Abstract
A long-standing challenge for scientific and clinical work on suicidal behavior is that people often are motivated to deny or conceal suicidal thoughts. We proposed that people considering suicide would possess an objectively measurable attentional bias toward suicide-related stimuli, and that this bias would predict future suicidal behavior. Participants were 124 adults presenting to a psychiatric emergency department who were administered a modified emotional Stroop task and followed for six months. Suicide attempters showed an attentional bias toward suicide-related words relative to neutral words, and this bias was strongest among those who had made a more recent attempt. Importantly, this suicide-specific attentional bias predicted which people made a suicide attempt over the next six months, above and beyond other clinical predictors. Attentional bias toward more general negatively-valenced words did not predict any suicide-related outcomes, supporting the specificity of the observed effect. These results suggest that suicide-specific attentional bias can serve as a behavioral marker for suicidal risk, and ultimately improve scientific and clinical work on suicide-related outcomes.
Keywords: suicide, attentional bias, Stroop task, prediction
Suicide is a leading cause of death in the United States and worldwide (Nock et al., 2008). Mortality data indicate that one person dies by suicide somewhere around the world every 40 seconds (Krug, Dahlberg, Mercy, Zwi, & Lozano, 2002). The high rate of suicide results in part from the fact that assessment primarily depends on people’s explicit self-report, which is unreliable because people often are motivated to deny their suicidal thoughts (Busch, Fawcett, & Jacobs, 2003). Developing more objective and scientifically rigorous ways of determining who is at risk for suicidal behavior is essential for both scientific and clinical work addressing this devastating behavior problem.
The National Institute of Mental Health (NIMH) Strategic Plan lists as one of its primary objectives the identification of biological and behavioral markers associated with mental disorders and clinical behavior problems (NIMH, 2009). Behavioral markers are objectively observable, behavior-based factors that indicate some underlying disease process and can aid in case identification, assessment, and treatment (NIMH, 2009; Biomarkers Definitions Working Group, 2001). Impressive progress has been made toward identifying biological markers associated with mental disorders (e.g., Kemp et al., 2009; Sawa & Cascella, 2009; Su et al., 2009); however, parallel research on behavioral markers has been lacking. Although biomarkers such as genetic mutations or neurotransmitter dysfunction undoubtedly influence the development of different psychological traits (e.g., impulsiveness), they are unlikely to accurately predict specific behavioral outcomes such as suicide attempt.
Recent advances in psychological science have made it possible to objectively measure psychological characteristics that may be associated with specific thoughts, feelings, and behaviors. For instance, Nock and colleagues recently showed that people who engage in nonsuicidal self-injury and suicidal behaviors show an implicit identification with self-injurious behavior on an objective, performance-based test (i.e., faster response when pairing “Me” with “Cutting” vs. “Me” with “Not Cutting”; Nock & Banaji, 2007a, 2007b). Moreover, performance on a death-specific version (i.e., faster response pairing “Me” with “Death) of this test predicts subsequent suicide attempts beyond common clinical predictors (Nock et al., 2010), suggesting that implicit death- or suicide-specific cognition can serve as a behavioral marker for suicide risk.1 Additional research aimed at identifying behavioral markers for suicide attempt is needed to improve the ability to better detect and predict suicidal behavior.
Attentional bias,2 which involves selective allocation of attentional resources toward specific aspects of stimuli, is a cognitive process that may further help to explain and predict suicidal behaviors. Cognitive theories of emotional disorders propose that distinct attentional biases—along with broader cognitive structures influencing all aspects of information-processing (i.e., schemas)—increase vulnerability toward particular disorders (Beck, 1976; Beck, Emery, & Greenberg, 2005). Empirical findings can elucidate pathways through which this may occur, and earlier research has suggested that attentional bias toward particular disorder-related stimuli indicates accessibility of the respective disorder-relevant thoughts. For example, studies using the emotional Stroop task (Williams, Mathews, & MacLeod, 1996) have demonstrated that depression is associated with attentional bias toward depressed-content words. Anxiety- (Foa, Feske, Murdock, Kozak, & McCarthy, 1991; McNally, Kaspi, Riemann, & Zeitlin, 1990; Teachman, Smith-Janik, & Saporito, 2007) and substance use-specific (Cox, Fadardi, & Pothos, 2006) Stroop effects have also received empirical support.
