation of GLO-I involves NO•, we measured NO• production in BREC and BRP after Ang II treatment in the presence or absence of candesartan. In BREC, Ang II had no effect on NO• levels, whereas in BRP, Ang II increased NO• production 1.2-fold. In both cell types, candesartan reduced NO• levels in Ang II-treated cells compared with those only receiving Ang II (Fig. 3).
FIG. 3.
NO• levels in BREC (A) and BRP (B) after treatment with Ang II and Cand for 24 h. A: Treatment of BREC with 100 nmol/l Ang II had no effect on NO• levels. In BREC treated with Ang II+Cand (1 μmol/l), NO• levels were reduced below both control and Ang II treated cells. *P < 0.01 versus control, †P < 0.03 versus Ang II. B: Treatment of BRP with 100 nmol/l Ang II significantly increased NO• levels. In BRP treated with Ang II+Cand, NO• levels were reduced to control levels. *P < 0.05 versus control, †P < 0.05 versus Ang II. BRP were analyzed by one-way ANOVA, followed by Bonferroni post hoc tests. BREC were analyzed by Kruskal-Wallis tests followed by Mann-Whitney U tests. Values are the means of 3 and 7 independent experiments (BRP and BREC, respectively) with triplicate samples within each experiment.
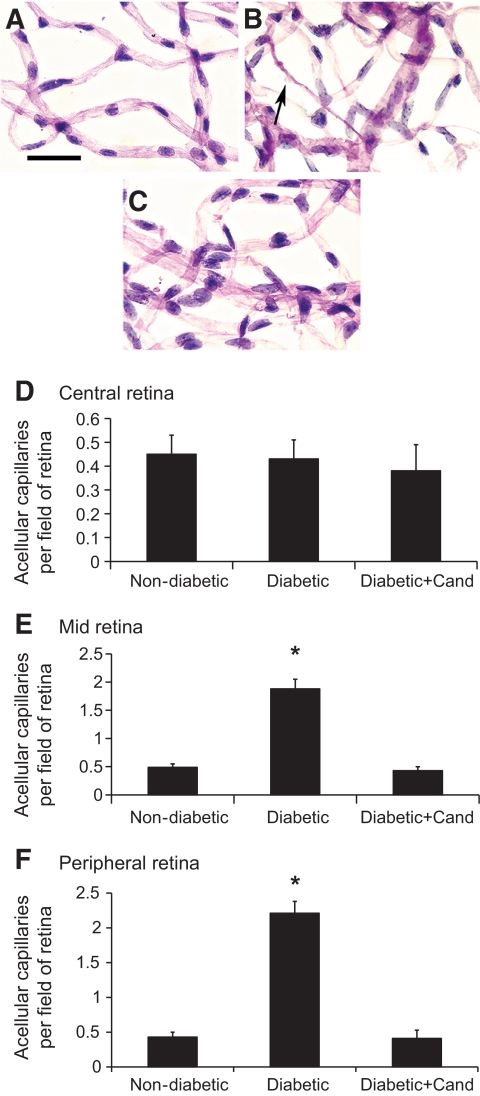
Diabetic Ren-2 rats develop acellular capillaries and increased retinal leukostasis, which is reduced with candesartan.
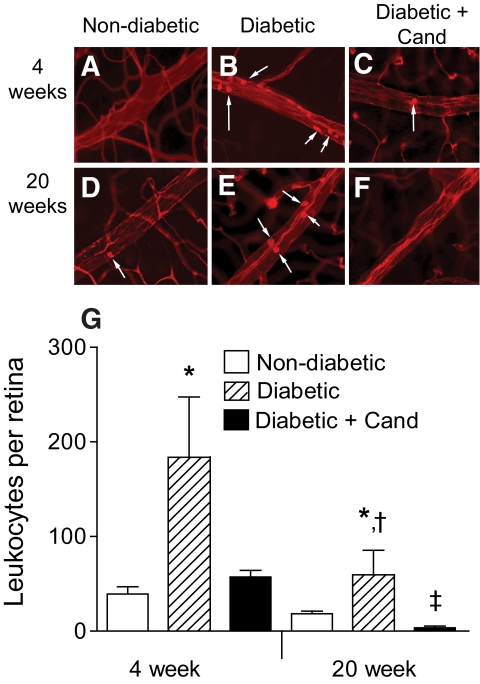
The in vivo counterpart of BREC and BRP apoptosis is the formation of acellular capillaries. To determine whether GLO-I expression is reduced in retina from diabetic Ren-2 rats and correlates with acellular capillary formation, we first evaluated the number of acellular capillaries in retina of Ren-2 rats after 20 weeks of diabetes. Acellular capillary formation was increased in the mid and peripheral retina of diabetic Ren-2 rats compared with nondiabetic controls and reduced with candesartan (Fig. 4). Because leukocyte adherence in retinal vessels may precede the development of acellular capillaries, both 4- and 20-week time points were examined. In diabetic Ren-2 rats, adherent leukocytes were increased after 4 and 20 weeks of diabetes compared with nondiabetic controls (Fig. 5), with leukocyte adherence most pronounced in the 4-week diabetic group. In diabetic Ren-2 rats, candesartan reduced the increase in leukocyte adherence in retinal vessels to control levels or below (Fig. 5).
