Abstract
OBJECTIVE
Compare the immediate affective and cognitive reactions to cancer survivor stories about mammography and breast cancer vs. a didactic, informational approach.
METHODS
Participants (N=489) were African American women age 40 years and older (Mean = 61). Most had ≤ high school education (67%), annual household income ≤ $20,000 (77%), and a prior mammogram (89%). Participants completed surveys before and after watching the narrative or informational video. We used structural equation modeling to examine the large number of inter-related latent constructs.
RESULTS
Women who watched the narrative video experienced more positive and negative emotions, found it easier to understand the video, had more positive evaluations of the video, reported stronger identification with the message source (i.e., perceived similarity, trust, liking), and were more engaged with the video.
CONCLUSIONS
Narratives elicited immediate reactions consistent with theorized pathways of how communication affects behavior. Future studies should examine whether and how these immediate outcomes act as mediators of the longer-term effects of narratives on affect, cognitions, and behavior.
PRACTICE IMPLICATIONS
Stories of other women’s experiences may be more powerful than a didactic presentation when encouraging African American women to get a mammogram.
1. Introduction
Breast cancer accounts for nearly one third of newly diagnosed cancers and is the second leading cause of cancer death among US women (1). Although breast cancer incidence is lower, mortality rates are higher among African American women compared with whites (1). As much as half of this disparity in breast cancer survival can be attributed to inadequate screening or late diagnosis (1–3). Although systematic reviews and meta-analyses have shown that a variety of intervention strategies are effective at increasing mammography use (4–7), we may need new strategies for targeting population sub-groups that bear a disproportionate burden of breast cancer, such as African American women, in order to improve mammography screening rates.
Health communication can influence knowledge and perceptions that change social norms and prompt action, and can model desired behaviors (8). For health communication to have these effects, it is necessary to identify effective messages, influential messengers, and accepted message delivery modes for specific populations. Communication research can help identify these optimal approaches and evaluate whether they work as hypothesized on cognitive and affective behavioral determinants.
Narrative communication may have several advantages over more informational forms of communication. While informational and expository styles of communication present reasons and arguments in favor of a particular course of action, narrative styles use storytelling and testimonials to depict events and consequences for characters (9). Several studies have found that narratives are more persuasive (10–12), whereas others have found that statistical evidence (i.e., averages, percentages) is superior to narrative (13, 14), especially when controlling for the vividness of the evidence (14). However, direct comparisons of narrative and statistical messages are difficult due to differences in their operational definitions across studies and hypothesized pathways of influence; narrative appeals may have a stronger impact on affect, whereas statistical appeals may have a stronger impact on cognitions (14, 15).
The effects of narrative communication may differ by characteristics of the audience (16). For example, the Elaboration Likelihood Model suggests that message involvement or personal relevance determines a person’s motivation to process information and also may moderate the effectiveness of didactic and narrative appeals on persuasion or behavior change (17). Because narratives engage audiences in stories that are not overtly persuasive, narratives reduce individuals’ tendency to thwart a persuasion attempt by avoiding or discounting a message or message source (i.e., selective message avoidance), especially if it is perceived to be untrustworthy or inaccurate (18, 19). Thus, narrative communications may be especially beneficial for subgroups of the population that may have negative perceptions of the message or source.
More theory-based experimental research is needed to understand the effects of narrative health communications (19–21). Some limitations of previous research include 1) the use of undergraduate samples, which are more educated and accustomed to statistical and argument-based evidence compared to the general public, and 2) the use of print-based narratives or fictional scenarios constructed by researchers (e.g., 15, 22, 23). Additionally, because operational definitions and measures for engagement and identification vary in the literature, it is difficult to compare results across studies (18). Engagement with the message often reflects the amount of absorption into the story, whereas identification with the message source denotes perceived similarity and attraction to, and liking by, the message receiver (20, 24, 25). More empirical evidence is needed to determine the unique role of related constructs such as perceived similarity and liking on reactions to narrative communication (18, 21). These outcomes and their inter-relations have not been examined simultaneously in previous studies. Further, scant research has reported the associations between cognitive and affective reactions to narratives (26).
This study examined women’s immediate cognitive and affective reactions to videos about breast cancer and mammography. Our primary aim was to compare women’s reactions to two videos of equivalent content but different delivery sources and styles: multiple personal narratives from African American women breast cancer survivors vs. a didactic, informational presentation by an African American woman narrator. Based on the literature, we hypothesized that the narrative video would influence affect (15) and cognitions (23, 27, 28) including engagement with the message and identification with the message source (18, 20, 24) more than the informational video. To extend previous research, we investigated multiple outcomes simultaneously to better understand the unique relative influences of narratives on inter-related cognitive and affective constructs. Because the construct validity of our measures had not been previously evaluated, our second study aim was to test each measurement model (items and factors) and then build a structural model (associations with and between factors) to assess effects of the video.
