Abstract
Background and objectives: Higher phosphate is associated with mortality in dialysis patients but few prospective studies assess this in nondialysis patients managed in an outpatient nephrology clinic. This prospective longitudinal study examined whether phosphate level was associated with death in a referred population.
Design, setting, participants & measurements: Patients (1203) of nondialysis chronic kidney disease (CKD) in the Chronic Renal Insufficiency Standards Implementation Study were assessed. Survival analyses were performed for quartiles of baseline phosphate relative to GFR, 12-month time-averaged phosphate, and baseline phosphate according to published phosphate targets.
Results: Mean (SD) eGFR was 32 (15) ml/min per 1.73 m2, age 64 (14) years, and phosphate 1.2 (0.30) mmol/L. Cox multivariate adjusted regression in CKD stages 3 to 4 patients showed an increased risk of all-cause and cardiovascular mortality in the highest quartile compared with that in the lowest quartile of phosphate. No association was found in CKD stage 5 patients. Patients who had values above recommended targets for phosphate control had increased risk of all-cause and cardiovascular death compared with patients below target. The highest quartile compared with the lowest quartile of 12-month time-averaged phosphate was associated with an increased risk of mortality.
Conclusions: In CKD stages 3 to 4 patients, higher phosphate was associated with a stepwise increase in mortality. As phosphate levels below published targets (as opposed to within them) are associated with better survival, guidelines for phosphate in nondialysis CKD patients should be re-examined. Intervention trials are required to determine whether lowering phosphate will improve survival.
Higher serum phosphate is associated with mortality in hemodialysis patients (1–3). There have been three studies in patients with chronic kidney disease (CKD), not on dialysis, evaluating the association of serum phosphate with mortality; two of these found a positive association (4–6). The relationship between serum phosphate and mortality in patients with CKD stages 3 to 5 (eGFR <60 ml/min per 1.73 m2) who are not on dialysis, and who are under regular nephrological review, has not previously been examined in a prospective systematic way. Survival data according to follow-up phosphate results are also lacking in CKD patients.
The aims of this single-center study were to investigate whether an association of serum phosphate with all-cause and cardiovascular mortality could be shown prospectively in outpatients with advanced CKD (stage 5) not receiving dialysis and also in those with earlier (stages 3 and 4) CKD. The relationship of 12-month time-averaged phosphate and mortality and the influence upon survival of a serum phosphate within guideline targets was examined in this population.
Materials and Methods
The Chronic Renal Insufficiency Standards Implementation Study (CRISIS) is a single-center prospective epidemiologic study of non–dialysis-dependent patients with an eGFR <60 ml/min per 1.73 m2 under review in the outpatient clinics of Salford Royal Foundation NHS Trust. All new patients with eGFR <60 ml/min per 1.73 m2 are approached for study entry, and those who provide informed consent are enrolled. The study has been recruiting since 2002 and its primary function is to determine factors influencing outcomes and progression of renal disease in CKD patients. Of the 1390 patients enrolled in CRISIS at the time of this analysis, 1203 had data that were available for analysis; 77 patients were excluded because of loss of follow-up and 110 patients were excluded because of lack of available baseline phosphate. All patients were followed up from recruitment into the study until either death or data lock (January 2008). Cause of death was obtained from the UK Office of National Statistics. All biochemical samples were analyzed in a single laboratory using a Roche Modular analyzer (creatinine using the compensated kinetic Jaffe method), with the exception of intact parathyroid hormone, which was analyzed with a second-generation assay on a Diagnostic Products Corporation Immulite 2000. Proteinuria was determined with either 24-hour urine collections or urine protein:creatinine ratio, depending on routine clinical practice at recruitment. Baseline clinical data determined at recruitment were collected for analysis including comorbidities and current medication. Cardiovascular disease was defined as previous myocardial infarction, coronary-artery bypass graft, coronary angioplasty, peripheral vascular disease, stroke, or angina.
Twelve-month time-averaged phosphate was determined as the average of all serum phosphate results in the first 12 months since recruitment. All patients who had two or more phosphate results available during the 12-month period were included. Change in eGFR over 1 year (δeGFR) was calculated using the following equation: ((eGFR1 − eGFR0)/(T1 − T0)) × 365.25.