FIG. 4.
Acellular capillaries in trypsin digests of retina in representative micrographs from Ren-2 rats after 20 weeks of diabetes. Retina stained with Periodic-acid Schiff's reagent. Scale bar = 20 μm. Nondiabetic (A), diabetic (B), and diabetic+Cand (5 mg/kg/day) (C). In diabetic Ren-2 rats, acellular capillaries were increased in the mid and peripheral retina compared with nondiabetic Ren-2 rats. In diabetic Ren-2 rats, Cand reduced acellular capillaries in the mid and peripheral retina to the level of nondiabetic control. Arrow denotes acellular capillary with pericyte ghost at arrowhead tip. Graphs showing number of acellular capillaries per retinal field (mean ± SEM) in the central (D), mid (E), and peripheral (F) retina. *P < 0.05 versus nondiabetic, diabetic+Cand. N = 8 animals/group. Data were analyzed by one-way ANOVA, followed by Bonferroni post hoc tests. (A high-quality color representation of this figure is available in the online issue.)
FIG. 5.
Leukocyte adherence in retinal blood vessels in representative micrographs of Ren-2 rats after 4 and 20 weeks of diabetes after perfusion with rhodamine coupled to Concanavalin A. Scale bar = 80 μm. Arrows denote adherent leukocytes. Leukocytes were counted in all retinal vessels. Four-week study: Nondiabetic (A), diabetic (B), and diabetic+Cand (C). Twenty-week study: Nondiabetic (D), diabetic (E), and diabetic+Cand (F). Diabetes at both 4 and 20 weeks is associated with an increase in leukocyte adherence in retinal vessels compared with age-matched nondiabetic control. In diabetic Ren-2 rats, Cand reduced leukocyte adherence in retinal vessels to the level of nondiabetic control. G: Graphical representation of leukocyte adherence in vessels of the retina (mean ± SEM). N = 6–10 animals/group. *P < 0.03 versus age-matched nondiabetic control and diabetic+Cand; †P < 0.02 versus week 4 diabetic; ‡P < 0.005 versus age-matched nondiabetic control. BREC were analyzed by Kruskal-Wallis tests followed by Mann-Whitney U tests. (A high-quality color representation of this figure is available in the online issue.)
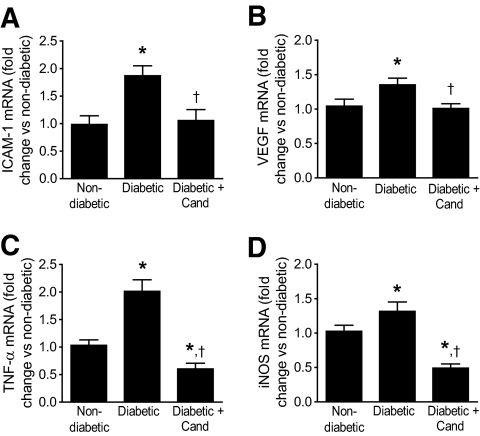
Gene expression of VEGF, inflammatory factors, and iNOS in retina of diabetic Ren-2 rats.
In diabetic Ren-2 rats, the level of retinal ICAM-1 and TNF-α mRNA doubled, and VEGF mRNA increased by 0.5-fold compared with nondiabetic controls. In diabetic Ren-2 rats, both ICAM-1 and VEGF mRNA levels in retina were reduced with candesartan to the level of nondiabetic controls (Fig. 6) and TNF-α mRNA was reduced to below nondiabetic control levels. (Fig. 6). In diabetic Ren-2 rats, the level of retinal iNOS mRNA was increased by 0.3-fold compared with nondiabetic controls, and candesartan reduced retinal iNOS mRNA levels to below the level of nondiabetic controls (Fig. 6).
FIG. 6.
ICAM-1 (A), VEGF (B), TNF-α (C), and iNOS (D) mRNA levels in retina of Ren-2 rats after 4 weeks of diabetes. Retinal ICAM-1, VEGF, TNF-α, and iNOS mRNA levels are increased in diabetic Ren-2 rats compared with nondiabetic control. In diabetic Ren-2 rats, Cand reduced both retinal ICAM-1 (A) and VEGF mRNA (B) to the level of nondiabetic controls, with TNF-α (C) and iNOS mRNA (D) decreasing to below control levels. For panels A, B, and D, data were analyzed by one-way ANOVA, followed by Bonferroni post hoc tests. *P < 0.05 versus nondiabetic control. †P < 0.05 versus diabetic control. For panel C, data were analyzed by Kruskal-Wallis tests followed by Mann-Whitney U tests. *P < 0.02 versus nondiabetic control. †P < 0.0001 versus diabetic control. N = 8–13 animals/group. Values are mean ± SEM.
