The importance of improving HLA matching for African-American recipients is frequently stressed in discussions of cadaver kidney allocation. The argument has been that such efforts will be especially important for improvement of graft survival of African-Americans who have had poorer results than members of all other subgroups. In reality, data supporting this assumption are conflicting except when there is a zero mismatch (1–6).
The opportunity to obtain clarifying information presented itself during performance of a recent multivariate analysis of 31,291 cases of primary cadaver kidney transplantation reported to the United Network for Organ Sharing (UNOS*) Scientific Registry between 1991 and 1995 (7), for which follow-up was to January 1, 1997. The collection included 8,111 African-Americans, whose graft survival at all gradations of HLA mismatch level is presented herein. The Pittsburgh experience was excluded because tacrolimus was routinely given to those patients during the period of the 5-year case accrual. Nevertheless, 3.2% of the patients at other UNOS centers were treated with this drug (2.5% of the 8,111 African-Americans and 3.4% of the 23,180 “all others”). The remaining 96.8% had cyclosporine-based therapy.
Donor and recipient serologic typing of the HLA-A, -B, and -DR loci was routinely obtained throughout the period of study. The degree of incompatibility was expressed in each case as zero to six HLA mismatches. It has been reported (8) and was confirmed herein (data not shown) that such results accurately reflect the compatibility expressed by the six-to-zero HLA match scale. As reported in detail elsewhere (7), the relationship between the level of HLA mismatch and rate of graft survival was assessed with Cox proportional hazards regression modeling (program 2L of the BMDP package [9]). Half-lives for kidneys still surviving at 1 year were estimated with both with the Cox regression method (see [7]) and with the conventional method that takes into account only actual data from 1 year onward (10). In Figure 1, the results with the latter method are given in parentheses.
Figure 1.
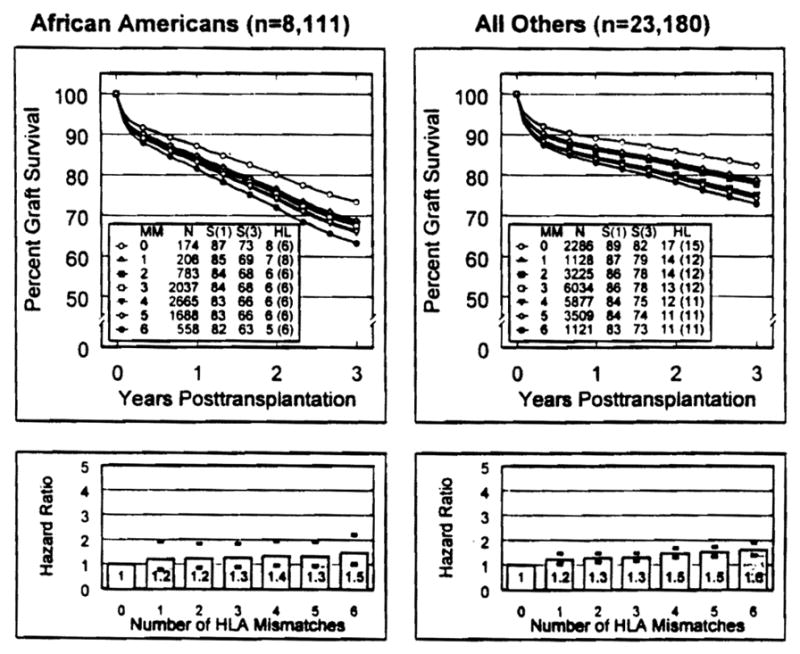
Graft survival and calculations of hazard ratios (HR equivalent to relative risk) over the first 3 posttransplant years, based on number of HLA mismatches and of African-American (n=8111) and all other primary cadaver kidney recipients reported to the UNOS Scientific Registry (1991–1995). The reference hazard ratio (1.0) was provided by zero mismatch cases. Half-lives (HL) calculated with Cox regression analysis are shown side by side with those calculated by the conventional method (10), which are in parentheses.
Only 174 (2.1%) of the 8,111 African-Americans received a zero mismatched kidney, compared with 9.9% in the 23,180 “all other” population (Table 1). At the other end of the matching scale, an additional 558 African-Americans (6.9%) received a six-antigen (full-house) mismatch. Thus, 91.2% of the African-American recipients were in the one-to-five mismatch spectrum, which also bracketed more than 85% of the “all other” cases (Table 1).
Table 1.
