INTRODUCTION AND EARLY HISTORY
The classical definition of a hormone is of a chemical messenger which leaves one area of the body by the blood stream and, arriving at another part of the body, causes a change in behaviour there. This broad definition has been refined more recently by considerations of local actions at the site of production and of the influence of other agents (such as growth factors) at the site of action. The human pituitary gland is an ovoid structure, approximately six mm in diameter, and consists of two lobes, anterior and posterior. Its anatomical relationships are of importance (Fig 1). It is found above the sphenoid sinus and immediately below the optic chiasm. It is connected superiorly by a stalk to the hypothalamus. The blood supply is complicated and includes one of the portal systems in the body - the veins from the hypothalamus draining into the pituitary gland. Release of the posterior lobe hormones, oxytocin and vasopressin, is controlled neuronally, but release of the anterior lobe hormones, follicle-stimulating hormone, luteinising hormone, thyroid-stimulating hormone, adrenocorticotrophic hormone, prolactin and growth hormone, is controlled by stimulating and inhibiting hormones from the hypothalamus which are carried to the anterior lobe via the portal venous system. The net effect of any one of the anterior hormones does not simply depend on the stimulation or otherwise of its particular releasing hormone (with negative feedback effect) but is influenced by numerous other factors including higher CNS function. The complex regulation of the growth hormone (GH)/insulin growth factor 1(IGF-1) axis is illustrated by Fig 2. Developments of our knowledge of pituitary pathophysiology and management have only been made possible through the interaction of many disciplines with contributions being made by the various groups listed in Table 1. In recent times the contributions of dedicated laboratory staff, and their ability to give reliable, precisely calibrated hormone levels allow us to practice modern endocrinology. Our endocrine nursing staff are key members of the team and their educational input allows people with pituitary disease to look after their illness better because of their increased knowledge of their own disease.
Fig 1.
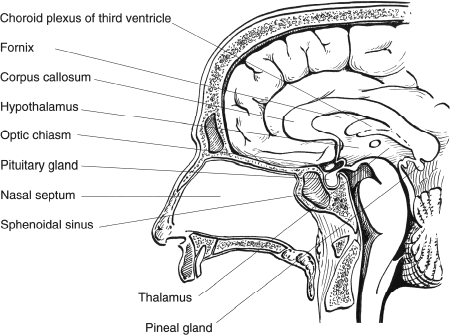
Sagittal section of head showing anatomical relationships of the pituitary gland
Fig 2.
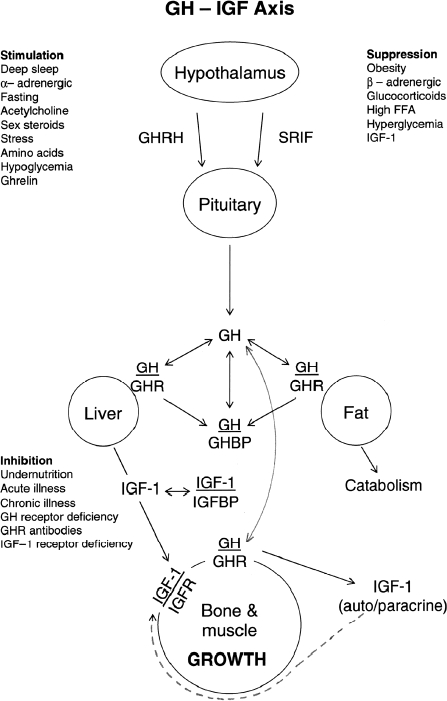
Physiological control of the growth hormone/Insulin growth factor 1 axis
Table 1.