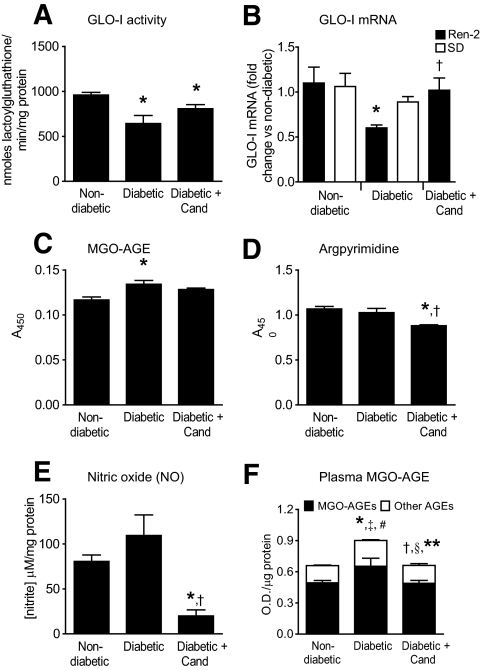
Retinal pathology in diabetic Ren-2 rats is associated with a reduction in retinal GLO-I.
In Ren-2 rats, the retinal pathology that occurred at 4 and 20 weeks of diabetes was accompanied by modulations in GLO-I function. A decrease in retinal GLO-I activity was observed at 4 weeks of diabetes, although changes in mRNA levels were not detected (Fig. 7 and supplementary Fig. 2, available in the online appendix, respectively). However, after 20 weeks of diabetes, retinal GLO-I mRNA was decreased (Fig. 7). Candesartan increased GLO-I expression in the retina of diabetic Ren-2 rats, which is consistent with our findings in BREC and BRP. To determine whether the reduction in retinal GLO-I in diabetic Ren-2 rats is related to the overexpression of the RAS in these animals, comparisons were made to nondiabetic and diabetic Sprague-Dawley rats with a suppressed RAS (Fig. 7). The expression of GLO-I in retina from nondiabetic Sprague-Dawley rats was unchanged with diabetes. We then investigated whether GLO-I dysregulation by the RAS increased MGO-derived AGEs. After 4 weeks of diabetes in Ren-2 rats, MGO-AGE levels in retina were increased. In diabetic Ren-2 rats, candesartan tended to reduce the increase in retinal MGO-AGE, but this was not significant (Fig. 7). The specific MGO-AGE, argpyrimidine, was also measured in retina and was unchanged with diabetes in the Ren-2 rat; however, candesartan did reduce the levels of retinal argpyrimidine compared with controls (Fig. 7). After 20 weeks of diabetes, both plasma MGO-AGEs and total AGEs were elevated in diabetes and significantly reduced with candesartan (Fig. 7). Retinal NO• was significantly suppressed in the diabetic Ren-2 rats treated with candesartan compared with both diabetic and nondiabetic controls (Fig. 7).
FIG. 7.
GLO-I activity and mRNA, and MGO-AGE levels in diabetic Ren-2 rats. In Ren-2 rats after 4 weeks of diabetes, retinal GLO-I activity (A) is reduced compared with nondiabetic control and tends to be restored with Cand, although this is not significant (*P < 0.03 vs. nondiabetic Ren-2 control). In Ren-2 rats after 20 weeks of diabetes, retinal GLO-I mRNA (B) is clearly reduced compared with nondiabetic control and is restored to control levels with Cand (*P < 0.005 vs. nondiabetic Ren-2 control, †P < 0.05 vs. diabetic Ren-2 control). In comparison, in Sprague-Dawley (SD) rats (B), no changes in retinal GLO-I mRNA are observed with 20 weeks of diabetes. In Ren-2 rats after 4 weeks of diabetes, the reduction in retinal GLO-I activity (A) is accompanied by an increase in the levels of retinal MGO-AGE (C), (*P < 0.01 vs. nondiabetic Ren-2 control). In diabetic Ren-2 rats, Cand tends to decrease the levels of retinal MGO-AGE, but this is not significant. In diabetic Ren-2 rats at 4 weeks, the levels in retina of the specific MGO-AGE, argpyrimidine (D), and NO• levels (E) are unchanged compared with nondiabetic controls; however, Cand reduced retinal argpyrimidine (*P < 0.05 vs. nondiabetic Ren-2 control, †P < 0.01 vs. diabetic Ren-2 control) and NO• levels (*P < 0.05 vs. nondiabetic Ren-2 control. †P < 0.01 vs. diabetic Ren-2 control). F: Plasma MGO-AGEs (black bars) are increased in Ren-2 rats after 20 weeks of diabetes compared with nondiabetic controls and are reduced with Cand to nondiabetic levels (*P < 0.05 vs. nondiabetic Ren-2 control; †P < 0.05 vs. diabetic Ren-2 control). Other AGEs (non-MGO AGEs, white bars) and total AGEs (MGO-AGE + other AGEs, black + white bars) were increased in Ren-2 rats after 20 weeks of diabetes and reduced with Cand to nondiabetic control levels (‡P < 0.005 versus “other AGE” nondiabetic Ren-2 control; §P < 0.04 versus “other AGE” diabetic Ren-2 control; #P < 0.02 versus “total AGE” nondiabetic Ren-2 control; **P < 0.02 versus “total AGE” diabetic Ren-2 control). N = 5–8 animals/group. Values are mean ± SEM. Data in panels C and D were analyzed by one-way ANOVA, followed by Bonferroni post hoc tests. All other datasets in this figure were analyzed by Kruskal-Wallis tests, followed by Mann-Whitney U tests.
