We describe a patient with a background of unexplained recurrent miscarriages who was diagnosed with Wilson's disease and subsequently gave birth to two children after treatment was commenced.
Introduction
Recurrent miscarriage is a less recognized feature of Wilson's disease and adequate treatment can alter the outcome of pregnancies favourably. Wilson's disease is a recessively inherited disorder of copper metabolism due to mutations in the ATP7B gene, which encodes for a copper-transporting P-type ATPase. Recurrent miscarriage is a complication of untreated Wilson's disease. It has been reported that miscarriages can predate neurological symptoms,1 and treatment with copper chelation improves the rate of successful pregnancies.1,2
Case report
In May 2007, a 41-year-old woman of Pakistani origin presented with a three-year history of tremor. She had two other siblings affected with Wilson's disease, and their parents were consanguineous. She presented late because she moved between cities frequently. On examination, she had very obvious Kayser-Fleischer rings in both eyes (Figure 1). She had action tremor of both upper limbs and an unsteady ataxic gait.
Figure 1.
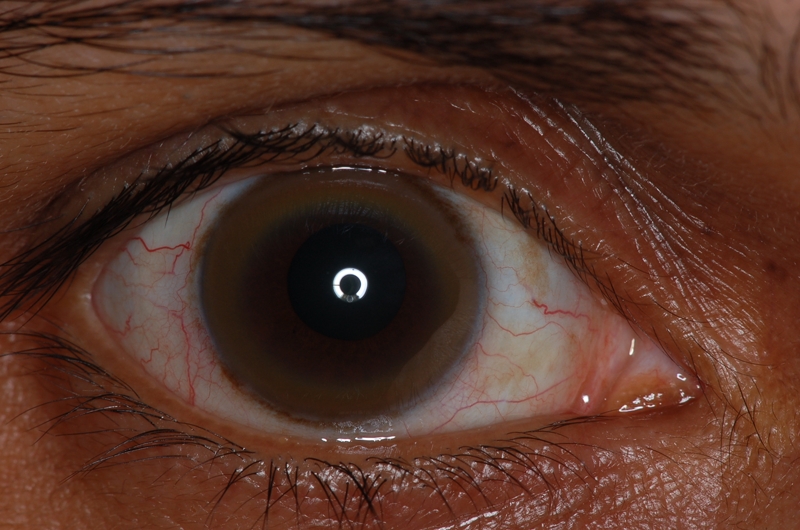
Kayser-Fleischer ring in the right eye of our patient
Investigations confirmed the strong clinical suspicion of Wilson's disease. Serum copper was 0.6 mg/L (0.7–1.6 mg/L). Serum caeruloplasmin was 0.13 g/L (0.2–0.5 g/L). Urinary copper excretion was 124 µg/24 hr (<50 µg/24 hr). All other serological tests including liver enzymes were normal. Magnetic resonance imaging of the brain showed diffuse abnormal high signal in both thalami, cerebral peduncles, midbrain and pons consistent with Wilson's disease. Gene sequencing of ATP7B gene showed that she was heterozygous for c.3008 C > T; p.Ala1003Val novel amino acid change.
However, her other main clinical problem was recurrent miscarriages. Up to the age of 34 years, corresponding to four years prior to onset of neurological symptoms, she had 10 miscarriages, all in the first trimester. Her menarche occurred aged 15, and her first pregnancy and miscarriage aged 18. Previous investigations including tests for antiphospholipid syndrome and exploratory laparoscopy and hysteroscopy revealed no causes for her miscarriages.
Penicillamine was commenced in June 2007. She responded neurologically but compliance was poor due to side-effects and anxieties of teratogenicity. She was found pregnant six months into suboptimal therapy, her first on treatment, at 16 weeks gestation when she stopped treatment herself. She had cervical incompetence diagnosed at 19 weeks, likely to be caused by repeated endoscopic removal of products of reception for her previous miscarriages. She gave birth to a male infant of 574 g at 24 weeks gestation by emergency Caesarean section due to spontaneous rupture of membrane and cord prolapse. He died unexpectedly aged eight weeks due to aspiration pneumonia. An autopsy was declined, and placental copper was 0.33 µg/g (0.2–0.5 µg/g). She became pregnant for the 12th time in March 2009, and was admitted to hospital under the obstetrician for strict bed rest to avoid complications from cervical incompetence. She remained fully compliant with medication (penicillamine 1 g/day, zinc acetate 150 mg/day, pyridoxine 50 mg/week) throughout this pregnancy and neurologically there were minimal cerebellar signs. She delivered a healthy female infant of 2430 g in July 2009 at 34 weeks by elective Caesarean section. She is developing normally and placental copper was 0.15 µg/g. She soon became pregnant for the 13th time, and the outcome was awaited.
