Abstract
Background
Midclavicular fractures are common clinically, accounting for about 76% of all clavicular fractures. Recent studies have revealed a previously unrecognized incidence of nonunion and malunion after conservative treatment of more severe midclavicular fractures. Our aim was to evaluate the clinical outcomes of midclavicular fractures treated with titanium elastic nails.
Methods
From February 2005 to February 2007, 41 patients with displaced midclavicular fractures received open reduction and internal fixation with a titanium elastic nail inserted through the sternal end of the clavicle. We evaluated the visual analogue scale (VAS), the Constant score and the Disabilities of the Arm, Shoulder and Hand (DASH) scale to determine outcomes.
Results
A mean follow-up of 14.5 months (range 7–24 mo) revealed radiographic fracture union in all patients with an average clinical healing time of 2.2 months. Mean subjective pain 3 days after surgery was significantly lower than the day before surgery (p < 0.001). The mean range of motion 3 days after surgery was significantly improved compared with the day before surgery (p < 0.001). The nails were removed in all patients a mean of 7.2 months (range 5.4–9.5 mo) after surgery, and no fractures recurred. The mean postoperative DASH score was 2.5 (range 0.5–8.0) and the mean postoperative Constant score was 95.2 (range 86.5–97.0).
Conclusion
Limited open reduction and internal fixation with titanium elastic nails is a safe and minimally invasive surgical procedure for the treatment of displaced midclavicular fractures in adults and achieves good functional results and high patient satisfaction.
Abstract
Contexte
Les fractures médioclaviculaires sont fréquentes et représentent quelque 76 % du total des fractures de la clavicule. Des études récentes ont révélé une incidence auparavant non reconnue de non-consolidation et de mauvaise consolidation après un traitement conservateur de fractures médioclaviculaires plus graves. Nous voulions évaluer l’issue clinique des fractures médioclaviculaires réduites au moyen de clous élastiques en titane.
Méthodes
De février 2005 à février 2007, 41 patients victimes d’une fracture médioclaviculaire déplacée ont subi une intervention ouverte de réduction et de fixation interne au moyen d’un clou élastique en titane inséré par l’extrémité sternale de la clavicule. Nous avons évalué l’échelle visuelle analogue (EVA), le score de Constant et l’échelle des incapacités du bras, de l’épaule et de la main (Disabilities of the Arm, Shoulder and Hand — DASH) pour déterminer les résultats.
Résultats
Un suivi moyen à 14,5 mois (intervalle de 7 à 24 mois) a révélé à la radiographie une consolidation de la fracture chez tous les patients dont la durée moyenne de guérison clinique s’est établie à 2,2 mois. La douleur subjective moyenne 3 jours après l’intervention chirurgicale était beaucoup moins forte que la veille de l’intervention (p < 0,001). L’amplitude moyenne du mouvement 3 jours après l’intervention chirurgicale était beaucoup améliorée comparativement à la veille de l’intervention (p < 0,001). Les clous ont été retirés chez tous les patients en moyenne 7,2 mois (intervalle de 5,4 à 9,5 mois) après l’intervention et il n’y a eu aucune récidive des fractures. Le score DASH postopératoire moyen s’est établi à 2,5 (intervalle de 0,5 à 8,0) et le score de Constant moyen après l’intervention était de 95,2 (intervalle de 86,5 à 97,0).
Conclusion
Une réduction ouverte limitée et la fixation interne au moyen de clous élastiques en titane constituent une intervention chirurgicale sécuritaire et à effraction minimale pour traiter la fracture médioclaviculaire déplacée chez les adultes, qui produit de bons résultats fonctionnels et un taux élevé de satisfaction chez les patients.
Midclavicular fractures are common clinically, accounting for about 76% of all clavicular fractures. Nondisplaced or minimally displaced midclavicular fractures respond well to conservative treatment.1 However, recent studies have revealed a previously unrecognized incidence of nonunion and malunion after conservative treatment of more severe midclavicular fractures.2–4 Hill and colleagues3 reported that when midclavicular fractures with a bone shortening of more than 2 cm in length were treated conservatively, a 15% incidence of nonunion could result, and 31% of the patients would be dissatisfied with their outcomes. Robinson4 reported a nonunion rate of 21% in the treatment of displaced midclavicular fractures; thus, he considered substantial fracture displacement or comminution as risk factors for delayed union or nonunion. Nonunion of midclavicular fractures usually leads to shoulder pain, weakness and asymmetry, thus compromising function and cosmetic appearance. We herein evaluated the treatment of displaced midclavicular fractures using internal fixation with titanium elastic nails (TENs).
