Abstract
Background
We evaluated the expression of epithelial-cell-adhesion-molecule (EpCAM) and the potential of MT201 (adecatumumab), a human-monoclonal-antibody targeting EpCAM against chemotherapy resistant ovarian disease.
Methods
EpCAM expression was evaluated by real-time-PCR and flow cytometry. Sensitivity to MT201-dependent-cellular-cytotoxicity (ADCC) and complement-dependent-cytotoxicity (CDC) was tested in 4-hour 51Cr-release-assays. The effect of interleukin-2 (IL-2) on MT201-mediated ADCC was also studied.
Results
High mRNA expression by real-time-PCR and high EpCAM surface expression by flow-cytometry was detected in 71% of ovarian cancers (five out of seven cell lines). While these cell lines were highly resistant to CDC and natural killer-dependent-cytotoxicity in vitro (range of killing 0%–7%), EpCAM-positive cell lines showed high sensitivity to MT201-mediated ADCC (range of killing 27%–66%). Incubation with IL-2 further increased the cytotoxic activity against EpCAM-positive ovarian cancer cell lines.
Conclusions
MT201 may represent a novel, potentially highly effective treatment option for ovarian carcinoma patients harbouring disease refractory to chemotherapy.
Keywords: ovarian cancer, EpCAM, MT201, adecatumumab, monoclonal antibody, chemotherapy resistance, cytotoxicity, natural killer cells
Introduction
Ovarian cancer is the gynepcologic malignancy with the highest mortality, with 21,550 new cases and 14,600 deaths estimated for 20091. Most ovarian cancers are diagnosed in advanced stages. Despite aggressive surgical treatment and chemotherapy, the 5-year survival rate of patients with advanced stage disease is 30%2. While most patients respond to the initial chemotherapy, they ultimately become resistant to the treatment3. Thus, there is great interest in the development of targeted agents active against chemotherapy-resistant ovarian disease3.
Epithelial cell adhesion molecule (EpCAM), also referred to as EGP-40, Trop-1, 17-1A, KSA, KS1/4, AUA1, GA733-2, CD326, has been shown to be overexpressed in ovarian cancer4. EpCAM is a 40 kd surface glycoprotein that was first discovered in 19795. The EpCAM gene is located on chromosome 4q and contains nine exons. It consists of an extracellular domain with two EGF-like repeats, a transmembrane as well as a short cytoplasmic domain5. EpCAM is expressed at low levels on the basolateral and intercellular surface of simple, pseudo-stratified and transitional epithelia, including most epithelial tissues in the female genital tract6. The homogenous distribution of EpCAM on the tumor cell, its glycosylation and the level of expression help differentiate tumor from normal cells7. Indeed, most neoplastic epithelial cells overexpress EpCAM5, as do 85% of adenocarcinomas and 72% of squamous cell carcinomas8. EpCAM is believed to contribute to signaling, cell migration, proliferation and differentiation9. It promotes cell adhesion via a calcium-independent mechanism5, and formation of EpCAM-mediated adhesions have a negative regulatory effect on adhesions mediated by cadherins10. Consistent with this view, EpCAM silencing with siRNA may lead to a reduction in proliferation, migration and invasion11.
Importantly, because of its localization on the cell surface of carcinomas, EpCAM is an attractive target for immunotherapy5. Edrecolomab (Panorex®), a chimeric murine anti-EpCAM IgG2a antibody, was shown to improve overall and disease-free survival in Dukes C colon cancer patients with minimal residual disease12. It subsequently gained approval in Germany as an adjuvant monotherapy in the treatment of colon carcinoma and was taken off the market only after the introduction of 5-fluorouracil with leucovorin in colon carcinoma lead to even better survival results.
Adecatumumab (MT201) is a fully human, recombinant monoclonal anti-EpCAM antibody13 that acts mainly through antibody-dependent cellular cytotoxicity (ADCC)8. Compared to the murine antibody edrecolomab, MT201 shows a longer half-life and reduced immunogenicity5. Unlike the previous murine high-affinity anti-EpCAM antibodies, adecatumumab is a low to intermediate affinity antibody13. The high-affinity antibodies were associated with significant toxicities in Phase I clinical trials13. Adecatumumab, however, appears to be well tolerated, has been tested in phase II trials in metastatic breast and early-stage prostate cancer 14,15, and is currently being evaluated in a phase IB trial in combination with docetaxel16 and another phase II study in patients undergoing liver resection for colorectal cancer metastases.
In this investigation, we evaluated EpCAM’s potential value as a novel target against ovarian cancer by studying its expression at both mRNA and protein level in multiple biologically aggressive ovarian cancer cell lines established from patients harboring chemotherapy-resistant disease.
Material and Methods
Establishment of ovarian cancer cell lines
Study approval was obtained from the Institutional Review Board, and all patients signed an informed consent form according to institutional guidelines. A total of seven ovarian cancer cell lines were established after sterile processing of samples from surgical biopsies as previously described17. Patient characteristics regarding the tumor cell line of origin are described in table 1. All patients received a combination of carboplatin and paclitaxel as primary chemotherapy regimen. Six of the seven patients whose cells were used for the establishment of cell lines demonstrated disease progression on chemotherapy. All seven primary ovarian cancer cell lines were found highly resistant in vitro to multiple chemotherapy drugs including carboplatin, cisplatin, paclitaxel, doxorubicin, ifofosfamide, gemcitabine and topotecan by Extreme Drug Resistant (EDR) assays (Oncotech, Irvine, CA).
Table 1.