In post-hoc analyses, we explored several potential moderators of the effect of the video on women’s reactions (aim 3). We examined potential moderators that could be related to message involvement or population characteristics. Based on the Elaboration Likelihood Model, we hypothesized that the narrative video would elicit stronger responses from women who were less aware of or not previously impacted by breast cancer (i.e., prior mammography use, close others with breast cancer). We also hypothesized that the narrative video would produce more beneficial responses for certain subgroups of women (i.e., lower education, greater medical mistrust and cancer fatalism) at-risk for greater message avoidance (18, 29).
2. Methods
Data were collected as part of a randomized control trial to compare women’s mammography use after watching either a narrative or informational video. This report focuses on the immediate effects of watching the video among all women, whereas differences in subsequent behavior are reported elsewhere (30). Details about the trial including recruitment and participation and intervention development, pre-testing, and content are reported elsewhere in this issue (30) and follow from previous studies (31). Study materials and procedures were approved by the Institutional Review Boards at Saint Louis University and Washington University in St. Louis.
2.1 Participants and Procedures
Between October 2007 and March 2008, participants (N=489) were recruited using neighborhood canvassing approaches in areas of St. Louis, MO where the rate of late stage breast cancer diagnosis was twice the expected rate for the state. Eligibility criteria included being female, African American, aged 40 years and older, never diagnosed with breast cancer, and able to complete a brief literacy screener written at the fifth-grade level. Onboard the Neighborhood Voice, a van customized for data collection in the field (32), participants provided informed consent and were randomly assigned to watch either the narrative or informational video and complete surveys on a 20” touch-screen computer monitor in one of two private interview areas. Survey items completed immediately before (baseline) and after women watched the video comprised the data used in this report.
Most women had a high school education or less (67%), a household income of $20,000 or less (77%), and a prior mammogram (89%). Forty-six percent of women had not had a mammogram in the 12 months prior to the intervention. The average age was 61 years old (SD=12). Intervention groups were equivalent at baseline on demographics, cancer-related beliefs, and behaviors (30).
2.2 Measures
2.2.1 Potential moderator variables
All potential moderators were assessed immediately prior to watching the video. Response options for all items used a 4- or 5-point scale ranging from strongly disagree to strongly agree, unless otherwise noted. Estimates of internal reliability are reported below for multi-item scales for the full sample (N=489) in this study.
Education
Participants were categorized as having less than a high school education (n = 151), a high school degree (n = 175), or more than 12 years of education (n = 162).
Medical mistrust
Five items assessed medical mistrust or perceived discrimination of “people in my ethnic group” (33). Internal reliability was good after removing one reverse coded item, alpha = .73.
Cancer fatalism
Three items assessed cancer fatalism (34). Internal reliability was good, alpha = .72.
Mammography status
Two items assessed whether women had ever had a mammogram and when they had their last mammogram. A dichotomous variable was created to distinguish women who had a mammogram in the 12 months pre-intervention (n = 261) from those who had a mammogram more than 12 months prior or never (n = 226). A similar variable was created to distinguish women based on a 24-month cutoff; 364 completed a mammogram within the 24 months pre-intervention and 123 women had not.
Breast cancer experience
Three separate yes/no items assessed whether women knew anyone who had breast cancer, had a close friend with breast cancer, and had a mother, sister or daughter with breast cancer (31). A dichotomous variable was created to distinguish between women who knew someone with breast cancer (n = 271) and women who knew someone but who was not a close friend or relative or who did not know anyone with breast cancer (n = 217).
2.2.2 Outcome variables
All outcome measures were assessed immediately after women watched the video. Response options for all items used a 4- or 5-point scale ranging from strongly disagree to strongly agree, unless otherwise noted. Items and internal reliability estimates for latent variables included in the final model are reported in Results.
Positive (4 items) and Negative Affect (9 items) in response to watching the video was assessed with adjectives from the PANAS (35). Responses ranged from 1=not at all to 5=extremely.
Cognitive reactions to the video included women’s perceptions that the video was Realistic (3 items; (36)), Lacked Novelty (2 items) and was Difficult to Understand (5 items), as well as their Overall Negative Evaluation (4 items) and General Liking of the video (1-item, “How much did you like or dislike this video?”; 10-point response scale). Three measures were developed based on previous work to assess identification with the message source: Six items assessed perceived Similarity of the character(s) in the video to the participant (37, 38), three items assessed Liking of the message source (“could be a good friend of mine”, “would fit into my circle of friends,” “I like the women in this video a lot”) (39), and seven items assessed Trust in the information and source (40).
Engagement with the message or absorption into the story was assessed with 5 of 15 items from Green and Brock’s (24) Transportation scale using a 7-point response scale (very much – not at all). Imagery items were not included in this study because they did not apply as well to stories presented in video form, and “reading” was changed to “watching” in the wording of some items.
