Abstract
Background/aims
To report the long term outcomes of photorefractive keratectomy (PRK) for the treatment of hyperopia associated with purely refractive accommodative esotropia.
Methods
Retrospective chart review of 40 patients age 17–39 who underwent PRK to eliminate their dependence on glasses. Pre and post-operative best spectacle corrected visual acuity (BSCVA), uncorrected visual acuity (UCVA), refractive spherical equivalent (SEQ), ocular alignment, and stereoacuity were reviewed.
Results
Forty patients (80 eyes) with mean age 27.9 years were treated for a mean pre-operative SEQ of +3.06D hyperopia. The mean final post-operative SEQ was +0.06. Pre-operative BSCVA was 0.04 logMAR, and did not change post-operatively. Mean UCVA significantly improved from 0.30 logMAR preoperatively to 0.08 logMAR post-operatively. Mean pre-operative esotropia at distance and near was 18.6 PD. All patients were orthophoric without correction at the one month, one year, and final post-operative evaluations. Visual acuity, refractive error and alignment remained stable after the one year post-operative examination. Stereoacuity was unchanged in 80% of patients postoperatively. There were no complications.
Conclusion
PRK can be used to treat low to moderate hyperopia associated with purely refractive accommodative esotropia in young adults.
Keywords: hyperopia, accommodative esotropia, refractive surgery, photorefractive keratectomy
Introduction
PRK and laser in situ keratomileusis (LASIK) have both been used to treat refractive accommodative esotropia, but the patient characteristics and outcomes vary from series to series, and most series report only a short follow-up interval.1–8 In 2003 we published the short-term results of a small series of eight young adults who underwent photorefractive keratectomy (PRK) to treat purely refractive accommodative esotropia.4 The purpose of this paper is to report the long-term outcomes of those patients, and to present the results of additional patients who have undergone the same treatment since the time of our first publication.
Materials and methods
We reviewed the medical records of consecutive patients with hyperopia and purely refractive accommodative esotropia who underwent refractive surgery to eliminate their dependence on glasses. Patients with less than one year of follow-up were excluded. Patients were not offered refractive surgery if they were found to have any ocular pathology other than esotropia, hyperopia, or amblyopia on their pre-operative evaluation. This evaluation included visual acuity determination, anterior and posterior segment examination, intra-ocular pressure measurement, orthoptic evaluation, topography of anterior and posterior corneal surfaces, evaluation of corneal endothelium with specular microscopy, and corneal pachymetry.
We recorded the patient's best spectacle corrected and uncorrected pre-operative and post-operative visual acuities. Cycloplegic retinoscopy and auto-refractometry were used to determine the refractive error; total hyperopia (manifest and latent hyperopia) was determined by instilling 2 drops of cyclopentolate 1.0% 10 minutes apart and performing retinoscopy 30 minutes after instillation of the second drop. Subjective determination of manifest hyperopia was also used. The target correction was the maximum spherical correction that could be given without decreasing visual acuity at distance when the patient was not cyclopleged (manifest hyperopia), and was within 0.50D of the total hyperopia in all eyes. All patients underwent a successful one-week contact lens simulation prior to proceeding with PRK. The strabismic angle was evaluated using the millimetric cover test9 by measuring, with a millimeter ruler, the limbus shift of the nonfixating eye upon assuming fixation with the cover test. Each millimeter of temporal limbus shift corresponds to an adduction of about 4.6 degrees, and each millimeter of nasal limbus shift to an abduction of about 4.8 degrees. This test was used to determine the amount of esotropia present at distance and near with and without correction. Degrees of deviation were then converted to prism diopters using the formula: PD = degrees × 1.75. All patients were orthophoric with correction in place. Since all patients' distance and near deviations were the same (purely refractive accommodative esotropia with a normal AC/A ratio), and since all stereopsis data were obtained at near only, sensory and motor data are reported for the near deviation. Stereopsis was measured The Randot® Preschool Stereoacuity Test SO-007 (Stereo Optical Co., Inc. | 8623 W. Bryn Mawr Ave., Suite 502 Chicago, IL 60631 USA) with glasses or contact lenses prior to PRK and without correction afterward.