The CRISIS study had ethical approval and investigations were performed in accordance with the principles of the Declaration of Helsinki as revised in 2000.
Statistical Analyses
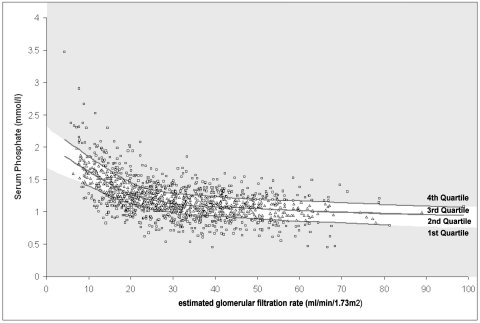
Because of the strong link between serum phosphate, eGFR, and mortality, the phosphate results were reported relative to renal function. Phosphate results were divided into quartiles relative to eGFR (calculated using a modified Modification of Diet in Renal Disease [MDRD] equation) (7) (see Figure 1) and adjustment was effected using a “local smoothing” technique in SigmaPlot 2001. This technique maintains the integrity of the data while reducing the “noise” and provides a “smooth line” through the middle of the data. This was then performed in the upper and lower halves of the phosphate data range to produce quartiles. This method was previously published in studies examining phosphate and mortality (5). ANOVA and χ2 tests were used to examine associations with potentially influential parameters across the quartiles; these were repeated according to eGFR category (15 to 59 ml/min per 1.73 m2 and <15 ml/min per 1.73 m2)—see below. All Cox regression survival analyses performed in this study were adjusted for age, gender, proteinuria, diabetes, hemoglobin, systolic BP, smoking status, cardiovascular disease, eGFR, and the use of vitamin D analogs and phosphate binders at baseline. Survival analyses were performed on baseline serum phosphate relative to eGFR in the whole population. As there is increasing evidence of reverse cardiovascular epidemiology in patients with advanced (stage 5) CKD (8,9), a group of patients who tend to have extensive comorbidities and multiple competing cardiovascular risk factors, analysis was also stratified for eGFR both above and below 15 ml/min per 1.73 m2.
Figure 1.
Phosphate quartiles generated relative to eGFR using local smoothing technique.
Survival analyses on 12-month time-averaged phosphate were performed from study baseline. Survival analyses were also performed on phosphate according to categories defined by the National Kidney Dialysis Outcomes Quality Initiative (KDOQI) (the guideline in use at the time of data lock) and UK Renal Association (UKRA) guidelines (10,11). These were determined according to stage of CKD: CKD stages 3 to 4 patients were “in target” with serum phosphate 0.87 to 1.48 mmol/L (KDOQI) or 0.9 to 1.5 mmol/L (UKRA); CKD stage 5 patients were “in target” with serum phosphate 1.13 to 1.78 mmol/L (KDOQI) and 1.1 to 1.8 mmol/L (UKRA). All analyses were performed using SPSS 14.0 and P < 0.05 was considered significant.
Results
Mean (SD) eGFR of the population was 32 (15) ml/min per 1.73 m2, age 64 (14) years, corrected calcium 2.29 (0.14) mmol/L, and phosphate 1.2 (0.30) mmol/L. Cardiovascular disease was present in 32% of patients at enrollment and 32% of patients had diabetes. Only 7% (n = 89) of patients were receiving a phosphate binder and 17% (n = 199) were receiving a vitamin D analog at baseline. Because of these small numbers, further analyses of binder and vitamin D analog usage were not performed, although baseline usage was adjusted for in survival analyses. Because of the strong associations between eGFR and both mortality and phosphate, analyses were performed on phosphate relative to eGFR to overcome this potentially confounding relationship, and the demographics according to these quartiles are shown in Table 1. This demonstrated that baseline eGFR–related phosphate quartiles were positively associated with female gender, proteinuria, diabetes, and current smokers. A negative association was seen with age, hemoglobin, weight, BMI, and cardiovascular disease. There was no significant difference in mean days of follow-up from lower to higher quartiles of phosphate (P = 0.8) and these were 1079, 1055, 1035, and 1036 days, respectively.
Table 1.