More recently, attentional bias also has been theorized to play a role in the pathway to suicide. Wenzel and Beck (2008) proposed that suicide-specific attentional bias—in combination with state hopelessness—leads to a fixation on suicide as the sole escape solution and ultimately to a suicide attempt. Measuring attentional bias would be an important initial step toward testing this theory and indirectly assessing the likelihood of future suicide attempt.
To date, only two studies have examined attentional bias toward suicide-related words. Williams and Broadbent (1986) found that recent suicide attempters took longer to name the color of suicide-related words relative to neutral words compared to control groups. Building on this work, Becker and colleagues (1999) showed that past year suicide attempters took significantly longer to name the color of suicide-related words than both neutral and generally negative words, whereas there were no differences in latencies among control participants. This finding suggests that suicide attempters attend specifically toward information relevant to suicidal thoughts and behaviors.
Despite initial support for the presence of suicide-specific attentional bias, several key issues remain unaddressed. First, it is not known whether suicide-specific attentional bias is associated with likelihood of future suicide attempt. Cognitive theories of suicide propose this relation (Wenzel & Beck, 2008); however, earlier work has been entirely cross-sectional in nature. Second, prior studies have assessed only bivariate relations between attentional bias and suicide attempt, as well as partial correlations within groups of suicide attempters. As a result it is not known whether attempters and non-attempters demonstrate different degrees of attentional bias in the presence of other risk factors for suicide (e.g., mood disorder).
The current study was designed to address these limitations and to advance the understanding and prediction of suicidal behavior in two ways. First, we hypothesized that people who had made a suicide attempt would show an attentional bias toward suicide-related words. If present, we expected that this bias would be strongest among those who made the most recent suicide attempts. Second, we hypothesized that this suicide-specific attentional bias would prospectively predict which patients will make a suicide attempt during the next six months, above and beyond clinician prediction and known risk factors. In order to determine the specificity of these effects, we examined attentional bias toward both suicide-related and negatively-valenced (i.e., unrelated to suicide) stimuli relative to neutral stimuli.
Method
Participants
Participants were 124 adults presenting to a psychiatric emergency department (ED). All participants were drawn from a larger sample of 198 adults seeking acute psychiatric care. Of the 198 adults, 143 were administered the modified Stroop task. Fifty-five people did not complete the Stroop task due to various reasons (e.g., initial presence of cognitive impairment, discharge from hospital). Of the 143 who completed the Stroop, 12 were excluded as outliers (described below) and 7 were excluded from analyses due to unreliable reports of suicidal behavior at each time point (e.g., repeatedly changing responses as to whether or not he/she has a history of suicide). There were no significant differences between those included versus excluded from the study on sex, race/ethnicity, or types of Axis I diagnoses, χ2s(1)=0.00-3.69, ps=.06-.99, Φs=.00-.14, or degree of Axis I disorder comorbidity, t(193)=0.8, p=.45, d=0.11. Those included were slightly younger (M=34.5, SD=11.8) than those excluded (M=38.7, SD=12.5), t(193)=2.3, p=.02, d=0.33. Sample size for the current study provides sufficient statistical power (.78-.99, with α=.05, two-tailed tests) to detect medium-large effects, respectively.