Contributors to the development of pituitary pathophysiology and management
| • Anatomists | • Radiologists |
| • Physiologists | • Geneticists and Molecular Biologists |
| • Descriptive clinicians | |
| • Chemists and Biochemists | • Radiotherapists/Oncologists |
| • Neurosurgeons | • Specialist Endocrine Laboratory Staff |
| • Endocrinologists | • Endocrine Specialist Nurses |
| • Clinical scientists | • Pituitary Patients |
There have been many false ideas and wrong turns during the development of endocrinology although some correct ideas (for example the removal of the ovaries or testes for control of breeding, the use of prolonged lactation to prevent pregnancy) have a long history, dating as far back as the ancient Egyptians and Chinese. Most importantly, Aristotle emphasised the importance of careful examination of the patient. Indeed, he recognised that eunuchs do not become bald and that obesity in females is associated with sterility. He also suggested that the brain is a gland which secretes cold humours to prevent overheating of the body by the fiery heart. His exhortation to careful examination came into its own with the recognition of a variety of endocrine diseases in the 19th century AD. However long before that we can find descriptions of giants in the Bible and it is possible that some had growth hormone producing pituitary tumours. Did Goliath have a classical visual field defect which allowed David to approach close enough to kill him with a stone from a sling? Later, in 2 Samuel 21 we find reference to familial giantism and in 2009 we now recognize a number of syndromes of familial pituitary disease.
Before moving to the history and development of endocrinology from the Middle Ages onward we need to pause and consider a view of Egyptian medicine expressed by Herodotos in the 5th Century BC. He stated “Medicine is practiced among them on a plan of separation: each physician treats a single disease, and not more: thus the country abounds with physicians, some undertaking to cure the diseases of the eyes, others of the head, others again of the teeth others of the intestine…”This is relevant to 21st century medicine where we must take care to use each other's knowledge to cross fertilise specialisms and to remain holistic in our approach to medical practice. General medical societies such as our own Ulster Medical Society can do much to foster this approach.
The middle ages were dark for the development of endocrinology. Galen had suggested that blood flows to and fro in the arteries carrying vital spirit to the various parts of the body. Harvey, to the contrary, recognized that blood circulates. Following on from this the important team of Lower (1631–1691) and Willis (1621–1675) are credited by some for the discovery that substances from the brain move from there through the infundibulum and pituitary stalk to the pituitary and also that the gland itself takes up substances from the blood.
Theophile de Bordeu of Montpelier suggested in 1775 “that each organ of the body gives off emanations - necessary and useful to the whole body. There is no gland which does not draw from the cellular tissue around it a large amount of serosities which co-mingle and inundate the whole region. The pituitary sucks up the superfluous moistures form the brain: they all go to end up in the funnel (stalk) and the pituitary gland receives them and discharges them.” He stated that it remained for physicians to “follow up and classify the various reflexes consequent upon the defective functioning of each particular organ.” Unfortunately, he was not an experimentalist and had no co-worker to perform the necessary experiments and therefore his ideas were not directly developed. His theories were, however, in many respects remarkably similar to those we hold today (Table 2).Will our dangerous neglect of and low priority for research in northern Ireland and particularly in the Belfast HealthTrust lead some of our future hypotheses to be untested and hence neglected for many years?
Table 2.
A comparison of the thoughts of Theophile de Bordeu in 1775 with our concepts of hormones in 2009
| Then |
| Each organ of the body gives off emanations which are necessary and useful to the whole body |
| There is no gland which does not draw from the cellular tissue around it a large amount of serosities which comingle and inundate the whole region |
| Now |
| Chemical messenger leaving one part of the body and via the blood stream delivering a message to another area or areas and causing an action there. |
| Refined in recent years by the knowledge of local actions where they are produced, neuronal interactions, and the influence of aspects such as growth factors etc at the site of action |
Claude Bernard in 1855 formalised what was probably already accepted for other glands, the adrenal in particular. He recognised that the liver had both external and internal secretions (bile and glucose respectively) and he transferred the idea of internal secretions to the “ductless glands” and, for example, began an analysis of extracts of the thyroid and adrenal glands.
Clinical descriptions of endocrinology syndromes began with those related to underactivity of glands (Addison on hypoadrenalism in 1849, Gull on hypothyroidism in 1873 and Hegar on the effects of oophorectomy in 1878). The diagnoses in those days were made when the clinical changes were obvious and therefore advanced, but nowadays we hope to pick up cases much earlier. Most of the early cases of Addison's disease were due to tuberculosis and the condition was invariably fatal as the patients were not able to mount a satisfactory response to infection without their steroid hormones.