Methods
Patients
From February 2005 to February 2007, 41 patients had displaced midclavicular fractures treated by open reduction and internal fixation with TENs inserted through the sternal end of the clavicle. We classified the fractures based on the Orthopaedic Trauma Association (OTA) classification scheme for midclavicular fractures.5 Inclusion criteria included displacement of more than 2 cm and minimal to slight comminution; OTA type C fractures were excluded. Limited open reduction and internal fixation with a TEN was carried out in all cases within 1 week of injury. We obtained written informed consent from all participants, and the study protocol was approved by the ethics review board of Shanghai Sixth People’s Hospital.
Surgical technique
General anesthesia or combined brachial plexus–cervical plexus nerve block were administered, and the patient was placed in the beach chair position. About 1 cm lateral to the sternoclavicular joint, a horizontal incision 1 cm in length was made along the axis of the clavicle. According to the width of the medullary cavity, a suitable TEN of 2.5–3.0 mm in diameter was selected and inserted into the medullary cavity of the clavicle through its sternal end. In most patients, the diameter of the medullary cavity of the clavicle ranged from 2.8 to 3.0 mm, therefore, a 2.5-mm TEN was most commonly used. A 2.0-mm TEN was used if the diameter of the medullary cavity of clavicle was smaller, and a 3.0-mm TEN was used if the diameter was larger. At the fracture site, a curved incision 2 cm in length was made perpendicular to the clavicle shaft. The skin flap was retracted, taking care to preserve the branches of supraclavicular nerves. The fracture line was exposed without stripping the periosteum, and the TEN was advanced across the fracture site under direction visualization to reduce the fracture. The TEN was further advanced laterally under C-arm radiographic guidance until the nail tip reached the acromial end of the clavicle. Nail tip curvature was adjusted to optimize fracture realignment. The TEN was cut at the sternal end, leaving 1.0–1.5 cm extending out of the clavicle. The end of the TEN was buried subcutaneously.
Immediately after surgery, the affected limb was supported with a neck–wrist sling for 4 weeks. The sling prevented the arm from drooping and interfering with bone union while allowing passive exercises in the early postoperative period. Shrugging exercises began 1 day after surgery. When a forearm sling was required to support the affected limb, passive non–weight bearing exercises began immediately after surgery and were continued for 2 weeks. The range of shoulder abduction was gradually increased but kept within 90º during the first 3 weeks after surgery.
Outcome evaluation
We defined radiographic union as disappearance of the fracture line and satisfactory growth of inner and outer callus on radiographic examination. We defined clinical fracture healing as absence of tenderness with firm palpation over the fracture site, a full range of motion and the presence of normal strength of the upper extremity. We measured subjective pain with a visual analogue scale (VAS) 1 day before and 3 days after surgery. The VAS ranged from 0 (no pain) to 100 (worst pain imaginable). Patients were asked to mark a point on the scale corresponding to their pain at that time. We evaluated shoulder motion, including abduction and flexion, 1 day before and 3 days after surgery. We evaluated shoulder function with Constant6 and Disabilities of the Arm, Shoulder and Hand (DASH)7 scales at final follow-up.
The degree of patient satisfaction regarding treatment outcome was subjectively obtained by questioning patients during follow-up visits. We evaluated shoulder joint performance, including incision site numbness, redness and swelling, and obviousness of scars. In addition, we evaluated complications, including TEN migration or breakage, nonunion, symptomatic malunion and infection. The presence of clavicular malunion, defined as postunion shortening as compared with the unaffected side, was determined by radiographs. An experienced professor (B.Z.) who was not part of the surgical team performed the outcome evaluations, including the interpretation of radiographs. Shoulder joint performance was evaluated by the surgeons who performed the surgery.