Patient characteristics
| Cell line | Histology | Age (years) | Race | Stage | Grade |
|---|---|---|---|---|---|
| OSPC-ARK-1 | OSPC | 68 | ** C | IV | G3 |
| OSPC-ARK-2 | OSPC | 64 | C | IIIC | G3 |
| OSPC-ARK-3 | OSPC | 53 | C | IIIA | G3 |
| OSPC-ARK-4 | OSPC | 33 | C | IV | G3 |
| OSPC-ARK-5 | OSPC | 55 | C | IV | G3 |
| CC-ARK-1 | CC | 42 | C | IIIC | G3 |
| * CC-ARK-2 | CC | 32 | C | IC | G3 |
With the exception of CC-ARK-2, all tumor biopsies from which ovarian cancer cell lines were established were collected from specimens at the time of tumor recurrence after multiple chemotherapy regimens. Primary ovarian cancer cell lines were not selected against chemotherapy drugs in vitro.
C: Caucasian.
Quantitative real-time polymerase chain reaction
RNA isolation from a total of 7 primary ovarian carcinoma cell lines was performed using TRIzol Reagent (Invitrogen) according to the manufacturer’s instructions. Quantitative PCR was done with a 7500 Real Time PCR System using the manufacturer’s recommended protocol (Applied Biosystems, Foster City, CA) to evaluate expression of EpCAM in all samples. The primers and probe for EpCAM (TACSTD1) were obtained from Applied Biosystems (Hs00158980_m1). The comparative threshold cycle (CT) method (Applied Biosystems) was used to determine gene expression in each sample relative to the value observed in the lowest nonmalignant ovarian epithelial cell sample, using glyceraldehyde-3-phosphate dehydrogenase (Assay ID Hs99999905_m1) RNA as internal controls.
Flow cytometry
The humanized anti-EpCAM mAb MT201 (Micromet, Munich, Germany) was used for flow cytometry studies. The chimeric anti-CD20 mAb rituximab (Rituxan, Genentech, San Francisco, CA, USA) was used as antibody isotype control for MT201. A goat anti-human F(ab’)2 immunoglobulin (BioSource International, Camarillo, CA, USA) was used as a secondary reagent. Analysis was conducted with a FACScalibur, using Cell Quest software (Beckton Dickinson, Franklin Lakes, NJ, USA).
ADCC measurements
A standard 4h chromium (51Cr) release assay was performed to measure the cytotoxic reactivity of Ficoll-Hypaque separated peripheral blood lymphocytes (PBL) obtained from several healthy donors against all seven ovarian cancer cell lines. In the majority of the experiments the release of 51Cr from the target cells was measured as evidence of tumor cell lysis after exposure of tumor cells to a concentration 5 μg/ml of MT201. Controls included the incubation of target cells alone or with PBL or mAb separately. The chimeric IgG1 anti-CD20 mAb rituximab (Rituxan, Genentech, San Francisco, CA, USA) was used as antibody isotype control for MT201 in all bioassays.
Interleukin-2 enhancement of ADCC
To investigate the effect of interleukin-2 (IL-2) on MT201-mediated ADCC, effector PBLs were incubated for four hours at 37°C at a final concentration of IL-2 (Aldesleukin; Chiron Therapeutics, Emeryville, CA) ranging from 50–100 IU/ml in 96-well microtiter plates. Target cells were primary ovarian cell lines exposed to MT201 (concentration 5 μg/ml), whereas controls included the incubation of target cells alone or with PBLs in the presence or absence of IL-2 or mAb, respectively. Rituximab was used as an isotype control mAb.
Test for complement-mediated target cell lysis and for inhibition by γ-immunoglobulin
A standard 4h chromium (51Cr) release assay identical to those used for ADCC assays was used, except that human serum in a dilution of 1:2 was added in place of the effector cells. This human serum was used as a source of complement to test for complement-mediated target cell lysis. To test for the possible inhibition of ADCC against ovarian cancer cell lines by physiological human serum concentrations of γ-immunoglobulin, heat inactivated (56°C for 60 minutes) human serum was diluted 1:2 before being added in the presence or absence of effector PBL. In some experiments, non-heat-inactivated human serum (diluted 1:2) was added in the presence of effector PBL. Controls included the incubation of target cells alone or with either lymphocytes or mAb separately. Rituximab was used as isotype control mAb.
Statistical analysis
q-rtPCR data were evaluated via unequal-variance t-test for ovarian carcinoma-versus-NOVA-difference. Differences in EpCAM expression by flow cytometry were analyzed by the unpaired t-test, and a p-value of < 0.05 among samples was considered to be significant. Kruskal-Wallis test and chi-square analysis was used to evaluate differences in MT201-induced ADCC levels in primary tumor cell lines. Statistical analysis was performed using SPSS version 15 (SPSS, Chicago, IL, USA).
Results
EpCAM transcript levels in ovarian carcinomas
A total of seven primary ovarian cancer cell lines were tested for EpCAM expression by q-rtPCR. Table 1 shows the histopathological characteristics of the ovarian cancer patients. Of the seven tumors tested, five carcinomas (three of five OSPCs, two of two clear cell carcinomas) showed a high mRNA copy number, ranging from 2059 to 6100 (Table 2). In contrast, low EpCAM expression by q-rtPCR was detected in two OSPC cell lines, ranging from 44 to 108 mRNA copy numbers (Table 2). The difference between ovarian cancer cell lines with low and high EpCAM expression was statistically significant (p=0.009).
Table 2.