2.3 Data Analysis
We chose a structural equation modeling (SEM) approach because of the number of potential latent variables and the expected high inter-correlations across similar cognitive or affective constructs. SEM has a number of advantages over multiple regression techniques (see Holmbeck (41) for a review). For example, SEM can estimate the inter-relations between variables rather than assume they are independent, and can estimate all associations simultaneously. SEM can include latent error terms to estimate the effects of omitted variables and measurement error. Data were analyzed with AMOS 16.0 (Chicago, IL).
Before examining the immediate effects of the two videos (aim 1), we conducted a series of exploratory measurement and structural model analyses (aim 2) to develop the final structural model used to answer our primary research question. To address aim 2, we attempted to confirm factors determined a priori based on previous research. Then we tested a series of sequential models to determine the final structural model and allowed for improvements and modifications. A low factor loading indicates that a specific item is a poor indicator or measure of the latent construct; items with loadings <.30 were dropped. Because the goal was to maximize the independence and construct validity of each latent variable, significant cross-loading items were also dropped. For our exploratory analyses, we used a random half of the sample and maximum likelihood estimation. To obtain modification indices, we excluded 14 participants who had any missing data (n=230).
Our exploratory approach to the series of confirmatory factor analyses was chosen instead of exploratory factor analysis because of hypothesized measurement models in the literature and because the results would be more consistent with our subsequent confirmatory test of the final structural model (42). Our approach was similar to Bollen’s jigsaw piecewise technique in which pieces of the model are examined prior to the whole model to see if the fit is still adequate as the final model is constructed (43). Because there was no theoretical rationale for the order of adding constructs to the model, we started with the factors with the highest number of items.
We used multiple fit indices to evaluate overall model fit including the comparative fit index (CFI) and Root Mean Square Error of Approximation (RMSEA) and its associated 90% confidence interval. CFI values between 0.90–0.95 or above suggest adequate to good fit (44, 45) and RMSEA values <.06 suggest good model fit (45).
To address aim 1, the final structural model developed with the exploratory sample was confirmed with a second random half of the sample (n=244) using full-information maximum likelihood estimation, and no modifications were allowed (46, 47). The results of the final model are reported for the full sample (N=489).
Using the final structural model to address aim 3, each baseline variable was explored separately as a potential moderator of the effect of the intervention on all outcome variables (48, 49). Moderator analyses were conducted with multiple group comparisons in AMOS to provide a significance test for any differences in path estimates across group, as well as to provide better path estimates than if we conducted separate analyses by group (50). Mean scores were dichotomized at the median and pairs of categorical responses were compared.
3. Results
3.1 Measurement model development with the random-half exploratory sample (n=230)
All estimates are significant (p < .05) and factor loadings >.30 unless otherwise noted.
Affect
The four positive and nine negative affect items were examined as a correlated two-factor model. Fit was not good, χ2(64)=186.29, p < .001; CFI = .81; RMSEA = .091 (.076–.107). One item “watching this video made me feel concerned” was a significant indicator of both factors and was dropped; model fit slightly improved: χ2(53)=151.21, p < .001; CFI=.84; RMSEA = .090 (.073–.107). Two correlated errors were added to the model and fit was acceptable; χ2(51)=90.66, p < .001; CFI = .93; RMSEA = .058 (.038–.078). The factors were not significantly correlated (r = .15, p = .10).
Realism
Two of the three items had factor loadings <.30 that were not statistically significant and were dropped. Both items suffered from severe ceiling effects. The remaining item (“watching this video can’t teach you anything about real life”) was retained for inclusion in the model as a manifest variable.
Difficult to understand
One of the five items was reverse coded and the factor loading was <.30 and not statistically significant. Model fit for the final four-item solution was very similar; χ2(2)=0.78, p = .68; CFI = 1.00; RMSEA < .001 (<.001–.099).
Negative evaluations of the video
The four items loaded on a single factor and fit was acceptable; χ2(2)=6.47, p = .039; CFI = .98; RMSEA = .099 (.019–.189).
We found a significant correlation between negative evaluations and difficult to understand measures; Beta=.81, p<.001. However, fit for a single factor model was substantially lower; therefore, we retained two independent, but correlated factors.
Perceived similarity
One of 8 items was reversed-coded, had a factor loading <.30, and was dropped. The 7-item factor had excellent fit; χ2(14)=17.85, p = .21; CFI = .99; RMSEA = .035 (<.001–.077).
Liking of message source
All items significantly loaded on one factor, but fit could not be estimated because the model was under-identified with only three items (51).
Trust in message source
The original 7 items were all significant indicators of a single factor with modest fit; χ2(14)=44.53, p < .001; CFI = .91; RMSEA = .094 (.063–.127).