Distribution of HLA mismatchesa
| African-Americans | HLA mismatches | All others |
|---|---|---|
| 174 (2.1%) | 0 | 2286 (9.9%) |
| 206 (2.5%) | 1 | 1128 (4.9%) |
| 783 (9.7%) | 2 | 3225 (13.9%) |
| 2037 (25.1%) | 3 | 6034 (26.0%) |
| 2665 (32.9%) | 4 | 5877 (25.3%) |
| 1688 (20.8%) | 5 | 3509 (15.1%) |
| 558 (6.9%) | 6 | 1211 (4.8%) |
Bold type constitutes 91.2% of African-American recipients and 85.3% of all others.
The graft survival in African-Americans at the 1-year post-transplant milestone was not markedly lower than that of the “all other” population at any of the HLA mismatch levels. More relevant to the primary objective of this study, only a zero mismatch conferred a major benefit (Table 2). One year allograft survival from the top to the bottom of the one-to-five HLA mismatch range varied by less than 2% (Table 2). The lack of a stepwise effect also was evident in the one-to-five mismatch range of the “all other” population, where the 1-year survival did not vary by as much as 3% (Table 2).
Table 2.
% graft survival at 1 and 3 yearsa
| African-Americans (n=8,111) | HLA mismatches | All others (n=23,180) |
|---|---|---|
| 87.1 (73.4) | 0 | 89.2 (82.3) |
| 84.6 (68.7) | 1 | 86.9 (78.7) |
| 84.3 (68.2) | 2 | 86.4 (77.9) |
| 83.9 (67.5) | 3 | 86.2 (77.6) |
| 83.0 (65.9) | 4 | 84.5 (75.0) |
| 83.3 (66.3) | 5 | 84.0 (74.3) |
| 81.5 (63.2) | 6 | 83.0 (72.9) |
Bold type constitutes 91.2% of African-American recipients and 85.3% of all others. Numbers in parentheses indicate 3-year survival rate (%).
By 3 years, graft survival in African-Americans had become inferior to that of “all others” (Table 2). However, because survival declined by approximately 10% at every level of HLA compatibility, including zero mismatches, the difference in 3-year graft survival all the way from one to five mismatches was only 2.4%, with reversal in order of the four and five HLA mismatched tiers. The pattern of results in the “all other” recipient population (Table 2) was essentially the same.
Between 1 and 3 years, there was very little divergence of survival in the various categories of HLA mismatch within the African-American population. Instead, the principal and relatively minor separation of curves had already occurred by the end of the first year at all levels of HLA mismatch (Table 2). Although the percentages were slightly different in the 23,180 “all other” cases, the graded HLA effect also was modest. Of interest, when half-lives were calculated using only actual data from 1 year onward (as opposed to the Cox regression prediction), the half-lives of zero mismatched kidneys in African-American recipients were the same as those with two to six mismatches (Fig. 1), which is different than in the “all other” population.
In Figure 1, the hazard ratio (or relative risk) over the first 3 years with various degrees of mismatch in African-Americans (left) or in all others (right) was calculated using the zero HLA mismatch as the reference standard of 1.0. The principal adverse effect came with the first mismatch, which for the African-Americans increased the relative risk of graft loss within 3 years to a modest 1.2 years. However, the relative risk only increased further to 1.3 years all the way from one to five mismatches. For the “all other” population (Fig. 1, right), the relative risk between one and five mismatches rose from 1.2 to 1.5.
UNOS has promoted trials of matching cross-reactive antigen groups (the so-called CREGs or public determinants) with the contention that this can be more discriminating as well as more equitable than conventional HLA matching for African-Americans (11, 12). We have reported elsewhere on the CREG match effect in the 31,291 UNOS cases (7), using the computer program of Takemoto et al. (11) to convert the conventional HLA phenotypes to CREGs. The results (see [7] for details) suggested that CREG-matched patients (particularly in African-Americans), who have only one HLA mismatch, may have a higher graft survival at 3 years than CREG-mismatched patients at this HLA tier. This was not true of CREG matches culled from two to four HLA incompatibility tiers (7).
Any enthusiasm generated by the CREG match findings in the 1-HLA mismatch category is dampened by an assessment of the distribution profile (Table 3). Because CREG matching is directly derived from HLA phenotypes, the 2460 zero HLA mismatched UNOS cases were by definition also CREG matched (a 100% yield). With the succession from one to four HLA mismatches, the CREG match yield fell to 35%, 10%, 2.5%, and less than 1% in these respective tiers. There were no CREG matches in the five and six HLA mismatch categories. The overall yield of CREG matches from the one to five HLA populations in which 90% of the UNOS recipients fell was only 3.6%. These CREG-matched organs went to only 3.2% of the 7,937 African-Americans who did not get a zero HLA mismatched kidney and to 4.3% of the comparable 20,894 “all others” (Table 4).