At this stage, a role of the pituitary in the production of end organ disease was not suspected but this followed when experiments in animals showed that the thyroid, gonads and adrenals atrophied when the pituitary was removed. These were vital linkage observations and were an important contribution to endocrine knowledge.
HYPERPITUITARISM
The first over-activity syndrome, acromegaly, was recognised in 1885 by Pierre Marie. It is caused by the secretion of excess growth hormone by a pituitary tumour in adult life. The same excess of growth hormone in children, before fusion of the epiphyses, leads to giantism. Cushing recognized that pituitary tumours could be associated with a moon face, central obesity, buffalo hump and stretch marks but his first series of cases of what is now known as Cushing’s syndrome was not published until 1930. He had described one case in 1910 in a paper describing a number of different diseases of the pituitary.
Both acromegaly and Cushing syndrome can cause debilitating physical and psychological disease and are associated with increased mortality. Both initially were untreatable.
Harvey Cushing himself was an extraordinarily tough neurosurgeon who worked relentlessly, wrote continuously and travelled extensively. He made numerous contributions to neurosurgery and did perform pituitary surgery for acromegaly. Curiously he never operated on a case of Cushing syndrome. He described the classical triple concept of pituitary problems: over-production, under-production, and pressure symptoms (and their combinations). In a famous letter he expressed also a hope that one day, as medicines developed, pituitary surgery would no longer be necessary. That day has still not come though we are edging closer to it.
Hyperprolactinaemia was described by Friesen only in 1971 although syndromes of amenorrhoea and galactorrhoea had long been recognised, and there had been experimental evidence in 1915 that the pituitary was involved in milk production. It was the development of an assay for prolactin which revealed the concept of hyperprolactinaemia and showed how common it was. It was not long before bromocriptine was found to be a useful treatment for prolactin excess and today surgery for hyperprolactinaemia is only rarely required.
HYPOPITUITARISM
Treatment of glandular underproduction by extracts of the glands themselves had been tried in antiquity without success. More recently, Brown-Sequard in Paris in 1889 suggested that testicular extracts contain “an active dynamogenic, invigorating substance which could rejuvenate men.” A world-wide response began within months, sometimes with wrong uses and wrong preparations and there was a very mixed medical response in Europe and North America.
George Murray, however, was successful in his treatment of hypothyroidism. He suggested in 1891 in Newcastle that hypothyroidism was due to loss of internal secretion and attempted treatment with sheep thyroid extract. An early patient survived for twenty-eight years with the use of extracts from about thirty-one sheep per year. Not all of his colleagues were initially sympathetic to his idea. One said “It would be just as sensible to treat locomotor ataxia with emulsion of spinal cord.” The proof, however, was seen in the great improvement in the well-being of treated patients.
Further work on extracts of various ductless glands followed and in 1950, Kendall, Reichstein and Hench received the Nobel Prize for their work on the nature and function of hormones secreted by the adrenal glands in mammals. They had carried out very detailed experiments and had isolated and studied 28 different compounds from the adrenal cortex. In doing so they identified and recognised the importance of the steroid ring which is characterised by a double bond next to a ketone group. They had painstakingly carried out small animal experiments on the compounds they had labelled as A, B, E and F before attempting to move to assessment in human subjects. Eventually they showed that compound E helped patients with Addison's disease. Hench had observed also that patients with rheumatoid arthritis often improved in pregnancy and this led to the development of a trial of E (cortisone) in rheumatoid arthritis. It was the success in this field which would lead to the commercial development of cortisone by drug companies; a spin-off from these being that replacement therapy for adrenal insufficiency then became available, rheumatoid disease being much commoner than hypoadrenalism.
Other advances in our understanding of the pituitary gland in the twentieth century included the recognition that its total removal is fatal (1908) and that necrosis of the gland may occur post-partum (1913). Extracts of anterior lobe were shown to increase growth rates in rats (1921) and to produce acromegaly in dogs (1929). Purification of the hormone occurred in the 1930s and 40s and growth hormone was extracted from human cadavers in 1957. This latter experiment led to growth hormone replacement in suitable short stature patients. This was done using extracted growth hormone, synthetic hormone not becoming available until many years later. The synthetic hormone avoids the contamination with viruses and prions sadly reported in some of the cases who had been successfully treated with extracts.