EpCAM mRNA and protein expression in ovarian cancer cell lines
| Cell line | Flow cytometry | q-rtPCR | |
|---|---|---|---|
| MFI* + SD | Cells (%) + SD | mRNA copy # | |
| OSPC-ARK-1 | 224.65 ± 47.95 | 92.30 ± 12.52 | 3264.798 |
| OSPC-ARK-2 | 293.63 ± 187.87 | 96.48 ± 6.86 | 2255.615 |
| OSPC-ARK-3 | 45.22 ± 20.71 | 12.45 ± 7.61 | 44.495 |
| OSPC-ARK-4 | 244.52 ± 187.19 | 90.24 ± 11.50 | 2058.884 |
| OSPC-ARK-5 | 25.22 ± 13.44 | 15.35 ± 8.79 | 108.336 |
| CC-ARK-1 | 362.79 ± 26.52 | 92.23 ± 13.41 | 3607.205 |
| CC-ARK-2 | 582.34 ± 76.58 | 92.79 ± 12.36 | 6100.327 |
MFI: Mean Fluorescence Intensity
EpCAM surface expression by flow cytometry in ovarian carcinomas
To determine whether the high expression of EpCAM mRNA detected by q-rtPCR assays in five out of seven of our primary ovarian cancer cell lines also resulted in high expression of the protein on the surface of tumor cells, we performed flow cytometry on all primary tumors. Five cell lines showed once again high EpCAM surface expression by flow cytometry (three of five OSPCs and two of two clear cell carcinomas) (Table 2). This data is consistent with the mRNA copy number measured by q-rtPCR. The difference in EpCAM surface expression between the cell lines with low and high EpCAM expression was statistically significant (p<0.001).
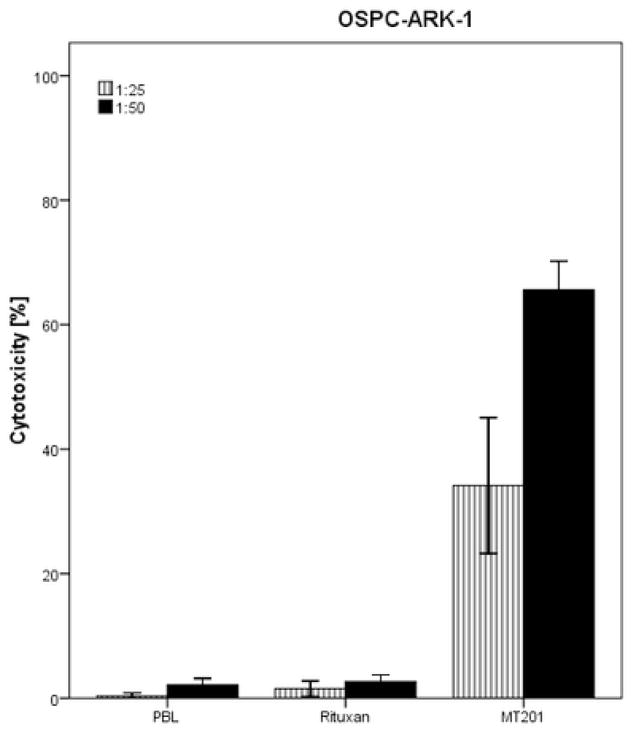
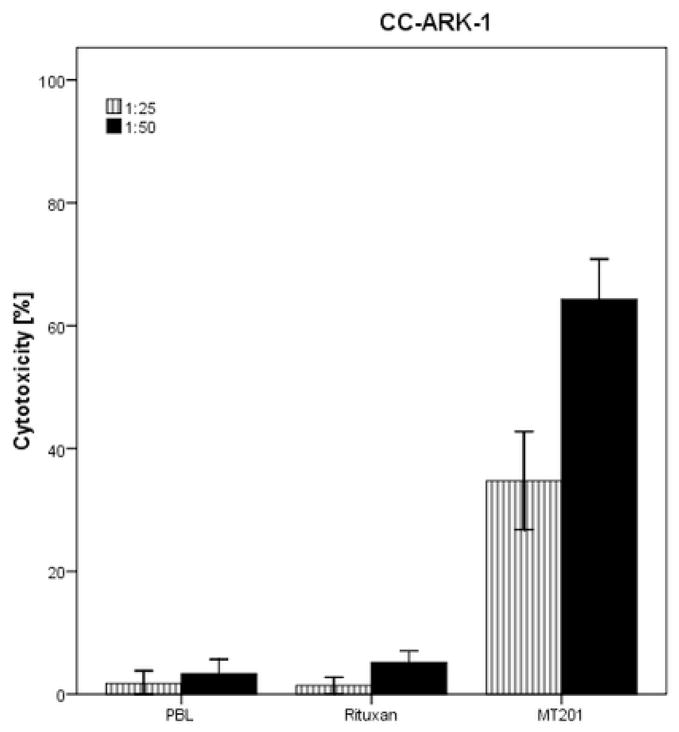
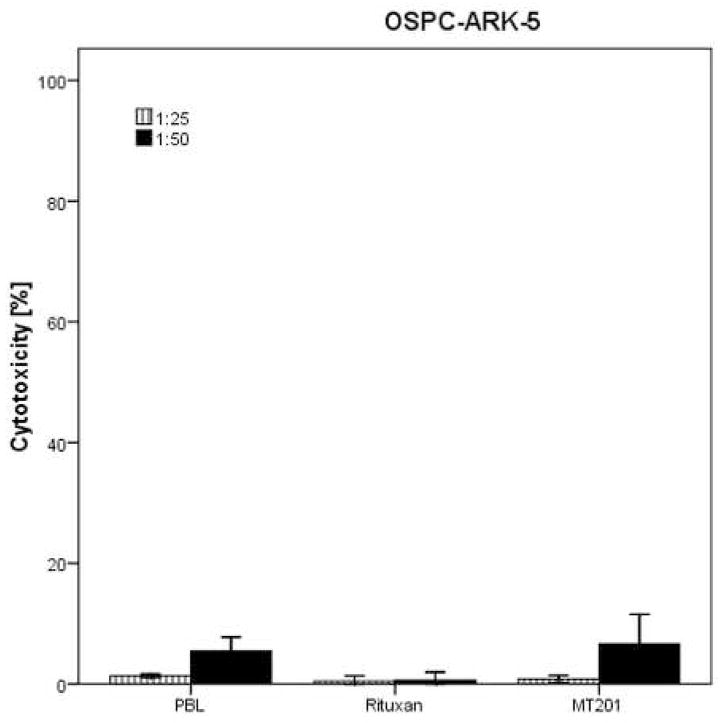