All patients underwent photorefractive keratectomy using the Chiron Technolas 217 eximer laser (Chiron, Claremont, CA). One surgeon (PN) performed all surgeries. The instruments and laser parameters were the same as those used for correction of hyperopia in adult patients without accommodative esotropia and have been previously reported.10, 11
All patients underwent bilateral simultaneous procedures because this minimized the disruption of binocularity, consolidated the recovery period, and is preferred over sequential unilateral procedures by the surgeon. All procedures were performed with the use of topical anesthesia consisting of ossibuprocaine or lidocaine 2%. Manual removal of corneal epithelium was performed using 20% alcohol and either a blade or sponge. Each patient self-fixated on a target, and the fellow eye was patched during treatment. Standard hyperopic nomograms were employed. Post-operatively, the patients wore a soft contact lens for 4 days and instilled tobramycin 0.3% solution twice a day for five days. Fluorometholone 0.1% eye drops were instilled three times a day and were continued for up to 4 months, with the dosage titrated based on return of best corrected acuity to pre-operative baseline. Artificial tears were prescribed for use 3 or 4 for times a day for 2 months. Patients took ibuprofen as needed for symptomatic relief of pain over the first five post-operative days.
We obtained informed consent from the patients (and, in the case of one minor child, his parents) acknowledging that the intended result of treatment was to correct both hyperopia and esotropia. Patients were fully aware that they were among the first patients to undergo refractive surgery for the correction of strabismus, and that no long-term outcome data for such treatment were available. Being a retrospective case series, the study was exempt from Institutional review by the University of Milan and received exempt approval from the Emory University School of Medicine Institutional review board after being submitted for review. All procedures were carried out in accordance with the declaration of Helsinki.
Statistical significance was determined using the 2-tailed, paired students t-test; values were considered statistically significant if p was less than 0.05. Snellen fractions were converted to logMAR equivalent for statistical analysis. We compared the various parameters between time intervals (short term = pre-operative examination to one-month examination, intermediate term = one-month examination to one-year examination, long term = one year examination to final examination). When comparing long-term results, patients with less than 2 years of follow-up were excluded from the analysis.
Results
Forty patients (80 eyes) were included in the study. (Table) Nineteen patients were male. The mean patient age was 27.9 (range 17–39) years. Twelve patients with amblyopia, (defined as two or more lines of difference in best corrected Snellen visual acuity) were identified preoperatively, although no eye with amblyopia had visual acuity less than 20/40 (logMAR 0.3). Mean follow-up was 3.4 years (range 1–6 years).
Table.
Patient Characteristics
| Total number of patients | 40 |
| Mean patient age (range) | 27.9 (17–39) |
