Abstract
A retrospective review of 982 patients treated for basal cell carcinoma (BCC) was conducted over a period of 8 years from 1996 to 2004. Of these patients, 16 presented a margin involvement. Two cohorts of patients with involved margin were identified: the group whose basal cell carcinoma was re-excised, and the “wait and see” group. Both sets of results obtained were compared, and then matched with recent international literature reviews. Reexcision is our current practice for incompletely excised tumor. However during the period examined only 36 patients of 116 with margin involvement, proceeded to re-excision, and of the remaining 80 patients just 39 were followed-up. The others were missed mainly because of the difficulty of attending follow-up consultations because of advanced age, poor general conditions, and unavailability of transport facilities. On the basis of several points, including a high number of residual tumors detected in the re-excised patients, and difficulty in maintaining diligent follow-up in the “wait and see” group, we stress the importance of considering an early re-excision in case of margin involvement (focal, lateral, or deep), to avoid a significant risk of recurrence. In this study 16 patients out of 39 in the “wait and see” group had recurrences over 8 years of follow-up; a significant number of recurrences was observed after 5 years. We therefore reserve a clinical follow-up only for patients in whom poor general health dissuades us from re-operation.
Keywords: basal cell carcinoma, excise, guidelines, tumor
Introduction
Although the basal cell carcinoma is one of the most common lesion treated by the plastic surgeon, there is a quantitative argument in the literature, about the correct treatment of the incompletely excised tumor.
Those favoring the “wait and see” method pointed out that only a minority of patients will develop recurrent disease and, if follow-up is diligent, supplementary treatment at that stage will keep the disease under control (Gooding et al 1965; Casson 1980; Huynh and Veness 2002; Wilson et al 2004; Wettstein et al 2006; Rogalski et al 2007).
Those favoring immediate re-excision considered any recurrence rate unacceptable, and thus the need for more radical surgery to control recurrent disease (Shanoff et al 1967; Koplin and Zarem 1980).
The purpose of this study is to compare the outcomes obtained by re-excision of the lesions with those of the “wait and see” group, as well as to match both these results with statistical data from the international literature.
Materials and methods
In our department, cases treated for basal cell carcinoma over a period of 8 years from 1996 to 2004 were analyzed. We compared the outcomes obtained by re-excision of the tumor with those of the “wait and see” group, and matched both these results with recent international literature reviews (Berlin et al 2002; Bisson et al 2002; Lalla et al 2003).
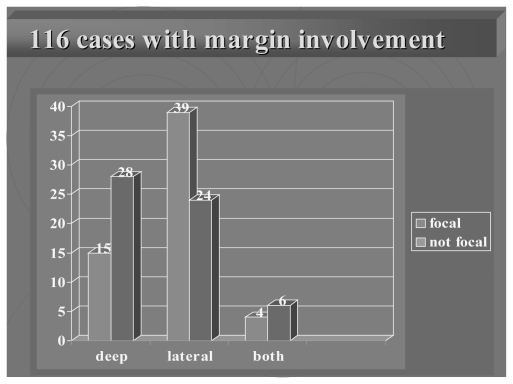
In accordance with statistical data from international literature and on the basis of the margin involvement (lateral or deep), we divided the incompletely excised tumors into two subgroups (Figure. 1). Collaboration with the histologist in our section helped us introduce two further concepts: “focal involvement” of the tumor margin and tumor “in close proximity” to the margin of excision.
Figure 1.
116 cases with margin involvement.
The former included the involvement of a portion of the lateral or deep margin, recording precisely the position, using a watch orientation. The latter concept meant margin involvement at less than 1 mm.
Moreover we evaluated the presence of residual tumor cells at the histological review.
During this study period we operated on 982 patients with basal cell carcinoma; 866 were reported as completely excised, of which 40 were in close proximity (less than 1 mm from the free margin of the tumor), while 116 had margin involvement.