Measures
Attentional bias
Attentional bias toward suicide-related and negatively-valenced stimuli was measured using a modified Stroop task (Stroop, 1935). This performance-based measure records response latencies of how quickly participants identify the color of different words presented on a computer screen. Larger response latencies were interpreted as representing greater interference due to the semantic content of the presented words. In the current study, stimuli for the task were presented and response latencies recorded using Empirisoft DirectRT v2004 software (Jarvis, 2004). Directions presented on the screen at the beginning of the task instructed participants to indicate the color of each presented word as quickly and as accurately as possible. Each trial started with a blank, white screen for four seconds followed by the presentation of a centered “+” for one second. The “+” was then replaced by a blank screen for one second, followed by the word printed in red or blue, which remained on the screen until a response was recorded. Participants were instructed to indicate the color of the words as quickly and as accurately as possible by pressing the red or blue key on the computer keyboard. They first completed eight practice trials, followed by 48 trials. In the critical trials participants were presented with suicide-related words (suicide, dead, funeral), negatively-valenced words (alone, rejected, stupid), and neutral words (museum, paper, engine). Twelve of the 48 test trials also included positive words (happy, success, pleasure); exploratory analyses showed that there was no evidence of an attentional bias toward these positive words. Suicide-related and negatively-valenced words were selected based on prior studies using behavioral measures assessing suicide-related constructs (e.g., Nock et al., 2010), as well as based on general relevance to these clinical topics. They did not significantly differ in length, concreteness, emotionality, or frequency of use in the English language, ts(4)=0.10-0.74, ps=.50-.93, ds=.10-.74. Trials were presented in a new random order to each participant. We calculated interference for suicide-related stimuli (i.e., suicide-specific attentional bias) by subtracting latencies for neutral words from latencies for suicide-related words. Similarly, we calculated interference for negatively-valenced stimuli (i.e., attentional bias toward negative content) by subtracting latencies for neutral words from latencies for negatively-valenced words.
Trials with correct responses were included in the analysis. Trials with response latencies ±2 SD from each participant’s mean response latency were eliminated. Additionally, participants (n=6) for whom the mean response latency was ±2 SD from the mean response latency for all participants were excluded from analysis, as were participants (n=6) for whom the error rate was 2 SD above the error rate for all participants. When compared across all participants, the response latencies for suicide-related (M=788.16 ms), negatively-valenced (M=775.02 ms), and neutral (M=775.96 ms) words did not significantly differ from one another, ps=.14-.93, ds=.03-.40.
Demographic and psychiatric factors
Information on demographic and psychiatric risk factors was collected from participants’ medical records in the ED. We assessed psychiatric risk factors by categorizing Axis I diagnoses according to overall class of disorders and by calculating the total number of current Axis I diagnoses.
History of suicidal behavior
History of suicide attempt was measured using the Self-Injurious Thoughts and Behavior Interview (SITBI; Nock, Holmberg, Photos, & Michel, 2007), which assesses presence, frequency, and other characteristics of a broad range of self-injurious thoughts and behaviors. These characteristics were assessed over time frames of lifetime, past year, past month, and past week. Baseline history of suicide attempt was defined as the presence of at least one suicide attempt in the participant’s life. Recency of suicide attempt was coded using the following values: 0 (never), 1 (lifetime but not in the past year), 2 (past year but not in the past month), 3 (past month but not in the past week), and 4 (past week). History of multiple suicide attempts was also coded (0,1) based on lifetime frequency values of suicide attempt. Nock et al. (2007) reported fair to excellent interrater reliability (κ=1.0), test-retest reliability over a six-month period (κ=.80), and construct validity (κ=.65) of the SITBI suicide attempt subscale. The SITBI was conducted in person at baseline and over the phone at follow-up. To improve detection of follow-up suicide attempts, we reviewed medical records for documentation of whether a participant had returned to the same hospital due to a suicide attempt within six months of the baseline assessment. Reports of follow-up suicide attempt from the SITBI and from medical records demonstrated a high level of agreement (κ=.75). Finally, severity of suicidal ideation at baseline was assessed using the Beck Scale for Suicidal Ideation, a commonly used self-report measure that has shown to have excellent validity and reliability (Beck & Steer, 1991).
Clinician and patient prediction of future suicide attempt
A brief questionnaire was completed by each participant’s primary clinician in the ED (e.g., attending psychiatrist, resident, psychiatry intern, psychology intern). Questionnaire items assessed knowledge of the participant’s history of suicide attempt, as well as the clinician’s prediction of a future suicide attempt within the next six months. The latter was measured using the following question: “Based on your clinical judgment and all that you know of this patient, if untreated, what is the likelihood that this patient will make a suicide attempt in the next 6 months? (0-10, with 0 being no likelihood and 10 being very high likelihood).” Patient prediction of future suicide attempt was assessed in the SITBI using the following question: “On this scale of 0 to 4, what is the likelihood that you will make a suicide attempt in the future?”