| Percentage of male patients | 47.5% |
| Mean pre-operative uncorrected distance deviation | 18.7 PD (range 14–24.5) |
| Mean pre-operative uncorrected near deviation | 18.7 PD (range 14–24.5) |
| Mean post-operative uncorrected distance deviation* | 0 PD (range 0–0) |
| Mean post-operative uncorrected distance deviation* | 0 PD (range 0–0) |
| Mean pre-operative UCVA | 0.3 log MAR (range 0–0.7) |
| Mean post-operative (1 month) UCVA | 0.3 logMar (range 0–0.7) |
| Mean post-operative (1 year) UCVA | 0.08 logMAR (range 0–0.3) |
| Mean pre-operative BSCVA | 0.04 logMAR (range 0–0.3) |
| Mean post-operative (1 month) BSCVA | 0.15 logMAR (range |
| Mean post-operative (1 year) BSCVA | 0.04 logMAR |
| Mean pre-operative SEQ | +3.06 ± 0.83 D |
| Mean post-operative (1 month) SEQ | −0.95 ± 0.41 D |
| Mean post-operative (1 year) SEQ | +0.06 ± 0.15 D |
| Mean pre-op stereopsis | 55 sec arc (range 40–200) |
| Mean post-op stereopsis (1 year) | 54 sec arc (range 40–200) |
data were the same for one month and one year time intervals
BSCVA = best spectacle corrected visual acuity
UCVA = uncorrected visual acuity
SEQ = spherical equivalent
PD = prism diopter
Visual acuity outcomes
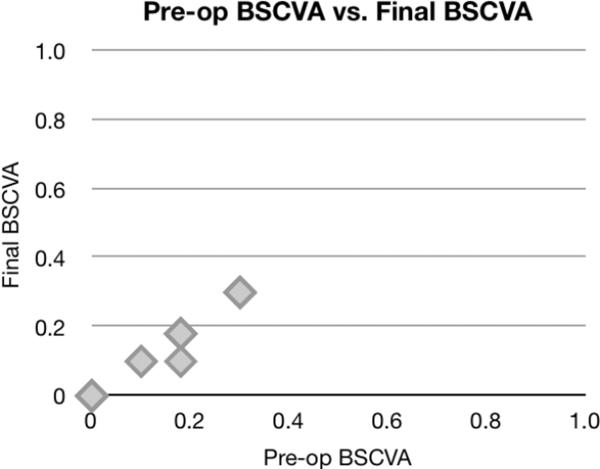
The mean pre-operative BSCVA was 0.04 logMAR (range 0 logMAR to 0.3 logMAR). Mean BSCVA at one-month post-operative exam was 0.15 logMAR, which represents a statistically significant reduction in visual acuity (p < 0.0001). A decrease in BSCVA was observed at the one-month examination in 57 of 80 eyes. During this interval, one patient had a reduction of 4 lines BSCVA in one eye. These decreases in BSCVA were attributed to temporary tear film instability, since no other plausible etiology could be identified. No patient had more than trace to mild haze, and haze, when present was located outside the visual axis. No other patient had a reduction of more than two lines BSCVA at the one-month post-operative examination. All patients responded well to the use of soft contact lens, Fluorometholone 0.1% eye drops, artificial tears, and ibuprofen for symptomatic relief of pain and blurred vision over the initial post-operative weeks. The mean BSCVA returned to the pre-operative level (0.04 logMAR) at the one-year post-operative examination (Figure 1). There was no statistically significant change in the final mean BSCVA when compared to pre-operative (p = 0.24) or the one-year post-operative mean BSCVA (p = 0.93).
Figure 1.
Safety: pre-operative vs. postoperative best spectacle corrected visual acuity (logMAR)
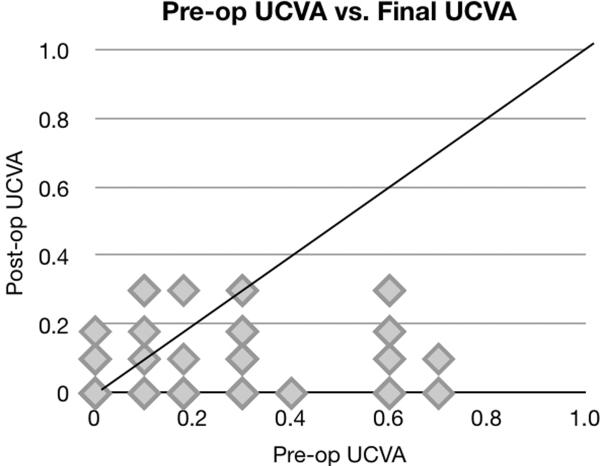
The mean pre-operative UCVA was 0.3 log MAR (range 0 logMAR to 0.7logMAR). The mean post-operative UCVA was 0.08 logMAR at the one-year post-operative examination (Figure 2). This improvement in UCVA was statistically significant (p < 0.0001). At the one-year post-operative examination the UCVA was 0.3 logMAR (20/40) or better in all eyes. It improved in 64 of 80 eyes, was unchanged in 9 eyes and decreased in 7 eyes. There was no statistically significant change in mean UCVA at the final follow-up examination when compared to the mean UCVA at the one-year post-operative follow-up examination (p = 0.07) although there was a trend toward improvement.
Figure 2.
