Abstract
Background
Multiple studies have reported echocardiographically determined normal reference values for left ventricular mass (LVM) derived using fundamental imaging (FI). Modern ultrasound systems now use harmonic imaging (HI) due to the improved LV endomyocardial definition. However, the 2005 American Society of Echocardiography (ASE) Recommendations noted that the applicability of the reference values to HI-derived measurements has not been established.
Methods
LV end-diastolic volume, diameter, wall thickness, and mass were determined using HI in healthy subjects (n=251) including a normal weight (NW, body mass index [BMI] < 25 kg/m2, n=149, 68% women) and an otherwise-healthy overweight (OW, BMI ≥25 and <30 kg/m2, n=102, 41% women) groups. Measurements were compared to ASE-endorsed reference values. The agreement between FI and HI was determined in a prospective cohort of 51 subjects.
Results
2D-derived LV volumes were similar between NW and OW subjects; although M-mode (MM)-derived LV diameters were slightly greater in OW. 2D- and MM-derived LVM was greater in OW compared to NW subjects, including after adjustment by height or height2.7; however, indexing to body surface area eliminated these differences. The partition values for abnormal 2D- and MM-derived LVM were generally greater in NW and OW subjects of both sexes compared with the ASE endorsed values (except MM-derived in NW men). However, there were no significant differences in LVM determined by HI compared to FI in a prospectively studied cohort.
Conclusions
Reference values for LVM derived from NW and OW cohorts are generally higher than the ASE-endorsed referenced values. The difference between NW and ASE-endorsed values is unlikely to result from the use of HI rather than FI since there is excellent agreement between these two imaging modalities. This study emphasizes the need to update normal reference values to reflect modern imaging methods.
Keywords: echocardiography, fundamental imaging, harmonic imaging, left ventricular mass, body mass index
Multiple studies have shown that echocardiographically-determined measurements of left ventricular mass (LVM) are predictive of cardiovascular morbidity and mortality. Normal reference values for LV geometry and mass and LVM have been published by several investigators and summarized by the American Society of Echocardiography (ASE); however, these values were derived by use of Fundamental Imaging (FI).1–8 Harmonic imaging (HI) is now routinely used for echocardiography in adults because of superior endomyocardial definition; however, it has been reported to result in smaller LV end-diastolic diameter which may result in greater measurements of LV wall thickness and mass compared to FI.9–12 The use of HI to determine normal values of LV end-diastolic volume, diameter, wall thickness, and LVM in normal weight (NW) and in otherwise-healthy but overweight (OW) individuals has not been well investigated.
Echocardiographic-derived measurements of LV end-diastolic diameter/volumes, wall thickness, and mass are usually adjusted for body habitus to allow reference to normative values. Echocardiographic measurements of LVM are also important for risk stratification in overweight and obese patients, including those without other overt CV risk factors.
The hypothesis of this study was that measurements of LV size, wall thickness, and mass determined by HI differ between NW and OW subjects compared to reported normal reference values. This hypothesis was tested by three aims: First, measurements of LV end-diastolic volume and diameter, wall thickness and mass were determined by HI in two groups of asymptomatic subjects without overt CVD or CVD-associated risk factors: a) NW subjects (body mass index [BMI] <25 kg/m2), and b) overweight (OW) subjects (BMI 25–29.9 kg/m2). Second, to compare these measurements to a reference standard published by the ASE. And third, prospectively assess in a subgroup of ambulatory subjects the agreement of LV end-diastolic volume and diameter, wall thickness and mass obtained by both HI and FI.