Transportation
Two of the five items were reverse coded and were not significant indicators of the construct and were dropped. The final three items had significant factor loadings, but model fit could not be estimated for so few items (51).
To rule out redundancy, exploratory single-factor, correlated two-factor, and second-order factor models were compared when identification and engagement measures were examined together. Results supported the independence of the four constructs.
3.2 Structural model development with the random-half exploratory sample (n=230)
The model with intervention group (0= non-narrative, 1= narrative), positive and negative affect, and similarity fit the data well, χ2(163)=229.28, p < .001; CFI = .93; RMSEA = .042 (.028–.054). When trust was added, one poor indicator of similarity was dropped; χ2(289)=446.27, p < .001; CFI = .89; RMSEA = .049 (.040–.057). When difficult to understand was added, model fit was similar; χ2(390)=594.48, p < .001; CFI = .89; RMSEA = .048 (.040–.055). Negative evaluations of the video was added and modification indices indicated that the reverse-coded negative evaluation item and a negative affect item (bored) significantly loaded on several other latent factors, so the items were dropped; χ2(474)=689.19, p < .001; CFI = .90; RMSEA = .045 (.037–.052). Adding liking of the message source to the model resulted in a non-positive definite matrix. The mean of the two items with more normal distributions was added to the model; χ2(467)=664.05, p < .001; CFI = .91; RMSEA = .043 (.035–.050). Transportation was added along with the three manifest (single item) variables (general liking of the video, novelty, and realism); χ2(638)=941.07, p < .001; CFI = .89; RMSEA = .046 (.039–.052). These three manifest items were not significantly associated with intervention group and were dropped, χ2(559)=839.67, p < .001; CFI = .89; RMSEA = .047 (.040–.053). In the final model, modification indices suggested correlating error terms between negative affect (sad) and transportation (affected me emotionally) items; χ2(558)=826.29, p < .001; CFI = .90; RMSEA = .046 (.039–.052).
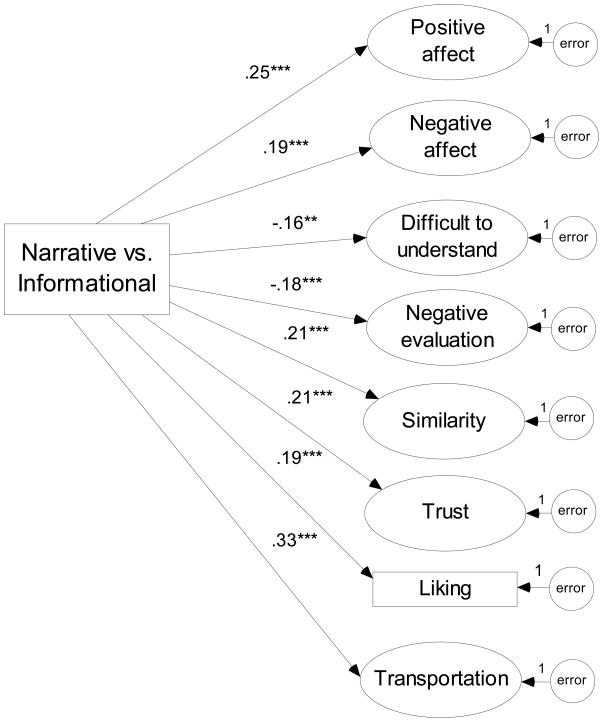
3.3 Structural model validation
The final exploratory model was assessed with the second random half of the sample; χ2(558)=892.23, p < .001; CFI = .87; RMSEA = .050 (.044–.056). Model fit with the confirmatory sample was adequate and no further modifications were made. Standardized estimates for paths in the final confirmatory model with the full sample (N=489) are presented in Figure 1; χ2(558)=1093.70, p < .001; CFI = .90; RMSEA = .044 (.040–.048). All items, factor loadings, and Cronbach’s alpha for each latent factor for the full sample are reported in Table 1 and the significant covariances between factors are reported in Table 2.
Figure 1.
Final structural model of the immediate effects of narrative vs. informational videos with the full sample (N = 489)
** p < .01; *** p < .001
Note. Standardized estimates are shown.
Table 1.