Refractive Efficacy: pre-operative uncorrected visual acuity vs. post-operative uncorrected visual acuity (logMAR)
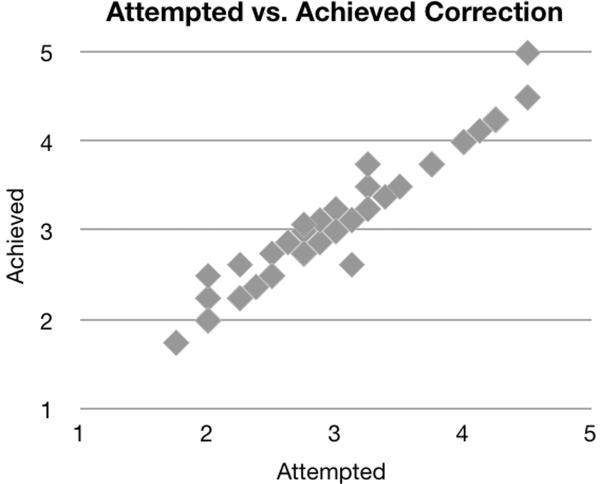
Refractive outcomes
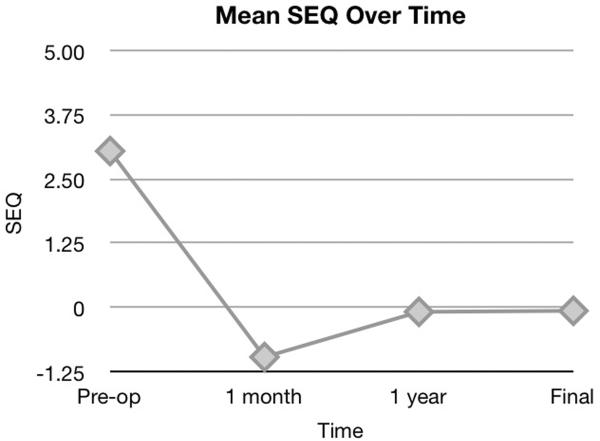
The mean spherical equivalent (SE) was +3.06 ± 0.83 D (SD) preoperatively, was −0.95 ± 41 D at the one month evaluation, was −0.07 ± 0.13 D at the one year evaluation and was 0.06 ± 0.15 D at the final evaluation (Figure 3). All eyes were within ± 0.5 D of emmetropia at the final evaluation. A mean hyperopic regression of 0.88 D (95% confidence interval 0.78 to 0.98) was observed between the one-month and one-year evaluation and was statistically significant (p < 0.0001). There was a mean change of 0.02 (95% confidence interval −0.01 to 0.05) between the one-year and the final evaluation, which was not statistically significant (p = 0.24) (Figure 4). No enhancements were required or performed. No patients required glasses or contact lenses postoperatively.
Figure 3.
Predictability: attempted vs. achieved spherical equivalent
Figure 4.
Refractive Stability: mean spherical equivalent over time
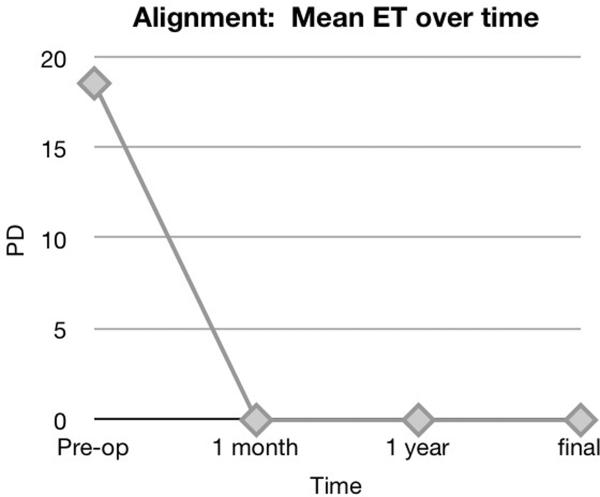
Alignment outcomes
The mean preoperative esotropic deviation at near and at distance without correction was 18.6 prism diopters (range 14 to 24.5). All patients had a normal AC/A ratio both pre and post-operatively. All patients were orthophoric at distance and near without correction at the one-year post-operative evaluation and at all subsequent evaluations (Figure 5). This change was statistically significant (mean change 18.6PD, confidence interval 17.6–19.7; p < 0.0001)
Figure 5.