Discussion
Recurrent miscarriage is defined as the occurrence of three or more pregnancy losses before 20 weeks of gestation and most cases are idiopathic or multifactorial.3 It affects 1% of all conceiving couples and 15% of clinically recognized pregnancies are lost before 20 weeks. It is common in untreated Wilson's disease according to a study in India (30%), which followed a cohort of 16 female Wilson's disease patients.4 However, more than half of the pregnancies in untreated patients went full term with no complications, suggesting pregnancy outcome was multifactorial. Recent laboratory work showed that the gene product of ATP7B has the role of transporting copper from the placenta to the maternal circulation,5 implying that its normal functioning prevents copper overload in the fetus. Thus we hypothesize that with ATP7B dysfunction, excess copper remains in the fetus due to defective clearance mechanism in the first trimester, causing free radical formation, oxidative damage and eventually fetal loss. This is supported by report of copper accumulation in placenta and fetus in untreated Wilson's disease.6
This case highlights the importance of considering Wilson's disease as a cause of recurrent miscarriage. It is an important differential diagnosis to antiphospholipid syndrome as far as pregnancy issues are concerned, especially in neurology practice as both conditions are readily treatable. Although multiple factors were implicated in our case, full treatment for Wilson's disease made a critical difference in pregnancy outcome, together with dedicated obstetric care. However, there is currently no consensus on treatment regimen for Wilson's disease during pregnancy and more focused studies in this area would improve treatment selection. It is worth enquiring for a personal and family history of early miscarriage in suspected Wilson's disease as this may prompt earlier diagnosis. Further, for female patients of child-bearing age, they should be counselled to receive effective treatment before planning pregnancy. Early involvement of obstetric care is also recommended to avoid similar problems to our patient's unfortunate neonatal loss.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written informed consent to publication has been obtained from the patient or next of kin
Guarantor
DJN
Contributorship
The patient in this case report is under the care of DJN who had the original idea of this report and contributed to the relevant literature search; TY was supervised by DJN, performed a large proportion of the relevant literature search and wrote and revised the report; GD was the obstetrician in charge of the patient and contributed expert opinion in her field; MM was responsible for harvesting and performing analysis on placental tissues from the patient, also providing expert opinion in his field
Acknowledgements
None
Reviewer
Sadia Malick
References
- 1.Schagen van Leeuwen JH, Christiaens GC, Hoogenraad TU Recurrent abortion and the diagnosis of Wilson disease. Obstet Gynecol 1991;78:547–9 [PubMed] [Google Scholar]
- 2.Walshe JM The management of pregnancy in Wilson's disease treated with trientine. Q J Med 1986;58:81–7 [PubMed] [Google Scholar]
- 3.Stirrat GM Recurrent miscarriage. Lancet 1990;336:673–5 [DOI] [PubMed] [Google Scholar]
- 4.Sinha S, Taly AB, Prashanth LK, Arunodaya GR, Swamy HS Successful pregnancies and abortions in symptomatic and asymptomatic Wilson's disease. J Neurol Sci 2004;217:37–40 [DOI] [PubMed] [Google Scholar]
- 5.Hardman B, Michalczyk A, Greenough M, Camakaris J, Mercer JFB, Ackland ML Distinct functional roles for the Menkes and Wilson copper translocating P-type ATPases in human placental cells. Cell Physiol Biochem 2007;20:1073–84 [DOI] [PubMed] [Google Scholar]
- 6.Oga M, Matsui N, Anai T, Yoshimatsu J, Inoue I, Miyakawa I Copper deposition of the fetus and placenta in a patient with untreated Wilson's Disease. Am J Obstet Gynecol 1993;169:196–8 [DOI] [PubMed] [Google Scholar]