Procedure
Consistent with standard clinical care at the study site, after initial evaluation by an ED clinical staff member, patients typically remained in the ED for 1-4+ hours while awaiting further evaluation, transfer to another unit, or discharge from the hospital. During this time, a research team member approached patients and explained the study with permission from the attending psychiatrist. All study participants met inclusion criteria: adult status (≥18 years-old) and presentation to the ED. Individuals were not recruited for the study if there was presence of any factor impairing their ability to effectively participate (e.g., inability to speak or write English fluently, presence of a gross cognitive impairment, presence of extremely agitated or violent behavior). Eligible participants were asked to provide informed consent and were administered baseline measures and the modified Stroop task in the ED. Participants were then interviewed via phone approximately six months following the date of their baseline interview. All procedures were approved by the university and hospital institutional review boards.
Results
Participant Characteristics
Lifetime suicide attempters and non-attempters did not differ significantly on age, sex, race/ethnicity, or presence of most current Axis I disorders (Table 1). There were significantly more cases of mood disorder among suicide attempters than non-attempters. As a result, we statistically controlled for the presence of mood disorder in all subsequent analyses.
Table 1. Characteristics of the Sample.
| Variable | Suicide Attempters (n = 68) |
Non- Attempters (n = 56) |
Test | Effect Size |
|---|---|---|---|---|
| Age in years (M ± SD) | 34.1 ± 10.5 | 35.1 ± 13.2 | t(122) = 0.49 | d = 0.09 |
| Sex (% female) | 42.6 | 35.2 | χ2(1) = 0.62 | Φ = 0.07 |
| Race (%) | ||||
| White | 73.5 | 83.9 | χ2(4) = 3.63 | Φ = 0.17 |
| Black | 14.7 | 8.9 | ||
| Hispanic | 4.4 | 5.4 | ||
| Asian | 4.4 | 1.8 | ||
| Other | 2.9 | 0.0 | ||
| Axis I disorders present (%) | ||||
| Any mood disorder | 85.3 | 62.5 | χ2(1) = 8.51** | Φ = 0.26 |
| Any psychotic disorder | 2.9 | 3.6 | χ2(1) = 0.04 | Φ = −0.02 |
| Any anxiety disorder | 20.6 | 21.4 | χ2(1) = 0.01 | Φ = −0.01 |
| Any impulse-control disorder | 0.0 | 1.8 | χ2(1) = 1.22 | Φ = −0.10 |
| Any eating disorder | 4.4 | 5.4 | χ2(1) = 0.06 | Φ = −0.02 |
| Any substance use disorder | 25.0 | 25.0 | χ2(1) = 0.00 | Φ = 0.00 |
| Any alcohol use disorder | 29.4 | 21.4 | χ2(1) = 1.02 | Φ = 0.09 |
| Any other Axis I disorder | 4.4 | 7.1 | χ2(1) = 0.43 | Φ = −0.06 |
| Number of Axis I disorders (M ± SD) | 1.7 ± 0.9 | 1.5 ± 0.9 | t(122) = 1.43 | d = 0.26 |
p < .01
Attentional Bias and Suicide Attempts
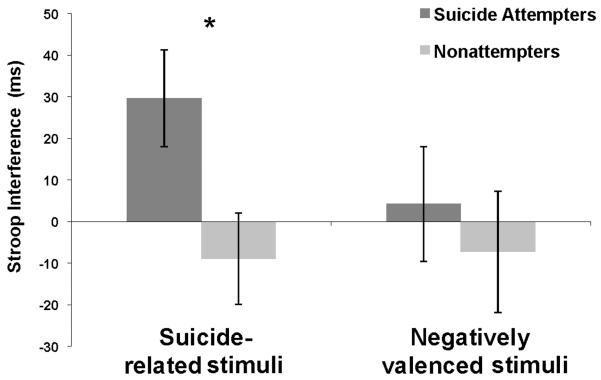
Our first hypothesis was that patients with a history of suicide attempt would show an attentional bias toward suicide-related stimuli but not toward negatively-valenced stimuli relative to psychiatrically distressed control participants. Consistent with this prediction, independent sample t tests revealed that interference for suicide-related words was significantly greater among suicide attempters than non-attempters, t(122)=2.37, p=.02, d=0.43, but no group differences in interference for negatively-valenced words, t(122)=0.57, p=.57, d=0.10 (see Figure 1). Results were unchanged after statistically controlling for the presence of a mood disorder: Interference for suicide-related words was significantly related to suicide attempt (OR=1.01, CI=1.00-1.01, p=.02), whereas interference for negatively-valenced words was not (OR=1.00, CI=0.99-1.01, p=.46). These results indicate that for each one millisecond increase in Stroop performance, there is a 1% increase in the odds of a suicide attempt. Notably, Stroop response latencies for neutral words did not significantly differ between suicide attempters and non-attempters at baseline, t(122)=.19, p=.85, d=.03, or follow-up, t(58)=.34, p=.73, d=.09.