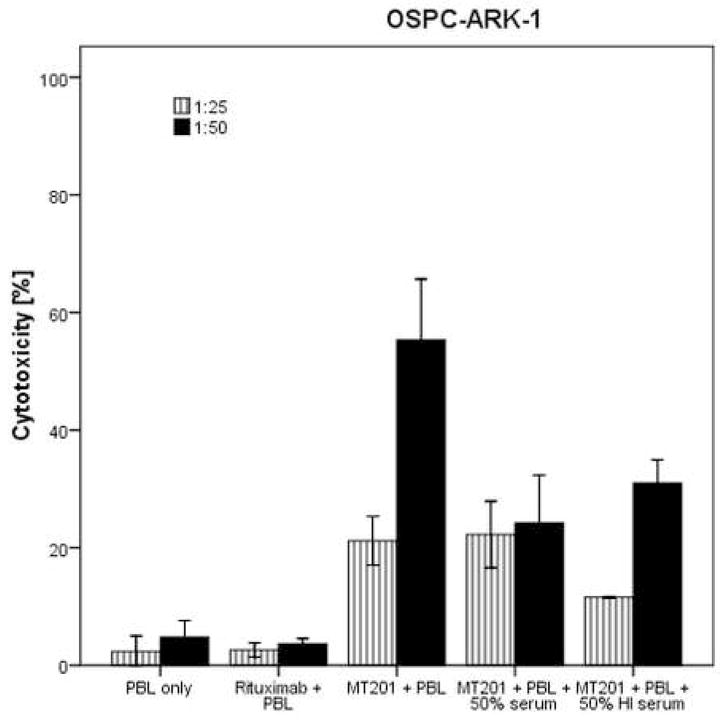
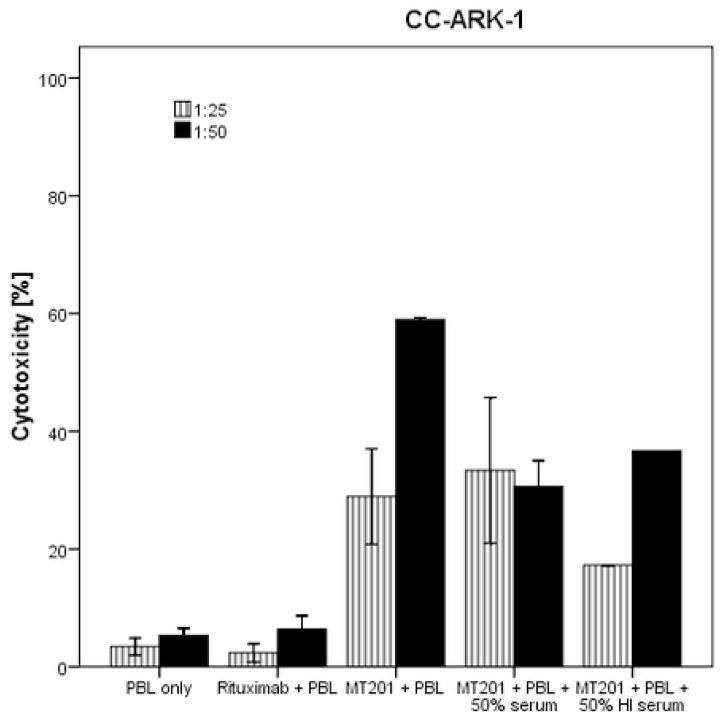
Ovarian carcinoma cell lines are highly resistant to NK cell activity but sensitive to MT201-mediated ADCC
All seven primary ovarian cancer cell lines were evaluated for their sensitivity to natural killer cells (NK). These cell lines were exposed to PBL collected from multiple healthy donors in cytotoxicity assays. Using dose titration experiments with different doses of MT201, killing of the ovarian cancer cells was found to plateau at an MT201 concentration of μ5 g/ml (data not shown). This dose was therefore used in all following experiments. Ovarian cancer cell lines were found highly resistant to NK cell-mediated killing with exposure to PBL at an effector : target ratio (E/T) of 25:1 and 50:1 (mean killing ± SD = 3.7% ± 2.6%) (Table 3). In contrast, significant killing was demonstrated against EpCAM-positive cell lines after incubation with MT201 to mediate ADCC (range of killing 40–62%, mean killing ± SD 41% ± 14%) (Figure 1, Table 3). As expected, EpCAM-negative cell lines were resistant to MT201 (Figure 1). These experiments were repeated a minimum of two times per ovarian cancer cell line. The results are consistent with the EpCAM expression data by q-rtPCR and flow cytometry (Table 2). All cell lines were highly resistant to incubation with rituximab isotype control antibody in the presence of PBL (Table 3 and Figure 1).
Table 3.