METHODS
Study Population
This was a single-center study of consecutive ambulatory subjects (ages 20–80 years) enrolled in an ongoing research study. Eligible subjects had no history, symptoms, physical findings, or echocardiographic evidence of cardiovascular disease. A total of 1,293 subjects were evaluated by review of their medical history, physical examination, and fasting blood chemistries obtained at the time of echocardiography. Systolic and diastolic blood pressures were measured after 15 minutes in the supine position by three consecutive recordings in both arms and averaged. Height and weight were measured using a calibrated stadiometer and scale. NW was defined as BMI <25 kg/m2 and OW as a BMI ≥25 and <30 kg/m2. The study was approved by the Human Research Protection Office at Washington University in Saint Louis; all subjects provided written informed consent.
Exclusion criteria were: 1) BMI ≥30 kg/m2; 2) reported history of prior cardiovascular event (i.e., heart failure, hospitalization for unstable angina or myocardial infarction, prior cardiovascular surgery, or cardiac catheterization demonstrating atherosclerosis); 3) reported history of cerebrovascular disease (e.g., stroke/transient ischemic attack); 4) hypertension (i.e., reported history, current anti-hypertensive drug therapy, or a blood pressure ≥140/90 mmHg at the time of study); 5) diabetes (i.e., reported history or current anti-diabetic drug therapy), 6) a fasting glucose ≥100 mg/dL or insulin level >15 uU/dL; or 7) fasting triglyceride level ≥150 mg/dL. In addition, subjects with echocardiographic evidence of a LV wall motion abnormality, cardiomyopathy, LV ejection fraction <50%, or valvular stenosis and/or valvular regurgitation greater than mild were also excluded.
Echocardiography
All subjects were studied by use of an Acuson Sequoia C256 ultrasound system (Siemens Medical Systems, Mountain View, CA, USA). The echocardiographic examination was performed in all subjects at a harmonic imaging frequency of 2.75 MHz. LV ejection fraction (LVEF) was derived from two-dimensional (2D) measurements of LV volumes (biplane method of discs in the apical 4- and 2-chamber views). LV end-diastolic volume was indexed for body surface area (BSA). 2D-derived LVM was determined by the area-length method and indexed for BSA.
2D-guided M-mode echocardiography was performed in the cross-sectional view. Measurements included end-diastolic LV diameter (Dd), and septal (VS), and posterior wall (PW) thickness by the leading edge method. M-mode-derived LVM was calculated based on the ASE-corrected method and indexed for BSA, height (Ht), and height2.7 (Ht2.7). Relative wall thickness (RWT) was calculated as 2 × PW/Dd. All measurements were made by one observer and represent the average of at least three consecutive cardiac cycles.
A prospective sub-study was conducted in an additional 51 consecutive subjects who underwent 2D and M-mode echocardiography using both harmonic and fundamental imaging. Images were unpaired and randomly evaluated by a single observer in a blinded fashion for measurement of 2D-derived LVM and M-mode-derived LV end-diastolic diameter, septal and posterior wall thickness, and LVM.
Prior studies from our laboratory have determined that the reproducibility for LV mass is excellent with an interclass correlation coefficients of 0.85–0.90.13,14
Statistical Analysis
Continuous variables are expressed as mean ± one standard deviation. Comparisons of echocardiographic variables between groups (i.e., NW vs. OW subjects) were performed using unpaired Student t-test. Reference values for the NW and OW groups shown in Table 3 were determined to be greater than two standard deviations above the mean in each group. In the substudy of 51 subjects, interclass correlation coefficients were used to determine the agreement between measures derived using HI and FI, and Bland-Altman plots were generated to assess for systematic bias. All statistical analyses were performed using SAS (version 9.2, SAS Institute, Cary, North Carolina, USA). Statistical significant was defined as p < 0.05.
Table 3.