Statistical analysis
We used SPSS version 10.0 statistical software (SPSS Inc.) to perform paired t tests on the pain visual analogue scale and the degree of shoulder mobility. We deemed differences to be statistically significant at p < 0.05.
Results
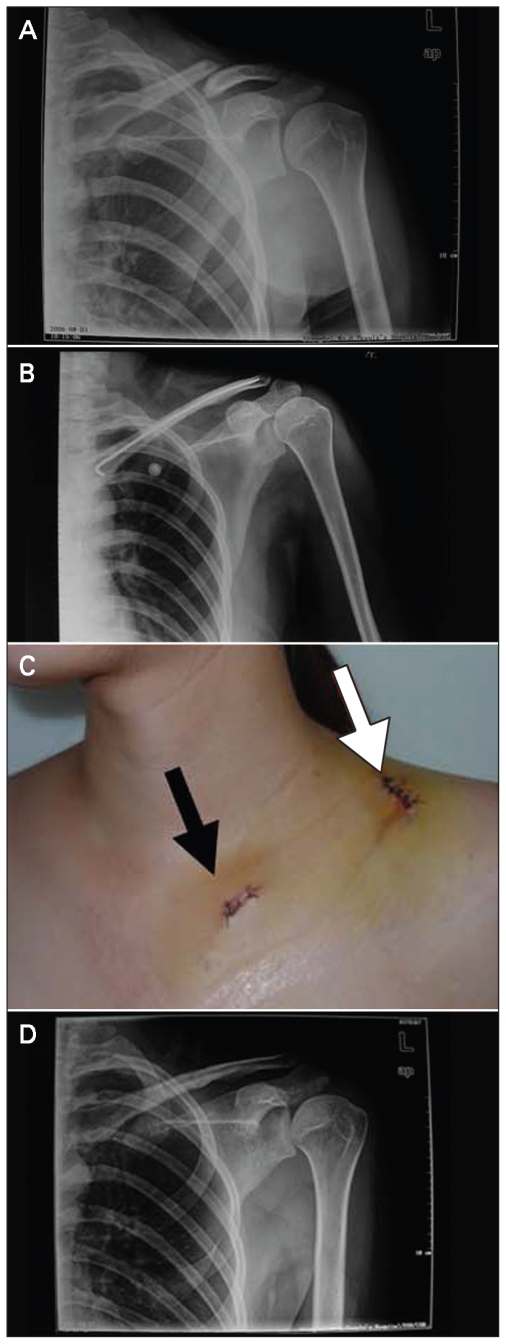
Of the 41 patients included in the study, there were 30 men and 11 women with a mean age of 38.3 (standard deviation [SD] 9.0, range 18–60) years. Patient demographic and clinical data are presented in Table 1. Based on the OTA classification scheme for midclavicular fractures,5 28 fractures were type A and 13 type B. The mean patient follow-up was 14.5 (SD 3.7, range 7–24) months. Clinical and radiographic healing occurred in all patients with a mean clinical healing time of 2.2 (SD 0.3) months (Table 2). No infection, hard wire breakage or migration occurred. The distal end of the TEN penetrated the cortex in 1 patient; however, function was not hindered. This was a short-term problem without any further complications or residual deficit. In this patient’s case, the final Constant and DASH scores were 86.5 and 8.0 points, respectively. The nails were removed from all patients after a mean period of 7.2 (range 5.4–9.5) months. No refractures after nail removal occurred. Healing in the anatomic position occurred in 38 patients, whereas bone shortening (as compared radiographically with the unaffected clavicle) over 5 mm in length was observed in 3 patients. A representative case is illustrated in Figure 1.
Table 1.
Demographic and clinical characteristics of 41 patients who received open reduction and internal fixation with a titanium elastic nail
| Characteristic | No. (%)* |
|---|---|
| Age, mean (SD) yr | 38.3 (9.0) |
| Sex | |
| Male | 30 (73.2) |
| Female | 11 (26.8) |
| Clavicle | |
| Left | 18 (43.9) |
| Right | 23 (56.1) |
| Cause of injury | |
| Motorcycle collision | 16 (39.0) |
| Falling off a bicycle | 8 (19.5) |
| Falling during sports | 11 (26.8) |
| Other activities | 6 (14.6) |
| OTA classification | |
| A | 28 (68.3) |
| B | 13 (31.7) |
OTA = Orthopaedic Trauma Association;
SD = standard deviation.