Demographic data across quartiles of phosphate adjusted for eGFR
| N = 1203, Mean (SD), n (%), Median (range) | All | First Quartile, n = 275 | Second Quartile, n = 345 | Third Quartile, n = 320 | Fourth Quartile, n = 263 | P |
|---|---|---|---|---|---|---|
| Age (years) | 64 (14) | 66 (13) | 65 (14) | 64 (13) | 61 (15) | <0.0005 |
| Female gender | 427 (36%) | 74 (27%) | 114 (33%) | 126 (40%) | 113 (43%) | <0.0005 |
| eGFR (ml/min per 1.73 m2) | 32 (15) | 32 (15) | 32 (15) | 31 (15) | 33 (16) | 0.561 |
| Corr. calcium (mmol/L) | 2.29 (0.14) | 2.28 (0.13) | 2.30 (0.15) | 2.28 (0.14) | 2.30 (0.15) | 0.119 |
| Phosphate (mmol/L) | 1.2 (0.31) (0.45 to 3.47) | 0.9 (0.17) (0.45 to 1.38) | 1.1 (0.16) (0.83 to 1.67) | 1.3 (0.20) (0.99 to 1.98) | 1.5 (0.32) (1.08 to 3.47) | <0.0001 |
| PTH (pg/ml) normal range 10 to 65 | 89 (1 to 1019) | 87 (4 to 677) | 88 (2 to 699) | 95 (3 to 1019) | 87 (1 to 488) | 0.683 |
| Hemoglobin (g/L) | 124 (17) | 130 (17) | 125 (18) | 122 (15) | 120 (17) | <0.0005 |
| Proteinuria (grams per day) | 1.1 (0 to 16.2) | 0.8 (0.05 to 8.9) | 0.8 (0.05 to 14.9) | 1.3 (0.1 to 16.2) | 1.5 (0 to 15.1) | <0.0005 |
| CVD | 379 (32%) | 93 (34%) | 119 (35%) | 105 (33%) | 62 (23%) | 0.015 |
| DM | 383 (32%) | 80 (29%) | 93 (27%) | 118 (37%) | 92 (35%) | 0.022 |
| SBP (mmHg) | 139 (22) | 141 (21) | 138 (21) | 140 (22) | 138 (24) | 0.338 |
| DBP (mmHg) | 76 (13) | 76 (13) | 76 (12) | 77 (13) | 76 (13) | 0.771 |
| PP | 63 (19) | 65 (19) | 62 (18) | 64 (19) | 63 (22) | 0.279 |
| Weight (kg) | 81 (18) | 85 (20) | 82 (17) | 79 (19) | 77 (17) | <0.0005 |
| BMI | 28 (6) | 29 (7) | 29 (5) | 28 (6) | 27 (6) | 0.003 |
| Current smoker | 156 (13%) | 18 (7%) | 37 (11%) | 52 (16%) | 49 (19%) | <0.0005 |
| Ever smoked | 832 (69%) | 190 (69%) | 242 (70%) | 209 (66%) | 191 (72%) | 0.363 |
| All binders | 90 (8%) | 16 (6%) | 17 (5%) | 24 (8%) | 33 (13%) | 0.003 |
| Non-Ca phosphate binders | 11 (1%) | 2 (0.7%) | 1 (0.3%) | 4 (1.3%) | 4 (1.5%) | 0.387 |
| Calcium-containing phosphate binders | 81 (7%) | 15 (6%) | 16 (5%) | 20 (6%) | 30 (12%) | 0.007 |
| Vitamin D analogs | 199 (17%) | 47 (17%) | 63 (18%) | 52 (16%) | 37 (14%) | 0.607 |
PTH, parathyroid hormone; CaxP, calcium × phosphate product; CVD, cardiovascular disease; DM, diabetes; SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pulse pressure; BMI, body mass index; Non-Ca, non–calcium containing.
Death occurred in 22% (n = 271) of the total population, with 9% (n = 109) because of cardiovascular causes, in a median follow-up period of 37.2 (0.5 to 64) months. There was a higher percentage of deaths in CKD stage 5 patients (62 of 167; 37%) compared with those with CKD stages 3 to 4 (209 of 1036; 20%, P < 0.001). Fifty-nine percent of CKD stage 5 patients progressed to renal replacement therapy during the follow-up period compared with only 9% of CKD stages 3 to 4 patients (P < 0.001). There was no significant difference in clinical characteristics between the study population and those patients who had been excluded from study (data not shown).