Partition values for abnormal left ventricular geometry and mass.*
| Women | Men | |||||
|---|---|---|---|---|---|---|
| ASE Guidelines† | NW | OW | ASE Guidelines† | NW | OW | |
|
2D-derived | ||||||
| EDV (mL) | ≥105 | ≥104 | ≥104 | ≥156 | ≥ 147 | ≥153 |
| EDV/BSA (mL/m2) | ≥76 | ≥62 | ≥57 | ≥ 76 | ≥73 | ≥72 |
| LVM (g) | ≥151 | ≥172 | ≥172 | ≥201 | ≥226 | ≥238 |
| LVM/BSA (g/m2) | ≥89 | ≥100 | ≥94 | ≥103 | ≥115 | ≥114 |
|
M-mode-derived | ||||||
| Dd (cm) | ≥5.4 | ≥5.3 | ≥5.5 | ≥6.1 | ≥5.8 | ≥ 6.1 |
| Dd/BSA (cm/m2) | ≥3.3 | ≥3.3 | ≥3.1 | ≥ 3.1 | ≥3.1 | ≥2.9 |
| LVM (g) | ≥163 | ≥173 | ≥184 | ≥225 | ≥223 | ≥269 |
| LVM/BSA (g/m2) | ≥96 | ≥101 | ≥101 | ≥116 | ≥114 | ≥127 |
| LVM/Ht (g/m) | ≥100 | ≥103 | ≥111 | ≥127 | ≥123 | ≥148 |
| LVM/Ht2.7 (g/m2.7) | ≥45 | ≥44 | ≥48 | ≥49 | ≥47 | ≥55 |
| Relative WT | ≥0.43 | 0.47 | ≥0.49 | ≥0.43 | ≥0.45 | ≥ 0.48 |
Abnormal partition is ≥ mean + 2 standard deviation. Abbreviations as in Table 2.
Schiller NB, et al. J Am Soc Echocardiogr 1989;2:358–67.
RESULTS
Of the 1,293 available study subjects, 251 (144 women, 107 men) qualified for the study based on the inclusion/exclusion criteria. The racial composition of the study group was primarily Caucasian (i.e., 91% of women, 92% of men). A majority of the women were NW (n = 102, 71%); OW women (n = 42, 29%) had higher systolic and diastolic blood pressures than NW women, although the values for both measurements were within normal limits (Table 1). The majority of men were OW (n = 60, 56%) and had higher diastolic blood pressures compared to NW men (n = 47, 44%) although the values were within normal limits. Age, height, and heart rate were similar between NW and OW subjects regardless of gender.
Table 1.
Clinical characteristics of study population
| Women (n=144) | Men (n=107) | |||
|---|---|---|---|---|
| NW (n=102) | OW (n=42) | NW (n=47) | OW (n=60) | |
| Age (years) | 46 ± 14 | 47 ± 12 | 43 ± 16 | 47 ± 13 |
| Height (cm) | 163 ± 6 | 163 ± 6 | 179 ± 7 | 180 ± 7 |
| BSA (m2) | 1.64 ± 0.12 | 1.78 ± 0.11* | 1.92 ± 0.14 | 2.07 ± 0.13* |
| BMI (kg/m2) | 22.2 ± 1.8 | 27.1 ± 1.5* | 22.9 ± 1.7 | 27.4 ± 1.4* |
| Heart rate (bpm) | 63 ± 9 | 66 ± 9 | 61 ± 10 | 63 ± 11 |
| SBP (mmHg) | 109 ± 11 | 112 ± 9‡ | 116 ± 9 | 116 ± 8 |
| DBP (mmHg) | 71 ± 7 | 74 ± 7‡ | 75 ± 6 | 77 ± 6‡ |
BSA, body surface area; BMI, body mass index; DBP, diastolic blood pressure; NW, normal weight; OW, overweight; SBP, systolic blood pressure.
Variables expressed as mean ± SD.
p ≤ .001,
p ≤ .01,
p < .05 vs. NW.
2D and M-mode Echocardiographic Measurements
2D-derived LV end-diastolic volumes (including correction for BSA) and LVEF were similar between NW and OW subjects, regardless of sex. The 2D-derived LVM was significantly greater in OW women and men compared to their respective NW groups; however, this difference was not significant after adjustment for BSA (Table 2).