Standardized factor loadings (Beta) and Cronbach’s alpha for latent constructs in the final model with the full sample (N=489)
| Factor | Items | Loading |
|---|---|---|
| Positive affect Alpha = .69 |
Watching this video made me feel hopeful | .51 |
| Watching this video made me feel proud | .66 | |
| Watching this video made me feel inspired | .65 | |
| Watching this video made me feel happy | .61 | |
| Negative affect Alpha = .79 |
Watching this video made me feel worried a | .61 |
| Watching this video made me feel sad a, c | .50 | |
| Watching this video made me feel afraid | .75 | |
| Watching this video made me feel uncertain | .61 | |
| Watching this video made me feel suspicious | .67 | |
| Watching this video made me feel angry b | .45 | |
| Watching this video made me feel frustrated b | .48 | |
| Difficult to understand Alpha = .77 |
The way information was presented in this video was hard for me to understand | .76 |
| This video was difficult to understand | .75 | |
| This video would be easier to understand if I could stop and rewind it to watch parts of it again | .55 | |
| This video had too much information for me to understand | .70 | |
| Negative evaluation Alpha = .74 |
It was hard for me to pay attention for the whole time the video was playing | .68 |
| The video was boring | .74 | |
| This video was too long | .70 | |
| Similarity Alpha = .79 |
The women in this video think like me | .76 |
| The women in this video come from a background like mine | .70 | |
| I could identify with the women in this video | .61 | |
| The women in this video have an education like mine | .57 | |
| The women in this video have values like mine | .54 | |
| The women in this video are a lot like me | .60 | |
| Trust Alpha = .79 |
If I had a question about breast cancer, I would want to talk to the women in this video | .59 |
| I trust the women in this video | .71 | |
| The women in this video are sincere | .56 | |
| I believe the women in this video | .65 | |
| If I had a question about mammograms, I would want to talk to the women in this video | .63 | |
| I trust the information in the video | .52 | |
| I believe the information in this video | .54 | |
| Transportation Alpha = .56 |
This video affected me emotionally c | .53 |
| I was mentally involved in this video while watching it | .44 | |
| I wanted to keep watching the video to find out more | .66 | |
Note: All factor loadings and variances were p < .001
The correlation between error terms was .23, p <.001
The correlation between error terms was .41, p <.001
The correlation between error terms was .22, p <.001
Table 2.
Significant correlations between factors in the final structural model with the full sample (N=489)
| Positive Affect | Negative Affect | Difficult | Negative Evaluation | Similarity | Trust | Liking | Transport | |
|---|---|---|---|---|---|---|---|---|
| Positive Affect | ||||||||
| Negative Affect | .16** | |||||||
| Difficult to Understand | .47*** | |||||||
| Negative Evaluation | −.30*** | .26*** | .81*** | |||||
| Similarity | .41*** | |||||||
| Trust | .50*** | −.12* | −.35*** | .61*** | ||||
| Liking of message source | .32*** | .12* | −.18*** | .64*** | .66*** | |||
| Transportation | .58*** | .42*** | −.33*** | .37*** | .49*** | .43*** | ||
p < .05;
p < .01;
p < .001
3.4 Summary of intervention effects
Women had stronger cognitive and affective responses immediately after watching the narrative video compared with the informational video (Figure 1). Specifically, women who watched the narrative video experienced more positive and negative emotions, found it easier to understand the video, had more positive evaluations of the video, reported stronger identification with the message source (i.e., perceived similarity, trust, liking), and were more engaged (i.e., transportation) with the video. Additionally, measures of engagement and identification with the message source were positively associated with each other and with positive and negative affect, and were inversely associated with negative evaluations of the video (Table 2). Difficulty in understanding, and negative evaluations of, the video were associated with more negative affect.
3.5 Moderator Analyses
Only medical mistrust was a significant moderator of the intervention effect. The narrative video was associated with less difficulty in understanding (β = −.24, p <.001) and fewer negative evaluations (β = −.29, p <.001), but only among women with greater medical mistrust at baseline (n=241). The effect of intervention group on these outcomes was not significant among women with low medical mistrust (n=248).
4. Discussion and Conclusion
4.1 Discussion
This study addressed a need for more theory-based experimental research on the effects of narrative communication (19–21). Our comparison of narrative and informational communication styles was the first to examine multiple inter-related outcomes simultaneously. Findings showed that narratives elicited immediate reactions that are consistent with theorized pathways of how communication interventions affect behavior. Compared to a content-equivalent informational video, the narrative video elicited stronger emotional reactions, which influence attitudes (52) and cognitions about the significance and meaning of an event (53–56). The narrative video was more engaging, which can reduce counterarguing (the generation of arguments against the persuasive message) thereby increasing persuasion (19, 24). Women were also more likely to identify with the cancer survivors, which affects knowledge, message recall, and self-efficacy (26). Narratives also were easier to understand and generated fewer negative evaluations, especially among those with greater medical mistrust. Future studies are needed to further examine whether and how these benefits of narrative communication translate into greater success changing behavioral determinants to promote cancer prevention behaviors and better health outcomes.
Consistent with previous research, the narrative video increased positive and negative affect (15). Additionally, negative affect was positively associated with greater liking of the message source and engagement (transportation). Greater negative affect may not be undesirable and may suggest greater message elaboration and empathy or involvement with the cancer survivors via absorption into the story (19, 24, 26). Future studies will need to determine whether the increase in affective responses to narratives have measureable, beneficial effects on attitudes and behaviors related to mammography use.