For each 0.323 mmol/L (1 mg/dl) increase of baseline phosphate, a 26% increase in all-cause mortality (HR 1.3 [1.1,1.5] P = 0.01) and a 50% increase in cardiovascular mortality (HR 1.5 [1.2,2.0] P = 0.002) was observed for the entire population (CKD stages 3 to 5) in multivariate analyses.
Cox regression showed no significant difference in mortality across phosphate quartiles relative to eGFR (HR 1.4 [0.9,2.2] P = 0.1) when comparing the highest with the lowest quartile in CKD stages 3 to 5. Cox regression stratified according to CKD stages 3 to 4 (n = 1036) and those with CKD stage 5 (n = 167) showed an increase in risk of all-cause mortality in CKD stages 3 to 4 patients across the phosphate quartiles with the highest quartile having a significantly increased hazard ratio of 1.8 (1.1,3.1; P = 0.02) compared with the lowest quartile (Table 2). Cardiovascular mortality risk was also increased in CKD stages 3 to 4 (HR 2.9 [1.3,6.4] P = 0.01). No such association was observed for patients with stage 5 CKD (HR 0.6 [0.2,1.4] P = 0.2).
Table 2.
Cox regression: Hazard ratios across quartiles of phosphate relative to eGFR in patients with CKD stages 3 to 4
| N = 1036, Phosphate Quartiles According to eGFR | All-Cause Mortality |
Cardiovascular Mortality |
||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| First quartile (low) | 1.0 | 1.0 | ||
| Second quartile | 1.6 (1.00, 2.4) | 0.05 | 1.8 (0.9, 3.7) | 0.1 |
| Third quartile | 1.6 (0.99, 2.5) | 0.06 | 2.8 (1.3, 5.9) | 0.007 |
| Fourth quartile (high) | 1.8 (1.1, 3.1) | 0.02 | 2.9 (1.3, 6.4) | 0.01 |
Analysis adjusted for age, gender, proteinuria, diabetes, hemoglobin, systolic blood pressure, current smoking status, cardiovascular disease, eGFR, renal replacement therapy, and vitamin D analog and phosphate binder use.
Cox regression survival analysis of the 12-month time-averaged phosphate results for CKD stages 3 to 5 showed an increase in mortality across the quartiles with the upper quartile having a significantly increased all-cause mortality compared with the lowest quartile (HR 1.8 [1.1,2.9] P = 0.01) (Table 3). Cardiovascular mortality also increased but did not reach significance (HR 1.8 [0.9,3.9] P = 0.1). When 1 year δeGFR was included in the multifactorial model, the relationship between time-averaged phosphate and mortality became insignificant (HR 1.4 [0.8,2.6] P = 0.3). Multifactorial analyses incorporating baseline phosphate with δeGFR and δphosphate were performed. This suggested that baseline phosphate (HR 2.2 [1.1,4.3] P = 0.03) and δeGFR (HR 1.2 [1.0,1.3] P = 0.05 [per 5 ml/min per 1.73 m2 per year change]) were significant factors affecting mortality whereas δphosphate showed no association (HR 1.1 [0.9,1.3] P = 0.4).
Table 3.
Results of survival analysis for quartiles of 12-month time-averaged phosphate for all patients (CKD stages 3 to 5)
| N = 1203, Quartiles: 12-Month Time-Averaged Phosphate (mmol/L) | All-Cause Mortality |
Cardiovascular Mortality |
||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| <1.02 | 1.0 | 1.0 | ||
| 1.02 to 1.15 | 1.2 (0.8, 1.9) | 0.4 | 1.5 (0.8, 2.9) | 0.2 |
| 1.16 to 1.34 | 1.2 (0.8, 1.8) | 0.5 | 1.2 (0.6, 2.3) | 0.7 |
| >1.34 | 1.8 (1.1, 2.9) | 0.01 | 1.8 (0.9, 3.9) | 0.1 |
Analysis adjusted for age, gender, proteinuria, diabetes, hemoglobin, systolic blood pressure, current smoking status, cardiovascular disease, eGFR, and vitamin D analog and phosphate binder use.