Alignment stability: mean uncorrected ocular alignment at 1 month, 12 months and final follow-op examinations (distance and near alignment was the same in all patients since they all had a normal AC/A ratio).
Sensory outcome
Thirty-two patients (80%) had no change in stereoacuity; four patients had an increase in stereoacuity after PRK (two patients gained 60 seconds of arc and two patients gained 30 seconds of arc), and four patients had a loss of stereoacuity after surgery (30 seconds of arc each). There was no change in stereoacuity between the one-year and the final follow-up examination.
Subjective Outcomes
Although we did not solicit the patient's subjective response to the outcome of their surgery with a formal survey, all patients informally reported satisfaction with the functional and aesthetic results.
Complications
There were no intra-operative or post-operative complications. There were no infections, decentered ablations or unexpected refractive outcomes. Minimal (trace to 1+) haze and tear film instability was seen in some patients and resolved with the post-operative medication regimen within 4 months in all patients with corresponding return of BSCVA to pre-operative levels. Initial postoperative myopia resolved as hyperopic regression ensued over the first postoperative year.
Discussion
Our results confirm our prior conclusion that PRK can be used successfully to treat hyperopia and esotropia associated with purely refractive accommodative esotropia in patients with hyperopia < 5D. Although hyperopic regression was seen between the first post-operative month and the one year post-operative evaluation, we found that refractive error and motor alignment remained stable after the first post-operative year in our population of patients who were followed for as many as six years. Only very minor changes in stereoacuity were seen after PRK, with 4 patients having improvements in stereoacuity, and 4 patients having a reduction of 30 sec arc stereoacuity each. These changes in stereoacuity were attributed to testing variability since no other plausible explanation could be identified, and since an equal number of patients “gained” as “lost” stereoacuity.
Both PRK and laser in situ keratomileusis (LASIK) have been used to treat refractive accommodative esotropia, but the patient characteristics and outcomes vary from series to series.1–8 Sabetti and co-authors compared PRK and LASIK for the treatment of refractive accommodative esotropia in young adults, and they found no difference in the mean post-operative angle of esotropia between the two modalities.7 No comparison was made of the refractive outcomes between the two modalities; however, the mean attempted correction in the PRK group was 4.6D and the mean attempted correction in the LASIK group was 6.64D, suggesting that LASIK was the preferred modality for larger magnitudes of hyperopia. All of the patients were given a 30 day contact lens trial to help predict the sensory and motor outcomes of the proposed refractive surgery. They did not observe any complications, and no patients required retreatment. These authors attribute their success in part to their use of a 30 day contact lens trial period, and recommend such a trial for all patients. They also caution against the use of refractive surgery to treat accommodative esotropia in children whose refractive status is not yet stable.
Phillips and co-authors reported a series of 15 pediatric and adolescent patients ranging in age from 9 to 18 years, who were treated with LASIK for both fully and partially accommodative esotropia.6 Although all patients in this series ultimately were able to discontinue spectacle or contact lens use, some required retreatment. The authors reported a mean undercorrection rate of 34% ± 17%, which they attributed to the high variability inherent in hyperopic LASIK. The authors suggest that the development of a different nomogram might be beneficial, although it is also interesting to note that their mean spherical treatment attempted was +4.5D, which was 0.85 D less than the mean preoperative spherical equivalent refraction of +5.35D. There were no other complications reported in this series
Farahi and Hasheim treated 10 patients with fully and partially accommodative esotropia ages 11 to 43 with LASIK.2 The attempted correction in these patients was the full cycloplegic refraction and ranged from +2.5 to +8.75D (mean +5.03). One year post- operatively, the mean cycloplegic refraction was +1.68 D (range −0.50 to +4.00). There was a mean hyperopic regression of 0.68D between the one month and the one year post-operative evaluations. All patients had a reduction in their esodeviation after LASIK, and there was no significant difference in the post-operative uncorrected ocular alignment and the pre-operative spectacle corrected alignment, which was the intended goal of the surgery. Complications included one corneal abrasion which led to scar formation and a loss of single line of BSCVA in one eye, and irregular astigmatism, which led to the loss of one line of BSCVA in both eyes of one patient.