Although re-excision was the treatment of choice, and our current practice for incompletely excised tumor, during the period examined only 36 patients out of 116 with margin involvement proceeded to re-excision. Of the remaining 80 patients just 39 were followed up from the “wait and see” group. The loss of patients was due to advanced age, poor general conditions, and unavailability of transport facilities.
Results
In our statistical investigation only one of the 40 patients with residual tumor in close proximity (less than 1 mm), reported a recurrence during 8 years of follow-up.
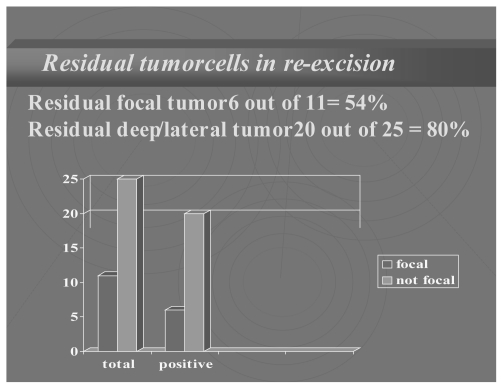
Of the 36 patients who proceeded to further re-excision, 26 (72%) revealed residual tumor.
In particular, of the 11 patients re-excised with focal margin involvement, 6 showed residual tumor in the specimen; of the 25 patients with lateral and deep margin involvement, 20 contained residual tumor at histological review (Figure 2).
Figure 2.
Residual tumor cells in re-excision.
All these patients were re-excised within a period of 4 weeks from the diagnosis; the pathology report and the surgical margin of visually normal skin was 2–3 mm.
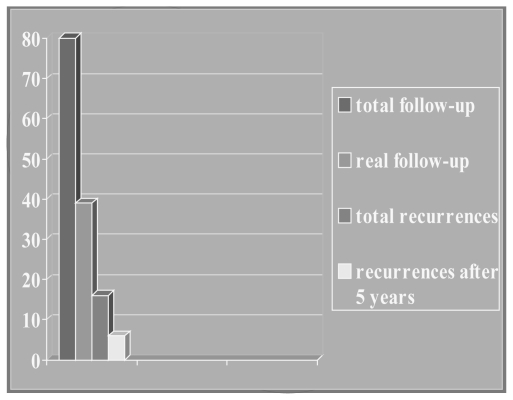
The “wait and see” group showed 16 recurrences out of 39 patients (41%) during 8 years of follow-up; a significant number of recurrences was observed after 5 years of follow-up (6 out of 16 cases = 37,5% with deep margin involvement; Figure 3).
Figure 3.
However it is necessary to point out that only 39 of 80 patients (the “wait and see” group) were kept under observation with continuous follow-up.
Discussion
The purpose of our study was to evaluate:
How many patients among the 40 “in close proximity” developed recurrent disease;
How many patients among the 36 re-excised showed residual tumor at histological review;
How many patients among the “wait and see” group developed recurrent disease;
Duration of follow-up.
Among the 40 patients with tumor “in close proximity” (less than 1 mm), only one showed a recurrence after 6 years of follow-up.
In this particular case, the tumor involved the inner canthus, where there is usually a high rate of recurrence (Shanoff et al 1967).
Griffiths (1999) examined all re-excised BCC specimens from lesions with incompletely excised margins at first surgery, to establish the percentage of residual tumor cells at histological review. He found that 54% of scar specimens showed residual tumor upon histological examination, while our investigation reported 72%.
Our data collected from the “wait and see” group showed 41% of recurrences, over a maximum period of 8 years of follow-up, in accordance with international literature (Rowe et al 1989; Griffiths 1999).
In contrast with previous literature (Silverman et al 1992), which advocated as sufficient a maximum period of 5 years of follow-up, we reported recurrences even after 5 years.
The 5-year probability of tumor recurrence was reported in the literature as 17% when the lateral margin was involved, and 33% for the deep margin (Liu et al 1991).
In conclusion, the clear margin of the histological specimen, including those “in close proximity”, represented a safe index for remaining relapse free, while margin involvement (including focal involvement), exposed a significant risk of recurrence and justified immediate re-excision.