Unless otherwise indicated.
Table 2.
Clinical outcomes of 41 patients who received open reduction and internal fixation with a titanium elastic nail
| Outcome | Mean (SD) |
|---|---|
| Duration of follow-up, mo | 14.5 (3.7) |
| Healing time, mo | 2.2 (0.3) |
| Final Constant score | 94.7 (2.4) |
| Final DASH score | 2.5 (1.6) |
DASH = Disabilities of the Arm, Shoulder and Hand;
SD = standard deviation.
Fig. 1.
A 25-year-old woman with (A) midshaft clavicular fracture with clavicle shortening. (B) A postoperative radiograph shows good reduction. (C) Surgical incisions: the black arrow indicates the incision near the sternoclavicular joint where the titanium elastic nail (TEN) was inserted. The tail of the nail was buried and the incision closed. The white arrow indicates the incision for fracture reduction. (D) A radiograph after TEN removal.
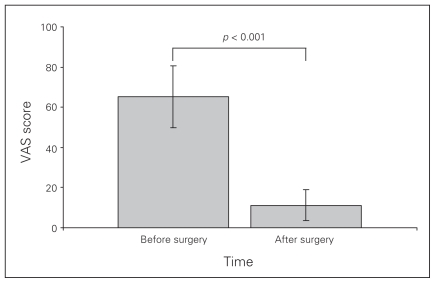
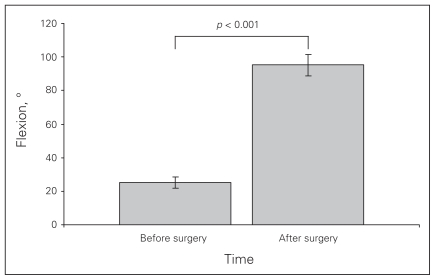
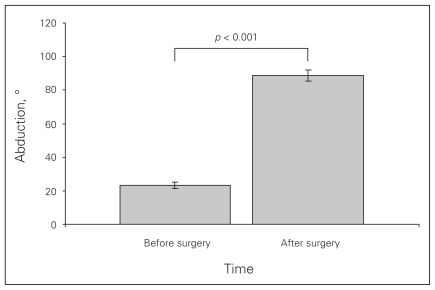
The mean VAS score decreased significantly from 15.5(SD 2.4) the day before surgery to 7.7 (SD 1.2) by the end of the third postoperative day (Fig. 2, p < 0.001). Preoperatively, mean shoulder flexion was 25.1° (SD 3.4°) and mean abduction was 23.3° (SD 1.9º). Three days after surgery, mean shoulder flexion was 95.1° (SD 4.6º) and mean abduction was 88.7° (SD 3.2º). Shoulder range of motion 1 day before surgery and 3 days after surgery demonstrated a significant difference (Figs. 3 and 4; both, p < 0.001).
Fig. 2.
Results of visual analogue scale (VAS) evaluation. Data are displayed as means and standard deviations.
Fig. 3.
Results of shoulder flexion evaluation. Data are displayed as means and standard deviations.
Fig. 4.
Results of abduction evaluation. Data are displayed as means and standard deviations.
No shoulder asymmetry was observed in this series. At each follow-up visit, patients were asked about any problems that had occurred. Slight numbness at the skin incision occurred in 2 (4.8%) patients. Skin redness and swelling at the nail entrance site occurred in 8 (19.5%) patients. One patient (2.4%) complained of an obvious scar at the skin incision.
At final follow-up, the mean shoulder joint Constant score was 95.2 (SD 1.9, range 86.5–97.0) points, and the mean DASH score was 2.5 (SD 1.6, range 0.5–8.0) points. All patients were satisfied with the treatment outcome except 2; 1 felt the incision scar was unpleasant and 1 complained of inconveniences in daily life because of penetration of the nail tip out of the lateral cortex until removal.