Fig 1.
Suicide Attempters Demonstrate Greater Interference for Suicide-Related Words than Non-Attempters
Note. Error bars represent standard error of the mean. *p<.05
We also hypothesized that attentional bias toward suicide-related stimuli would be significantly associated with recency of suicide attempt, even after controlling for relevant clinical predictors (i.e., mood disorder). Multinomial regression analyses revealed that interference for suicide-related words was related to recency of suicide attempt (R2=.14, Model χ2(8) =16.68, p =.03). Specifically, interference for suicide-related words was associated only with suicide attempt occurring within the past week (versus no history of suicide attempt; OR=1.01, CI=1.00-1.01, p=.03), but not in the past month, past year, or in one’s lifetime beyond the most recent year (ps=.06-.58). Attentional bias toward negatively-valenced words was unrelated to recency of suicide attempt (R2=.09, Model χ2(8)=11.28, p=.19).
Attentional Bias as a Behavioral Marker for Future Suicide Attempt
Our final hypothesis was that attentional bias toward suicide-related stimuli would prospectively predict suicide attempt above and beyond common clinical predictors. These results are based on the 60 participants who completed the six-month follow-up assessment, 10 of whom reported attempting suicide during the six-month period. The 60 follow-up participants were demographically and clinically similar to baseline-only participants, except that there were significantly fewer cases of alcohol use disorder in the follow-up sample, χ2(1)=7.38, p=.01, Φ=−0.24. Baseline and follow-up suicide attempters did not significantly differ in history of multiple attempts as measured at baseline (55% and 60%, respectively, had history of multiple attempts), χ2(1)=0.09, p=.77, Φ=−0.04.
Most importantly, attentional bias toward suicide-related stimuli measured at baseline added incrementally to the prediction of suicide attempts during the follow-up period, even after controlling for commonly used clinical predictors, including: history of mood disorder, history of multiple suicide attempt,3 severity of suicidal thoughts, and both patient and clinician prediction of a future suicide attempt (Table 2). Attentional bias toward negatively-valenced stimuli did not predict follow-up suicide attempt status.
Table 2. Hierarchical Logistic Regression Predicting Suicide Attempt during the 6-Month Follow-Up Period (n=60).
