Abstract
Background
Gallstone pancreatitis is a consequence of ampullary obstruction by common bile duct (CBD) calculi. Magnetic resonance cholangiopancreatography (MRCP) has been advocated for routine use to diagnose choledocholithiasis. However, the selective use of MRCP in clinically equivocal situations has not been explored until now. This study examines the diagnostic value of selective MRCP in gallstone pancreatitis.
Methods
We conducted a retrospective audit of all presentations of gallstone pancreatitis between January 2001 and December 2007 at Middlemore Hospital, Auckland, New Zealand. Demographic data, clinical presentation, biochemical and radiological findings and outcomes were reviewed.
Results
There were 339 cases of gallstone pancreatitis during the study period; 236 patients were women and the mean age was 52 years. Overall, choledocholithiasis was diagnosed in 95 patients. A total of 117 patients underwent MRCP within a median of 4 days of admission, with 15 (13.7%) showing choledocholithiasis. There was no significant difference in time to MRCP between positive and negative groups. Endoscopic retrograde cholangiopancreatography (ERCP)/intraoperative cholangiography (IOC) confirmed 13 of 15 stones within a median of 2.5 days. However, MRCP missed 8 cases of choledocholithiasis subsequently demonstrated on ERCP/IOC, where clinical suspicion remained after a negative MRCP. Its sensitivity was 62% and specificity 98%. The positive likelihood ratio was 6.5 and the negative likelihood ratio was 0.1. In all, 222 patients followed different clinical pathways with 82 CBD stones diagnosed by ERCP/IOC.
Conclusion
Selective MRCP is highly specific in gallstone pancreatitis but may not be sensitive enough to exclude choledocholithiasis in this context.
Abstract
Contexte
La pancréatite biliaire est une conséquence de l’obstruction de l’ampoule par des calculs du canal cholédoque. On a préconisé le recours à la cholangiopancréatographie par résonance magnétique (CPRM) comme mesure standard pour diag-nostiquer la cholédocholélithiase. Toutefois, l’emploi sélectif de la CPRM dans des situations cliniquement équivoques n’a fait l’objet d’aucune étude jusqu’à présent. La présente étude se penche sur l’utilité diagnostique de la CPRM sélective dans la pancréatite biliaire.
Méthodes
Nous avons effectué un examen rétrospectif de tous les cas de pancréatite biliaire répertoriés entre janvier 2001 et décembre 2007 au Middlemore Hospital d’Auckland, en Nouvelle-Zélande. Nous avons passé en revue les données démo-graphiques, les tableaux cliniques, les résultats d’analyses biochimiques et d’épreuves radiologiques, de même que l’issue chez les patients.
Résultats
Nous avons dénombré 339 cas de pancréatite biliaire au cours de la période de l’étude; 236 touchaient des femmes et l’âge moyen était de 52 ans. Globalement, la cholédocholélithiase était le diagnostic chez 95 patients. En tout, 117 patients ont subi une CPRM après une période médiane de 4 jours suivant leur admission, 15 d’entre eux (13,7 %) présentant des signes de cholédocholélithiase. On n’a noté aucune différence significative quant à l’intervalle avant la CPRM entre les groupes positifs et négatifs. La cholangiopancréatographie endoscopique rétrograde (CPER)/cholangiographie peropératoire (CPO) ont confirmé 13 calculs sur 15 au cours d’une période médiane de 2,5 jours. Toutefois, la CPRM n’a pas réussi à mettre au jour 8 cas de cholédocholélithiase ultérieurement révélés par la CPER/CPO qui continuaient d’éveiller des soupçons cliniques après une CPRM négative. Sa sensibilité a été évaluée à 62 % et sa spécificité à 98 %. Le rapport positif probable était de 6,5 et le rapport négatif probable de 0,1. En tout, 222 patients ont fait l’objet de démarches cliniques différentes et 82 cas de calculs du cholédoque ont été diagnos-tiqués au moyen de la CPER/CPO.
Conclusion
La CPRM sélective est fortement spécifique dans les cas de pancréatite biliaire, mais pourrait ne pas être suffisamment sensible pour exclure la cholédocholélithiase dans ce contexte.
