Abstract
Solitary fibrous tumor of the pleura (SFTP) is a mesenchymal tumor that tends to involve the pleura, and is also described in other thoracic and extrathoracic sites. SFTP usually presents as a peripheral mass abutting the pleural surface, to which it is attached by a broad base or by a pedicle that allows it to be mobile. SFTPs exist in benign and malignant forms. A precise pre-operative diagnosis can be arrived at with a cutting-needle biopsy, although most cases are diagnosed with postoperative histology and immunohistochemical analysis. In this pictorial essay, we review a large series of cases, with emphasis on the radiographic appearance of these lesions and their findings from computed tomography, magnetic resonance imaging, ultrasonography and positron emission tomography.
Key words: computed tomography, pleura, solitary fibrous tumor of the pleura, tumor, ultrasonography
Introduction
Solitary fibrous tumor of the pleura (SFTP), first described as a distinct clinical entity by Klemperer and Rabin in 1931,1 is a mesenchymal neoplasm which usually involves the pleura, but it can occur in other thoracic areas (mediastinum, pericardium, and lung) as well as in extra-thoracic areas (meninx, epiglottis, salivary glands, thyroid, kidneys and breast).2,3 SFTP occurs with equal frequency in both sexes and is more commonly found in the fourth, fifth, and sixth decades of life.4
Most of the patients are asymptomatic at the time of diagnosis, and SFTP is discovered only on routine roentgenograms of the chest. In the remaining patients, the most common clinical symptoms are chest pain, cough and dyspnea.5,6 SFTP may occur in benign and malignant forms, these latter showing locally invasive properties or relapsing after surgical resection. Pre-operative diagnosis can be obtained by a transthoracic cutting needle biopsy, but in most cases only pathological evaluation of the resected specimen supported by immunoreactivity of neoplastic cells for CD34 or CD99 allows confirmatory diagnosis.5,7
Concerning microscopic features, the most common architectural pattern is the so-called “patternless pattern”, in which spindle cells with bland ovoidal vesicular nuclei and scarce cytoplasm, and connective tissue are arranged in a random pattern characterized by a combination of alternating hypocellular and hypercellular areas. In the second most common pattern, tumor cells lie in close contiguity with irregular branching small vessels that result in a hemangiopericytoma-like appearance. Hypercellular areas may alternate with hypo-cellular fibrous areas, hemorrhagic, mixoid or necrotic areas.8 Tumor cells are immunoreactive for CD34− and CD99, and are also variably positive for Bcl-2; usually cytokeratins and desmin are negative.9
In this pictorial essay we present a large series of SFTP, all surgically resected, with some emphasis on the radiographic appearance of these lesions and their findings at computed tomography (CT), magnetic resonance (MR), ultrasonography (US), positron emission tomography (PET), with histological correlation. We selected the most significative images in a series of 50 patients from 1990 to 2009. The aim of our paper is to help radiologists and chest physicians to become familiar with the broad spectrum of imaging appearances of SFTP.
Chest radiograph
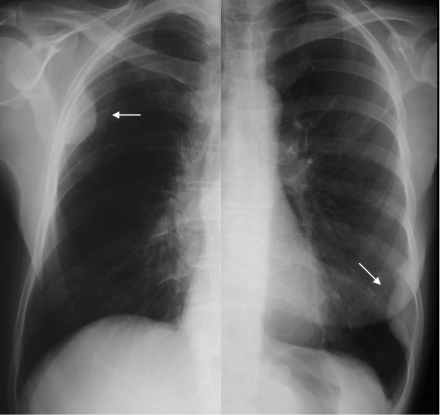
Chest radiographs of patients with small SFTP typically demonstrate a well defined, lobular, solitary mass, which may be visualized in the lung periphery and typically abuts a pleural surface or is located within a fissure (Figures 1and 2).
Figure 1.