A strength of using structural equation modeling was our ability to explore competing measurement models, which supported the inclusion of three separate, but related factors reflecting identification with the message source (perceived similarity, liking, and trust) which also were independent from our measure of engagement (transportation). Our results showed consistent positive effects of narratives on all four constructs. In contrast to the Elaboration Likelihood Model which posits that issue involvement governs information processing, the Extended Elaboration Likelihood Model suggests that message engagement or absorption is more important for evaluating the influence of narrative communications (19). Future studies should examine the distal effects of narratives on cognitive rehearsal, recall, and knowledge via these independent measures of identification and engagement to better understand the potential mediating pathways influencing attitudes and behavior change.
Our post-hoc moderator analyses suggested that the narrative video was especially beneficial for women with higher medical mistrust, who might be resistant to more traditional forms of health and medical information. It is not clear whether this interaction is due to the narrative form of the video, because the messengers were African American breast cancer survivors, or some combination of the two. However, prior communication research among African American adults also found that medical mistrust moderated the effect of cancer news stories on cancer screening intentions (57). Future research should further examine subgroup differences in more heterogeneous samples.
Several study limitations should be considered
Most of the a priori measures produced independent latent constructs with sufficient internal reliability. Even though surveys used plain language and a low reading level, consistently, reverse coded items were not strong indicators of the latent constructs measured in this study. The strong association between “negative evaluations” and “difficult to understand” factors suggests future measurement improvement is needed to better distinguish confusion from aversion. Not everyone in this sample was due for a mammogram, but no differences in the reactions to the videos were observed between women not adherent and adherent to a 12 or 24 month screening interval.
4.2 Conclusions
Narratives had several unique advantages over traditional informational approaches to health communication. They were easier to understand, more engaging, and had a greater emotional impact on viewers. Our findings are consistent with theories and models of how communication affects attitudes and behaviors; however, future studies are needed to examine if and how these immediate outcomes act as mediators of the longer-term effects of narratives on affect, cognitions, and behavior.
4.3 Practice Implications
Clinicians and educators might improve their success with patients and the public by considering how narratives could be integrated into their efforts. It is also clear that women identified more with the breast cancer survivors in the narrative video than with women in the informational video. People who are from the target audience and have personal experience with the health topic of interest may be especially valuable as trusted and credible messengers of health information. Future studies will determine whether the use of narratives is desirable in all cases (58–60).
Acknowledgments
The authors thank Tayo Afuwape, Vicki Amerson, Christine Dao, Kim Dao, Eycine Stewart, Delea Payne for data collection, and the women who contributed to the videos and participated in this study.
Footnotes
Authorship
All authors made substantial contributions to (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, and (3) final approval of the version to be submitted.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Cancer Society. Cancer facts and figures, 2008. Atlanta: American Cancer Society; 2008. [Google Scholar]
- 2.Burns RB, McCarthy EP, Freund KM, Marwill SL, Swartz M, Ash A, Moskowitz MA. Black women receive less mammography even with similar use of primary care. Ann Intern Med. 1996;125:173–82. doi: 10.7326/0003-4819-125-3-199608010-00002. [DOI] [PubMed] [Google Scholar]
- 3.Weiss SE, Tartter PI, Ahmed S, Brower ST, Brusco C, Bossolt K, Amberson JB, Bratton J. Ethnic differences in risk and prognostic factors for breast cancer. Cancer. 1995;76:268–74. doi: 10.1002/1097-0142(19950715)76:2<268::aid-cncr2820760217>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 4.Baron RC, Rimer BK, Breslow RA, Coates RJ, Kerner J, Melillo S, Habarta N, Kalra GP, Chattopadhyay S, Wilson KM, Lee NC, Mullen PD, Coughlin SS, Briss PA Task Force on Community Preventive Services. Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening: A systematic review. Am J Prev Med. 2008;35:S34–S55. doi: 10.1016/j.amepre.