This re-excision must be performed as soon as possible in order to avoid an incorrect diagnosis between recurrence and scar.
Koplin and Zarem (1980) recommended immediate reexcision of all lesions with positive margins as soon as the wounds were adequately healed.
We therefore recommend, in accordance with Koplin and Zarem (1980), immediate re-excision of all lesions with positive margins.
These criteria are confirmed by some investigators, who found a recurrence rate as high as 67% without distinguishing between lateral and deep margin (Shanoff et al 1967).
Other authors (Liu et al 1991) showed that of the “wait and see” group, only a minority of patients with incompletely excised BCC developed recurrent disease, where the followup was continuous and diligent. In this case they performed a re-excision only on patients with clinical evidence of recurrent disease.
In our experience we had remarkable difficulty in maintaining a diligent follow-up, due to poor attendance, mainly as a result of advanced age, poor general conditions, and lack of transport facilities.
We also experienced difficulty in discriminating between scar and tumor.
Conclusion
The statistical data of our retrospective study have strengthened our belief that histologically incomplete BCC should be re-excised.
The essential points that confirm this belief are:
The high number of residual tumors at histological review (72%);
Difficulty in maintaining diligent follow-up;
Possibility of finding recurrence after 5 years of follow-up (in particular on the deep margin);
The need for more destructive surgery, than immediate re-excision;
Possible diagnostic error between recurrence and scar;
It is important to note that the percentage of recurrence in the “wait and see” group (41%), in accordance with the international literature (Dellon et al 1985), was obtained on the basis of a low number of checks (39 out of 80 patients with regular follow-up), owing to the problem mentioned in point two. Moreover we observed that a clear margin in the histological specimen, including those “in close proximity”, represented a safe index of remaining relapse free, while margin involvement (including focal), exposed a significant risk of recurrence and justified immediate re-excision.
We therefore reserve a clinic follow-up only for patients whose poor general health dissuades us from re-operation.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- Berlin J, Katz KH, Helm KF. The significance of tumor persistence after incompletely excision of basal cell carcinoma. J Am Acad Dermatol. 2002;46:549–53. doi: 10.1067/mjd.2002.117733. [DOI] [PubMed] [Google Scholar]
- Bisson MA, Dunkin CS, Survana SK. Do plastic surgeons resect basal cell carcinomas too widely? A prospective study comparing surgical and histological margins. Br J Plast Surg. 2002;55:293–7. doi: 10.1054/bjps.2002.3829. [DOI] [PubMed] [Google Scholar]
- Casson P. Basal cell carcinoma. Clin Plast Surg. 1980;7:301–11. [PubMed] [Google Scholar]
- Dellon AL. Histologic study of recurrent basal cell carcinoma. Plast Reconstr Surg. 1985;75:853–59. doi: 10.1097/00006534-198506000-00017. [DOI] [PubMed] [Google Scholar]
- Dellon AL, DeSilva S, Connolly M, et al. Prediction of recurrence incompletely excised basal cell carcinoma. Plast Reconstr Surg. 1985;75:860–71. doi: 10.1097/00006534-198506000-00018. [DOI] [PubMed] [Google Scholar]
- Dixon AY, Lee SH, McGregor DH. Factors predictive of recurrence of basal cell carcinoma. Am J Dermatopathol. 1989;11:222–32. doi: 10.1097/00000372-198906000-00005. [DOI] [PubMed] [Google Scholar]