Currently we have many replacement treatments available for insufficiency of the pituitary gland and its dependent glands. Amongst other things this has led to safer surgery for endocrine over-production syndromes. For example both bilateral adrenalectomy for Cushing syndrome and pituitary surgery for acromegaly became possible very soon after cortisone acetate became available and was shown to prevent death from hypoadrenalism.
The pituitary is difficult to locate as it is a small gland sited deep within the head and is surrounded by delicate and important structures such as blood vessels, the optic chiasm and a variety of other important brain structures. Initial surgery to it carried high mortality and morbidity as it was performed via the transfrontal route. Knowing this, Cushing developed a transsphenoidal approach through the nose but the technical requirements of good illumination and magnification were not then available and he gave up that approach and reverted to his previous transfrontal technique which was then used for many years, despite access to the pituitary being difficult and distant. The fact that it was so often successful is a tribute to our neurosurgical colleagues. Now, with modern equipment and modern sub-specialisation, the transsphenoidal approach is associated with very low morbidity and mortality and our RVH, Belfast figures compare well with those in Europe and the USA.
External pituitary irradiation, when properly given, is helpful in controlling tumour re-growth after operation although care has to be taken with the fields and the dose must given in small fractions over a period of six weeks to protect vision. One remaining disadvantage is the possibility of eventual hypopituitarism due to the non-selective nature of the treatment.
Most pituitary tumours are benign and oncological drugs are generally not required as part of their treatment. However some tumours are locally aggressive and in the past have not responded well to any therapy. Very recently, temozolomide, an alkylating agent, has been demonstrated to be useful in some of these very aggressive cases and further research is eagerly awaited.
Some pituitary disease has a genetic basis and at present we know of four familial pituitary tumour syndromes. The genes involved are also known and animal models exist for three of the four (Table 3). Genetic testing is surrounded by the usual difficulties of family tracing and sensitivity to the possibility of early and perhaps unwanted diagnoses being made in other family members. Close liaison with laboratory, geneticists etc. is required and rigorous follow up is required. Hopefully the novel animal models will allow basic research to point us to new methods of treatment for all types of pituitary disease.
Table 3.
Known familial genetic pituitary tumour syndromes
| SYNDROME | GENE | OTHER FEATURES | ANIMAL MODEL |
|---|---|---|---|
| MEN1 | MEN1 11q13 | Hyperparathyroidism Pancreatic tumours Carcinoid syndrome | Yes |
| MEN1-like | CDKN1B 12p13 | HPT | Yes |
| Carney Complex | PRKAR1A 17q23-24 | Atrial myxomas, Adrenal hyperplasia | Yes |
| Familial isolated pituitary adenomas | AIP 11q13.3 | None | No |
Research on the hormones of the hypothalamus has also been very successful. The various hypothalamic releasing and inhibiting hormones were not described until the 1960s and 70s. One point of interest is the fact that many of these hormones are released in pulses - if they are infused continuously their effect is considerably reduced or indeed abolished. Knowledge of the physiology of the hypothalamus and pituitary has led to a variety of drug discoveries. LHRH is used in the treatment of prostate cancer and endometriosis while the combined oral contraceptive pill and hormone replacement therapy are used frequently. New drugs have been developed for use in infertility while dopamine agonist and somatostatin analogues are used for pituitary disease and for various other indications (e.g.parkisonism, gut endocrine tumours).
The effect of native somatostatin lasts for a few minutes only but octreotide, an analogue of it, lasts for about eight hours, and by suitable packaging of that peptide in miniature spheres, can have duration of about one month after an intramuscular injection (Fig 3) These analogues are now widely used in the treatment of growth hormone producing pituitary tumours and can produce a good response including regression of the tumour, in approximately two thirds of patients. There are, in fact, five types of somatostatin receptors present in the pituitary, and octreotide and a similar analogue, lanreotide, predominantly have affinity for ss2. Their effect in acromegaly is good but there is poor responsiveness in Cushing syndrome, where the predominant type is ss5. A new somatostatin analogue, pasireotide, has forty times the affinity of octreotide for the ss5 receptor, and a proof of concept, open-label, single-arm trial has shown good results in Cushing syndrome. Side-effects were common but mild. Further trials are underway and could possibly herald the advent of primary medical therapy for pituitary-dependent Cushing's syndrome.