MT201-dependent cytotoxicity results in ovarian cancer cell lines
| Cell line | Control ± SD | Rituximab ± SD | MT201 ± SD | p-value* |
|---|---|---|---|---|
| OSPC-ARK-1 | 2.5% ± 1.5 | 2.4% ± 1.4 | 61.8% ± 18.7 | |
| OSPC-ARK-2 | 7.4% ± 6.5 | 6.2% ± 4.4 | 60.8% ± 9.2 | |
| OSPC-ARK-3 | 3.7% ± 3.6 | 3.3% ± 2.9 | 4.6% ± 6.5 | |
| OSPC-ARK-4 | 1.6% ± 1.4 | 1.9% ± 0.6 | 47.0% ± 24.1 | |
| OSPC-ARK-5 | 5.5% ± 1.6 | 0.7% ± 0.9 | 6.7% ± 3.5 | |
| CC-ARK-1 | 2.4% ± 1.4 | 4.0% ± 2.5 | 54.8% ± 17.2 | |
| CC-ARK-2 | 2.7% ± 2.0 | 1.6% ± 1.4 | 50.6% ± 21.8 | |
| Average** | 3.7% ± 2.6 | 2.9% ± 2.0 | 40.9 ± 14.4 | <0.0001 |
Cytotoxicity results in EpCAM-positive cell lines versus controls by Kruskal-Wallis test.
Average of 36 cytotoxicity experiments.
Figure 1.
Representative cytotoxicity experiments using MT201 against OSPC-ARK-1 (upper panel), CC-ARK-1 (middle panel) and OSPC-ARK-5 (lower panel) cell lines. High levels of ADCC MT201 induced cytotoxicity were evident against OSPC-ARK-1 and CC-ARK-1 primary cell lines expressing high levels of EpCAM. In contrast, negligible cytotoxicity was detectable against OSPC-ARK-5 (i.e., a low EpCAM expressor cell line). In all cell lines tested, no significant cytotoxicity was detected in the absence of MT201 or in the presence of rituximab control mAB.
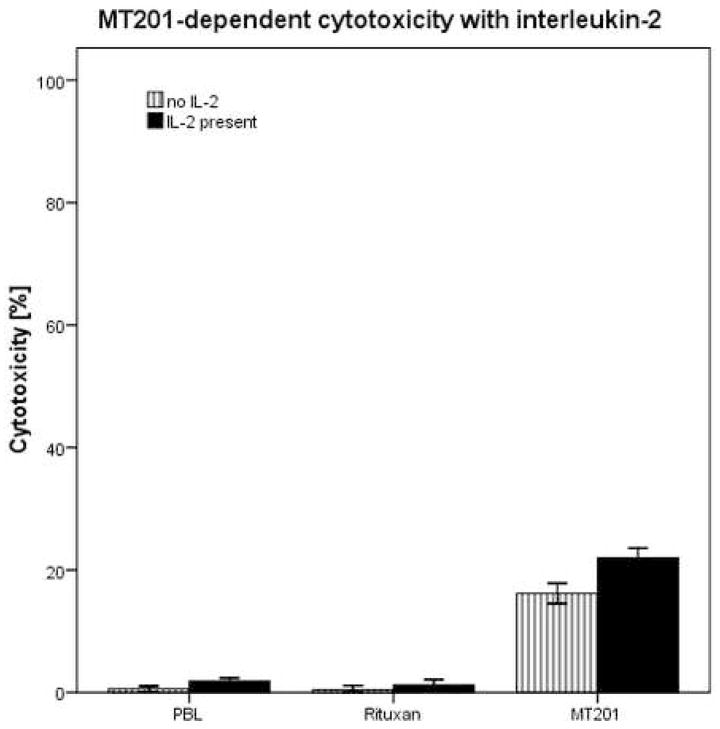
IL-2 enhancement of ADCC against ovarian carcinoma
To investigate the effect of interleukin-2 (IL-2) in combination with MT201 (5 μg/ml) on ADCC against ovarian carcinoma cell lines, PBL from healthy donors were incubated with 50–100 IU/ml of IL-2 for 4 hours. As representatively shown in Figure 2, MT201-mediated ADCC was significantly increased in the presence of IL-2 in all primary cell lines tested (p<0.0001). While the stimulation of PBL with IL-2 leads to a significantly higher ADCC in the presence of MT201, it did not significantly increase tumor killing in the absence of MT201 or in the presence of rituximab isotype control antibody and PBL (Figure 2).
Figure 2.
Representative effect of low doses of interleukin-2 (IL-2) in combination with MT201 (5 μg/ml) on ADCC against OSPC-ARK-1 primary cell line (Effectors to target ratio 25:1). PBL from healthy donors were incubated for 4 hours in the presence of 100 IU/ml of IL-2. MT201-mediated ADCC was significantly increased in the presence of low doses of IL-2. No significant increase in cytotoxicity was detected after 4-h IL-2 treatment in the absence of MT201 or in the presence of the rituximab isotype control mAb.