- Gooding CA, White G, Yatsuhashi M. Significance of marginal extention in excised basal cell carcinoma. New Engl J Med. 1965;273:923–4. doi: 10.1056/NEJM196510212731708. [DOI] [PubMed] [Google Scholar]
- Griffiths RW. Audit of histologically incompletely excised basal cell carcinomas: recommendations for management by re-excision. Br J Surg. 1999;52:24–8. doi: 10.1054/bjps.1998.3018. [DOI] [PubMed] [Google Scholar]
- Huynh NT, Veness MJ. Basal cell carcinoma of the lip treated with radiotherapy. Australas J Dermatol. 2002;43:15–19. doi: 10.1046/j.1440-0960.2002.00557.x. [DOI] [PubMed] [Google Scholar]
- Koplin L, Zarem HA. Recurrence basal cell carcinoma: a review concerning the incidence behavior and management of recurrent basal cell carcinoma, with emphasis on the incompletely excised lesion. Plast Reconstr Surg. 1980;65:656–64. [PubMed] [Google Scholar]
- Lalla R, Brown TL, Griffiths RW. Where to draw the line: the error in marking surgical excision margins defined. Br J Plast Surg. 2003;56:603–6. doi: 10.1016/s0007-1226(03)00203-0. [DOI] [PubMed] [Google Scholar]
- Liu FF, Maki E, Warde P, et al. A management approach to incompletely excised basal cell carcinomas of skin. Int J Radiat Oncol Biol Phys. 1991;20:423–8. doi: 10.1016/0360-3016(91)90052-6. [DOI] [PubMed] [Google Scholar]
- Pascal RR, Hobby LW, Lattes R, et al. Prognosis of incompletely excised versus completely excised basal cell carcinoma. Plast Reconstr Surg. 1968;41:328–32. doi: 10.1097/00006534-196804000-00006. [DOI] [PubMed] [Google Scholar]
- Rogalski C, Kauer F, Simon JC, et al. Meta-analysis of published data on incompletely excised basal cell carcinomas of the ear and nose with introduction of an innovative treatment strategy. J Dtsch Dermatol Ges. 2007;5:118–26. doi: 10.1111/j.1610-0387.2007.06197.x. [DOI] [PubMed] [Google Scholar]
- Rowe D, Carroll RJ, Day CL., Jr Long-term recurrence rates in previously untreated (primary) basal cell carcinoma: implications for patient follow-up. J Dermatol Surg Oncol. 1989;15:315–28. doi: 10.1111/j.1524-4725.1989.tb03166.x. [DOI] [PubMed] [Google Scholar]
- Shanoff L, Spira M, Hardy SB. Basal cell carcinoma: a statistical approach to rational management. Plast Reconstr Surg. 1967;39:619–24. [PubMed] [Google Scholar]
- Silverman MK, Kopf AW, Grin CM, et al. Recurrence rates treated basal cell carcinomas. Part 1: Overview. J Dermatol Surg Oncol. 1991a;17:713–18. doi: 10.1111/j.1524-4725.1991.tb03424.x. [DOI] [PubMed] [Google Scholar]
- Silverman MK, Kopf AW, Grin CM, et al. Recurrence rates treated basal cell carcinomas. Part 2: Curettage-electrodessication. J Dermatol Surg Oncol. 1991b;17:720–18. doi: 10.1111/j.1524-4725.1991.tb03425.x. [DOI] [PubMed] [Google Scholar]
- Silverman MK, Kopf AW, Bart RS, et al. Recurrence rates treated basal cell carcinomas. Part 3: Surgical excision. J Dermatol Surg Oncol. 1992;18:471–6. doi: 10.1111/j.1524-4725.1992.tb03307.x. [DOI] [PubMed] [Google Scholar]
- Taylor GA, Barisoni D. Ten years’ experience in the surgical treatment of basal cell carcinoma. A study of factors associated with recurrence. Br J Surg. 1973;60:522–25. doi: 10.1002/bjs.1800600706. [DOI] [PubMed] [Google Scholar]
- Wettstein R, Kalbermatten DF, Rieger U, et al. High magnification assessment improves complete resection of facial tumors. Ann Plast Surg. 2006;57:517–20. doi: 10.1097/01.sap.0000226930.67941.7f. [DOI] [PubMed] [Google Scholar]
- Wilson AW, Howsam G, Santhanam V, et al. Surgical management of incompletely excised basal cell carcinomas of the head and neck. Br J Oral Maxillofacial Surg. 2004;42:311–14. doi: 10.1016/j.bjoms.2004.02.030. [DOI] [PubMed] [Google Scholar]