Benign SFTP in 2 asymptomatic patients. Postero-anterior (PA) chest radiograph shows smooth marginated masses abutting pleural surfaces (arrows).
Figure 2.
Incidental finding of a small thoracic mass on the magnification of chest X-ray. PA (a) and lateral (b) views of a 52-year old man, suggesting an intrafissural location. During surgery, the lesion presented as a solid mass located within the fissure.
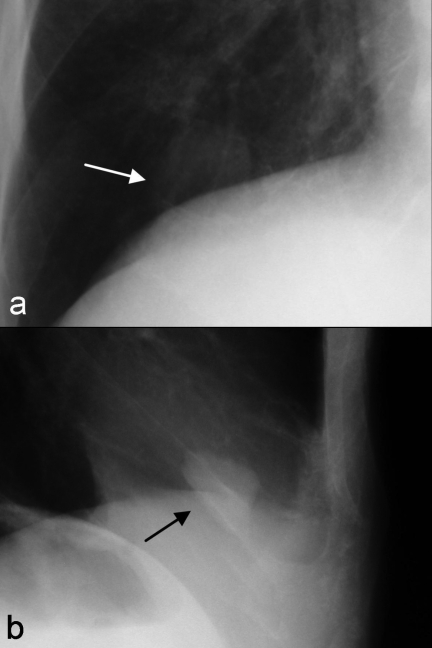
“The incomplete border sign” of extrapleural lesions is useful to differentiate SFTPs from lung masses (Figure 3a). Because extrapleural lesions may exhibit tapered borders, posteroanterior radiography results in an ill-defined margin. Focal pleural masses may also exhibit this “incomplete border” in addition to sharply defined margins when imaged tangentially.5
Figure 3.
SFTP in a 63-year old man. This was an incidental finding of a chest radiograph obtained in a patient with cardiac arrhythmia. PA chest radiograph (a) demonstrating a rounded mass in the right middle hemi-thorax. The lower edge of the lesion is well-defined, but its right-superior