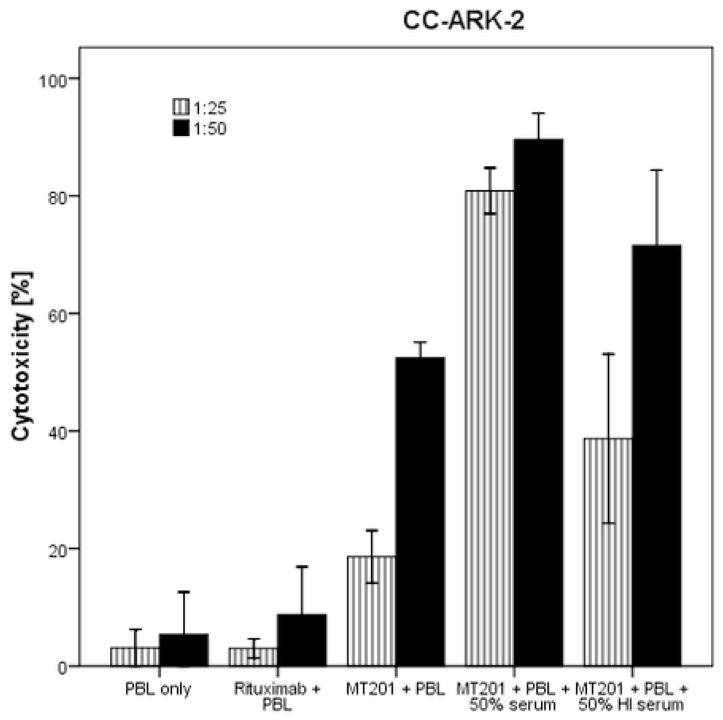
Effect of complement and physiological concentrations of IgG on MT201-mediated ADCC
In order to evaluate the effect of complement on the MT201-mediated ADCC as well as its potential inhibition by physiological IgG serum concentrations, human serum diluted 1:2 (with and without heat inactivation) was added to the ovarian cancer cell lines during standard 4h 51Cr release assays. In the majority of EpCAM-positive cell lines (three OSPC and one clear cell carcinoma), decreased killing after incubation with serum compared to incubation without serum was noted (Figure 3 upper and middle panel). These results illustrate the inhibitory effect of high concentrations of IgG on MT201-mediated ADCC in vitro. In contrast, in one clear cell carcinoma cell line (i.e., CC-ARK-2), the addition of serum lead to a significant increase in killing (p=0.02) while the addition of heat-inactivated serum with MT201 and PBL to this cell line resulted in a decrease of killing compared to the killing in the presence of serum (Figure 3, lower panel). These results are consistent with a peculiar high sensitivity of this ovarian clear cell cancer cell line to complement in vitro.
Figure 3.
Representative cytotoxicity experiments adding human serum to MT201 against OSPC-ARK-1 (upper panel), CC-ARK-1 (middle panel) and CC-ARK-2 (lower panel) cell lines. Ovarian cancer cell lines were challenged by diluted (1:2) serum (with or without heat inactivation) in the presence or absence of the effector cells and MT201 to standard 4-h 51Cr release assays. Addition of physiological concentrations of IgG (i.e., heat-inactivated serum diluted 1:2) to PBL in the presence of MT201 significantly reduced the degree of ADCC achieved in the presence of MT201 against OSPC-ARK-1 and CC-ARK-1. Addition of untreated serum (diluted 1:2) to PBL in the presence of MT201 consistently increased MT201-mediated cytotoxicity against and CC-ARK-1 (p < 0.03) (lower panel).
Discussion
The high mortality of ovarian cancer patients harboring disease refractory to standard treatment mandates the need for a better understanding of the molecular basis of the aggressive biologic behavior of these tumors as well as for the development of novel, target-specific and more effective treatment modalities against chemotherapy resistant/recurrent disease. EpCAM, an adhesion molecule found highly differentially expressed in ovarian cancer by our research group17 as well as others18, may represent a potentially effective target for the immunotherapy of chemotherapy-resistant disease.
Although EpCAM was initially assumed to be mainly involved in cell adhesion19, it is now clear that it also plays a role in carcinogenesis via the upregulation of oncogenes like c-myc and cell-cycle-regulating genes of the cyclin family19. This finding is further confirmed by the fact that silencing EpCAM leads to a decrease in proliferation and metabolism of tumor cells, suggesting that EpCAM may be an attractive target for immunotherapy5. Intramembrane proteolysis and shedding of EpCAM’s extracellular domain have been shown to activate EpCAM signaling6. The extracellular domain, once cleaved, may also function as an agonist to EpCAM expressing cells6. Tumor necrosis factor (TNF)-α can down-regulate, and several chemotherapeutic agents can modulate EpCAM expression9. EpCAM knockdown reduces the expression of c-myc, cyclin D and survivin8. Importantly, EpCAM expression has been described as a marker of progression in cervical dysplasia5,10 and squamous cell lung cancer20 and its overexpression is an independent prognostic marker for reduced survival in breast and ovarian cancer18.
Our study carefully evaluated EpCAM expression level in biologically aggressive and chemotherapy-resistant ovarian cancer cell lines as well as their sensitivity to adecatumumab (MT201), a novel humanized monoclonal antibody (mAb) targeting EpCAM in vitro. We found EpCAM to be overexpressed in five out of seven of the primary ovarian cancer cell lines available to this study, by rtPCR and by flow cytometry. The overexpression of EpCAM in primary chemotherapy resistant ovarian cancer is consistent with results of previous studies by us as well as others performed on fresh frozen and formalin-fixed paraffin embedded ovarian cancer tissues4,17. EpCAM expression may be dependent on the stage and differentiation of the tumor. Bellone et al. described significantly higher levels of EpCAM expression in recurrent and metastatic ovarian tumors17. In other study, EpCAM expression was reported to be significantly lower in stages III and IV than in stage I disease by immunohistochemistry4. In the latter study, the results have been explained by the fact that EpCAM also acts as an adhesion molecule, and the down-regulation of this molecule may facilitate the development of metastases4. Other studies, however, have shown no correlation between EpCAM expression of ovarian cancer tissue and tumor stage18.
The cytotoxic activity of MT201 against ovarian cancer tumor cells in the presence of PBL has previously been demonstrated by Xiang et al.21. In our study, we extend the results of Xiang et al. evaluating the cytotoxic potential of MT201 against multiple biologically aggressive, high grade serous and clear cell chemotherapy-resistant ovarian cancer cell lines. We found all primary ovarian tumors tested showing high EpCAM expression, regardless of their serous or clear cell histology (i.e., OSPC-ARK-1, OSPC-ARK-2, OSCP-ARK-4, CC-ARK-1, CC-ARK-2) to be highly susceptible to MT201-mediated ADCC in the presence of effector cells. In this regard, it is worth noting that although these cell lines were extremely resistant to natural killer cytotoxic activity (i.e., average killing at 50:1 effectors to target cell ratio in controls = 3%), MT201-mediated ADCC resulted in killing of up to 60% in 4-hour 51Cr release assays.