Body weight, blood glucose, and systolic blood pressure.
The results are found in the online appendix in Table S2.
DISCUSSION
The present study provides novel evidence that GLO-I, an enzyme critical for retinal vascular cell survival (12), is downregulated by Ang II in the retina. Our findings are supported by evidence that the AT1-RB, candesartan, improves acellular capillary formation and inflammation in diabetic retinopathy with a concomitant restoration of retinal GLO-I expression and a reduction of MGO-AGEs and, in particular, the specific MGO-AGE argpyrimidine. These findings broaden the known actions of Ang II in the AGE pathway to include not only extracellular AGE-related events such as RAGE-mediated cellular apoptosis (24,29,30) but also the intracellular formation of MGO-AGEs. In terms of the mechanism by which retinal GLO-I is regulated, our previous study in retinal pericytes indicated a role for NO• (12). We now extend this finding to report that, in retinal vascular cells, candesartan reduces NO• levels, which is accompanied by the restoration of GLO-I. Overall, the present study provides new information about how Ang II interacts with the AGE pathway and the cellular mechanisms by which candesartan exerts its potent protective effects in diabetic retinopathy (Fig. 8).
FIG. 8.
Proposed mechanism by which Ang II downregulates GLO-I in retinal vascular cells, leading to the generation of AGEs and vascular injury. The AT1-RB, Cand, is able to prevent diabetic retinal vascular injury by reducing nitric oxide and restoring GLO-I levels.
At 20 weeks of diabetes, we observed increased acellular capillary formation in the mid and peripheral retina of the Ren-2 rat, which is consistent with our previous studies in the Ren-2 rat (13) and observed in diabetic patients (31). Acellular capillary formation is a pathology that occurs in retinal microvessels after the apoptosis of both endothelial cells and pericytes (32). These events may result in areas of retinal nonperfusion, which are viewed to lead to the upregulation of angiogenic growth factors such as VEGF with subsequent pathological angiogenesis. The mechanisms responsible for retinal vascular cell apoptosis are not fully defined; however, previous studies by our group indicate that GLO-I is necessary for the survival of human retinal pericytes (12). The present study builds on this information by identifying in retinal vascular cells that Ang II is a novel, negative regulator of GLO-I activity and expression and inducer of cellular apoptosis. Supporting an interaction between Ang II and GLO-I is our finding that, in diabetic Ren-2 rats with an enhanced extrarenal RAS in tissues including the eye (15), retinal GLO-I expression is reduced with a concomitant increase in acellular capillaries. It is noteworthy that, in age-matched diabetic Sprague-Dawley rats, retinal GLO-I is not reduced and these animals do not develop acellular capillaries (13). We acknowledge that GLO-I activity was not measured in long-term diabetes when acellular capillaries appear; nevertheless, GLO-I activity was reduced in the early stages of diabetic retinopathy when inflammation is maximal. The ability of candesartan to restore retinal GLO-I and attenuate retinal vasculopathy including inflammation, which is viewed to contribute to diabetic retinopathy (33), may be important when considering the underlying mechanisms by which Ang II blockers such as candesartan provide retinoprotection.
Although the glyoxalase system is a critical regulator of the AGE pathway, it is the formation of MGO-AGEs that are implicated in cellular damage. To date, the majority of studies in this area have focused on the contribution of AGEs via RAGE to AGE-mediated pathology, including in diabetic retinopathy (34). However, AGEs may not be the primary RAGE ligands in vivo, given that proteins must be heavily glycated before they can bind to RAGE, and this extensive glycation may not occur to a major extent in vivo (35). There are limited reports detailing the contribution of intracellular AGEs to pathology, although there is increasing evidence to support this possibility (36,37). Another dimension to the RAGE paradigm is the recent finding that GLO-I can control the expression of RAGE and its ligands by modulating the levels of MGO (38), consistent with the view that intracellular glycation can control RAGE expression. The influence of the RAS on AGE formation has been established in the diabetic nephropathy (20–23), with in general a focus on RAGE-mediated signaling. This is true also for the limited studies in diabetic retinopathy, where Ang II mediates increases in RAGE and AGE-induced apoptosis of retinal pericytes (24,29,30). In the present study, an evaluation of intracellular MGO-AGE formation, as detected by ELISA using an antibody raised against a heterogeneous mixture of MGO-AGEs, revealed an increase in retina from diabetic Ren-2 rats. A specific MGO-AGE, argpyrimidine, formed on reaction of MGO with arginine residues, was also examined, given the known preferential modification of arginine over lysine (39) and the previous detection of this specific moiety in the diabetic kidney (39,40). However, despite an elevation in retinal MGO-AGEs in diabetic Ren-2 rats, argpyrimidine was not increased, a finding which may be explained by its presence in lower quantities relative to other MGO-AGEs (41). Further evidence that Ang II influences retinal MGO-AGEs arises from our finding that candesartan, which restored GLO-I in diabetic Ren-2 retina, also reduced retinal MGO-AGEs and argpyrimidine levels. These results are consistent with a previous study, which reported that candesartan reduced immunolabeling of the AGE pentosidine in the retina of diabetic rats, although in that study pentosidine levels were not specifically quantitated (42). Consistent with candesartan's reduction of retinal MGO-AGEs, candesartan lowered plasma MGO-AGE, and it is noteworthy that the majority of AGEs detected in plasma using our assay were MGO-derived. Overall, our findings establish a mechanism for the observed regulation of AGEs by the RAS in diabetic retinopathy that may be indeed relevant to other diabetic complications (20–23).