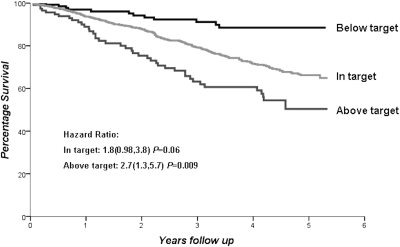
Cox regression was also performed according to whether or not patients had a phosphate level within the KDOQI or UKRA targets for phosphate control (Table 4). Phosphate within target was associated with nearly double the mortality risk compared with levels below target in patients with CKD stages 3 to 5 for both guidelines (UKRA HR 1.7 [1.0,2.8] P = 0.05, KDOQI HR 1.8 [1.0,3.8] P = 0.06). However, phosphate above the target range conferred a 2.5- to 3-fold increased risk of death (UKRA HR 2.8 [1.5,5.4] P = 0.002, KDOQI HR 2.7 [1.3,5.7] P = 0.009) compared with serum phosphate below the lower limit of the target range. The risk of cardiovascular death was even greater for patients above target compared with those below target (UKRA HR 4.1 [1.5,10.6] P = 0.004, KDOQI HR 4.0 [1.4,11.9] P = 0.01). The Kaplan-Meier survival curve according to attainment of KDOQI guidelines is shown in Figure 2; the hazard ratios stated are multifactorial adjusted analyses.
Table 4.
Cox regression: Hazard ratios across international targets of serum phosphate for CKD stages 3 to 5
| UK Renal Association |
KDOQI |
|||||||
|---|---|---|---|---|---|---|---|---|
| All-Cause Mortality |
CV Mortality |
All-Cause Mortality |
CV Mortality |
|||||
| HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | |
| Below target | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| In target | 1.7 (1.0, 2.8) | 0.05 | 1.6 (0.8, 3.5) | 0.2 | 1.8 (0.98, 3.8) | 0.06 | 1.8 (0.7, 4.6) | 0.2 |
| Above target | 2.8 (1.5, 5.4) | 0.002 | 4.1 (1.5, 10.6) | 0.004 | 2.7 (1.3, 5.7) | 0.009 | 4.0 (1.4, 11.9) | 0.01 |
UKRA target range: CKD stages 3 to 4: 0.9 to 1.5 mmol/L; CKD stage 5: 1.1 to 1.8 mmol/L. KDOQI target range: CKD stages 3 to 4: 0.87 to 1.48 mmol/L; CKD stage 5: 1.13 to 1.78 mmol/L. Analysis adjusted for age, gender, proteinuria, diabetes, hemoglobin, systolic blood pressure, current smoking status, cardiovascular disease, eGFR, and vitamin D analog and phosphate binder use.
Figure 2.
Survival according to phosphate levels relative to KDOQI guidelines.
Discussion
The aim of this study was to determine, in a large nondialysis CKD population, whether an association exists between serum phosphate and mortality in patients under regular outpatient nephrological care. The CRISIS data were used, which is collected with the primary purpose of prospectively examining outcomes and progression of nondialysis CKD. We found that higher serum phosphate, even within the normal laboratory range, was associated with an increase in mortality in patients with CKD stages 3 to 4. More than 90% of our CKD stages 3 to 4 patients had a serum phosphate within the normal laboratory range and this is consistent with other studies (12). Evidence from the Framingham offspring study suggests that differences within the normal range of phosphate are associated with increased cardiovascular risk in the general population (13). Analyses of the ARIC study have also found an increased risk of cardiovascular events and death in association with higher “normal” range baseline serum phosphate in community-dwelling adults (14). Although other studies have also examined the relationship of phosphate to mortality in patients with non–dialysis-treated CKD, our study differs in that it is the first single-center prospective study that has investigated nondialysis patients with CKD stages 3 to 5 who are under regular outpatient nephrological follow-up. The study population was large and patients received focused management of their renal disease, suggesting that even when under regular specialist care the mortality risk associated with serum phosphate is still significant.