Gallstone pancreatitis is a consequence of ampullary obstruction by common bile duct (CBD) calculi.1 Successful management of gallstone pancreatitis therefore requires accurate diagnosis and, occasionally, removal of CBD stones.2,3 Until recently, endoscopic retrograde cholangiopancreatography (ERCP) was used to both diagnose and remove CBD stones.3,4 However, ERCP is associated with substantial morbidity and variable rates of technical failure, and it is only of benefit to those patients who actually have CBD stones.5,6 Consequently, diagnostic ERCP has fallen out of favour in clinical practice in this context.4
Magnetic resonance cholangiopancreatography (MRCP) has been advocated as the investigation of choice to detect choledocholithiasis as it represents a low-risk alternative to ERCP.7 Previous studies have reported sensitivities and specificities of 95%–97% for detection of CBD stones with MRCP.7–10 As a consequence, some institutions use MRCP as a first-line investigation.7,8,10 However, other studies investigating the value of MRCP specifically in gallstone pancreatitis have been less encouraging, reporting lower sensitivities of 80%–82%.11,12 Owing to issues of cost and availability, MRCP is often used selectively in hospitals.9,13,14 These considerations have prompted our institution to use MRCP selectively when available clinical, biochemical and radiological (ultrasound) evidence is equivocal regarding the presence of choledocholithiasis. To our knowledge, no studies have investigated the efficacy of MRCP when used selectively in this context. We aimed to assess the diagnostic value of MRCP in this setting.
Management of gallstone pancreatitis In Middlemore Hospital
Patients presenting to Middlemore Hospital (MMH), Aukland, New Zealand, with a suspected diagnosis of acute pancreatitis are triaged and referred to the surgical registrar on call. After a history and examination, blood tests are obtained with routine biochemical assays, including serum liver enzymes, bilirubin and amylase (liver function tests [LFTs]). An abdominal ultrasound is obtained to look for the presence of gallstones and screen for the presence of a CBD stone or CBD dilatation. If, based on these investigations, there is a strong clinical suspicion of choledocholithiasis, patients receive preoperative ERCP with subsequent laparoscopic cholecystectomy or undergo surgery with intraoperative cholangiography (IOC) depending on the surgeon’s preference. Cholecystectomy is performed during the index admission unless prevented by patient comorbidities or choice.9 In clinically equivocal scenarios (i.e., when clinical assessment, biochemical tests, including LFTs, and abdominal ultrasound cannot exclude choledocholithiasis or are not collectively convincing enough to suggest an ERCP is necessary), MRCP is used. All demonstrated CBD stones are removed either by preoperative ERCP or during surgery. If MRCP is negative, patients will only receive ERCP or IOC if a strong clinical suspicion persists regarding the presence of CBD stones. Patients do not undergo routine IOC as a policy of identifying clinically relevant stones is followed.
Methods
We searched the electronic database (Concerto 6.3) at MMH using International Classification of Diseases (ICD)-10 codes for patients discharged with a diagnosis of gallstone pancreatitis during the years 2001–07. Thereafter, we manually screened records to confirm the diagnosis of gallstone pancreatitis.
Gallstone pancreatitis was diagnosed based on clinical features with supporting biochemical evidence of amylase 3 times above normal and evidence of gallstones. We excluded patients with other causes of pancreatitis.
All scans were performed on the Siemens Vision 1.5 T magnetic resonance imaging machine. Three plane half-Fourier single-shot fast spin echo (HASTE) sequences were first performed followed by thick-slab HASTE images in several oblique coronal planes. Fine-slice maximum intensity projections were only occasionally used when a small distal stone was suspected. Two fellows of the Royal Australian and New Zealand College of Radiologists read the scans.
We recorded demographic, biochemical and radiological data, type of treatment received (operative or non-operative) and time to investigations and treatment. We defined CBD stones as “confirmed” when they were detected on either ERCP or IOC. All data were recorded and analyzed using SPSS 13.0 software.
Results
From 2001 to 2007, there were 339 patients with gallstone pancreatitis (236 women, 103 men, mean age 52 yr). Of these, 280 cases were mild and 59 were classified as severe according to the modified Glasgow criteria.15 Overall, 95 (28%) patients had choledocholithiasis, as confirmed by ERCP/IOC.
