Abstract
Meningeal fibrosarcomas are rare tumors. Only 41 cases have been reported in the literature to date. Primary central nervous system fibrosarcomas are very aggressive neoplasms and have a poor prognosis. Hence they need to be correctly diagnosed. This is a case of a 13-year old boy with intracranial space occupying lesion. The mass was completely removed and histological examination was characteristic of meningeal fibrosarcoma. The pathological diagnosis is usually made on routine light microscopic examination; however, occasionally these may be difficult to distinguish from other malignant neoplasms such as gliomas, meningiomas and metastases. The diagnosis of fibrosarcoma is based on the identification of a predominant herringbone architectural pattern, the overall uniformity of the spindle cell population, the prominent vimentin positivity, and the presence of pericellular reticulin fibre network. IHC helps to exclude other diagnoses.
Key words: meninges, fibrosarcoma, herringbone pattern
Introduction
Fibrosarcomas arising from the brain parenchyma or its meninges are very rare tumors. These account for 1.5% of intracranial neoplasms.1 To the best of our knowledge, only 41 cases have been reported in the literature to date. The origin of these tumors is still controversial.
These are thought to arise from mesenchymal cells in the Duramater, leptomeninges, vascular adventitia or stalk of the choroids plexus.1,2 Ultrastructural studies have demonstrated either a fibroblastic or a meningothelial origin.3 The pathological diagnosis is usually made on routine light microscopic examination; however, occasionally these may be difficult to distinguish from other malignant neoplasms such as gliomas, meningiomas and metastases.3 Primary central nervous system fibro sarcomas are very aggressive neoplasms and have a poor prognosis.1,4
We document such a case in a 13-year old child. The rarity of the case and the need to differentiate it from other diagnoses makes the discussion of this case of particular importance.
Case history
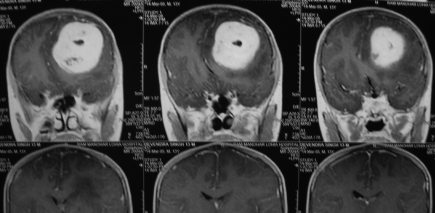
A 13-year old child presented with a 15-day history of generalized tonic clonic convulsions followed by headaches and vomiting. There was history of frontal trauma one month previously. There was no current or recent history of fever. Cerebrospinal fluid, routine and biochemistry were within normal limits. No CT scan was performed at the time of frontal trauma. CT scan on admission revealed a duramater based space occupying lesion in the left frontal region (Figure 1). The provisional diagnosis was a meningioma. The patient underwent left frontal craniotomy and a dural based mass was completely resected. His perioperative course was uneventful. Histopathological examination of the excised mass revealed fibrosarcoma. The patient was referred to a more specialized center for radiotherapy. The patient is still on regular follow-up. He comes to the neurosurgery department once every three months and a CT scan is being performed biennially. The patient has now been symptom free for 33 months.
Figure 1.
CT scan on admission revealed a Duramater-based space occupying lesion in the left frontal region.
Neuropathological findings
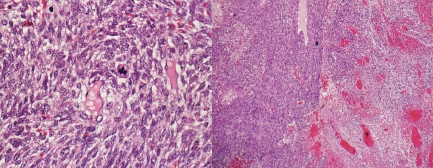
The specimen received for HPE consisted of multiple grayish brown soft friable tissue fragments, the largest of which measured 2.5×1.5×1.5 cm. Paraffin processed hematoxylin and eosin stained sections revealed a cellular tumor composed of cells in interlacing fascicles and in a herringbone pattern (Figure 2). Individual cells were spindly with high nucleocytoplasmic ratio, hyperchromatic vesicular nucleus and 5–6 mitosis/high power. The tumor was seen originating from Duramater.
Figure 2.
Paraffin processed hematoxylin- and eosin-stained sections revealed a cellular tumor composed of cells in interlacing fascicles and in a herringbone pattern.
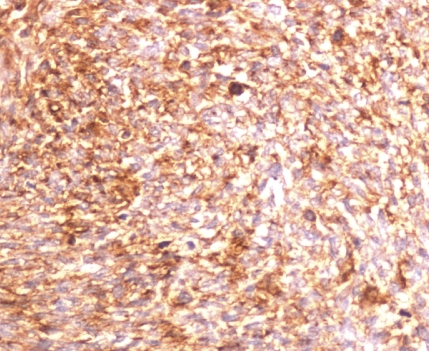
Intercellular reticulin fibers were seen on reticulin stain. Immunohistochemistry was performed using commercially available antibodies (Novocastra, New Delhi, India). The cells were immunopositive for vimentin (Figure 3) while they were negative for epithelial membrane antigen (EMA) and glial fibrillary acidic protein (GFAP).