Kestenbaum (5) et al. studied a large U.S. veteran population who had impaired renal function although only 10% was under regular nephrology care at baseline. The study showed that serum phosphate adjusted for creatinine clearance was associated with mortality. Patients with the lowest serum phosphate had the best survival, as in our study, with a hazard ratio <1, but this did not reach statistical significance. This study also reported a HR 1.2 (1.1,1.4) for each 1 mg/dl increase of serum phosphate in multivariate analysis, which is comparable with our results (HR 1.3 [1.1,1.5]).
Menon (4) et al. investigated the association of serum phosphate and mortality in 840 randomized patients within the MDRD study but showed no association after adjusting for other influential factors such as GFR. Voormolen (6) et al. prospectively studied predialysis patients with eGFR <20 ml/min per 1.73 m2 and found an association of phosphate with progression of renal disease and mortality. Their population had much higher levels of phosphate compared with our study, which is not unexpected given the differences in renal function between the two studies (mean eGFR [SD] was 13 [5.4] ml/min per 1.73 m2 versus 32 [14] ml/min per 1.73 m2 in our study). Forty-eight percent of that study population had a phosphate above target range according to KDOQI guidelines compared with only 9.7% of our population; only 2% were below the target range compared with 12% in our study. In contrast to the findings of Voormolen et al., we found that in patients with CKD stage 5 the association of serum phosphate with mortality, when adjusted for GFR, was no longer significant. There are several potential explanations for this finding. Our sample size of CKD stage 5 patients was relatively small. There is no doubt that factors contributing to mortality in CKD stage 5 become more complex even before commencement of dialysis. Studies that have investigated modification of other cardiovascular risk factors, such as reducing cholesterol with statins, have shown no benefit to survival in dialysis patients perhaps because of the effects of multiple competing risk factors (15) (e.g., left ventricular hypertrophy, cardiac dilation, and arterial stiffness). Evidence of this reverse epidemiology is also seen in nondialysis patients with an eGFR <15 ml/min per 1.73 m2 (8,9). Our stage 5 CKD group was biased toward even higher risk patients as those patients within CRISIS who opted for conservative care of ESRD were included. As such patients tend to have greater comorbidity and are older and more malnourished than their counterparts who had chosen to receive renal replacement therapy, or than those with higher levels of eGFR, it would be expected that in this subgroup a lower phosphate might confer a higher risk of death, conflicting with the evidence found in the larger CKD stages 3 to 4 population. Block et al. (1) have shown lower phosphate to be associated with increased mortality in hemodialysis patients, presumably partly explained by malnutrition in the sicker patients.
The 12-month time-averaged phosphate data showed a relationship between persistent elevation of phosphate and mortality. This association became insignificant when δeGFR was included in the multivariate model. This could be due to the deterioration of renal function being such a major risk factor for mortality that increased numbers or longer follow-up would be needed to show the effect of phosphate. Also, the time-averaged phosphate included all phosphate results analyzed within the first year after enrollment, including those during hospital admissions and in patients with acute renal impairment, whereas δeGFR involved only two measurements and so may miss important additional changes that had occurred during the year.
A pathogenetic link might explain the associations between mortality and higher phosphate found in this study. One plausible explanation is the involvement of phosphate in the pathogenesis of vascular calcification, which has been well documented in the literature (16–19). Other CKD-related disturbances can also potentially explain the association. Serum phosphate level has been associated with CKD progression (6) and left ventricular hypertrophy (20), which are known to contribute to cardiovascular disease and death. Our results confirm an association of increasing phosphate with declining eGFR. Native vitamin D21 and the phosphatonin, fibroblast growth factor 23 (FGF23) (22), are factors thought to have regulatory roles in mineral metabolism and abnormalities occur early in CKD before changes in calcium, phosphate, and parathyroid hormone. FGF23 is now thought to be the main regulator of phosphate homeostasis and increasing levels have been associated with mortality in hemodialysis patients, an effect independent of serum phosphate (23). The mechanisms of this association with mortality remain unknown.
Diet could be a further explanation for the association of higher phosphate and mortality in both the general and CKD population, with higher serum phosphate perhaps reflecting a more unhealthy high phosphate diet. Conversely, an increased risk of death is seen in dialysis patients with low serum phosphate, (24,1) the relationship thought to reflect malnutrition or co-existing illness. This association was not apparent in our study of nondialysis patients and, importantly, lower serum phosphate (i.e., even below the current target ranges for CKD) seemed to be associated with improved survival. This suggests that malnutrition may be less of a problem in the nondialysis population with earlier CKD, and interestingly we found that patients with higher serum phosphate actually had lower weight and BMI.