Table 2.
Two-dimensional and M-mode measurements.*
| Women (n=144) |
Men (n=107) |
|||
|---|---|---|---|---|
| NW (n=102) | OW (n=42) | NW (n=47) | OW (n=60) | |
|
2D | ||||
| EDV (mL) | 76±14 (43–102) | 80±12 (60–109) | 103±22 (70–151) | 107±23 (71–163) |
| EDV/BSA (mL/m2) | 46±8 (29–67) | 45±6 (37–59) | 54±10 (35–76) | 52±10 (35–74) |
| LVM (g) | 125±24 (81–202) | 135±18‡ (99–191) | 164±31 (122–240) | 178±30‡ (127–281) |
| LVM/BSA (g/m2) | 76±12 (52–111) | 76±9 (61–96) | 86±15 (65–118) | 86±14 (56–130) |
| LVEF (%) | 64±6 (53–78) | 64±4 (52–74) | 62±5 (52–72) | 61±6 (51–75) |
|
M-mode | ||||
| Dd (cm) | 4.5±0.4 (3.8–5.6) | 4.7±0.4† (3.9–5.9) | 5.0±0.4 (4.3–5.9) | 5.2±0.5‡ (4.4–6.4) |
| Dd/BSA (cm/m2) | 2.8±0.2 (2.3–3.4) | 2.7±0.2† (2.1–3.2) | 2.6±0.2 (2.3–3.1) | 2.5±0.2† (2.2–3.1) |
| VS (cm) | 0.82±0.09 (0.60–1.10) | 0.86±0.10‡ (0.73–1.20) | 0.92±0.09 (0.70–1.10) | 0.98±0.12† (0.76–1.20) |
| PW (cm) | 0.83±0.10 (0.65–1.30) | 0.88±0.09† (0.7–1.20) | 0.92±0.08 (0.70–1.10) | 0.98±0.10† (0.76–1.16) |
| LVM (g) | 121±27 (75–205) | 138±23* (92–199) | 165±29 (115–237) | 190±39* (123–313) |
| LVM/BSA (g/m2) | 74±14 (48–118) | 78±12 (55–108) | 86±15 (57–118) | 92±18 (61–145) |
| LVM/Ht (g/m) | 74±15 (48–120) | 85±13* (59–117) | 95±15 (64–128) | 106±21* (69–171) |
| LVM/Ht2.7 (g/m2.7) | 32±6 (21–49) | 37±6* (26–51) | 35±6 (25–45) | 39±8* (26–61) |
| Relative WT | 0.37±0.05 (0.27–0.59) | 0.38±0.06 (0.27–0.55) | 0.37±0.04 (0.27–0.45) | 0.38±0.05 (0.28–0.47) |
Variables expressed as mean ± 1 SD and (range);
p ≤ .001,
p ≤ .01,
p ≤ .05 vs. NW.
Abbreviations: BSA, body surface area; Dd, end-diastolic diameter; EDV, end-diastolic volume; Ht, height; LVEF, left ventricular ejection fraction; LVM, left ventricular mass; NW, normal weight; OW, overweight; PW, posterior wall; VS, ventricular septum; WT, wall thickness.
2D-guided M-mode LV end-diastolic diameters (Dd) were greater in OW women and men compared to NW subjects. However, when LV Dd was corrected for BSA, OW women and men had smaller LV end-diastolic diameters compared to NW subjects. LVM, LVM/Ht and LVM/Ht2.7 were greater in OW women and men compared to the respective NW groups, whereas LVM/BSA and RWT were similar between groups.
