Abstract
Nevi are common skin tumors caused by abnormal overgrowth of cells from the epidermal and dermal layers of the skin. Most nevi are benign, but some pre-cancerous nevi must be monitored or removed. The giant congenital nevus is greater than 10 cm in size, pigmented and often hairy. Between 4% and 6% of these lesions will develop into a malignant melanoma. Since approximately 50% of the melanoma develop by the age of two, and 80% by the age of seven, early removal is recommended. The objective of this paper is to present a unique case of giant nevi and their surgical management.
Key words: nevus, melanoma, giant, congenital.
Introduction
The word Nevus derives from the Latin word Knee-vus meaning birthmark or mole. The nevus is defined as a congenital, developmental tumor-like malformation of the skin or mucous membrane.1 Acquired nevi are extremely common. They appear at about the eight month of life and increase in number with age.
Classification of nevus:
-
congenital
small
giant
-
acquired
intra dermal nevus (common mole)
junctional nevus
compound nevus
spindle cell nevus
epetheloid cell nevus
blue nevus (Jadassohn-Tieche)2
Familial tendencies exist and approximately 1 in 20,000 new born is found to have a large congenital nevus.3 Melanocytes (pigment producing skin cells) are found in utero at about 40 days gestation and it is thought that congenital nevi develop between the 2nd and 6th month of gestation. It develops from neuro ectodermal cell between the intra uterine life of the 8th to 24th week of pregnancy. Body protein HGE/SF (hepatocyte growth factor/scatter factor) seems to be responsible for encouraging these neuroectodermal cells to develop, migrate and scatter. In those of us with a nevus, it seems that we have too much or the wrong type of this body protein HGE/SF in some cells, so we develop extra pigment and abnormal skin cells called nevus cells. Congenital nevi are generally seen in 1 in every 20,000 children, whereas the giant variety involving much of the body surface area are less common, possibly around one in every 200,000. While congenital nevi are typically larger than the common acquired nevi, they cannot always be distinguished by size alone. They are often round or oval, clearly demarcated and some times slightly intact. Pigmentation is usually even, although some congenital nevi have a speckled appearance. Coarse dark hair may be present. The congenital nevi occur in 1–1.25% of neonates and with the passage time, may change from flat, pale, tan macules to elevated verrucous hairy lesions. The head and neck area involve approximately 15% of all nevus. Intraoral occurrence is extremely rare. In cases of acquired nevus, junctional nevus develops at the age of two years, progressing to a compound nevus through the teenage years, and then to a dermal nevus in adulthood. Congenital nevi are significant because of their much higher incidence of melanoma transformation. A Bathing Trunk nevus is a darkly pigmented, disfiguring, often hairy patch of skin present at birth, which may cover an extremely large area of the body. Some times the nevus covers most of the trunk, the upper arm and thigh. Bathing trunk nevi are thought to be caused by spontaneous mutations or other events during fetal development, but in some families, the frequent appearance of these lesions suggest that they may be genetically inherited. They may be associated with other birth defects.8 The distinction between congenital nevi and other forms of acquired nevi can usually be made on clinical examination. Any nevus larger than 1.5 cm is likely to be congenital. The congenital nevi are rare; they are often darkly pigmented and may be hairy and papillary in appearance. Occasionally they cover an extensive area of skin, up to 25% or more of the body surface. They may undergo malignant change even during childhood. The life-time risk for malignant degeneration in a large congenital nevus is approximately 6%.5,6 In these cases melanoma can arise in the first few years of life and excision should be considered as soon as possible. No specific investigation is required for small nevi. People with nevus presenting neurological symptoms, like worsening headache and vomiting, need to have an MRI of the brain.4,7 Those with seizures also need to have repeated MRI performed periodically. The risk of malignant change in giant nevi is probably the most contentious issue in its management. The consensus is that lesions are pre-malignant, but the purported incidence of malignancy varies wildly from 0–42%. Surgical excision remains the mainstay of treatment for large congenital melanocytic nevi, and most giant nevi are managed by staged excision and resurfacing with skin grafts or tissue expanders and flaps. For facial nevi, laser treatment is one of the best known options available for the removal of giant nevi.9
Histologically, nevi are transformed melanocytes, which are normally highly dendritic cells interspersed among basal keratinocytes. The genetic basis of these lesions is not known. Findings of a culture of melanocytes from such a lesion showed chromosome rearrangements involving 1p,12q, and 19p. The giant nevi might be associated to several diseases: neurocutaneous melanosis, diffuse lipomatosis, structural brain malformations, hypertrophy of skull bones, limb atrophy, skeletal asymmetry involving both soft tissues hyper-and hypoplasia, von Recklinghausen's disease and vitiligo.
Case Report
A 5-year old female presented with multiple dark black colored, wart like patches, on her face, neck, shoulder, leg and entire back. No other abnormality was found on physical examination. Family history failed to show any other individuals with a similar lesion (Figure 1). The concern of the present problem of the patient was only esthetic. On examination extra orally, there were 5–6 small to medium sized black discolored patches with coarse hair grown over it present on the right side of the face, neck, shoulder, both the legs and the entire back indicating Bathing Trunk nevus. There was no history of pain, itching or discomfort. The patient lives a normal life and the only concern was the esthetic problem of the facial nevi. Routine blood examination and X-ray chest were in the normal range. Surgical excision of all the facial nevi was planned and it was excised under G.A. using Propofol. (Figures 2–4) Primary closure was performed using 6–0 prolene. Since all the nevi are small in size, no reconstruction is required (Figure 5). An antibiotic was advised. Cefadroxil syrup was indicated 1tsf B. D. for 7 days. Histopathological examination revealed large discrete cells, each with an ovoid, vesicular nucleus and pale cytoplasm. The nevus cells are situated within the connective tissue and are separated from the overlying epithelium by a well defined band of connective tissue. (Figures 3–6).
Figure 1.