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Sabatino SA, Habarta N, Baron RC, Coates RJ, Rimer BK, Kerner J, Coughlin SS, Kalra GP, Chattopadhyay S Task Force on Community Preventive Services. Interventions to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers: Systematic reviews of provider assessment and feedback and provider incentives. Am J Prev Med. 2008;35:S67–S74. doi: 10.1016/j.amepre.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: a meta-analysis review. Prev Med. 2007;45:252–61. doi: 10.1016/j.ypmed.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stone EG, Morton SC, Hulscher MEJL, Maglione MA, Roth EA, Grimshaw JM, Mittman BS, Rubenstein LV, Rubenstein LZ, Shekelle PG. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 8.U. S. Department of Health & Human Services, National Institute of Health, National Cancer Institute. Making health communication programs work. 2004. [Google Scholar]
- 9.Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D, Clark EM, O’Keefe DJ, Erwin DO, Holmes K, Hinyard LJ, Houston T, Wooley S. Narrative communication in cancer prevention and control: A framework to guide research and application. Ann Behav Med. 2007;33:221–35. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- 10.Harte Y. The evidence in persuasive communication. Cent States Speech J. 1976;27:42–6. [Google Scholar]
- 11.Nisbett R, Ross L. Human inference: Strategies and shortcomings of social judgment. Englewood Cliffs: Prentice Hall; 1980. [Google Scholar]
- 12.Sherer M, Rogers RW. The role of vivid information in fear appeals and attitude change. J Res Pers. 1984;18:321–34. [Google Scholar]
- 13.Allen M, Preiss RW. Comparing the persuasiveness of narrative and statistical evidence using meta-analysis. Commun Res Rep. 1997;14:123–31. [Google Scholar]
- 14.Baesler EJ, Burgoon JK. The temporal effects of story and statistical evidence on belief change. Communic Res. 1994;21:582–602. [Google Scholar]
- 15.Kopfman JE, Smith SW, Ah Yun JK, Hodges A. Affective and cognitive reactions to narrative versus statistical evidence organ donation messages. J Apple Commun Res. 1998;26:279–300. [Google Scholar]
- 16.Keller PA, Lehmann DR. Designing effective health communications: A meta-analysis. J Public Policy Mark. 2008;27:117–30. [Google Scholar]
- 17.Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. In: Berkowitz L, editor. Advances in Experimental Social Psychology. New York: Academic Press; 1986. pp. 123–205. [Google Scholar]
- 18.Moyer-Guse E. Toward a theory of entertainment persuasion: Explaining the persuasive effects of entertainment-education messages. Commun Theory. 2008;18:407–25. [Google Scholar]
- 19.Slater MD, Rouner D. Entertainment-education and elaboration likelihood: Understanding the processing of narrative persuasion. Commun Theory. 2002;12:173–91. [Google Scholar]
- 20.Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: A conceptual, theoretical, and empirical overview. Health Educ Behav. 2007;34:777–92. doi: 10.1177/1090198106291963. [DOI] [PubMed] [Google Scholar]
- 21.Petraglia J. Narrative intervention in behavior and public health. J Health Commun. 2007;12:493–505. doi: 10.1080/10810730701441371. [DOI] [PubMed] [Google Scholar]
- 22.Kazoleas DC. A comparison of the persuasive effectiveness of qualitative versus quantitative evidence: A test of explanatory hypotheses. Communication Quarterly. 1993;41:40–50. [Google Scholar]
- 23.Slater MD, Buller DB, Waters E, Archibeque M, LeBlanc M. A test of conversational and testimonial messages versus didactic presentations of nutrition information. J Nutr Educ Behav. 2003;35:255–9. doi: 10.1016/s1499-4046(06)60056-0. [DOI] [PubMed] [Google Scholar]
- 24.Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol. 2000;79:701–21. doi: 10.1037//0022-3514.79.5.701. [DOI] [PubMed] [Google Scholar]
- 25.Lefebvre RC, Tada Y, Hilfiker SW, Baur C. The assessment of user engagement with eHealth content: The eHealth engagement scale. J Comput Mediat Commun. In press. [Google Scholar]
- 26.Dal Cin S, Zanna MP, Fong GT. Narrative persuasion and overcoming resistance. In: Knowles ES, Linn JA, editors. Resistance and Persuasion. Mahwah: Lawrence Erlbaum Associates; 2004. pp. 175–91. [Google Scholar]
- 27.Graesser AC, Olde B, Klettke B. How does the mind construct and represent stories? In: Green MC, Strange JJ, Brock TC, editors. Narrative Impact: Social and Cognitive Foundations. Mahwah: Erlbaum; 2002. pp. 229–62. [Google Scholar]
- 28.Green MC. Narratives and cancer communication. J Commun. 2006;56:S163–83. [Google Scholar]
- 29.Blumberg SJ. Guarding against threatening HIV prevention messages: An information-processing model. Health Educ Behav. 2000;27:780–95. doi: 10.1177/109019810002700611. [DOI] [PubMed] [Google Scholar]
- 30.Kreuter MW, Holmes K, Kalesan B, Alcaraz K, Rath S, Richert M, McQueen A, Caito N, Robinson L, Clark EM. The power of stories: Comparing narrative and non-narrative communication to increase mammography in low-income African American women. Patient Education and Counseling. doi: 10.1016/j.pec.2010.09.008. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kreuter MW, Buskirk TD, Holmes K, Clark EM, Robinson L, Rath S, Erwin D, Philipneri A, Cohen E, Mathews K. What makes cancer survivor stories work? An empirical study among African American women. J Cancer Surviv. 2008;2:33–44. doi: 10.1007/s11764-007-0041-y. [DOI] [PubMed] [Google Scholar]