It is possible its relationship with mortality may simply represent an association, with phosphate being co-localized with other more important factors. For example, genetic influence of phosphate control may be associated with a predisposition to cardiovascular disease, or higher phosphate may just be a marker of some other cause of cardiovascular risk and mortality. This may explain the recent finding in the CARDIA population that higher serum phosphate even within the normal range was associated with greater likelihood of coronary calcification at 15 years in a healthy young population (25). More research is needed to investigate these possibilities.
It was interesting to note that patients who had serum phosphate below the targets recommended in the KDOQI and the UKRA guidelines (10,11) had the best survival. It should not be overlooked that guidelines for serum phosphate in CKD were devised using only studies involving dialysis patients (10,11), a potential shortcoming for guidelines that have been followed internationally and generalized to nondialysis CKD patients. Our study would suggest that in nondialysis CKD patients a lower limit, as opposed to an upper limit, for serum phosphate is not required in the guidelines.
Our study does have several limitations. Patients have been recruited into the CRISIS study consecutively since 2002, and so the length of follow-up period was not consistent. The CRISIS population is 98% Caucasian, indicative of our catchment population, and our results may not be generalizable to CKD patients of other ethnic origins. Although we assessed 12-month time-averaged phosphate, we were unable to correct for an equivalent 12-month time-averaged eGFR; hence, we could not correct for similar episodes of ill health during the 12-month period. As the majority of the patients had a phosphate within the normal laboratory range and <10% of patients were prescribed binder therapy, data relating to the effect of phosphate binder usage in the study was not analyzed, but the multivariate analyses were corrected for their use.
In conclusion, this large prospective study of CKD patients not receiving dialysis, but managed in a secondary care renal service, suggests that all-cause and cardiovascular mortality risk independently increases as serum phosphate increases in patients with CKD stages 3 to 4. Patients with phosphate levels even within contemporary CKD guideline targets were associated with poorer outcome than those with serum phosphate below the target range. This suggests that even in earlier stages of renal dysfunction a lower phosphate is associated with better survival. Intervention trials that investigate whether lowering phosphate will improve survival for patients with earlier stages of CKD are indicated.
Disclosures
None.
Acknowledgment
This work was supported by an educational grant from Genzyme.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. Block GA, Hulbert-Shearon TE, Levin NW, Port FK: Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: A national study. Am J Kidney Dis 31: 607–617, 1998 [DOI] [PubMed] [Google Scholar]
- 2. Ganesh SK, Stack AG, Levin NW, Hulbert-Shearon T, Port FK: Association of elevated serum PO(4), Ca x PO(4) product, and parathyroid hormone with cardiac mortality risk in chronic hemodialysis patients. J Am Soc Nephrol 12: 2131–2138, 2001 [DOI] [PubMed] [Google Scholar]
- 3. Stevens LA, Djurdjev O, Cardew S, Cameron EC, Levin A: Calcium, phosphate, and parathyroid hormone levels in combination and as a function of dialysis duration predict mortality: Evidence for the complexity of the association between mineral metablism and outcomes. J Am Soc Nephrol 15: 770–779, 2004 [DOI] [PubMed] [Google Scholar]
- 4. Menon V, Greene T, Pereira AA, Wang X, Beck GJ, Kusek JW, Collins AJ, Levey AS, Sarnak MJ: Relationship of phosphorus and calcium-phosphorus product with mortality in CKD. Am J Kidney Dis 46: 455–463, 2005 [DOI] [PubMed] [Google Scholar]
- 5. Kestenbaum B, Sampson JN, Rudser KD, Patterson DJ, Seliger SL, Young B, Sherrard DJ, Andress DL: Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol 16: 520–528, 2005 [DOI] [PubMed] [Google Scholar]