border is ill-defined suggesting a pleural origin. Corresponding axial T1-weighted MRI shows a mass of intermediate to high signal intensity (b), while multiphase gadolinium-enhanced T1-weighted image demonstrates early heterogeneous enhancement (c). During the 2-min-late phase, the lesion showed a more homogeneous contrast enhancement than in the arterial phase (d). Corresponding sonographic scan (e) showing a hypoechoic rounded mass with regular margins. Peripheral signals at colordoppler show the presence of a capsular vascularization corresponding to the real anatomy of the lesion (f ). The doppler signals inside the mass are due to centripetal blood vessels moving from the vascular hilum. PET (g) and PET-CT fusion (h) images of the same patient demonstrate a low activity mass.
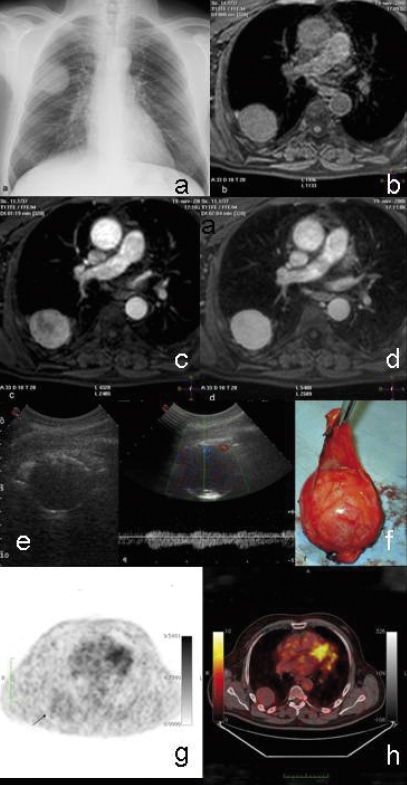
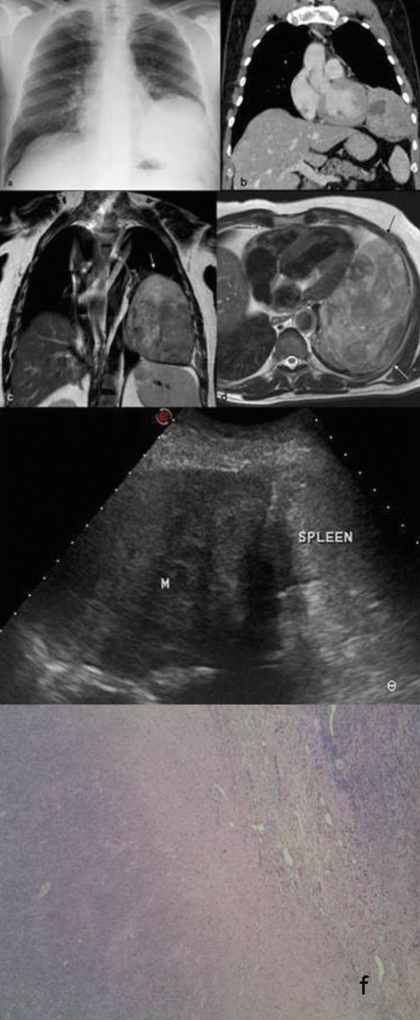
Larger tumors or tumors arising from the mediastinal portion of the parietal pleura may be indistinguishable from primary pulmonary or mediastinal masses (Figure 4a and Figure 5a).
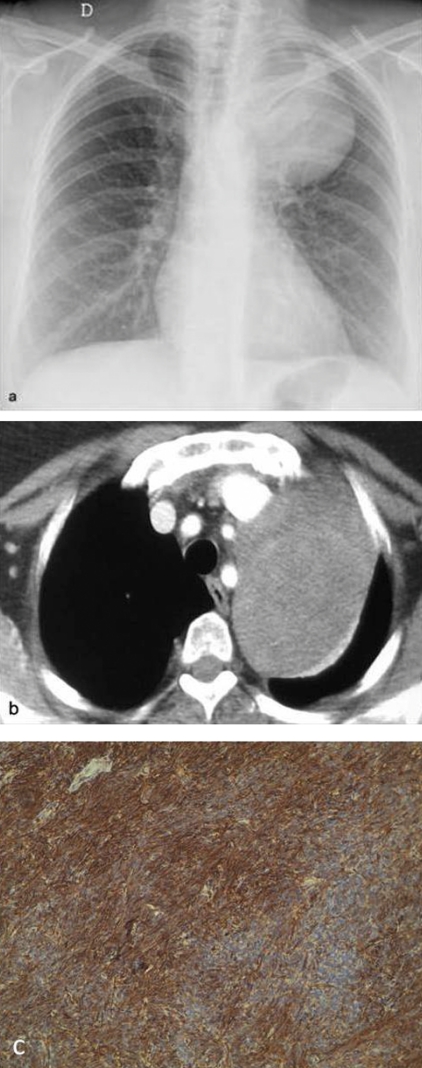
Figure 4.