Fig 3.
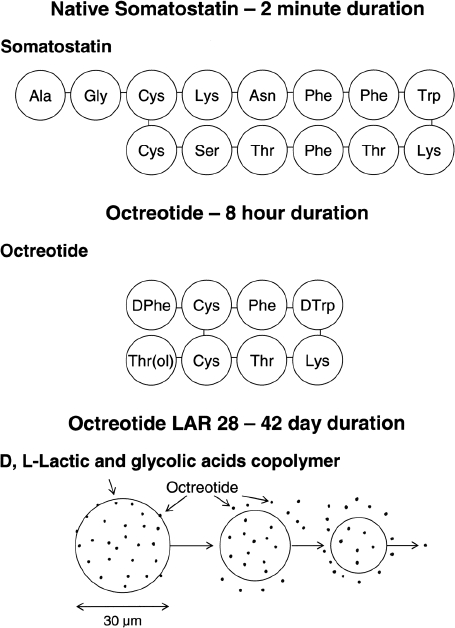
Development of longer acting analogue of native somatostatin and its incorporation by chemists into a preparation which can be given monthly to control GH overproduction
The RVH Regional Endocrinology and Diabetes Centre (Metabolic Unit) has contributed to many of the advances in the treatment of pituitary disease, engaging in its own work and also in many of the international trials (Table 4). This research and the advances in the management of pituitary patients would not have been possible without the skilled assistance of the laboratories, the nursing staff in the unit, surgical and radiological colleagues and many other clinical and research collaborators.
Tables 4a, 4b and 4c.
Some contributions to pituitary research from the Regional Endocrinology and Diabetes Centre, Royal Victoria Hospital, Belfast, 1954–2009
| 4a |
|---|
| Growth Hormone |
| • Visual failure after external pituitary irradiation 1979 |
| • Controlled trial of hGH in adult deficiency 1992 |
| • Some limited efficacy of bromocriptine in acromegaly 1886 |
| • Early dose response studies of octreotide in acromegaly 1990, 1993 |
| • First case series of changing glucose tolerance and of gallstones after octreotide in acromegaly 1989 |
| • Efficacy of octreotide LAR in acromegaly 1999 |
| • Effect of Octreotide LAR on tumour size in acromegaly 2002 |
| • Effect of hGH on insulin resistance in hypopituitarism 2002 |
| • Long term efficacy of XRT in acromegaly 2009 |
| 4b |
|---|
| Cushing's Syndrome |
| • First E uropean series of bilateral adrenalectomy for CS 1954 |
| • Early description of CS secondary to a lung tumour (carcinoid type) 1957 |
| • Invasive pituitary tumor developing after adrenalectomy 1959 |
| • Cyclical CS |
| – 2 rhythms in the same patient 1985 |
| – First ever series of patients 1985 |
| – Importance in assessments after surgery 1992, 1999, 2005 |
| • Petrosal sinus sampling in the diagnosis of ACTH-dependent CS 1989, 1999, 2000 |
| • Assessment of remission of CS after pituitary Surgery 1995, 1996, 2005 |
| • SOM-230(pasireotide) in pituitary-dependent CS 2008 |
| 4c |
|---|
| Other Pituitary Disease Research |
| • Normal puberty and fertility with bromocriptine alone in prolactinoma 1987 |
| • Comparison of cabergoline and bromocriptine in prolactinoma 1984 |
| • Macroprolactinemia as an important cause of hyperprolactinemia 2001 |
| • Assessment of H -P - A axis after pituitary surgery |
| • Metyrapone and naloxone in H-P –A axis assessment 2000 |
| • Low dose vs. regular dose synacthen vs. Insulin hypoglycaemia response 2000 |
| • Early post-operative serum cortisolto predict need for long term steroids after pituitary surgery 2004 |
More exciting discoveries lie ahead and our knowledge of the pituitary gland will continue to increase. The experience of the past suggests that many of todays accepted facts and therapies will be shown to be inadequate or wrong but progress in the management of this group of patients will continue unabated as it has done across the years from then to now.
