Abstract
Malignant vascular tumors are rare and angiosarcomas of the breast in patients under 21 years of age are exceedingly uncommon. In this report an angiosarcoma in the breast of a 14-year-old girl is described. She died nine months after mastectomy with recurrent disease in the bones and the contralateral breast. The etiology of most primary angiosarcomas is unknown. Secondary angiosarcomas can develop after radiotherapy and chronic lymphedema. The histology of this angiosarcoma is illustrated.
Key words: angiosarcoma, infancy, breast.
Introduction
Malignant vascular tumors are extremely rare in patients under 21 years of age. Among 228 vascular tumors in 222 children and adolescents observed in a 25-year period, only four (2%) were malignant [three angiosarcomas (AS) and one Kaposi sarcoma].1 In a series of 99 AS from all sites, only a single 3-year-old patient is described.2 The largest series of malignant vascular tumors in the English literature is reported by the Italian and German Soft Tissue Cooperative Group.3 Among 18 patients with malignant vascular tumors, 12 patients ranging from one to 16 years of age were diagnosed with AS. The most frequent sites of AS in childhood are the head and neck region, liver, and skin.2–4 They have been reported also in the brain,5 heart,6 thoracic cavity,7 and mesentery.8 Primary sarcomas of the breast are extremely rare and only a few patients under the age of 21 years have been described in an overview series.9,10 The ages were 13 and 16 years, but in one series it is clear that the 15-year-old patient had AS.11 To our knowledge our study is of the second youngest patient to be reported with AS in both breasts.12
Case Report
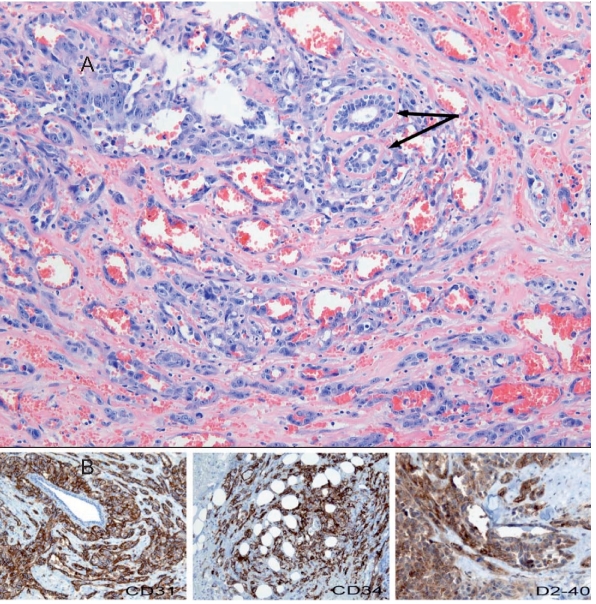
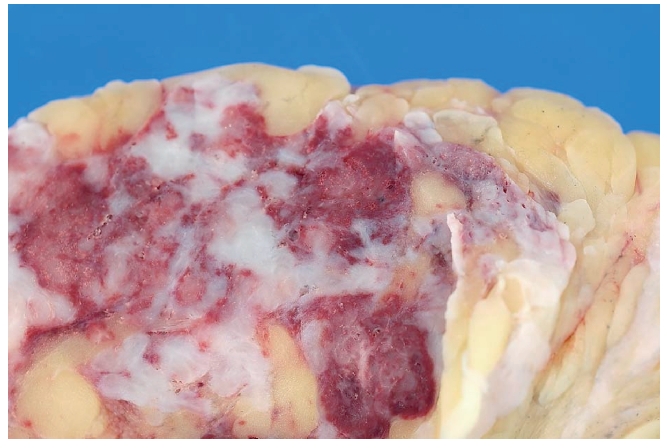
A 14-year-old girl was admitted to our hospital with a rapidly enlarging mass in the right breast. Histological findings of a needle biopsy specimen were consistent with AS. Further investigation did not reveal distant metastases and a simple mastectomy was performed. A complete resection was achieved with very close margins (Figure 1), and for that reason the chest wall was irradiated with a dose of 60 Gy in 33 fractions. The histology of the mastectomy specimen showed the typical features of AS composed of ramifying irregular vascular structures in the breast tissue parenchyma (Figure 2A). Atypical endothelial cells with hyperchromatic nuclei varying in size lined the vascular structures. Occasional multilayering was present, with mitoses readily identified. Focal solid areas of tumor cells were evident. Immunohistochemical staining confirmed the endothelial nature of the tumor cells with strong staining for CD31, CD34, D2-40 (Figure 2B), and FVIII (not shown). After extensive discussion with the pediatric oncology group she received adjuvant therapy of six courses of paclitaxel (175 mg/m2). Five months after surgery she developed several bone metastases and the left humerus was irradiated. One month later the left breast showed a rapidly enlarging tumor and subsequently multiple local recurrences appeared on the right side. A palliative simple mastectomy of the left breast was performed (Figure 3). Three months later and nine months after the first diagnosis she died with bone metastases and an extensive local recurrence of the disease.