Pre-operative photograph of the patient on OT table.
Figure 2.

Intra-operative photograph of the same patient.
Figure 3.

Resected specimen of the same patient.
Figure 4.

Post-operative photograph of the same patient on OT table.
Figure 5.

Post-operative photograph of the same patient.
Figure 6.
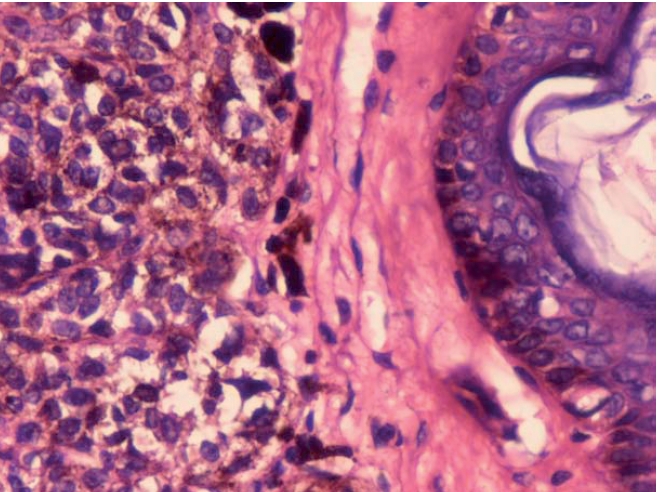
(40×) Histopathological examination shows nevi cells are separated with connective tissue layer.
Discussion
Congenital nevi are generally seen in 1 in every 20,000 children whereas giant congenital varieties involving much of the body surface area are less common, possibly around 1 in 200,000. They can vary in size from being less than 1/4 inch to covering almost the entirebody. The cause of congenital moles may have recently been discovered. Abnormal HGF/SF (hepatocyte growth factor/scatter factor) seems to develop in certain body cells accidentally, called spontaneous autosomal dominant genetic mutations. These mutations are not hereditary. Congenital moles will hardly ever disappear on their own. However, they are important because they can sometimes lead to a potentially deadly skin cancer called malignant melanoma. Malignant changes of giant nevus can occur at any age but most often occur in infants or toddlers. Pregnancy increases the production of melanin in the body. Most dermatologists recommend avoiding excess sun by wearing broad-brimmed hats, sunglasses, long-sleeved shirts, long pants or skirts, gloves and especially avoiding sunburn by staying in the shade, but not all are true. There are cases of melanoma occurring in a mole locating in the arm pit, which is a part of body that receives virtually no sun exposure whatsoever. Complete excision should include removal of each and every cell of melanoma. Since it is actually impossible to totally remove every last single cell of the nevus, the extensive surgeries required to nearly totally remove a nevus can cause other severe, sometimes nearly fatal, complications. Literature says people with nevus in our group die of cancer after their giant nevus had been totally removed. Other literature says that we have had members who underwent numerous surgeries to successfully remove the entire external giant skin nevus only to die later of brain or spinal cord melanoma. Now the cultured skin autograft are sometimes used as a reconstruction of the large excised melanoma. There are a number of treatment options available, but they are not ideal and also have some disadvantages e.g. integra, dermabrasion, laser, chemical peels, tissue expanders and so on.
References
- 1.Chunj C, Forte AJ, Narayan D, et al. A review. J Craniofac Surg. 2006:1210–15. doi: 10.1097/01.scs.0000231619.95263.a2. [DOI] [PubMed] [Google Scholar]
- 2.Gosain AK, Santoro TD, Larson DL, et al. Congenital Nevi: a 20 - year experience and an algorithm for their management. Plast Reconstr Surg. 2001;108:622–36. doi: 10.1097/00006534-200109010-00004. [DOI] [PubMed] [Google Scholar]
- 3.McWhorter HE, Woolner LB. Pigmented Nevi, Juvenile Melanoma and Malignant melanoma in children. Cancer. 2006;7:564–85. doi: 10.1002/1097-0142(195405)7:3<564::aid-cncr2820070316>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 4.Zemtsov A, Lorig R, Bergfeld W, et al. Magnetic resonance imaging of cutaneous melanocytic lesions. J Dermatol Surg Oncol. 1989;15:854–8. doi: 10.1111/j.1524-4725.1989.tb01174.x. [DOI] [PubMed] [Google Scholar]
- 5.Shaw M. Malignant melanoma arising from a giant hairy naevus. Br J Plast Surg. 1962;15:426–31. doi: 10.1016/s0007-1226(62)80068-x. [DOI] [PubMed] [Google Scholar]
- 6.Lorentzen M, Pers M, Brettville-Jensen G. The incidence of malignant transformation in giant pigmented nevi. Scand J Plast Reconstr Surg. 1977;11:163–711. doi: 10.3109/02844317709025513. [DOI] [PubMed] [Google Scholar]
- 7.Frieden I, Williams M, Barkovich A. Giant congenital melanocytic nevi: Brain magnetic resonance findings in neurologically asymptomatic children. J Am Acad Dermatol. 1994;31:423–9. doi: 10.1016/s0190-9622(94)70204-7. [DOI] [PubMed] [Google Scholar]
- 8.Conway H. Bathing trunk nevus. Surgery. 1939;6:585–585. [Google Scholar]