- 32.Alcaraz KI, Weaver NL, Andresen EM, Christopher K, Kreuter MW. The Neighborhood Voice: Evaluating a mobile research vehicle for recruiting African Americans to participate in cancer control studies. Ethn Health. doi: 10.1177/0163278710395933. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W. The group-based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med. 2004;38:209–18. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 34.Powe BD. Cancer fatalism among African-Americans: a review of the literature. Nurs Outlook. 1996;44:18–21. doi: 10.1016/s0029-6554(96)80020-0. [DOI] [PubMed] [Google Scholar]
- 35.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scale. J Pers Soc Psychol. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 36.Busselle RW. Television exposure, perceived realism, and exemplar accessibility in the social judgment process. Media Psychol. 2001;3:43–67. [Google Scholar]
- 37.Cohen J. Defining identification: A theoretical look at the identification of audiences with media characters. Mass Communication and Society. 2001;4:245–64. [Google Scholar]
- 38.Simons HN, Berkowitz N, Moyer R. Similarity, credibility, and attitude change: A review and a theory. Psychol Bull. 1970;73:1–16. [Google Scholar]
- 39.Roskos-Ewoldsen DR, Fazio RH. The accessibility of source likability as a determinant of persuasion. Pers Soc Psychol Bull. 1992;18:19–25. doi: 10.1037//0022-3514.63.2.198. [DOI] [PubMed] [Google Scholar]
- 40.Wheeless LR, Grotz J. The measurement of trust and its relationship to self-disclosure. Hum Commun Res. 1977;3:250–7. [Google Scholar]
- 41.Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. J Consult Clin Psychol. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- 42.Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- 43.Bollen KA. Modeling strategies: In search of the holy grail. Struct Equ Modeling. 2000;7:74–81. [Google Scholar]
- 44.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 45.Hu L, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling. Thousand Oaks: Sage Publications; 1995. pp. 76–99. [Google Scholar]
- 46.Cudeck R, Browne MW. Cross-validation of covariance structures. Multivariate Behav Res. 1983;18:147–67. doi: 10.1207/s15327906mbr1802_2. [DOI] [PubMed] [Google Scholar]
- 47.MacCallum RC, Roznowski M, Necowitz LB. Model modifications in covariance structure analysis: The problem of capitalization on chance. Psychol Bull. 1992;111:490–504. doi: 10.1037/0033-2909.111.3.490. [DOI] [PubMed] [Google Scholar]
- 48.King AC, Ahn DF, Atienza AA, Kraemer HC. Exploring refinements in targeted behavioral medicine intervention to advance public health. Ann Behav Med. 2008;35:251–60. doi: 10.1007/s12160-008-9032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kraemer HC, Frank E, Kupfer DJ. Moderators of treatment outcomes: Clinical, research, and policy importance. JAMA. 2006;296:1286–9. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- 50.Arbuckle JL. Amos 16.0 User’s Guide. Chicago, IL: 1995–2007. [Google Scholar]
- 51.Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 2005. [Google Scholar]
- 52.Fuegen K, Brehm JW. The intensity of affect and resistance to social influence. In: Knowles ES, Linn JA, editors. Resistance and Persuasion. Mahwah: Lawrence Erlbaum Associates; 2004. pp. 39–64. [Google Scholar]
- 53.Lazarus RS. Comparing theory and research: Past, present, and future. Psychosom Med. 1993;55:234–47. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Aspinwall LG, Taylor SE. A stitch in time: self-regulation and proactive coping. Psychol Bull. 1997;121:417–36. doi: 10.1037/0033-2909.121.3.417. [DOI] [PubMed] [Google Scholar]
- 55.Bagozzi RP, Gopinath M, Nyer PU. The role of emotions in marketing. J Acad Market Sci. 1999;27:184–206. [Google Scholar]
- 56.Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. 2000;55:647–54. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- 57.Nicholson RA, Kreuter MW, Lapka C, Wellborn R, Clark EM, Sanders-Thompson V, Jacobsen HM, Casey C. Unintended effects of emphasizing disparities in cancer communication to African-Americans. Cancer Epidemiol Biomarkers Prev. 2008;17:2946–53. doi: 10.1158/1055-9965.EPI-08-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people’s health care decisions: Is a picture worth a thousand statistics? Med Decis Making. 2005;25:398–405. doi: 10.1177/0272989X05278931. [DOI] [PubMed] [Google Scholar]
- 59.Khangura S, Bennett C, Stacey D, O’Connor AM. Personal stories in publicly available patient decision aids. Patient Educ Couns. 2008;73:456–64. doi: 10.1016/j.pec.2008.07.035. [DOI] [PubMed] [Google Scholar]
- 60.Ubel PA, Jepson C, Baron J. The inclusion of patient testimonials in decision aids: Effects on treatment choices. Med Decis Making. 2001;21:60–8. doi: 10.1177/0272989X0102100108. [DOI] [PubMed] [Google Scholar]