| Variable | b | SE | Wald | OR (95% CI) | R2 |
|---|---|---|---|---|---|
| Step 1 | 0.13 | ||||
| Any mood disorder | 1.31 | 1.12 | 1.38 | 3.72 (0.42-33.20) | |
| Multiple suicide attempts | 1.07 | 0.73 | 2.14 | 2.93 (0.70-12.34) | |
| Step 2 | 0.19 | ||||
| Scale for Suicidal Ideation | 0.05 | 0.05 | 1.28 | 1.05 (0.96-1.15) | |
| Clinician prediction | 0.07 | 0.17 | 0.16 | 1.07 (0.77-1.49) | |
| Patient prediction | 0.18 | 0.96 | 0.04 | 1.20 (0.18-7.84) | |
| Step 3a | 0.19 | ||||
| Attentional bias toward negatively-valenced words | 0.00 | 0.01 | 0.02 | 1.00 (0.99-1.01) | |
| Step 3b | 0.37 | ||||
| Attentional bias toward suicide-related words | 0.02 | 0.01 | 5.40 | 1.02 (1.00-1.03)* |
p < .05
Note. OR = odds ratio; CI = confidence interval
Discussion
One of the greatest barriers to studying suicidal thoughts and behaviors has been the reliance on self-report to assess these constructs. We attempted to overcome this challenge by examining whether suicide attempters show a specific attentional bias toward suicide-related stimuli, and whether this bias can predict subsequent suicidal behavior. Results of this study support our primary hypotheses, by showing that suicide-specific attentional bias was related to history and recency of past attempts, and most importantly that it predicted future suicide attempt above and beyond common clinical predictors. Suicide-specific attentional bias was indeed more strongly associated with suicide attempt than negatively-valenced attentional bias, given that the latter was not related to any suicide-related outcome. Consistent with prior studies (e.g., Becker et al., 1999), even the bivariate relation between suicide attempt history and attentional bias to negatively-valenced words was not significant. This is likely due to the fact that non-attempters in the current study were patients presenting to the psychiatric emergency center who also experienced a substantial degree of distress, albeit not directly from suicide attempt, and therefore demonstrated similar levels of attentional bias to negatively-valenced stimuli as did suicide attempters.
These results provide the first evidence that a suicide-specific attentional bias can serve as a behavioral marker for subsequent suicide attempt. Past studies assessing suicide-specific (Becker et al., 1999; Williams & Broadbent, 1986) and general (e.g., Harkavy-Friedman et al., 2006; Keilp et al., 2008; Malloy-Diniz et al., 2009) attentional bias among suicide attempters have been cross-sectional in nature. In contrast, the current prospective design showed that this attentional bias is not only associated with, but also precedes suicide attempt. This finding is unlikely due to the baseline association between suicide-specific attentional bias and lifetime history of suicide attempts, since: (1) The strength of this attentional bias seemed to vary as a function of how recently a patient had attempted suicide (i.e., likely not stable over time), and (2) It predicted future attempt controlling for baseline history, as discussed below. These findings support Wenzel and Beck’s (2008) cognitive theory of suicide, and suggest that suicide-specific attentional bias possibly accelerates the likelihood of suicide attempt, and that it indeed precedes this outcome. Future work is encouraged to test other aspects of this theory by prospectively examining the effects of suicide-specific attentional bias in the context of hopelessness, and by assessing the potential mediating role of attentional fixation.
The current study also revealed that suicide-specific attentional bias is a behavioral marker of suicide attempt adding predictive value in two ways. First, suicide-specific attentional bias predicts future suicide attempt above and beyond known risk factors, namely, history of mood disorder and suicide attempt, severity of prior suicidal thoughts, and patient and clinician prediction of future suicide attempts. This finding builds on prior work showing bivariate relations between Stroop performance and suicide attempt (e.g., Becker et al., 1999; Keilp et al., 2008; Malloy-Diniz et al., 2009). Statistically controlling for mood disorder rather than sampling for mood disorder (e.g., Malloy-Diniz et al., 2009) allowed us to assess attentional bias in relation to suicide attempt in a more representative clinical sample. These findings thereby provide a more complete understanding of risk factors for suicide attempt.
Second, the finding that suicide-specific attentional bias predicts future suicide attempt above and beyond clinicians’ predictions is especially noteworthy and underscores the value of using objective behavioral measures to predict future behavior. Previous research suggests that an actuarial (i.e., statistical) approach toward predicting human behavior may be just as good, if not more accurate, than clinicians’ predictions (Dawes, 1996). In the case of predicting suicide attempt, an additional challenge is that the information based on which the clinician must predict a patient’s outcome may be deliberately misleading since suicidal patients may be motivated to conceal such intentions to avoid unwanted treatment (Beck & Steer, 1989; Pierce, 1977). Although the current study did not directly test the clinical utility of the “Suicide Stroop task”, this is an important first step toward developing objective tools that can aid in clinical decision-making regarding suicide risk assessment.