2D and M-mode Echocardiography Measurements by HI Compared to ASE Reference Values
The measurements of LV geometry and mass derived using HI in both NW and OW subjects were compared to ASE-reported normal reference values (Table 3). The partition values for abnormal measurements were determined as greater than or equal to the mean plus two standard deviations.8,15 The partition values for 2D-derived LV end-diastolic volume were similar in NW and OW women and smaller in NW and OW men compared to the ASE reference values; when indexed by BSA, the resulting values were all smaller than the ASE partition values, regardless of BMI or sex. 2D-derived LVM values, even after adjustment for BSA, were uniformly greater in NW and OW men and women compared with the ASE reference values. The results suggest 2D-derived LVM by HI using the area-length method, may result in high reference values compared to current ASE-reported values.
M-mode-derived measurements of LV end-diastolic diameter by HI, even when adjusted for BSA, were similar to ASE reference values regardless of BMI group or sex. Whereas M-mode-derived LVM in NW men was similar to the ASE partition value, the values in women and OW men were greater than that of the ASE; these relationships persisted if LVM was indexed by BSA or by height. However, indexing LVM to height2.7 (LVM/Ht2.7) resulted in values in NW and OW men and women that were similar to the ASE reference values, except for the value in OW men which was greater. Relative wall thickness was greater in NW and OW in both sexes compared to the ASE values.
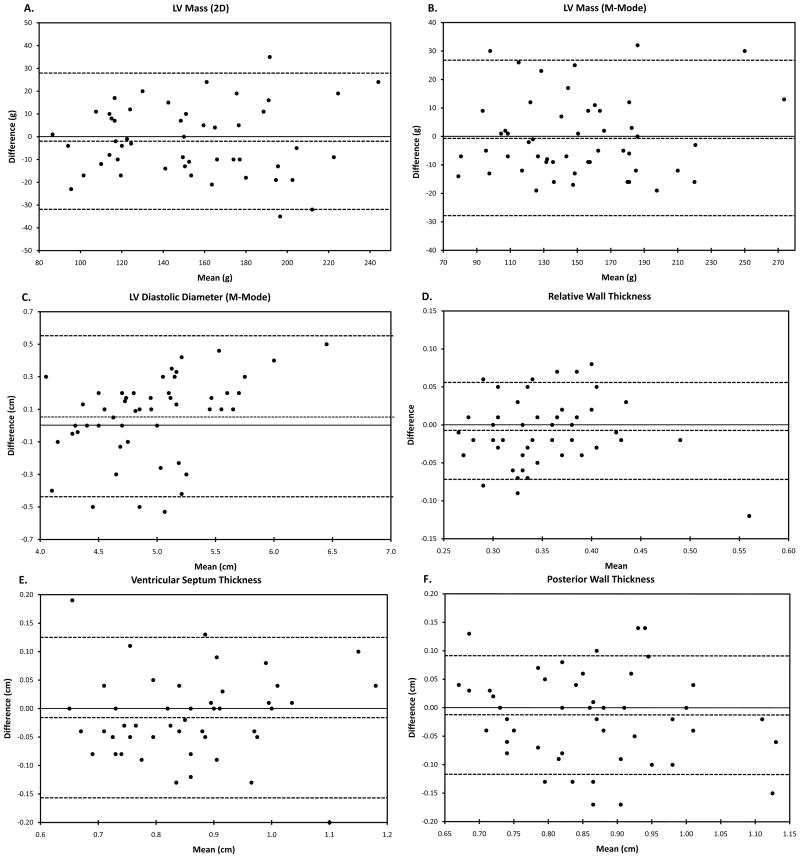
Measurements of LV Geometry and Mass by Harmonic and Fundamental Imaging
We then compared measurements of LV geometry and mass by both FI and HI in a prospective consecutive group of 51 subjects (29 women, age 48 ± 16 years, NW: n=26, OW: n=25). All subjects had normal 2D-determined LV volumes and ejection fraction. There were no differences in LV diameters, wall thickness, or LVM by FI vs. HI (Table 4) and the agreement between measurements of LV geometry and mass between HI and FI were excellent. The Bland-Altman plots demonstrated a bias towards larger M-mode-derived LV diastolic diameters with FI when the LV diastolic diameter was greater than 5.3 cm (Figure, Panel C). There were no other clinically meaningful systematic over- or under-estimation of measurements of LV wall thickness or LVM between HI and FI.