Dvali et al treated 63 eyes of 46 hyperopic children ranging in age from 8 to 16 years with LASIK.12 The spherical equivalent refraction of these eyes ranged from +1.0 to + 6 D and hyperopic astigmatism ranged from +1.0 to +5.5D, and all eyes were treated for their total hyperopia. Although detailed data were not given, there was a significant improvement in UCVA, amblyopia, the angle of strabismic deviation, and binocularity in the series of children. These findings were stable three to six months after treatment. Complications were not discussed in the paper. The authors advocate LASIK for school-aged children with severe anisometropia and high astigmatism if refractive stability can be documented for six to 12 months.
Hoyos and coauthors reported the outcomes of LASIK to treat refractive accommodative esotropia in nine adults ranging in age from 18 to 38 years (mean 28).3 Patients were followed for 20 months. The mean pre-operative spherical equivalent of these patients' eyes was +5.01D (range +2.5 to +7.0) preoperatively, and +0.06D (range −0.75 to +1.25) post-operatively. Half of the eyes required retreatment within three to five months of the initial treatment. Mean UCVA significantly improved, and there was no significant change in mean BSCVA, although four eyes lost one line of visual acuity and one eye gained one line. Post-operatively, all patients were orthophoric without optical correction or maintained their spectacle-corrected pre-operative microesotropia. Complications in this study included topographic decentration in three eyes, superficial punctate epitheliopathy in two eyes, and peripheral epithelialization in two eyes after retreatment. One patient with decentration complained of glare and night halos.
Stidham et al reported a series of 24 patients (48 eyes) treated with LASIK for accommodative estropia.8 Among these patients, 10 were classified as having purely refractive accommodative esotropia. Of these 10 patients, only two became orthophoric after LASIK, four patients converted from an esotropia preoperatively to an esophoria post-operatively, and four showed no reduction in their deviation. In these patients, the mean pre-operative spherical equivalent was +7.36 with a mean attempted correction of 6D, and the post-operative spherical equivalent averaged 2.1D. Interestingly, there were a number of patients in their study who were orthophoric post-operatively, in spite of a residual hyperopic refractive error of over 2 D. In Stidham's series, visually significant flap striae were seen in 25% of eyes, decentered ablations were seen in 8% of eyes, DLK was treated in 4% of eyes, and 23% of patients lost one or more lines of best corrected visual acuity.
With the exception of Sabetti et al, our previously reported series4, 5 and a single case report1, the remainder of published reports utilize LASIK as opposed to PRK to treat refractive accommodative esotropia. Proponents of LASIK cite the ability to correct larger refractive errors, better predictability, faster healing times, less postoperative discomfort, less haze, shorter course of post-operative steroids, avoidance of post-operative contact lens use and preservation of Bowman's membrane as advantages of LASIK over PRK. Although we agree that LASIK allows for the correction of larger magnitudes of hyperopia than PRK, our results suggest that for small to moderate hyperopic refractive errors (< 5D) associated with refractive accommodative esotropia PRK is predictable and safe. None of our patients had post-operative residual hyperopia, in contrast to most of the above-cited studies, in which a substantial number of patients were left under-corrected or required retreatment.2, 3, 6 Although several of the above studies2, 3, 6, 8 showed that good alignment can be achieved even in patients with residual hyperopia, other series have shown unpredictable alignment when residual hyperopia is present.8 In our series, we limited treatment to patients with 4.75D of hyperopia or less, and within this range, we have not been faced with the need to retreat patients for residual hyperopia. We believe that the extra measure of safety provided by PRK warrants consideration, especially if refractive surgery is being considered in school-aged children and young adults, in whom the risks of flap complications and corneal ectasia are likely to be of greater concern.
Limitations of our study include its retrospective nature, lack of a comparison group, failure to measure patient satisfaction, and limited generalizability because of select patient population with low to moderate hyperopia.
In conclusion, PRK is an effective means to correct low to moderate hyperopia and esotropia in patients with purely refractive accommodative esotropia, and can eliminate the need for spectacle correction. We recommend that PRK be considered as an acceptable modality to treat mild to low moderate hyperopia associated with purely refractive accommodative esotropia.