Figure 3.
The cells were immunopositive for vimentin while they were negative for epithelial membrane antigen and glial fibrillary acidic protein.
Based on the light microscopic and immunohistochemical findings, a diagnosis of meningeal fibrosarcoma was made. The diagnosis was based on predominant herringbone architectural pattern, the presence of intercellular reticulin and prominent vimentin positive nature.
Discussion
Meningeal fibrosarcomas are rare tumors. These are thought to arise from mesenchymal cells of the durameter, leptomeninges, vascular adventitia or the stalk of the choroids plexus. They have been reported in all age groups; however, most cases have been reported early in life.
Histologically these tumors exhibit herringbone pattern architecture and frequently show areas of necrosis.1 Areas of calcification are occasionally seen. The diagnosis of fibrosarcoma is based on the identification of a predominant herringbone architectural pattern, the overall uniformity of the spindle cell population, the prominent vimentin positivity, and the presence of pericellular reticulin fibre network. IHC is of limited value although it may facilitate exclusion of other diagnoses.2,5
The most important diagnostic consideration is malignant meningioma. These are characterized by group of cells with poorly defined cell borders forming characteristic whorls around vessels or stromal elements, and the presence of psammoma bodies. Malignant meningiomas exhibit marked nuclear and cellular pleomorphism, high mitotic activity, and necrosis. In our case, whorling was not seen and IHC was negative for EMA.
Typical solitary fibrous tumors show patternless architecture characterized by a combination of alternating hypocellular and hypercellular areas separated from each other by thick bands of hyalinized, somewhat keloidal, collagen and branching hemangiopericytomalike vessels. The non-atypical, round to spindle-shaped tumor cells have little cytoplasm with indistinct borders, dispersed chromatin within vesicular nuclei and CD34 positivity. None of these features were seen in our case. The recognition of this entity is important because of its favorable prognosis.1
Malignant fibrous histiocytoma (MFH) consists of spindled plump and pleomorphic giant cells that can be arranged in a storiform or fasicular pattern. Further MFH would be positive for histiocytic markers.
Fibrosarcoma presenting with systemic metastases is a rare event. However, the possibility should always be kept in mind. A thorough clinical history would help us exclude or confirm the diagnosis.
Meningiomatosis is a focal malformative lesion of the leptomeninges and underlying cerebral cortex usually occurring in children or young adults. The lesion is characterized by cortical meningovascular proliferation and leptomeningeal calcification interwoven with bands of fibroconnective tissue. The simultaneous occurrence of fibrosarcoma and meningiomatosis is well known.2 Meningiomatosis is also documented in association with meningioma and oligodendroglioma.
Fibrosarcomas can occur in the setting of a pre-exsisting glioma, particularly post radiotherapy. Hence the lesion should be evaluated carefully for presence of any residual focus. Again, a complete clinical history is always helpful.
In summary, fibrosarcomas are rare tumors with an aggressive course and a poor prognosis. Complete or maximum possible resection gives longer disease free survival to the patient. A thorough clinical history and typical histology help make diagnosis easier.The importance of IHC lies in the exclusion of other diagnoses.
References
- 1.Ning C, Kahn LB. A report of primary brain fibrosarcoma with literature review. J Neuro-Oncol. 2004;68:161–7. doi: 10.1023/b:neon.0000027740.70380.5c. [DOI] [PubMed] [Google Scholar]
- 2.Donnet A, Figarella-Branger D, Grisoli F. Primary meningeal fibrosarcoma: a particular neuroradiological presentation. J Neuro-Oncol. 1999;42:79–83. doi: 10.1023/a:1006100119406. [DOI] [PubMed] [Google Scholar]
- 3.Gaspar LE, Mackenzie IRA, Gilbert JJ, Kaufmann JCE, Fisher BF, Macdonald DR, et al. Primary cerebral Fibrosarcomas. Clinicopathological study and review of the literature. Cancer. 1993;72:3277–81. doi: 10.1002/1097-0142(19931201)72:11<3277::aid-cncr2820721124>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 4.Vatsal DK, Sharma S, Renjen PN, Kaul S, Jha AN. Primary fibrosarcoma of brain. Neurology India. 2000;48:396–8. [PubMed] [Google Scholar]
- 5.Torres G, Petit F, Vilchez V, Romero Z, Dorfman S, Cardozo D. Primary cerebral fibrosarcoma in a child. Clin Neuropathol. 2007;26:284–7. doi: 10.5414/npp26284. [DOI] [PubMed] [Google Scholar]