Table 4.
Comparison of harmonic imaging and fundamental imaging measurements (n=51)
| Harmonic | Fundamental Imaging | Imaging ICC (ρ) | |
|---|---|---|---|
|
2D derived | |||
| LVM (g) | 154 ± 39 | 152 ± 39 | 0.96 |
|
M-mode derived | |||
| Dd (cm) | 4.9 ± 0.5 | 5.0 ± 0.6 | 0.94 |
| VS (cm) | 0.87 ± 0.13 | 0.85 ± 0.13 | 0.92 |
| PW (cm) | 0.87 ± 0.13 | 0.85 ± 0.12 | 0.89 |
| LVM (g) | 150 ± 42 | 150 ± 43 | 0.97 |
| Relative WT | 0.36 ± 0.06 | 0.35 ± 0.06 | 0.85 |
Values expressed as mean ± SD.
ICC, intra-class correlation coefficient; LVM, left ventricular mass; Dd, end-diastolic diameter; VS, ventricular septum; PW, posterior wall; WT, wall thickness.
All p values were not significant.
Figure.
Bland-Altman analysis of differences and 95% confidence intervals of subjects evaluated by both fundamental and harmonic imaging of 2D-derived LV mass (panel A), M-mode measurements of LV end-diastolic diameter (panel B), septal thickness (panel C), posterior wall thickness (panel D), M-mode-derived LV mass (panel E), and M-mode-derived relative wall thickness (panel F). Positive values on the y-axis reflect larger values measured with FI.
DISCUSSION
This investigation determined the mean and standard deviation for LV volume, diameter, and mass by 2D and M-mode echocardiography using HI in a carefully phenotyped group of NW and otherwise-healthy OW subjects. The salient results of this study demonstrate several important findings. First, LV volumes by 2D were similar between NW and OW groups although M-mode-derived LV diameters were slightly greater in OW subjects. Second, 2D- and M-mode-derived LVM by HI was greater in otherwise-healthy OW subjects compared to NW subjects, including after adjustment by Ht or Ht2.7; however, indexing to BSA eliminated these differences. The relative wall thickness was also similar between NW and OW subjects. Third, our study determined that the partition values for abnormal 2D and M-mode LVM were generally greater in NW and OW subject of both sexes compared with the ASE endorsed value (except M-mode-derived in NW men). Fourth, in a prospective substudy, there were no significant differences in LVM determined by HI compared to FI.
Normal Values for LV Geometry and Mass by Harmonic Imaging
The present study compared measurements of LV volume, diameter, wall thickness, and mass determined by HI with ASE-reported reference values that were determined using FI.1–8 We compared the partition values for abnormal measurement in our study with that from ASE-recommended values and found the more prominent differences were for 2D- and M-mode-derived LVM. It is noteworthy that in addition to using HI, our study determined 2D LVM using the area-length method whereas the ASE reference values were derived using the truncated ellipsoid equation in FI which may contribute to smaller measurements.6,7
In an effort to better explain these differences, we investigated prospectively whether the use of HI rather than FI resulted in systematic differences in these measures. Prior studies have reported smaller LV end-diastolic diameters but greater LV wall thickness and mass by M-mode when determined by HI compared to FI.10,11,16 In the 51 consecutively studied individuals that were assessed using both HI and FI, the measurements did not differ between imaging modalities and the intraclass correlation coefficients were excellent for all variables tested. We considered that HI, by improving the endomyocardial border detection, resulted in larger measurements of LVM, particularly in an overweight population where FI can be challenging. However, the only evidence of a systematic difference between HI and FI was a slight tendency toward larger LV end-diastolic diameters with FI at diameters greater than 5.3 cm. Since there is no evidence of meaningful differences in the measurements acquired using HI versus FI, imaging modality is unlikely to explain the differences in reference values between this study and the ASE guidelines. More likely is that the use in this study of the area-length rather than truncated ellipsoid formula for determination of 2D-dervied LVM resulted in a systematic difference.