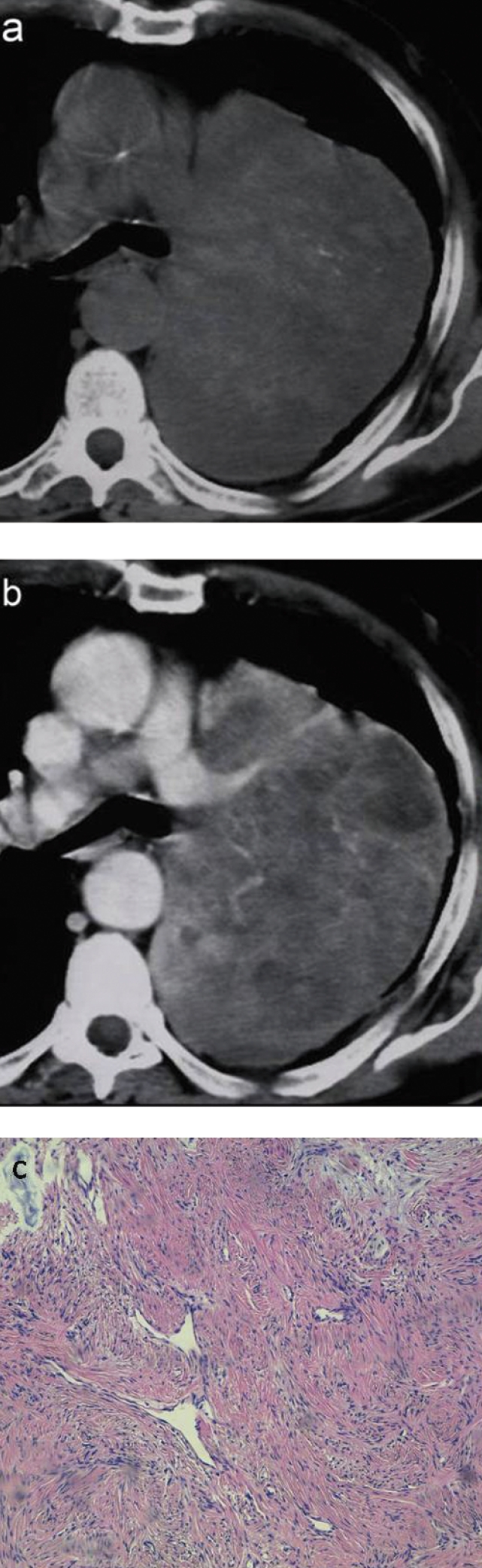
Benign SFTP in a 53-year old man with left-sided chest pain. PA chest radiographs (a) demonstrate a rounded well-defined mass of the left inferior hemithorax inseparable from the diaphragm. Coronal multi-detector CT study (b) demonstrates a large heterogeneous soft-tissue mass with lobular borders. Following the administration of intravenous contrast medium, there is a marked enhancement, with visualization of a large oval area of focal low attenuation due to necrosis or cystic degeneration. Note the mass effect on the ipsilateral hemidiaphragm. There are no signs of invasion to the heart or to the chest wall. At surgery the mass consisted of five pedicles by which it was attached to the mediastinal, diaphragmatic, parietal and lingular visceral pleura. Corresponding axial (c) and coronal (d) T2-weighted MRI demonstrates a large lobular heterogeneous mass with mixed intensity signal (arrows). Compared to CT, MRI better demonstrates the presence of a cleavage plan. Intercostal US scan through the left inferior lateral chest area (e) allows visualization of the spleen (S) and diaphragm as well as the supradiaphragmatic heterogeneous mass (M). (f ) Histopathology on surgical specimen corresponding to hypodensity area on TC imaging: a necrotic central area is evident (40× E-E).
Figure 5.
A 61-year old woman with benign localized fibrous tumor originating from the mediastinal pleura. PA chest radiograph (a) and CT (b) showed the typical pattern of a mediastinal mass. At surgery, the mass was found to arise from the mediastinal pleura. (c) Immunohistochemical staining with strong immunoreactivity of bland fusiform neoplastic cells for CD34 confirm the the diagnosis 100× E-E.
Occasionally, changes in location of a pedunculated mass may be demonstrated.5,10
Computed tomography
CT findings are strictly dependent on tumor size. In case of small SFTP, CT more frequently typically demonstrates a homogeneous well-defined, non-invasive, lobular, soft-tissue mass, usually adjacent to the chest wall (Figures 6a, b and c) or within a fissure, showing an obtuse angle with the pleural surface (Figure 7).10
Figure 6.