Figure 1.
Gross appearance of the complete resection of the right breast.
Figure 2.
(A) Histological section of the right breast illustrating typical features of AS: ramifying irregular vascular structures, focal solid areas of tumor cells, and multilayered cells with hyperchromatic nuclei. Note (arrows) residual normal ductal structures embedded within angiosarcoma tissue. Hematoxylin and eosin stain; 100× magnification. (B) Immunohistochemical staining of the tumor cells for CD31 (left), CD34 (middle), and D2-40(right); 50× magnification.
Figure 3.
Extensive local recurrence after bilateral mastectomy and radiotherapy on the right side.
Discussion
AS is a rare tumor and the etiology is unclear in most cases. Prior irradiation after conservative therapy for breast cancer is a well-known risk for developing mammary AS.13 AS also occurs after chronic lymphedema following axillary and inguinal lymph node dissection.14 In children AS has been described following radiotherapy for vascular disorders at a very young age.15 Other documented risk factors include: xeroderma pigmentosum,16 neurofibromatosis I,7 and exposure to vinyl chloride.17 The diagnosis of AS in the breast may be suspected on clinical examination when red-blue discoloration of the skin is present; in later stages nodular tumor growth appears. The diagnosis may be supported further by fine needle aspiration, in particular when combined with immunocytochemistry.18 A tissue biopsy provides confirmation of the diagnosis of AS. The treatment of choice is surgery whether or not in combination with radiotherapy. In contrast to small cell sarcomas in children (Ewing's sarcoma or primitive neuroectodermal tumor, and rhabdomyosarcoma), AS, like other non-small cell soft tissue sarcomas, are very insensitive to chemotherapy.18,19 The prognosis is very poor, with a five-year survival rate of 20% or less.2,20,21
References
- 1.Coffin CM, Dehner LP. Vascular tumors in children and adolescents: a clinicopathologic study of 228 tumors in 222 patients. Pathol Annu. 1993;28:97–120. [PubMed] [Google Scholar]
- 2.Naka N, Ohsawa M, Tomita Y, et al. Angiosarcoma in Japan. A review of 99 cases. Cancer. 1995;75:989–96. doi: 10.1002/1097-0142(19950215)75:4<989::aid-cncr2820750414>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 3.Ferrari A, Casanova M, Bisogno G, et al. Malignant vascular tumors in children and adolescents: a report from the Italian and German Soft Tissue Sarcoma Cooperative Group. Med Pediatr Oncol. 2002;39:109–14. doi: 10.1002/mpo.10078. [DOI] [PubMed] [Google Scholar]
- 4.Lezama-del Valle P, Gerald WL, Tsai J, et al. Malignant vascular tumors in young patients. Cancer. 1998;83:1634–9. doi: 10.1002/(sici)1097-0142(19981015)83:8<1634::aid-cncr20>3.3.co;2-j. [DOI] [PubMed] [Google Scholar]
- 5.Lach B, Hassounah M, Khafaga Y. Primary angiosarcoma of the brain in a child. Fetal Pediatr Pathol. 2008;27:175–83. doi: 10.1080/15513810802216002. [DOI] [PubMed] [Google Scholar]
- 6.Booth AM, LeGallo RD, Stoler MH, et al. Pediatric angiosarcoma of the heart: a unique presentation and metastatic pattern. Pediatr Dev Pathol. 2001;4:490–5. doi: 10.1007/s10024001-0046-x. [DOI] [PubMed] [Google Scholar]
- 7.Elli M, Can B, Ceyhan M, et al. Intrathoracic malignant peripheral nerve sheath tumor with angiosarcoma in a child with NF1. Tumori. 2007;93:641–4. doi: 10.1177/030089160709300625. [DOI] [PubMed] [Google Scholar]