A total of 313 (92.3%) patients underwent ultrasound as the first radiological investigation, with the remainder either proceeding directly to MRCP (n = 15) or ERCP (n = 8). Three patients self-discharged. After ultrasound, patients either underwent MRCP (n = 102), ERCP (n = 132) or were managed operatively without further pre-operative imaging (n = 67). Twelve patients were managed nonoperatively. Patients progressed to either ERCP or IOC based on clinical suspicion and either ultrasound-demonstrated CBD stone (n = 29), ultrasound-demonstrated CBD dilation (n = 68) or obstructive LFTs (n = 102).
In all, 117 (34.5%) patients underwent MRCP within a median of 4 days of admission. Whereas there were heterogeneous indications (Table 1), most patients (102 of 117, 87%) underwent MRCP following equivocal ultrasound results and/or LFTs. Fifteen of 117 (13.7%) MRCPs were positive for choledocholithiasis. There was no significant difference in time to MRCP between positive and negative groups. Thirteen of 15 stones were confirmed on ERCP/IOC within a median of 2.5 days from MRCP. Magnetic resonance cholangiopancreatography missed 8 cases of choledocholithiasis subsequently demonstrated on ERCP/IOC. Overall performance of MRCP in this setting is displayed in Table 2.
Table 1.
Indications for and performance of magnetic resonance cholangiopancreatography
| Indication | No. of MRCPs | Result of MRCP, no. (%) | False positive | False negative | Sensitivity, % | Specificity, % | |
|---|---|---|---|---|---|---|---|
| Positive | Negative | ||||||
| US showed CBD stone, n = 29 | 4 | 3 (75) | 1 (25) | 0 | 0 | 100 | 100 |
| US showed no stone, no cholestasis on LFTs, n = 104 | 30 | 3 (10) | 27 (90) | 1 | 1 | 66.7 | 96.3 |
| US unclear, no cholestasis on LFTs, n = 33 | 13 | 1 (8) | 12 (92) | 0 | 1 | 50.0 | 100 |
| US showed no stone, LFTs showed cholestasis, n = 86 | 38 | 4 (11) | 34 (89) | 1 | 4 | 37.5 | 96.7 |
| US unclear, LFTs showed cholestasis, n = 61 | 17 | 3 (18) | 14 (82) | 0 | 1 | 75.0 | 100 |
| US not done, no cholestasis on LFTs, n = 6 | 3 | 0 (0) | 3 (100) | 0 | 0 | — | 100 |
| US not done, LFTs showed cholestasis, n = 20 | 12 | 1 (8) | 11 (92) | 0 | 1 | 50.0 | 100 |
| Overall | 117 | 15 | 102 | 2 | 8 | 62.0 | 97.9 |
CBD = common bile duct; LFTs = liver function tests; MRCP = magnetic resonance cholangiopancreatography; US = ultrasonography.
Table 2.
Accuracy of magnetic resonance cholangiopancreatography in gallstone pancreatitis
| Measure | Accuracy, % |
|---|---|
| Sensitivity | 62.0 |
| Specificity | 97.9 |
| Positive likelihood ratio | 6.5 |
| Negative likelihood ratio | 0.1 |
| Positive predictive value | 86.7 |
| Negative predictive value | 92.0 |
The remaining CBD stones were diagnosed by direct ERCP (n = 6), ERCP after ultrasound (n = 65) and by selective IOC (n = 11).
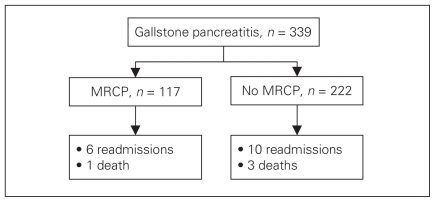
In the patients who received MRCP, there were 6 readmissions and 1 death. In the remaining 222 patients, there were 10 readmissions and 3 deaths (Fig. 1).
Fig. 1.
Readmissions and mortality in patients receiving magnetic resonance cholangiopancreatography (MRCP).
Discussion
In this study of patients with gallstone pancreatitis, we have demonstrated that when MRCP is used selectively in a discriminatory capacity in otherwise clinically equivocal situations, it has a sensitivity of 62% and a specificity of 98% for CBD calculi.