A possible candidate for Ang II's downregulation of GLO-I in the retina is via an increase in NO•. This postulate is based on our previous studies in human retinal pericytes, which indicated that GLO-I is regulated at the transcriptional level by NO• (12). Furthermore, there is considerable evidence that Ang II stimulates NO• production, which leads to vascular pathology (43), including retinal inflammation and breakdown of the blood–retinal barrier (44,45). In the present study, although Ang II reduced GLO-I activity and expression in both cultured retinal endothelial cells and pericytes, it only increased NO• levels in retinal pericytes. The reasons for Ang II not stimulating NO• in retinal endothelial cells is not clear; however, our data would indicate that Ang II via the AT1-R influences NO• production in retinal endothelial cells, with candesartan reducing NO• levels in both cell populations. Similarly, in Ren-2 retina, NO• levels were not significantly elevated with diabetes; however, candesartan reduced NO• levels below nondiabetic control, supporting the idea that in retina Ang II influences NO• production via the AT1-R. A consideration when interpreting our results is that physiological levels of NO• are required for normal tissue function and can inhibit leukocyte adhesion (46) and mediate vasorelaxation (47). Our finding that candesartan reduced retinal iNOS and NO• below control levels may indicate that further studies are required to determine whether lower doses of AT1-RB can maintain NO• at physiological levels within the retina with a concomitant reduction in retinal pathology and restoration of GLO-I. In terms of a pathological role for the NO• system in diabetic retinopathy, our findings are consistent with previous studies where iNOS is implicated as a major contributor to the increased NO• levels in diabetic retinopathy (48,49) and reports that tissue iNOS can be reduced with candesartan (22).
A possible limitation of the present study is that the effectiveness of candesartan on diabetic retinopathy in the Ren-2 rat could be due to a reduction of the hypertension of this animal rather than inhibition of the growth factor effects of angiotensin II. However, in our previous studies, a comparison of age- and blood pressure-matched diabetic spontaneously hypertensive rats to diabetic Ren-2 rats revealed that the former did not develop as severe diabetic retinopathy, suggesting that the overexpression of the RAS in the Ren-2 rat was largely responsible for the development of diabetic retinopathy in this model (15). Furthermore, in diabetic Ren-2 rats, the β-blocker, atenolol, and the AT1-RB, valsartan, both produced similar reductions in systolic blood pressure; however, only valsartan attenuated retinal acellular capillary formation and the decline in retinal function (13,14). Nonetheless, whether hypertension per se influences retinal GLO-I activity and expression in diabetes is to our knowledge unknown and warrants investigation in future studies.
In conclusion, the results from the current study are timely, given the positive findings from recent clinical trials, which indicate that AT1-RB and angiotensin converting enzyme inhibition confer protective effects on the retinal vasculature in diabetic retinopathy (18,19,50). Our data suggest that GLO-I could be a key enzyme that bridges the RAS and AGE pathways, thereby contributing to the development of diabetic retinopathy (Fig. 8). These findings enhance our understanding of how RAS blockers such as candesartan act at the molecular level to confer retinal vascular protection in disorders such as diabetes.
Supplementary Material
ACKNOWLEDGMENTS
This study was funded by a Diabetes Australia Research Trust and an Eli Lilly New Investigator grant awarded to A.G.M., as well as by AstraZeneca (Mölndal, Sweden) and National Institutes of Health grants to Ram Nagaraj (R01EY-016219 and R01EY-09912). A.G.M. is a Juvenile Diabetes Research Foundation Postdoctoral Fellow. J.L.W.B. is a National Health and Medical Research Council (NHMRC) of Australia, Senior Research Fellow. M.E.C. is a NHMRC Australia Fellow and a Juvenile Diabetes Research Foundation Scholar. M.C.T. is supported by Kidney Health Australia (Bootle Award). No other potential conflicts of interest relevant to this article were reported.
A.G.M. designed and conducted experiments, analyzed data, and prepared the manuscript. G.T. conducted experiments and analyzed data. K.J.B. conducted experiments, analyzed data, and reviewed the manuscript. R.J.P. designed and performed plasma ELISA. M.C.T. designed plasma ELISA experiments. R.H.N. and M.E.C. provided advice for some experiments and reviewed the manuscript. J.L.W.B. designed experiments and assisted with discussion and preparation of the manuscript.