Prior studies have failed to identify many significant differences between HI and FI cohorts of patients evaluated by both methods.11,12,17 However, there are important distinctions between our study and these works. Graham, McGavigan, and Mansencal studied individuals referred for echocardiography for clinical indications; characterization of body habitus and the presence of cardiovascular disease and associated risk factors were not provided for these cohorts. Thus, the subjects in these studies do not represent “normal control” populations as does the NW cohort in our study. Furthermore, unlike the current manuscript where agreement between FI and HI is assessed for 2D-derived LV mass, Mansencal and McGavigan only assessed agreement for M-mode-derived LV mass and Graham only in M-mode derived wall thickness. Finally, the analysis methods used in the current manuscript, namely the intraclass correlation coefficients (to assess agreement between different measurement instruments [e.g., HI vs. FI]) and Bland-Altman plots (to determine the presence of systematic bias) provide a better assessment of agreement than do the methods in the other three manuscripts, which include Student’s t-tests and Pearson’s correlation coefficients (which only tests for random error, not systematic bias).18 Therefore, our study represents data from a more selected control cohort using similar sample sizes as these other works and also includes 2D-derived LV mass, and thus represents novel data.
Limitations
No “gold standard” such as cardiac magnetic resonance imaging was available for comparison to the echocardiographic measurements. The current study was composed predominantly of Caucasian subjects (91%) which may limit the generalizability of findings to other racial groups.
CONCLUSIONS
When using harmonic imaging, 2D- and M-mode-derived LVM is greater in otherwise-healthy OW subjects compared to NW subjects, including after adjustment by height or height2.7; however, indexing to BSA eliminated these differences. The partition values for abnormal 2D and M-mode LVM were generally greater in NW and OW subject of both sexes compared with the ASE endorsed value. The difference between NW and ASE-endorsed values is unlikely to result from the use of HI rather than FI since the agreement between these two imaging modalities was found to be excellent. This study emphasizes the need to update normal reference values to reflect modern imaging methods.
Acknowledgments
This study was supported in part by grants from the National Institutes of Health awards R21HL094668-01, K12RR023249, KL2RR024994, and UL1RR024992 (LdlF), S10RR14778 and R01HL071782 (VGD-R), the Robert Wood Johnson Foundation (LdlF), and the Barnes-Jewish Hospital Foundation to the Cardiovascular Imaging and Clinical Research Core Laboratory.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19:1550. doi: 10.1016/0735-1097(92)90617-v. [DOI] [PubMed] [Google Scholar]
- 2.de Simone G, Devereux RB, Roman MJ, Alderman MH, Laragh JH. Relation of obesity and gender to left ventricular hypertrophy in normotensive and hypertensive adults. Hypertension. 1994;23:600–6. doi: 10.1161/01.hyp.23.5.600. [DOI] [PubMed] [Google Scholar]
- 3.Lauer MS, Anderson KM, Larson MG, Levy D. A new method for indexing left ventricular mass for differences in body size. Am J Cardiol. 1994;74:487–91. doi: 10.1016/0002-9149(94)90909-1. [DOI] [PubMed] [Google Scholar]