Gallstone pancreatitis is a consequence of distal bile duct obstruction due to migrating gallstones.1 In many cases, this obstruction is transient with the majority of stones passing into the duodenum.16 Previous work has shown that gallstone pancreatitis tends to be caused by small calculi in the distal third of the CBD surrounded by periampullary inflammation.17,18 Whereas smaller size may facilitate spontaneous stone passage,19,20 shown to mostly occur within the first 48 hours,2 it makes radiological assessment of the CBD difficult.21,22 The most common modalities available to assess the CBD include MRCP and ERCP, with the use of endoscopic ultrasound not currently widespread. As noted above, however, ERCPs are no longer favoured as a diagnostic tool owing to their associated risks and variable rates of technical failure.4–6
Magnetic resonance cholangiopancreatography has been adopted in some institutions as a first-line investigation owing to reported sensitivities and specificity ranging up to 95%–100%.7,8,10 Our study reports the sensitivity of MRCP to be 62%, which is in marked contrast to this finding. However, the main point of difference between our study and others published is that, to our knowledge, this is the first study to explore the selective use of MRCP in gallstone pancreatitis. In our institution, MRCP is used only in a discriminatory capacity when the available clinical, biochemical and radiological (ultrasound) evidence is equivocal regarding the presence of choledocholithiasis. A policy of indiscriminate MRCP will lead to some patients with a very high pretest probability of CBD stones receiving MRCPs with predictably positive results. Such patients should be considered for ERCP after ultrasound without undergoing MRCP, especially since the duration of ampullary obstruction is correlated to severity of gallstone pancreatitis and patient morbidity.3,23,24 Similarly, routine MRCP leads to patients who are at low risk for CBD stones also receiving potentially unnecessary scans. Although this mathematically improves the sensitivity and specificity of MRCP, it represents inefficient use of scarce resources with the delay to a therapeutic intervention also increasing patient morbidity.3,13,24
Limitations
Any study investigating the prediction of choledocholithiasis is hampered by the phenomenon of stone passage. Delay to MRCP decreases the diagnostic yield of CBD stones.11 Thus, the accuracy of MRCP may be impaired as it is possible that gallstones either entered the CBD from the gallbladder or, conversely, passed through the ampulla in the interim between admission and scans and also in between confirmatory tests (ERCP/IOC). This would, of course, affect the results of MRCP. However, the turnaround times in our study are comparable to those published at other institutions.8
Another potential limitation of this study is that all patients did not undergo confirmatory ERCP/IOC, therefore we lacked a common denominator in judging the true number of calculi, introducing verification bias. In our institution, IOC is not routinely undertaken. Routine ductal evaluation has been shown to be unnecessary in low-risk patients.25,26 Furthermore, IOC increases operative time and is associated with a 5%–10% cannulation failure rate.27,28 Although an IOC represents an ideal time to detect and then remove CBD stones, prior detection and removal of CBD stones is favoured in our institution. Postoperative ERCP is also sparingly used as it is associated with significant morbidity and causes further delay by necessitating another intervention for the patient.29 Two recent meta-analyses have compared laparoscopic CBD exploration with ERCP and shown it to be at least equal to or better than ERCP.30,31 However, its use is currently restricted to trained enthusiasts and is often prevented by lack of operating equipment or time.32 Our institutional policy is to exonerate the CBD preoperatively. Intraoperative cholangiography is used as per the discretion of the surgeon, and laparoscopic CBD exploration or postoperative ERCP is then used to remove the CBD stones if necessary. Results from this paper are prompting us to reconsider our current policies on the use of IOC in these patients.
Conclusion
Magnetic resonance cholangiopancreatography is a low-risk procedure with a high sensitivity and specificity for choledocholithiasis when used as a first-line investigation in gallstone pancreatitis. However, our study shows that selective MRCP is not sensitive enough to exclude choledocholithiasis, and negative results should be interpreted with caution in this setting.
Footnotes
This study was presented at the Royal Australasian College of Surgeons’ Annual Scientific Congress, May 2009, in Brisbane, Australia.
Competing interests: None declared.