We thank Kylie McMaster, Department of Immunology, Monash University, for excellent technical assistance. We also thank Dr. Mike Griffin of Bio21, University of Melbourne, for access to equipment to conduct the GLO-I activity experiments.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 2.Yamagishi S, Amano S, Inagaki Y, Okamoto T, Koga K, Sasaki N, Yamamoto H, Takeuchi M, Makita Z: Advanced glycation end products-induced apoptosis and overexpression of vascular endothelial growth factor in bovine retinal pericytes. Biochem Biophys Res Commun 2002;290:973–978 [DOI] [PubMed] [Google Scholar]
- 3.Stitt AW, Li YM, Gardiner TA, Bucala R, Archer DB, Vlassara H: Advanced glycation end products (AGEs) co-localize with AGE receptors in the retinal vasculature of diabetic and of AGE-infused rats. Am J Pathol 1997;150:523–531 [PMC free article] [PubMed] [Google Scholar]
- 4.Wilkinson-Berka JL: Angiotensin and diabetic retinopathy. Int J Biochem Cell Biol 2006;38:752–765 [DOI] [PubMed] [Google Scholar]
- 5.Thornalley PJ: The glyoxalase system: new developments towards functional characterization of a metabolic pathway fundamental to biological life. Biochem J 1990;269:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosca MG, Mustata TG, Kinter MT, Ozdemir AM, Kern TS, Szweda LI, Brownlee M, Monnier VM, Weiss MF: Glycation of mitochondrial proteins from diabetic rat kidney is associated with excess superoxide formation. Am J Physiol Renal Physiol 2005;289:F420–430 [DOI] [PubMed] [Google Scholar]
- 7.Yao D, Taguchi T, Matsumura T, Pestell R, Edelstein D, Giardino I, Suske G, Rabbani N, Thornalley PJ, Sarthy VP, Hammes HP, Brownlee M: High glucose increases angiopoietin-2 transcription in microvascular endothelial cells through methylglyoxal modification of mSin3A. J Biol Chem 2007;282:31038–31045 [DOI] [PubMed] [Google Scholar]
- 8.Karachalias N, Babaei-Jadidi R, Ahmed N, Thornalley PJ: Accumulation of fructosyl-lysine and advanced glycation end products in the kidney, retina and peripheral nerve of streptozotocin-induced diabetic rats. Biochem Soc Trans 2003;31:1423–1425 [DOI] [PubMed] [Google Scholar]
- 9.Fosmark DS, Berg JP, Jensen AB, Sandvik L, Agardh E, Agardh CD, Hanssen KF: Increased retinopathy occurrence in type 1 diabetes patients with increased serum levels of the advanced glycation endproduct hydroimidazolone. Acta Ophthalmol 2009;87:498–500 [DOI] [PubMed] [Google Scholar]
- 10.Barati MT, Merchant ML, Kain AB, Jevans AW, McLeish KR, Klein JB: Proteomic analysis defines altered cellular redox pathways and advanced glycation end-product metabolism in glomeruli of db/db diabetic mice. Am J Physiol Renal Physiol 2007;293:F1157–1165 [DOI] [PubMed] [Google Scholar]
- 11.Phillips SA, Mirrlees D, Thornalley PJ: Modification of the glyoxalase system in streptozotocin-induced diabetic rats. Effect of the aldose reductase inhibitor Statil. Biochem Pharmacol 1993;46:805–811 [DOI] [PubMed] [Google Scholar]
- 12.Miller AG, Smith DG, Bhat M, Nagaraj RH: Glyoxalase I is critical for human retinal capillary pericyte survival under hyperglycemic conditions. J Biol Chem 2006;281:11864–11871 [DOI] [PubMed] [Google Scholar]
- 13.Wilkinson-Berka JL, Tan G, Jaworski K, Ninkovic S: Valsartan but not atenolol improves vascular pathology in diabetic Ren-2 rat retina. Am J Hypertens 2007;20:423–430 [DOI] [PubMed] [Google Scholar]
- 14.Phipps JA, Wilkinson-Berka JL, Fletcher EL: Retinal dysfunction in diabetic ren-2 rats is ameliorated by treatment with valsartan but not atenolol. Invest Ophthalmol Vis Sci 2007;48:927–934 [DOI] [PubMed] [Google Scholar]
- 15.Moravski CJ, Skinner SL, Stubbs AJ, Sarlos S, Kelly DJ, Cooper ME, Gilbert RE, Wilkinson-Berka JL: The renin-angiotensin system influences ocular endothelial cell proliferation in diabetes: transgenic and interventional studies. Am J Pathol 2003;162:151–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagai N, Izumi-Nagai K, Oike Y, Koto T, Satofuka S, Ozawa Y, Yamashiro K, Inoue M, Tsubota K, Umezawa K, Ishida S: Suppression of diabetes-induced retinal inflammation by blocking the angiotensin II type 1 receptor or its downstream nuclear factor-kappaB pathway. Invest Ophthalmol Vis Sci 2007;48:4342–4350 [DOI] [PubMed] [Google Scholar]