Discussion
In this study, we found that limited open reduction and internal fixation with TENs in the treatment of midclavicular fractures in adults resulted in a high fracture healing rate, rapid functional recovery and minimal complications. The procedure is minimally invasive and achieved high patient satisfaction.
Several options are available for the surgical treatment of clavicle shaft fractures, including plating and nailing. Plating is the most commonly used surgical treatment; however, plating requires relatively extensive periosteal stripping, which may increase destruction of the blood supply at the fracture site, thus hindering fracture healing. Stress shielding produced by rigid plates can lead to an 8% refracture rate after plate removal.8,9 Surgical time is considerable, and infection rates of up to 18% have been reported.8–11 Additionally, the relatively long scar can be a cosmetic issue in some patients, and some individuals experience discomfort induced by the plate underneath the skin. Fixation with TENs, though a newer therapeutic method, provides fixation that is more consistent with the physiologic bone structure to permit early functional exercise, leads to faster functional recovery, provides early pain relief and avoids the complications associated with longer operating time and periosteal stripping.
Anatomically, the clavicle has an irregular S shape. Titanium elastic nails, manufactured from titanium alloy, are elastic enough to match the shape of the medullary cavity and strong enough to stabilize the fragment ends. Their curved tip facilitates nail passage within the medullary cavity and allows it to be anchored to the distal cortex and fit tightly to the inner wall of the cavity, thus improving fixation stability. When placed, each nail provides 3 points for support within the medullary canal to effectively control rotation, angulation and shortening of the fragments.
Titanium elastic nails were initially designed for the treatment of diaphyseal and metaphyseal fractures of long bones in children. In 1996, they were used to treat displaced midclavicular fractures in 12 professional athletes, all of whom returned to training and competition after a mean period of 16.8 days.12 Jubel and colleagues13 reported only 1 case of nonunion in a series of 62 midclavicular fractures treated with TENs with mean follow-up of 3.5 years, and the mean postoperative Constant score was 95.2 points. Mueller and colleagues14 used TENs to treat 32 displaced midclavicular fractures. In that series, with follow-up ranging from 1 to 5 years, nonunion was not observed; however, 12 clavicles healed with a shortening of more than 5 mm. The nails were removed in 29 patients a median of 6 (range 1.3–15.0) months postoperatively, and no refracture occurred after TEN removal. The mean Constant score was 95.2 (SD 1.9) points and the mean DASH score was 5.0 (SD 2.3) points. Other studies have shown similar positive results with TENs for the treatment of clavicular fractures,15,16 though some authors point out that the procedure is technically demanding, and minor complications can be encountered in the postoperative phase.17
Our study, with a mean follow-up of 14.5 months, revealed union in all 41 patients. Except for 1 patients in whom the distal TEN pierced through the bone cortex, there were no other complications after TEN removal, and the final mean Constant and DASH scores were 95.2 and 2.5 points, respectively. We observed local skin irritation in early patients of this series when the medial end of the TEN was bent upwards with its tip located directly beneath the skin. This complication ceased to occur when nail end management was improved by bending it laterally.
It should be noted that TENs are only indicated in OTA type A and B midclavicular fractures. They are not suited for osteoporotic or/and comminuted fractures in which fixation with a TEN will not obtain 3-point support. The sharp-pointed end of the TEN may easily penetrate the cortical bone in osteoporotic patients, resulting in the TEN sliding and thus making the fixation unstable. In comminuted fractures, support from the middle point is not present, which may lead to unstable fixation, shortening and malunion.
To perform the procedure correctly, several technical points should be considered.
The diameter of the TEN should be correctly determined before placement to allow ease of insertion and prevent possible breakage during early postoperative functional exercises. A TEN that is too thick will dam-age the medullary canal, and one that is too narrow will not provide adequate stability.
The TEN should be inserted from the medial end of the clavicle laterally because the sternal end has a wider medullary cavity. However, the insertion point should not be located too medial, or sternoclavicular joint function may be affected.
The TEN should be long enough to reach the lateral end of the clavicle for better anchoring of its tip and to leave 1.0–1.5 cm extending out of the medial clavicle to facilitate tail bending and clipping, eliminating skin irritation.