- 4.Shub C, Klein AL, Zachariah PK, Bailey KR, Tajik AJ. Determination of left ventricular mass by echocardiography in a normal population: effect of age and sex in addition to body size. Mayo Clin Proc. 1994;69:205–11. doi: 10.1016/s0025-6196(12)61058-1. [DOI] [PubMed] [Google Scholar]
- 5.Ilercil A, O’Grady MJ, Roman MJ, Paranicas M, Lee ET, Welty TK, et al. Reference values for echocardiographic measurements in urban and rural populations of differing ethnicity: the Strong Heart Study. J Am Soc Echocardiogr. 2001;14:601–11. doi: 10.1067/mje.2001.113258. [DOI] [PubMed] [Google Scholar]
- 6.Byrd BF, Wahr D, Want YS, Bouchard A, Schiller NB. Left Ventricular Mass and Volume/Mass Ratio Determined by Two-Dimensional Echocardiography in Normal Adults. J Am Coll Cardiol. 1985;6:1021. doi: 10.1016/s0735-1097(85)80304-1. [DOI] [PubMed] [Google Scholar]
- 7.Park SH, Shub C, Nobrega TP, Bailey KR, Seward JB. Two-dimensional echocardiographic calculation of left ventricular mass as recommended by the American Society of Echocardiography: correlation with autopsy and M-mode echocardiography. J Am Soc Echocardiogr. 1996;9:119–28. doi: 10.1016/s0894-7317(96)90019-x. [DOI] [PubMed] [Google Scholar]
- 8.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Rubin DN, Yazbek N, Garcia MJ, Stewart WJ, Thomas JD. Qualitative and quantitative effects of harmonic echocardiographic imaging on endocardial edge definition and side-lobe artifacts. J Am Soc Echocardiogr. 2000;13:1012–8. doi: 10.1067/mje.2000.108348. [DOI] [PubMed] [Google Scholar]
- 10.Hirata K, Watanabe H, Beppu S, Muro T, Teragaki M, Yoshiyama M, et al. Pitfalls of echocardiographic measurement in tissue harmonic imaging: in vitro and in vivo study. J Am Soc Echocardiogr. 2002;15:1038–44. doi: 10.1067/mje.2002.121537. [DOI] [PubMed] [Google Scholar]
- 11.McGavigan AD, Dunn FG, Goodfield NE. Secondary harmonic imaging overestimates left ventricular mass compared to fundamental echocardiography. Eur J Echocardiogr. 2003;4:178–81. doi: 10.1016/s1525-2167(02)00164-6. [DOI] [PubMed] [Google Scholar]
- 12.Mansencal N, Bordachar P, Chatellier G, Redheuil A, Diebold B, Abergel E. Comparison of accuracy of left ventricular echocardiographic measurements by fundamental imaging versus second harmonic imaging. Am J Cardiol. 2003;91:1037–9. A9. doi: 10.1016/s0002-9149(03)00137-1. [DOI] [PubMed] [Google Scholar]
- 13.Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva-Ware Z, et al. Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation. 2004;109:2191–6. doi: 10.1161/01.CIR.0000127959.28627.F8. [DOI] [PubMed] [Google Scholar]
- 14.de las Fuentes L, Waggoner AD, Mohammed BS, Stein RI, Miller BV, Foster GD, et al. Effect of Moderate Diet-Induced Weight Loss and Weight Regain on Cardiovascular Structure and Function. J Am Coll Cardiol. 2009;54:2376–81. doi: 10.1016/j.jacc.2009.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–67. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 16.Mansencal N, Bouvier E, Joseph T, Farcot JC, Pilliere R, Redheuil A, et al. Value of tissue Doppler imaging to predict left ventricular filling pressure in patients with coronary artery disease. Echocardiography. 2004;21:133–8. doi: 10.1111/j.0742-2822.2004.03045.x. [DOI] [PubMed] [Google Scholar]
- 17.Graham RJ, Gallas W, Gelman JS, Donelan L, Peverill RE. An assessment of tissue harmonic versus fundamental imaging modes for echocardiographic measurements. J Am Soc Echocardiogr. 2001;14:1191–6. doi: 10.1067/mje.2001.113816. [DOI] [PubMed] [Google Scholar]
- 18.Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol. 2003;22:85–93. doi: 10.1002/uog.122. [DOI] [PubMed] [Google Scholar]