- 6. Voormolen N, Noordzij M, Grootendorst DC, Beetz I, Sijpkens YW, van Manen JG, Boeschoten EW, Huisman RM, Krediet RT, Dekker FW: High plasma phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant 22: 2909–2916, 2007 [DOI] [PubMed] [Google Scholar]
- 7. Levey AS, Greene T, Kusek JW, Beck GJ: A simplified equation to predict glomerular filtration rate from serum creatinine (abstract). J Am Soc Nephrol 11: 155A, 2000 [Google Scholar]
- 8. Kalantar-Zadeh K, Kovesdy CP, Derose SF, Horwich TB, Fonarow GC: Racial and survival paradoxes in chronic kidney disease. Nat Clin Pract Nephrol 3: 493–506, 2007 [DOI] [PubMed] [Google Scholar]
- 9. Kovesdy CP, Anderson JE: Reverse epidemiology in patients with chronic kidney disease who are not yet on dialysis. Semin Dial 20: 566–569, 2007 [DOI] [PubMed] [Google Scholar]
- 10. National Kidney Foundation: K/DOQI clinical practice guidelines: Bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42: S1–S201, 2003 [PubMed] [Google Scholar]
- 11. UK Renal Association: Clinical Practice Guidelines. Module 2: Complications, 4th Ed., 2007. Available at: http://www.renal.org/Clinical/GuidelinesSection/ComplicationsofCKD.aspx Accessed July 28, 2010
- 12. Reichel H, Deibert B, Schmidt-Gayk H, Ritz E: Calcium metabolism in early chronic renal failure: Implications for the pathogenesis of hyperparathyroidism. Nephrol Dial Transplant 6: 162–169, 1991 [DOI] [PubMed] [Google Scholar]
- 13. Dhingra R, Sullivan LM, Fox CS, Wang TJ, D'Agostino RB, Sr., Gaziano JM, Vasan RS: Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med 167: 879–885, 2007 [DOI] [PubMed] [Google Scholar]
- 14. Foley RN, Collins AJ, Ishani A, Kalra PA: Calcium-phosphate levels and cardiovascular disease in community-dwelling adults: The Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J 156: 556–563, 2008 [DOI] [PubMed] [Google Scholar]
- 15. Wanner C, Krane V, Marz W, Olschewski M, Mann JF, Ruf G, Ritz E: Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med 353: 238–248, 2005 [DOI] [PubMed] [Google Scholar]
- 16. Giachelli CM: The emerging role of phosphate in vascular calcification. Kidney Int 75: 890–897, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hruska KA, Mathew S, Lund RJ, Memon I, Saab G: The pathogenesis of vascular calcification in the chronic kidney disease mineral bone disorder: The links between bone and the vasculature. Semin Nephrol 29: 156–165, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ketteler M, Biggar PH: Review article: Getting the balance right: Assessing causes and extent of vascular calcification in chronic kidney disease. Nephrology (Carlton) 14: 389–394, 2009 [DOI] [PubMed] [Google Scholar]
- 19. Nikolov IG, Mozar A, Drueke TB, Massy ZA: Impact of disturbances of calcium and phosphate metabolism on vascular calcification and clinical outcomes in patients with chronic kidney disease. Blood Purif 27: 350–359, 2009 [DOI] [PubMed] [Google Scholar]
- 20. Strozecki P, Adamowicz A, Nartowicz E, Odrowaz-Sypniewska G, Wlodarczyk Z, Manitius J: Parathormon, calcium, phosphorus, and left ventricular structure and function in normotensive hemodialysis patients. Ren Fail 23: 115–126, 2001 [DOI] [PubMed] [Google Scholar]
- 21. Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, Andress DL: Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: Results of the study to evaluate early kidney disease. Kidney Int 71: 31–38, 2007 [DOI] [PubMed] [Google Scholar]
- 22. Marsell R, Grundberg E, Krajisnik T, Mallmin H, Karlsson M, Mellstrom D, Orwoll E, Ohlsson C, Jonsson KB, Ljunggren O, Larsson TE: Fibroblast growth factor-23 is associated with parathyroid hormone and renal function in a population-based cohort of elderly men. Eur J Endocrinol 158: 125–129, 2008 [DOI] [PubMed] [Google Scholar]
- 23. Gutierrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, Smith K, Lee H, Thadhani R, Juppner H, Wolf M: Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med 359: 584–592, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM: Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol 15: 2208–2218, 2004 [DOI] [PubMed] [Google Scholar]
- 25. Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA: Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol 20: 397–404, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]