For effective cytotoxicity, the effector cells must be able to interact with the antibody at the target site in vivo, even in the presence of high concentrations of human IgG. In this study, the addition of high concentrations (50%) of human serum resulted in reduced antibody-mediated ADCC in all but one EpCAM-positive ovarian cell line. Our results, showing an inhibitory effect of serum in the majority of the ovarian cancer cell lines tested supports the previous findings of Preithner et al. who also identified endogenous non-specific IgG as the major inhibitory component in human serum22. This group described inhibition of ADCC at physiologic levels of human sera and the reversibility of this effect after addition of IgG22. While the inhibitory effect of IgG on NK cell-mediated ADCC has been described in several studies, results of binding assays, however, suggest that IgG affects the interaction of MT201 with CD16 on NK cells, but not the binding of MT201 to tumor tissue22.
MT201-mediated tumor cell lysis depends on the presence of effector cells13,21 and CD56-positive lymphocytes have been shown to contribute most to the effect of IgG1-mediated ADCC in vitro as well as in vivo22. Interleukin-2 (IL-2) treatment leads to the activation of NK cell cytotoxicity and expansion of the NK cell population within the PBL in vivo23. Consistent with its immuno-stimulatory effect on NK cells24, IL-2 has been previously shown to work synergistically with monoclonal antibodies in vivo25. Importantly, contrary to the significant toxicity of high-dose rIL-2 therapy (recombinant IL-2), low-dose IL-2 administered subcutaneously or by continuous infusion has been shown to have high clinical and immunological activity with a low toxicity profile24. These findings are particularly interesting because a modulation of the number and function of NK cells has been associated with tumor progression in both experimental and animal models and pre-treatment of the PBLs with IL-2 can increase the cytotoxicity levels in patients with suppressed ADCC to levels similar to those of normal donors26,27. Consistent with this data, our in vitro experiments reveal a significant increase of MT201-induced cytotoxicity after the pre-treatment of tumor cells with IL-2 compared to the cytotoxicity in the absence of IL-2. IL-2 seems to therefore enhance the cytotoxic potential of the effector cells. The administration of low doses of IL-2 might therefore be a valid therapeutic option in order to increase MT201-mediated ADCC in heavily pretreated ovarian cancer patients.
The widespread expression of EpCAM in chemotherapy-resistant ovarian cancer cells makes EpCAM an attractive target in the treatment of drug-resistant disease. Consistent with this view, a bispecific anti-EpCAM/anti-CD3 antibody (catumaxomab/Removab®) has been shown to significantly reduce the accumulation of malignant ascites in ovarian cancer patients when administered intraperitoneally (i.p.)28, and has recently received market approval by the European Medicines Agency (EMEA) for this indication. There is a strong need for effective novel targeted therapies in the treatment of chemotherapy-resistant ovarian cancer. In this study, we have demonstrated significant MT201-mediated killing against primary chemotherapy-resistant ovarian carcinoma cell lines. MT201 might therefore represent a fascinating new addition to the treatment of this aggressive disease.
Acknowledgments
Supported by grants from the Angelo Novicelli, the Berlucchi and the Camillo Golgi Foundation, Brescia, Italy, NIH R01 CA122728-01A2 to AS, and grants 501/A3/3 and 00227557 from the Italian Institute of Health (ISS) to AS. This investigation was also supported by NIH Research Grant CA-16359 from the National Cancer Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer Statistics, 2009. CA Cancer J Clin. 2009;59:225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Cho KR, Shih I-M. Ovarian Cancer. Annu Rev Pathol. 2009;4:287–313. doi: 10.1146/annurev.pathol.4.110807.092246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin LP, Schilder RJ. Management of recurrent ovarian carcinoma: current status and future directions. Semin Oncol. 2009;36(2):112–125. doi: 10.1053/j.seminoncol.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Kim J-H, Herlyn D, Wong K-K, et al. Identification of epithelial cell adhesion molecule autoantibody in patients with ovarian cancer. Clin Cancer Res. 2003;9:4782–4791. [PubMed] [Google Scholar]
- 5.Armstrong A, Eck SL. EpCAM. A new therapeutic target for an old cancer antigen. Cancer Biol Ther. 2003;2(4):320–325. doi: 10.4161/cbt.2.4.451. [DOI] [PubMed] [Google Scholar]
- 6.Muenz M, Baeuerle PA, Gires O. The emerging role of EpCAM in cancer and stem cell signaling. Cancer Res. 2009;69(14):5627–5629. doi: 10.1158/0008-5472.CAN-09-0654. [DOI] [PubMed] [Google Scholar]
- 7.Muenz M, Fellinger K, Hofmann T, Schmitt B, Gires O. Glycosylation is crucial for stability of tumor and cancer stem cell antigen EpCAM. Front Biosci. 2008;13:5195–5201. doi: 10.2741/3075. [DOI] [PubMed] [Google Scholar]