These findings should be interpreted in light of several limitations. First, many participants were excluded due to the Stroop scoring criteria, and those included in this study were younger than those excluded. Results based on Stroop performance may therefore be best generalized to younger adult samples. Second, the sample size was relatively small and a number of cases were lost at follow-up. Future studies replicating these effects should include large and clinically diverse samples at both baseline and follow-up. Third, our assessment was somewhat narrow in the current study and did not test whether the identified behavioral marker provides better prediction of suicide attempts than other bio- or behavioral markers. The development of methods for collecting and combining such data represents one of the most important directions for future research in this area. Ultimately, the most accurate understanding and prediction of suicidal behavior will emerge from a synthesis of data from behavioral, biological, and other sources. Despite these limitations, this study represents an important step toward improving the understanding and prediction of suicide attempts. With further empirical support, behavioral markers have the potential to aid scientists and clinicians in assessing suicidal patients and ultimately intervening to prevent future suicide attempts.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health. (R03MH076047) and the Norlien Foundation to MKN.
Footnotes
We acknowledge that the term “cognitive marker” also is appropriate here, but use “behavioral marker” because we operationalized cognitive factors using objective, behavioral measures.
Stroop interference is referred to as attentional bias to maintain consistency with previous suicide Stroop studies and relevant theories. Some suggest the Stroop task may capture other cognitive processes (e.g., response bias; MacLeod, Mathews, & Tata, 1986). We acknowledge this possibility and encourage future research to tease apart the distinction between attentional and response biases in relation to suicide attempt (e.g., via visual dot probe task).
Results were identical when controlling for overall history of suicide attempt (i.e., replacing history of multiple attempts), such that interference for suicide-related (R2=0.37, b=0.02, SE=0.01, Wald=5.21, OR=1.02, CI=1.00-1.03, p=.02) but not for negatively-valenced words (R2=0.19, b=0.00, SE=0.01, Wald=0.03, OR=1.00, CI=0.99-1.01, p=.86). However, we report multiple attempts in the final model given that this is a more rigorous test.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ABN
Contributor Information
Christine B. Cha, Department of Psychology, Harvard University, Cambridge, MA
Sadia Najmi, Department of Psychology, Harvard University, Cambridge, MA.
Jennifer M. Park, Harvard Medical School
Christine T. Finn, Harvard Medical School
Matthew K. Nock, Department of Psychology, Harvard University, Cambridge, MA
References
- Beck AT. Cognitive therapy and the emotional disorders. New American Library; New York: 1976. [Google Scholar]
- Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. 2nd ed. Basic Books; New York: 2005. [Google Scholar]
- Beck AT, Steer RA. Clinical predictors of eventual suicide: A 5- to 10-year prospective study of suicide attempters. Journal of Affective Disorders. 1989;17:203–209. doi: 10.1016/0165-0327(89)90001-3. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Scale for Suicide Ideation. The Psychological Corporation; San Antonio: 1991. [Google Scholar]
- Becker ES, Strohbach D, Rinck M. A specific attentional bias in suicide attempters. Journal of Nervous and Mental Disease. 1999;187:730–735. doi: 10.1097/00005053-199912000-00004. [DOI] [PubMed] [Google Scholar]
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clinical Pharmacology & Therapeutics. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. Journal of Clinical Psychiatry. 2003;64:14–19. doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- Cox WM, Fadardi JS, Pothos EM. The Addiction-Stroop Test: Theoretical considerations and procedural recommendations. Psychological Bulletin. 2006;132:443–476. doi: 10.1037/0033-2909.132.3.443. [DOI] [PubMed] [Google Scholar]
- Dawes RM. House of cards: Psychology and psychotherapy built on myth. The Free Press; New York: 1996. [Google Scholar]