- 8.Costa da Cunha Castro E, Galambos C, Shaw P, et al. Primary mesenteric angiosarcoma in a child with associated lymphangectasia: a case report. Pediatr Dev Pathol. 2008;11:482–6. doi: 10.2350/08-03-0438.1. [DOI] [PubMed] [Google Scholar]
- 9.Bousquet G, Confavreux C, Magne N, et al. Outcome and prognostic factors in breast sarcoma: a multicenter study from the rare cancer network. Radiother Oncol. 2007;85:355–61. doi: 10.1016/j.radonc.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Rainwater LM, Martin JK, Jr, Gaffey TA, et al. Angiosarcoma of the breast. Arch Surg. 1986;121:669–72. doi: 10.1001/archsurg.1986.01400060063008. [DOI] [PubMed] [Google Scholar]
- 11.Sher T, Hennessy BT, Valero V, et al. Primary angiosarcomas of the breast. Cancer. 2007;110:173–8. doi: 10.1002/cncr.22784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar A, Gupta S, Chopra P, et al. Bilateral angiosarcoma of the breast: an overview. Aust NZ J Surg. 1990;60:341–5. doi: 10.1111/j.1445-2197.1990.tb07381.x. [DOI] [PubMed] [Google Scholar]
- 13.Kirova YM, Gambotti L, De Rycke Y, Vilcoq, et al. Risk of second malignancies after adjuvant radiotherapy for breast cancer: a large-scale, single-institution review. Int J Radiat Oncol Biol Phys. 2007;68:359–63. doi: 10.1016/j.ijrobp.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Offori TW, Platt CC, Stephens M, et al. Angiosarcoma in congenital hereditary lymphoedema (Milroy's disease)--diagnostic beacons and a review of the literature. Clin Exp Dermatol. 1993;18:174–7. doi: 10.1111/j.1365-2230.1993.tb01008.x. [DOI] [PubMed] [Google Scholar]
- 15.Cancellieri A, Eusebi V, Mambelli V, et al. Well-differentiated angiosarcoma of the skin following radiotherapy. Report of two cases. Pathol Res Pract. 1991;187:301–6. doi: 10.1016/S0344-0338(11)80788-0. [DOI] [PubMed] [Google Scholar]
- 16.Marcon I, Collini P, Casanova M, et al. Cutaneous angiosarcoma in a patient with xeroderma pigmentosum. Pediatr Hematol Oncol. 2004;21:23–6. [PubMed] [Google Scholar]
- 17.Kirchner SG, Heller RM, Kasselberg AG, et al. Infantile hepatic hemangioendothelioma with subsequent malignant degeneration. Pediatr Radiol. 1981;11:42–5. doi: 10.1007/BF00972043. [DOI] [PubMed] [Google Scholar]
- 18.Boucher LD, Swanson PE, Stanley MW, et al. Cytology of angiosarcoma. Findings in fourteen fine-needle aspiration biopsy specimens and one pleural fluid specimen. Am J Clin Pathol. 2000;114:210–9. doi: 10.1309/PXMU-LF05-3894-W29F. [DOI] [PubMed] [Google Scholar]
- 19.Chui CH. Nonrhabdomyosarcoma soft tissue sarcoma (NRSTS) Surg Oncol. 2007;16:187–93. doi: 10.1016/j.suronc.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Koscielniak E, Jurgens H, Winkler K, et al. Treatment of soft tissue sarcoma in childhood and adolescence. A report of the German Cooperative Soft Tissue Sarcoma Study. Cancer. 1992;70:2557–67. doi: 10.1002/1097-0142(19921115)70:10<2557::aid-cncr2820701027>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 21.Mark RJ, Poen JC, Tran LM, et al. Angiosarcoma. A report of 67 patients and a review of the literature. Cancer. 1996;77:2400–6. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2400::AID-CNCR32>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]