A 61-year old woman with benign localized fibrous tumor of the pleura originating from the costal pleural space. Axial and coronal contrastenhanced chest CT respectively show a 2 cm, semilunar, pleura-based soft nodular tissue (42 UH) with obtuse tumor-pleura angle (arrow) (a) in the left middle hemithorax, demonstrating a slightly homogeneous enhancement pattern. Corresponding histopathology on surgical specimen (c): a hypocellular area with discreetly hyalinized keloidal collagen tissue is observed 100× E-E.
Figure 7.
Benign SFTP in an asymptomatic 35-year old woman. Unenhanced chest CT scan (lung window) demonstrates a small well-defined mass of the right superior hemithorax. The main mass forms an obtuse angle with the adjacent pleural surface.
Larger lesions are typically heterogeneous and may not exhibit CT features suggestive of focal pleural tumors (Figure 8). Such lesions usually form acute angles with the adjacent pleural surface mimicking a subpleural pulmonary mass that could be misdiagnosed as peripheral lung cancer.5
Figure 8.
Benign SFTP in a 64-year old woman with chest pain and dyspnea. Contrast-enhanced chest CT scan (mediastinal window) demonstrates an enormous heterogeneous soft-tissue mass in the right hemithorax that produces mass effect on the heart. Because of its large size, this lesion may raise questions of diagnostic interpretation, or even lead to a misdiagnosis.
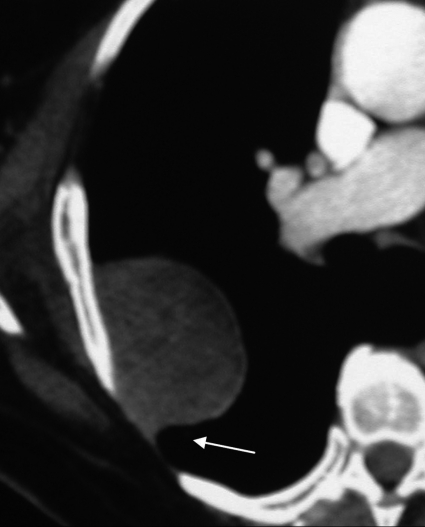
Dedrick et al.11 stated that a “smoothly tapering angle” of the tumor with the adjacent pleura (seen in 5 of their 6 cases) was a highly characteristic finding that could help in establishing the pleural location of the masses (Figure 9). Tumors that are localized within an interlobar fissure can sometimes be interpreted as a pulmonary mass when they appear completely surrounded by the pulmonary parenchyma.
Figure 9.
Benign SFTP in an asymptomatic 71-year old man. Chest enhanced CT scan targeted to the visualization of the lesion (mediastinal window) demonstrates a homogeneous oval lobular soft tissue mass abutting the parietal pleura. Although the lesion forms an acute angle with the pleura layers, a smooth tapering margin (arrow) is also seen.
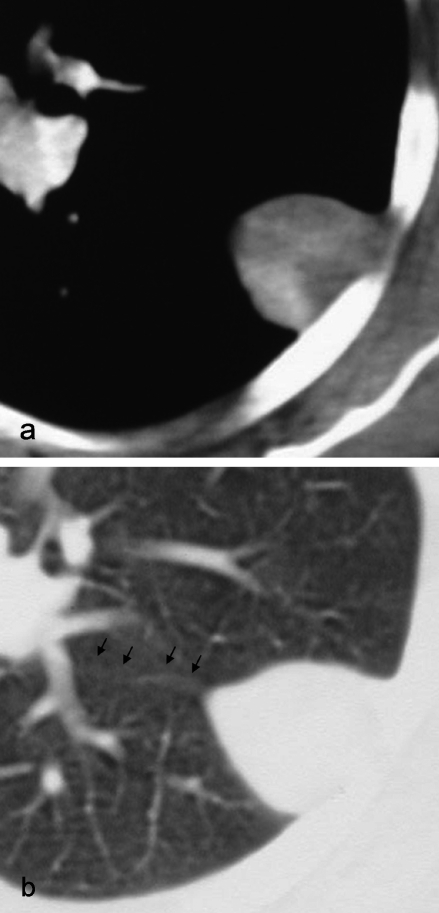
However, multidetector CT provides improved visualization of interlobar fissure and its relationship with the tumor (Figure 10). SFTP that have a mediastinic pleural origin can mimic a medistinal neoplasm; differential diagnosis from a true mediastinal tumor is often impossible (Figure 5b and c). Furthermore, multiplanar and volumetric reformatted CT images are crucial in the differential diagnosis of SFTP originating from the mediastinal pleura, which may mimic a thymic or a germ cell tumor.