- Foa EB, Feske U, Murdock TB, Kozak MJ, McCarthy PR. Processing of threat-related information in rape victims. Journal of Abnormal Psychology. 1991;100:156–162. doi: 10.1037//0021-843x.100.2.156. [DOI] [PubMed] [Google Scholar]
- Harkavy-Friedman JM, Keilp JG, Grunebaum MF, Sher L, Printz D, Burke AK, et al. Are BPI and BPII suicide attempters distinct neuropsychologically? Journal of Affective Disorders. 2006;94:255–259. doi: 10.1016/j.jad.2006.04.010. [DOI] [PubMed] [Google Scholar]
- Jarvis B. DirectRT. Empirisoft Corp; New York: 2004. (Version 2004) [Computer software] [Google Scholar]
- Keilp JG, Gorlyn M, Oquendo MA, Burke AK, Mann JJ. Attention deficit in depressed suicide attempters. Psychiatry Research. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp AH, Hopkinson PJ, Hermens DF, Rowe DL, Sumich AL, Clark CR, et al. Fronto-temporal alterations within the first 200 ms during an attentional task distinguish major depression, non-clinical participants with depressed mood and healthy controls: A potential biomarker? Human Brain Mapping. 2009;30:602–614. doi: 10.1002/hbm.20528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World report on violence and health. World Health Organization; Geneva, Switzerland: 2002. [Google Scholar]
- MacLeod C, Mathews A, Tata P. Attentional bias in emotional disorders. Journal of Abnormal Psychology. 1986;95:15–20. doi: 10.1037//0021-843x.95.1.15. [DOI] [PubMed] [Google Scholar]
- Malloy-Diniz LF, Neves FS, Abrantes SSC, Fuentes D, Corrêa H. Suicidal behavior and neuropsychological assessment of type I bipolar patients. Journal of Affective Disorders. 2009;112:231–236. doi: 10.1016/j.jad.2008.03.019. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Kaspi SP, Riemann BC, Zeitlin SB. Selective processing of threat cues in posttraumatic stress disorder. Journal of Abnormal Psychology. 1990;99:398–402. doi: 10.1037//0021-843x.99.4.398. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health (NIMH) The National Institute of Mental Health Strategic Plan. 2009 Retrieved September 21, 2009 from http://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml#strategic-objective1.
- Nock MK, Banaji MR. Assessment of self-injurious thoughts using a behavioral test. American Journal of Psychiatry. 2007a;164:820–823. doi: 10.1176/ajp.2007.164.5.820. [DOI] [PubMed] [Google Scholar]
- Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. Journal of Consulting and Clinical Psychology. 2007b;75:707–715. doi: 10.1037/0022-006X.75.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD. The Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment. 2007;19:309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the “suicidal mind:” Implicit cognition predicts suicidal behavior. Psychological Science. 2010;21:511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce DW. Suicidal intent and self-injury. British Journal of Psychiatry. 1977;130:377–385. doi: 10.1192/bjp.130.4.377. [DOI] [PubMed] [Google Scholar]
- Sawa A, Cascella NG. Peripheral olfactory system for clinical and basic psychiatry: A promising entry point to the mystery of brain mechanism and biomarker identification in schizophrenia. American Journal of Psychiatry. 2009;166:137–139. doi: 10.1176/appi.ajp.2008.08111702. [DOI] [PubMed] [Google Scholar]
- Stroop JR. Studies of interference in verbal reactions. Journal of Experimental Psychology. 1935;12:242–248. [Google Scholar]
- Su T, Zhang L, Chung M, Chen Y, Bi Y, Chou Y, et al. Levels of the potential biomarker p11 in peripheral blood cells distinguish patients with PTSD from those with other major psychiatric disorders. Journal of Psychiatric Research. 2009;43:1078–1085. doi: 10.1016/j.jpsychires.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Smith-Janik SB, Saporito J. Information processing biases and panic disorder: Relationships among cognitive and symptom measures. Behavior Research and Therapy. 2007;45:1791–1811. doi: 10.1016/j.brat.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel A, Beck AT. A cognitive model of suicidal behavior: Theory and treatment. Applied and Preventive Psychology. 2008;12:189–201. [Google Scholar]
- Williams JMG, Broadbent K. Distraction by emotional stimuli: Use of a Stroop task with suicide attempters. British Journal of Clinical Psychology. 1986;25:101–110. doi: 10.1111/j.2044-8260.1986.tb00678.x. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Mathews A, MacLeod C. The Emotional Stroop Task and psychopathology. Psychological Bulletin. 1996;120:3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]