Acknowledgments
I wish to thank all those who gave me, and maintain my enthusiasm for the science and art of endocrinology. These include my mentors, my consultant colleagues in many disciples including endocrinology, my biochemistry colleagues and all of the excellent junior colleagues who have either worked clinically or researched with me across the years. The nursing staffs of ward 7D and of the old Metabolic Unit of the Royal Victoria Hospital, Belfast have been wonderful colleagues. I thank my secretary Jennifer McDowell for all her help and I dedicate this talk and article to my wife Hilary and my family for all of their outstanding love and support.
SELECTED REFERENCES
- Atkinson AB, Kennedy A, Wiggam MI, McCance DR, Sheridan B. Long-term remission rates after pituitary surgery for Cushing's disease. The need for long-term surveillance. Clin Endocrinol (Oxf) 2005;63(5):549–59. doi: 10.1111/j.1365-2265.2005.02380.x. [DOI] [PubMed] [Google Scholar]
- Bliss M. Harvey Cushing: a life in surgery. Oxford: Oxford University Press; 2005. [Google Scholar]
- Boscaro M, Ludlam WH, Atkinson B, Glusman JE, Petersenn S, Reincke M, Treatment of pituitary-dependent Cushing's disease with the multireceptor ligand somatostatin analog pasireotide (SOM230) A multicenter, phase II trial. J Clin Endocrinol Metabol. 2009;94(1):115–22. doi: 10.1210/jc.2008-1008. [DOI] [PubMed] [Google Scholar]
- Cushing HW. The pituitary body and its disorders. Philadelphia: Lippincott; 1912. [Google Scholar]
- Cushing HW. The basophil adenomas of the pituitary body and their clinical manifestations (pituitary basophilism) Bull Johns Hopkins Hospital Bull. 1932;50:137–95. [Google Scholar]
- De Herder WW. Acromegaly and gigantism in the medical literature. Case descriptions in the era before and the early years after the initial publication of Pierre Marie (1886) Pituitary. 2009;12(3):236–44. doi: 10.1007/s11102-008-0138-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elston MS, McDonald KL, Clifton-Bligh RJ, Robinson BG. Familial pituitary tumor syndromes. Nat Rev Endocrinol. 5(8):453–61. doi: 10.1038/nrendo.2009.126. [DOI] [PubMed] [Google Scholar]
- Hwang P, Guyda H, Friesen H. A radioimmunoassay for human prolactin. Proc Natl Acad Sci U.S.A. 1971;68(8):1902–6. doi: 10.1073/pnas.68.8.1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall EC. Nobel lecture, December 11, 1950. Amsterdam: Elsevier Publishing Company; 1964. The development of cortisone as a therapeutic agent. Available online from: http//:nobelprize.org/nobel_prizes/medicine/laureates/1950/kendall-lecture.pdf. Last accessed March 2010. [Google Scholar]
- Littley MD, Shalet SM, Beardwell CG, Ahmed SR, Applegate G, Sutton ML. Hypopituitarism following external radiotherapy for pituitary tumours in adults. Q J Med. 70(262):145–60. [PubMed] [Google Scholar]
- Medvei VC. The history of clinical endocrinology: a comprehensive account of endocrinology from earliest times to the present day. Carnforth, UK: Parthenon Publishing Group; 1993. [Google Scholar]
- McCormack AM, McDonald KL, Gill AJ, Clark SJ. Low O6-methylguanine-DNA methyltransferase (MGMT) expression and response to temozolomide in aggressive pituitary tumours. Clini Endocrinol. 2009;71(2):226–33. doi: 10.1111/j.1365-2265.2008.03487.x. [DOI] [PubMed] [Google Scholar]
- Kronenberg HM, Melmed S, Polonsky KS, Laarsen PR, editors. William's Textbook of endocrinology. >11th. Philadelphia: Elsevier Saunders; 2008. [Google Scholar]