- 17.Gilbert RE, Kelly DJ, Cox AJ, Wilkinson-Berka JL, Rumble JR, Osicka T, Panagiotopoulos S, Lee V, Hendrich EC, Jerums G, Cooper ME: Angiotensin converting enzyme inhibition reduces retinal overexpression of vascular endothelial growth factor and hyperpermeability in experimental diabetes. Diabetologia 2000;43:1360–1367 [DOI] [PubMed] [Google Scholar]
- 18.Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J, Parving HH, Bilous R, Sjølie AK, DIRECT Programme Study Group Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet 2008;372:1394–1402 [DOI] [PubMed] [Google Scholar]
- 19.Sjølie AK, Klein R, Porta M, Orchard T, Fuller J, Parving HH, Bilous R, Chaturvedi NDIRECT Programme Study Group Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet 2008;372:1385–1393 [DOI] [PubMed] [Google Scholar]
- 20.Forbes JM, Cooper ME, Thallas V, Burns WC, Thomas MC, Brammar GC, Lee F, Grant SL, Burrell LM, Burrell LA, Jerums G, Osicka TM: Reduction of the accumulation of advanced glycation end products by ACE inhibition in experimental diabetic nephropathy. Diabetes 2002;51:3274–3282 [DOI] [PubMed] [Google Scholar]
- 21.Forbes JM, Thomas MC, Thorpe SR, Alderson NL, Cooper ME: The effects of valsartan on the accumulation of circulating and renal advanced glycation end products in experimental diabetes. Kidney Int Suppl 2004;92:105–107 [DOI] [PubMed] [Google Scholar]
- 22.Fan Q, Liao J, Kobayashi M, Yamashita M, Gu L, Gohda T, Suzuki Y, Wang LN, Horikoshi S, Tomino Y: Candesartan reduced advanced glycation end-products accumulation and diminished nitro-oxidative stress in type 2 diabetic KK/Ta mice. Nephrol Dial Transplant 2004;19:3012–3020 [DOI] [PubMed] [Google Scholar]
- 23.Nangaku M, Miyata T, Sada T, Mizuno M, Inagi R, Ueda Y, Ishikawa N, Yuzawa H, Koike H, van Ypersele de Strihou C, Kurokawa K: Anti-hypertensive agents inhibit in vivo the formation of advanced glycation end products and improve renal damage in a type 2 diabetic nephropathy rat model. J Am Soc Nephrol 2003;14:1212–1222 [DOI] [PubMed] [Google Scholar]
- 24.Yamagishi S, Takeuchi M, Matsui T, Nakamura K, Imaizumi T, Inoue H: Angiotensin II augments advanced glycation end product-induced pericyte apoptosis through RAGE overexpression. FEBS Lett 2005;579:4265–4270 [DOI] [PubMed] [Google Scholar]
- 25.Wilkinson-Berka JL, Kelly DJ, Koerner SM, Jaworski K, Davis B, Thallas V, Cooper ME: ALT-946 and aminoguanidine, inhibitors of advanced glycation, improve severe nephropathy in the diabetic transgenic (mREN-2)27 rat. Diabetes 2002;51:3283–3289 [DOI] [PubMed] [Google Scholar]
- 26.Wilkinson-Berka JL, Tan G, Jaworski K, Miller AG: Identification of a retinal aldosterone system and the protective effects of mineralocorticoid receptor antagonism on retinal vascular pathology. Circ Res 2009;104:124–133 [DOI] [PubMed] [Google Scholar]
- 27.Romeo G, Liu WH, Asnaghi V, Kern TS, Lorenzi M: Activation of nuclear factor-kappaB induced by diabetes and high glucose regulates a proapoptotic program in retinal pericytes. Diabetes 2002;51:2241–2248 [DOI] [PubMed] [Google Scholar]
- 28.Nussler AK, Glanemann M, Schirmeier A, Liu L, Nüssler NC: Fluorometric measurement of nitrite/nitrate by 2,3-diaminonaphthalene. Nat Protoc 2006;1:2223–2226 [DOI] [PubMed] [Google Scholar]
- 29.Yamagishi S, Matsui T, Nakamura K, Inoue H, Takeuchi M, Ueda S, Fukami K, Okuda S, Imaizumi T: Olmesartan blocks advanced glycation end products (AGEs)-induced angiogenesis in vitro by suppressing receptor for AGEs (RAGE) expression. Microvasc Res 2008;75:130–134 [DOI] [PubMed] [Google Scholar]
- 30.Yamagishi S, Matsui T, Nakamura K, Inoue H, Takeuchi M, Ueda S, Okuda S, Imaizumi T: Olmesartan blocks inflammatory reactions in endothelial cells evoked by advanced glycation end products by suppressing generation of reactive oxygen species. Ophthalmic Res 2008;40:10–15 [DOI] [PubMed] [Google Scholar]
- 31.Cardillo Piccolino F, Zingirian M, Mosci C: Classification of proliferative diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 1987;225:245–250 [DOI] [PubMed] [Google Scholar]
- 32.Mizutani M, Kern TS, Lorenzi M: Accelerated death of retinal microvascular cells in human and experimental diabetic retinopathy. J Clin Invest 1996;97:2883–2890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joussen AM, Poulaki V, Le ML, Koizumi K, Esser C, Janicki H, Schraermeyer U, Kociok N, Fauser S, Kirchhof B, Kern TS, Adamis AP: A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J 2004;18:1450–1452 [DOI] [PubMed] [Google Scholar]