Acknowledgments
Supported in part by an unrestricted grant to the Emory Eye Center from Research to Prevent Blindness, Inc., New York, New York.
Footnotes
Competing interest: None declared
Accepted for presentation at the 35th Annual Meeting of The American Association of Pediatric Ophthalmology and Strabismus, April 17–21 2009, San Francisco, CA.
References
- 1.Bilgihan K, Akata F, Or M, Hasanreisoglu B. Photorefractive keratectomy in refractive accommodative esotropia. Eye. 1997;11(Pt 3):409–10. doi: 10.1038/eye.1997.86. [DOI] [PubMed] [Google Scholar]
- 2.Farahi A, Hashemi H. The effect of hyperopic laser in situ keratomileusis on refractive accommodative esotropia. European Journal of Ophthalmology. 2005;15(6):688–94. doi: 10.1177/112067210501500606. [DOI] [PubMed] [Google Scholar]
- 3.Hoyos JE, Cigales M, Hoyos-Chacon J, et al. Hyperopic laser in situ keratomileusis for refractive accommodative esotropia. Journal of Cataract & Refractive Surgery. 2002;28(9):1522–9. doi: 10.1016/s0886-3350(02)01433-5. [DOI] [PubMed] [Google Scholar]
- 4.Nucci P, Serafino M, Hutchinson AK. Photorefractive keratectomy for the treatment of purely refractive accommodative esotropia. Journal of Cataract & Refractive Surgery. 2003;29(5):889–94. doi: 10.1016/s0886-3350(03)00011-7. [DOI] [PubMed] [Google Scholar]
- 5.Nucci P, Serafino M, Hutchinson AK. Photorefractive keratectomy followed by strabismus surgery for the treatment of partly accommodative esotropia. Journal of Aapos: American Association for Pediatric Ophthalmology & Strabismus. 2004;8(6):555–9. doi: 10.1016/j.jaapos.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Phillips CB, Prager TC, McClellan G, Mintz-Hittner HA. Laser in situ keratomileusis for high hyperopia in awake, autofixating pediatric and adolescent patients with fully or partially accommodative esotropia. Journal of Cataract & Refractive Surgery. 2004;30(10):2124–9. doi: 10.1016/j.jcrs.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Sabetti L, Spadea L, D'Alessandri L, Balestrazzi E. Photorefractive keratectomy and laser in situ keratomileusis in refractive accommodative esotropia. Journal of Cataract & Refractive Surgery. 2005;31(10):1899–903. doi: 10.1016/j.jcrs.2005.03.077. [DOI] [PubMed] [Google Scholar]
- 8.Stidham DB, Borissova O, Borissov V, Prager TC. Effect of hyperopic laser in situ keratomileusis on ocular alignment and stereopsis in patients with accommodative esotropia. Ophthalmology. 2002;109(6):1148–53. doi: 10.1016/s0161-6420(02)01031-x. [DOI] [PubMed] [Google Scholar]
- 9.Paliaga GP, Ghisolfi A, Giuna G, Decarli A. Millimetric cover test--a linear strabismometric technique. Journal of Pediatric Ophthalmology and Strabismus. 1980;17(5):331–6. doi: 10.3928/0191-3913-19800901-16. [DOI] [PubMed] [Google Scholar]
- 10.Vinciguerra P, Epstein D, Radice P, Azzolini M. Long-term results of photorefractive keratectomy for hyperopia and hyperopic astigmatism. J Refract Surg. 1998;14(2 Suppl):S183–5. doi: 10.3928/1081-597X-19980401-08. [DOI] [PubMed] [Google Scholar]
- 11.Pacella E, Abdolrahimzadeh S, Gabrieli CB. Excimer laser photorefractive keratectomy for hyperopia. Ophthalmic Surg Lasers. 2001;32(1):30–4. [PubMed] [Google Scholar]
- 12.Dvali ML, Tsintsadze NA, Mirtskhulava SI. Features of hyperopic LASIK in children. Journal of Refractive Surgery. 2005;21(5 Suppl):S614–6. doi: 10.3928/1081-597X-20050902-11. [DOI] [PubMed] [Google Scholar]