Table 3.
CREG matched cases (31,291)a
| HLA mismatch | CREG match/mismatch | % |
|---|---|---|
| 0 | 2460/2460 | 100 |
| 1 | 471/1334 | 35.3 |
| 2 | 416/4008 | 10.4 |
| 3 | 206/8071 | 2.6 |
| 4 | 57/8542 | 0.7 |
| 5 | 0/5197 | 0 |
| 6 | 0/1679 | 0 |
Bold type indicates HLA-defined tiers in which 91.2% of African-American and 85.3% of all other recipients are placed (UNOS 1991–1995). The CREG match yield was 1150 (3.6%).
Table 4.
CREG-matched cases in different HLA mismatch tiers
| African-American | HLA mismatches | All others |
|---|---|---|
| 174/174 (100%) | 0 | 2286/2286 (100%) |
| 81/206 (39.3%) | 1 | 390/1128 (34.6%) |
| 172/5485 (3.1%) | 2–4 | 507/15136 (3.3%) |
| 0/2246 (0%) | 5,6 | 0/6034 (0%) |
| 253/7937 (3.2%)a | 897/20894 (4.3%)a |
CREG match yield other than zero HLA matches.
In conclusion, HLA matching except when there is zero HLA-A, -B, and -DR incompatibility has had even less influence on short or long term primary cadaver kidney survival in African-Americans than the minimal effect in the non-African-American population.
Footnotes
This work was supported by project grant DK 29961 from the National Institutes of Health, Bethesda, MD.
Abbreviations: CREG, cross-reactive antigen group; UNOS, United Network for Organ Sharing.
References
- 1.Butkus DE, Meydrech EF, Raje SR. Racial difference in the survival of cadaveric renal allografts: overriding effect of HLA matching and socioeconomic factors. N Engl J Med. 1992;327:840. doi: 10.1056/NEJM199209173271203. [DOI] [PubMed] [Google Scholar]
- 2.Katznelson S, Gjertson DW, Cecka JM. The effect of race and ethnicity on kidney allograft outcome. In: Cecka JM, Terasaki PI, editors. Clinical transplants 1994. Los Angeles: UCLA Tissue Typing Laboratory; 1995. p. 379. [PubMed] [Google Scholar]
- 3.Opelz G, Engelmann A. Effect of HLA matching in cyclosporine-treated black kidney transplant recipients. Transplant Proc. 1989;21:3881. [PubMed] [Google Scholar]
- 4.Cecka JM, Gjertson DW, Cho Y, Terasaki PI. HLA polymorphisms, ethnicity, and graft survival: United Network for Organ Sharing. Transplant Proc. 1993;25:2446. [PubMed] [Google Scholar]
- 5.Chertow GM, Milford EL. Poorer graft survival in African-American transplant recipients cannot be explained by HLA matching. Adv Renal Replacement Ther. 1997;M4:40. doi: 10.1016/s1073-4449(97)70015-3. [DOI] [PubMed] [Google Scholar]
- 6.Gaston RS. Factors affecting renal allograft survival in African-American. Blood Purif. 1996;14:327. doi: 10.1159/000170281. [DOI] [PubMed] [Google Scholar]
- 7.Starzl TE, Eliasziw M, Gjertson D, et al. HLA and cross-reactive antigen group (GREG) matching for cadaver kidney allocation. Transplantation. 1997;64:983. doi: 10.1097/00007890-199710150-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou YC, Cecka JM. Effect of HLA matching on renal transplant survival. In: Cecka JM, Terasaki PI, editors. Clinical transplants 1993. Los Angeles: UCLA Tissue Typing Laboratory; 1994. p. 499. [PubMed] [Google Scholar]
- 9.Dixon WJ, Brown MB, Engelman L, Jennrich RI. BMDP statistical software. Berkeley, CA: University of California Press; 1990. p. 769. [Google Scholar]
- 10.Opelz G, Mickey MR, Terasaki PI. Calculations of long-term graft and patient survival in human kidney transplantation. Transplant Proc. 1987;9:27. [PubMed] [Google Scholar]
- 11.Takemoto S, Terasaki PI, Gjertson DW, Cecka JM. Equitable allocation of HLA-compatible kidneys for local pools and for minorities. N Engl J Med. 1994;331:760. doi: 10.1056/NEJM199409223311202. [DOI] [PubMed] [Google Scholar]
- 12.Thompson JS, Thacker LR. CREG matching for first cadaveric kidney transplants (TNX) performed by SEOPF centers between October 1987 and September 1995. Clin Transplant. 1996;10:586. [PubMed] [Google Scholar]