- 34.Glenn JV, Stitt AW: The role of advanced glycation end products in retinal ageing and disease. Biochim Biophys Acta 2009;1790:1109–1116 [DOI] [PubMed] [Google Scholar]
- 35.Thornalley PJ: Dietary AGEs and ALEs and risk to human health by their interaction with the receptor for advanced glycation endproducts (RAGE)–an introduction. Mol Nutr Food Res 2007;51:1107–1110 [DOI] [PubMed] [Google Scholar]
- 36.Shinohara M, Thornalley PJ, Giardino I, Beisswenger P, Thorpe SR, Onorato J, Brownlee M: Overexpression of glyoxalase-I in bovine endothelial cells inhibits intracellular advanced glycation endproduct formation and prevents hyperglycemia-induced increases in macromolecular endocytosis. J Clin Invest 1998;101:1142–1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.El-Osta A, Brasacchio D, Yao D, Pocai A, Jones PL, Roeder RG, Cooper ME, Brownlee M: Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J Exp Med 2008;205:2409–2417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yao D, Brownlee M: Hyperglycemia-induced reactive oxygen species increase expression of the receptor for advanced glycation end products (RAGE) and RAGE ligands. Diabetes 2010;59:249–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oya T, Hattori N, Mizuno Y, Miyata S, Maeda S, Osawa T, Uchida K: Methylglyoxal modification of protein. Chemical and immunochemical characterization of methylglyoxal-arginine adducts. J Biol Chem 1999;274:18492–18502 [DOI] [PubMed] [Google Scholar]
- 40.Padival AK, Crabb JW, Nagaraj RH: Methylglyoxal modifies heat shock protein 27 in glomerular mesangial cells. FEBS Lett 2003;551:113–118 [DOI] [PubMed] [Google Scholar]
- 41.Ahmed N, Thornalley PJ: Chromatographic assay of glycation adducts in human serum albumin glycated in vitro by derivatization with 6-aminoquinolyl-N-hydroxysuccinimidyl-carbamate and intrinsic fluorescence. Biochem J 2002;364:15–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sugiyama T, Okuno T, Fukuhara M, Oku H, Ikeda T, Obayashi H, Ohta M, Fukui M, Hasegawa G, Nakamura N: Angiotensin II receptor blocker inhibits abnormal accumulation of advanced glycation end products and retinal damage in a rat model of type 2 diabetes. Exp Eye Res 2007;85:406–412 [DOI] [PubMed] [Google Scholar]
- 43.Olson S, Oeckler R, Li X, Du L, Traganos F, Zhao X, Burke-Wolin T: Angiotensin II stimulates nitric oxide production in pulmonary artery endothelium via the type 2 receptor. Am J Physiol Lung Cell Mol Physiol 2004;287:L559–568 [DOI] [PubMed] [Google Scholar]
- 44.Leal EC, Manivannan A, Hosoya K, Terasaki T, Cunha-Vaz J, Ambrósio AF, Forrester JV: Inducible nitric oxide synthase isoform is a key mediator of leukostasis and blood-retinal barrier breakdown in diabetic retinopathy. Invest Ophthalmol Vis Sci 2007;48:5257–5265 [DOI] [PubMed] [Google Scholar]
- 45.Zheng L, Du Y, Miller C, Gubitosi-Klug RA, Ball S, Berkowitz BA, Kern TS: Critical role of inducible nitric oxide synthase in degeneration of retinal capillaries in mice with streptozotocin-induced diabetes. Diabetologia 2007;50:1987–1996 [DOI] [PubMed] [Google Scholar]
- 46.Kubes P, Suzuki M, Granger DN: Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci U S A 1991;88:4651–4655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmetterer L, Polak K: Role of nitric oxide in the control of ocular blood flow. Prog Retin Eye Res 2001;20:823–847 [DOI] [PubMed] [Google Scholar]
- 48.Du Y, Smith MA, Miller CM, Kern TS: Diabetes-induced nitrative stress in the retina, and correction by aminoguanidine. J Neurochem 2002;80:771–779 [DOI] [PubMed] [Google Scholar]
- 49.Berkowitz BA, Luan H, Gupta RR, Pacheco D, Seidner A, Roberts R, Liggett J, Knoerzer DL, Connor JR, Du Y, Kern TS, Ito Y: Regulation of the early subnormal retinal oxygenation response in experimental diabetes by inducible nitric oxide synthase. Diabetes 2004;53:173–178 [DOI] [PubMed] [Google Scholar]
- 50.Mauer M, Zinman B, Gardiner R, Suissa S, Sinaiko A, Strand T, Drummond K, Donnelly S, Goodyer P, Gubler MC, Klein R: Renal and retinal effects of enalapril and losartan in type 1 diabetes. N Engl J Med 2009;361:40–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.