Contributors: Drs. Sammour and Hill designed the study. Drs. Srinivasa, Sammour, McEntee and Davis acquired the data, which Drs. Srinivasa and Sammour analyzed. Drs. Srinivasa and Hill wrote the article, which Drs. Sammour, McEntee, Davis and Hill reviewed. All authors approved publication of the article.
References
- 1.Opie E. The etiology of acute hemorragic pancreatitis. Bull Johns Hopkins Hosp. 1901;12:182–8. [Google Scholar]
- 2.Acosta JM, Ronzano GD, Pellegrini CA. Ampullary obstruction monitoring in acute gallstone pancreatitis: a safe, accurate, and reliable method to detect pancreatic ductal obstruction. Am J Gastroenterol. 2000;95:122–7. doi: 10.1111/j.1572-0241.2000.01671.x. [DOI] [PubMed] [Google Scholar]
- 3.Fan ST, Lai EC, Mok FP, et al. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med. 1993;328:228–32. doi: 10.1056/NEJM199301283280402. [DOI] [PubMed] [Google Scholar]
- 4.Canlas KR, Branch MS. Role of endoscopic retrograde cholangiopancreatography in acute pancreatitis. World J Gastroenterol. 2007;13:6314–20. doi: 10.3748/wjg.v13.i47.6314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang L, Lo S, Stabile BE, et al. Preoperative versus postoperative endoscopic retrograde cholangiopancreatography in mild to moderate gallstone pancreatitis: a prospective randomized trial. Ann Surg. 2000;231:82–7. doi: 10.1097/00000658-200001000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Folsch UR, Nitsche R, Ludtke R, et al. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. The German Study Group on Acute Biliary Pancreatitis. N Engl J Med. 1997;336:237–42. doi: 10.1056/NEJM199701233360401. [DOI] [PubMed] [Google Scholar]
- 7.Makary MA, Duncan MD, Harmon JW, et al. The role of magnetic resonance cholangiography in the management of patients with gallstone pancreatitis. Ann Surg. 2005;241:119–24. doi: 10.1097/01.sla.0000149509.77666.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hallal AH, Amortegui JD, Jeroukhimov IM, et al. Magnetic resonance cholangiopancreatography accurately detects common bile duct stones in resolving gallstone pancreatitis. J Am Coll Surg. 2005;200:869–75. doi: 10.1016/j.jamcollsurg.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 9.Kejriwal R, Liang J, Anderson G, et al. Magnetic resonance imaging of the common bile duct to exclude choledocholithiasis. ANZ J Surg. 2004;74:619–21. doi: 10.1111/j.1445-1433.2004.03114.x. [DOI] [PubMed] [Google Scholar]
- 10.Miletic D, Uravic M, Mazur-Brbac M, et al. Role of magnetic resonance cholangiography in the diagnosis of bile duct lithiasis. World J Surg. 2006;30:1705–12. doi: 10.1007/s00268-005-0459-1. [DOI] [PubMed] [Google Scholar]
- 11.De Waele E, Op de Beeck B, De Waele B, et al. Magnetic resonance cholangiopancreatography in the preoperative assessment of patients with biliary pancreatitis. Pancreatology. 2007;7:347–51. doi: 10.1159/000107269. [DOI] [PubMed] [Google Scholar]
- 12.Moon JH, Cho YD, Cha SW, et al. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005;100:1051–7. doi: 10.1111/j.1572-0241.2005.41057.x. [DOI] [PubMed] [Google Scholar]
- 13.Arguedas MR, Dupont AW, Wilcox CM. Where do ERCP, endoscopic ultrasound, magnetic resonance cholangiopancreatography, and intraoperative cholangiography fit in the management of acute biliary pancreatitis? A decision analysis model. Am J Gastroenterol. 2001;96:2892–9. doi: 10.1111/j.1572-0241.2001.04244.x. [DOI] [PubMed] [Google Scholar]
- 14.Romagnuolo J, Currie G Calgary Advanced Therapeutic Endoscopy Center study group. Noninvasive vs. selective invasive biliary imaging for acute biliary pancreatitis: an economic evaluation by using decision tree analysis. Gastrointest Endosc. 2005;61:86–97. doi: 10.1016/s0016-5107(04)02472-1. [DOI] [PubMed] [Google Scholar]