A second incision is necessary in patients with substantial displacement where closed reduction is not possible. Without perfect reduction, the TEN cannot be inserted.
The entire insertion process of the TEN should be carried out under C-arm radiographic guidance.
Limitations
There are some limitations of the study that should be considered. The number of patients included was relatively small and nonrandomized, and there was no comparison or control group. We interpreted our results in comparison with those of the studies in the literature that used other methods. However, the outcomes achieved with the technique in this study were favourable. Many patients recovered completely within 3–6 months after surgery, and all patients had complete recovery by their final follow-up visit.
Conclusion
The treatment of displaced midclavicular fractures in adults with limited open reduction and internal fixation with a TEN is a safe and minimally invasive surgical procedure. A high bone union rate, good functional outcome, favourable patient satisfaction, early shoulder pain relief and functional recovery can be obtained with few complications. Randomized controlled trials with adequate follow-up are required to determine the optimal surgical method to treat midclavicular fractures.
Footnotes
Competing interests: None declared.
Contributors: Drs. Y.-f. Chen, Zeng and Chai designed the study. Drs. Y.-f. Chen, Y.-j. Chen, Wang, Xue, Xie and Zhang acquired the data, which Drs. Y.-f. Chen, Zeng, Xue and Chai analyzed. Dr. Y.-f. Chen wrote the article. All authors critically reviewed the article and approved its publication.
References
- 1.Jeray KJ. Acute midshaft clavicular fracture. J Am Acad Orthop Surg. 2007;15:239–48. doi: 10.5435/00124635-200704000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 3.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537–9. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 4.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–84. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 5.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(Suppl):S1–133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 6.Beaton DE, Katz JN, Fossel AH, et al. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14:128–46. [PubMed] [Google Scholar]
- 7.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 8.Böstman O, Manninen M, Pihlajamäki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma. 1997;43:778–83. doi: 10.1097/00005373-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Poigenfürst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: results of 122 operations. Injury. 1992;23:237–41. doi: 10.1016/s0020-1383(05)80006-3. [DOI] [PubMed] [Google Scholar]
- 10.Verborgt O, Pittoors K, Van Glabbeek F, et al. Plate fixation of middle-third fractures of the clavicle in the semi-professional athlete. Acta Orthop Belg. 2005;71:17–21. [PubMed] [Google Scholar]
- 11.Wu CC, Shih CH, Chen WJ, et al. Treatment of clavicular aseptic nonunion: comparison of plating and intramedullary nailing techniques. J Trauma. 1998;45:512–6. doi: 10.1097/00005373-199809000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Jubel A, Andemahr J, Bergmann H, et al. Elastic stable intra-medullary nailing of midclavicular fractures in athletes. Br J Sports Med. 2003;37:480–3. doi: 10.1136/bjsm.37.6.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jubel A, Andermahr J, Schiffer G, et al. Technique of intramedullary osteosynthesis of the clavicle with elastic titanium nails. Unfallchirurg. 2002;105:511–6. doi: 10.1007/s00113-001-0386-z. [DOI] [PubMed] [Google Scholar]
- 14.Mueller M, Burger C, Florczyk A, et al. Elastic stable intramedullary nailing of midclavicular fractures in adults: 32 patients followed for 1–5 years. Acta Orthop. 2007;78:421–3. doi: 10.1080/17453670710014013. [DOI] [PubMed] [Google Scholar]
- 15.Kettler M, Schieker M, Braunstein V, et al. Flexible intramedullary nailing for stabilization of displaced midshaft clavicle fractures: technique and results in 87 patients. Acta Orthop. 2007;78:424–9. doi: 10.1080/17453670710014022. [DOI] [PubMed] [Google Scholar]
- 16.Smekal V, Irenberger A, Struve P, et al. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23:106–12. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 17.Frigg A, Rillmann P, Perren T, et al. Intramedullary nailing of clavicular midshaft fractures with the titanium elastic nail: problems and complications. Am J Sports Med. 2009;37:352–9. doi: 10.1177/0363546508328103. [DOI] [PubMed] [Google Scholar]