- 8.Baeuerle PA, Gires O. EpCAM (CD326) finding its role in cancer. Br J Cancer. 2007;96:417–423. doi: 10.1038/sj.bjc.6603494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trzpis M, McLaughlin PMJ, de Leij LMHF, Harmsen MC. Epithelial cell adhesion molecule. More than a carcinoma marker and adhesion molecule. Am J Pathol. 2007;171(2):386–395. doi: 10.2353/ajpath.2007.070152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Litvinov SV, Balzar M, Winter MJ, et al. Epithelial cell adhesion molecule (EpCAM) modulates cell-cell interactions mediated by classic cadherins. J Cell Biol. 1997;139:1337–1348. doi: 10.1083/jcb.139.5.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osta WA, Chen Y, Mikhitarian K, et al. EpCAM is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Res. 2004;64:5818–5824. doi: 10.1158/0008-5472.CAN-04-0754. [DOI] [PubMed] [Google Scholar]
- 12.Riethmueller G, Holz E, Schlimok G, et al. Monoclonal antibody therapy for resected Duke’s C colorectal cancer: seven-year outcome of a multicenter randomized trial. J Clin Oncol. 1998;16(5):1788–1794. doi: 10.1200/JCO.1998.16.5.1788. [DOI] [PubMed] [Google Scholar]
- 13.Naundorf S, Preithner S, Mayer P, et al. In vitro and in vivo activity of MT201, a fully human monoclonal antibody for pancarcinoma treatment. In J Cancer. 2002;100:101–110. doi: 10.1002/ijc.10443. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt M, Scheulen ME, Dittrich C, et al. An open-label, randomized phase II study of adecatumumab, a fully human anti-EpCAM antibody, as monotherapy in patients with metastatic breast cancer. Ann Oncol. 2009 doi: 10.1093/annonc/mdp314. (epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 15.Marschner N, Rűttinger D, Zugmaier G, et al. Phase II study of the human anti-EpCAM antibody adecatumumab in prostate cancer patients with increasing serum levels of prostate specific antigen after radical prostatectomy. Urol Int. 2010 doi: 10.1159/000318055. (in press) [DOI] [PubMed] [Google Scholar]
- 16.Sebastian M, Hanusch C, Schmidt, et al. Safety and antitumor activity of 3 weekly anti-EpCAM antibody adecatumumab in combination with docetaxel for patients with metastatic breast cancer: results of a multicenter phase Ib trial. J Clin Oncol. 2009;27(suppl):15s. abstr 1009. [Google Scholar]
- 17.Bellone S, Siegel ER, Cocco E, et al. Overexpression of epithelial cell adhesion molecule in primary, metastatic, and recurrent/chemotherapy-resistant epithelial ovarian cancer. Int J Gynecol Cancer. 2009;19(5):860–866. doi: 10.1111/IGC.0b013e3181a8331f. [DOI] [PubMed] [Google Scholar]
- 18.Spizzo G, Went P, Dirnhofer S, et al. Overexpression of epithelial cell adhesion moleculre (EpCAM) is an independent prognostic marker for reduced survival of patients with epithelial ovarian cancer. Gynecol Oncol. 2006;103:483–488. doi: 10.1016/j.ygyno.2006.03.035. [DOI] [PubMed] [Google Scholar]
- 19.Maetzel D, Denzel S, Mack B, et al. Nuclear signaling by tumour-associated antigen EpCAM. Nat Cell Biol. 2009;11(2):162–171. doi: 10.1038/ncb1824. [DOI] [PubMed] [Google Scholar]
- 20.Piyathilake CJ, Frost AR, Weiss H, Manne U, Heimburger DC, Grizzle WE. The expression of Ep-CAM (17-1A) in squamous cell cancers of the lung. Hum Pathol. 2000;31:482–487. doi: 10.1053/hp.2000.6711. [DOI] [PubMed] [Google Scholar]
- 21.Xiang W, Wimberger P, Dreier T, et al. Cytotoxic activity of novel human monoclonal antibody MT201 against primary ovarian tumor cells. J Cancer Res Clin Oncol. 2003;129:341–348. doi: 10.1007/s00432-003-0438-6. [DOI] [PubMed] [Google Scholar]
- 22.Preithner S, Elm S, Lippold S, et al. High concentrations of therapeutic IgG1 antibodies are needed to compensate for inhibition of antibody-dependent cellular cytotoxicity by excess endogenous immunoglobulin G. Mol Immunol. 2006;43:1183–1193. doi: 10.1016/j.molimm.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 23.Caligiuri MA, Murray C, Robertson MJ, et al. Selective modulation of human natural killer cells in vivo after prolonged infusion of low dose recombinant interleukin 2. J Clin Invest. 1993;91:123–132. doi: 10.1172/JCI116161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boyman O, Surh CD, Sprent J. Potential use of IL-2/anti-IL-2 antibody immune complexes for the treatment of cancer and autoimmune disease. Expert Opin Biol Ther. 2006;6(12):1323–1331. doi: 10.1517/14712598.6.12.1323. [DOI] [PubMed] [Google Scholar]
- 25.Hoojberg E, Sein JJ, van den Berk PCM, et al. Eradication of large human B cell tumors in nude mice with unconjugated CD20 monoclonal antibodies and interleukin 2. Cancer Res. 1995;55:2627–2634. [PubMed] [Google Scholar]
- 26.Choe B, Frost P, Morrison N, Rose N. Natural killer cell activity of prostatic cancer patients. Cancer Invest. 1987;5:285–288. [PubMed] [Google Scholar]
- 27.Honsik CJ, Jung G, Reisfeld RA. Lymphokine-activated killer cells targeted by monoclonal antibodies to the disialogangliosides GD2 and GD3 specifically lyse human tumor cells of neuroectodermal origin. Proc Natl Acad Sci USA. 1986;83:7893–7897. doi: 10.1073/pnas.83.20.7893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burges A, Wimberger P, Kuemper C, et al. Effective relief of malignant ascites in patients with advanced ovarian cancer by a trifunctional anti-EpCAM x anti-CD3 antibody: a phase I/II study. Clin Cancer Res. 2007;13(13):3899–3905. doi: 10.1158/1078-0432.CCR-06-2769. [DOI] [PubMed] [Google Scholar]