- 15.Blamey SL, Imrie CW, O’Neill J, et al. Prognostic factors in acute pancreatitis. Gut. 1984;25:1340–6. doi: 10.1136/gut.25.12.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Acosta JM, Ledesma CL. Gallstone migration as a cause of acute pancreatitis. N Engl J Med. 1974;290:484–7. doi: 10.1056/NEJM197402282900904. [DOI] [PubMed] [Google Scholar]
- 17.Jendresen MB, Thorboll JE, Adamsen S, et al. Preoperative routine magnetic resonance cholangiopancreatography before laparoscopic cholecystectomy: a prospective study. Eur J Surg. 2002;168:690–4. doi: 10.1080/11024150201680024. [DOI] [PubMed] [Google Scholar]
- 18.Venneman NG, Buskens E, Besselink MGH, et al. Small gallstones are associated with increased risk of acute pancreatitis: potential benefits of prophylactic cholecystectomy. Am J Gastroenterol. 2005;100:2540–50. doi: 10.1111/j.1572-0241.2005.00317.x. [DOI] [PubMed] [Google Scholar]
- 19.Frossard JL, Hadengue A, Amouyal G, et al. Choledocholithiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc. 2000;51:175–9. doi: 10.1016/s0016-5107(00)70414-7. [DOI] [PubMed] [Google Scholar]
- 20.Taylor TV, Armstrong CP. Migration of gall stones. Br Med J (Clin Res Ed) 1987;294:1320–2. doi: 10.1136/bmj.294.6583.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diehl AK, Holleman DR, Jr, Chapman JB, et al. Gallstone size and risk of pancreatitis. Arch Intern Med. 1997;157:1674–8. [PubMed] [Google Scholar]
- 22.Varghese JC, Liddell RP, Farrell MA, et al. Diagnostic accuracy of magnetic resonance cholangiopancreatography and ultrasound compared with direct cholangiography in the detection of choledocholithiasis. Clin Radiol. 2000;55:25–35. doi: 10.1053/crad.1999.0319. [DOI] [PubMed] [Google Scholar]
- 23.Acosta JM, Rubio Galli OM, Rossi R, et al. Effect of duration of ampullary gallstone obstruction on severity of lesions of acute pancreatitis. J Am Coll Surg. 1997;184:499–505. [PubMed] [Google Scholar]
- 24.Neoptolemos JP, Carr-Locke DL, London NJ, et al. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988;2:979–83. doi: 10.1016/s0140-6736(88)90740-4. [DOI] [PubMed] [Google Scholar]
- 25.Ito K, Ito H, Tavakkolizadeh A, et al. Is ductal evaluation always necessary before or during surgery for biliary pancreatitis. Am J Surg. 2008;195:463–6. doi: 10.1016/j.amjsurg.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 26.Sheen AJ, Asthana S, Al-Mukhtar A, et al. Preoperative determinants of common bile duct stones during laparoscopic cholecystectomy. Int J Clin Pract. 2008;62:1715–9. doi: 10.1111/j.1742-1241.2007.01469.x. [DOI] [PubMed] [Google Scholar]
- 27.Flowers JL, Zucker KA, Graham SM, et al. Laparoscopic cholangiography. Results and indications. Ann Surg. 1992;215:209–16. doi: 10.1097/00000658-199203000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sackier JM, Berci G, Phillips E, et al. The role of cholangiography in laparoscopic cholecystectomy. Arch Surg. 1991;126:1021–5. doi: 10.1001/archsurg.1991.01410320111016. discussion 5–6. [DOI] [PubMed] [Google Scholar]
- 29.Rhodes M, Sussman L, Cohen L, et al. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–61. doi: 10.1016/s0140-6736(97)09175-7. [DOI] [PubMed] [Google Scholar]
- 30.Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2006:CD003327. doi: 10.1002/14651858.CD003327.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Clayton ES, Connor S, Alexakis N, et al. Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ. Br J Surg. 2006;93:1185–91. doi: 10.1002/bjs.5568. [DOI] [PubMed] [Google Scholar]
- 32.Bingener J, Schwesinger WH. Management of common bile duct stones in a rural area of the United States: results of a survey. Surg Endosc. 2006;20:577–9. doi: 10.1007/s00464-005-0322-3. [DOI] [PubMed] [Google Scholar]