Figure 10.
A 35-year old man with an incidental finding of a pleural-based intrafissural lung nodule on axial CT showed at mediastinal (a) and parenchymal (b) windows. The final diagnosis of SFTP was confirmed at surgery.
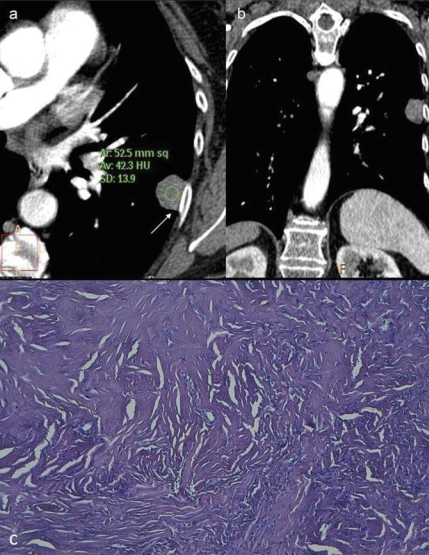
SFTP have been reported to exhibit intermediate to high attenuation on unenhanced CT scans (Figure 11a). This attenuation has been attributed to the high physical density of collagen and the abundant capillary network within these lesions.5
Figure 11.
An 81-year old man with cough, dyspnea and acute hypoglycemia. At CT scanning a mediastinal mass was diagnosed. At surgery, the mass was found to arise from the mediastinal pleura. Unenhanced chest CT scans (a) exhibit intermediate to high attenuation, while contrast-enhanced corresponding scans (b) show heterogeneous enhancement pattern. Note the serpiginous branching linear areas of enhancement consistent with intralesional vessels and the geographical patterns of low attenuation within the lesion. Morphological aspect on surgical specimen (c): a hypocellular area due to collagenized stromal tissue with blood vascular branching vessels, interspersed with bland spindle cells arranged in short fascicles. Mixoid changes are observed. 100× E-E.
Intralesional calcifications (punctate, linear or coarse) are constantly associated with areas of necrosis and more easily seen in larger lesions.5,10 In the case of large masses with calcification, enhancement after contrast medium is typically intense and heterogeneous with central areas of low attenuation (Figure 4b). Such intralesional geographic pattern has been shown to correlate with myxoid changes and areas of hemorrhage, necrosis, or cystic degeneration (Figure 4f and Figure 11b and c).3,10,12
Magnetic resonance imaging
SFTPs show variable signal intensity on MRI. Signal intensity has been described as isoipointense to muscle on T1, and ipointense on T2-weighted images.5,13,14 Ferretti et al.13 reported 4 cases of SFTP with heterogeneous signal intensity on T2-weighted images (Figure 4c and d). Signal intensity increased with intravenous gadolinium (Figure 3b, c and d). It has been suggested that this variable signal intensity mainly depends on the relative amount of collagen and fibroblasts, and presence of areas of hemorrhage, necrosis, or cystic degeneration in the tumor. Intense enhancement of an SFTP is generally due to high vascularity.4
Ultrasonography
SFTPs appear as well-circumscribed non-calcified homogeneous low echogenicity or heterogeneous tissue masses (Figure 3e and f, Figure 4e).
In a previous case report, 6 out of 9 lesions were heterogeneous and exhibited hypoechoic and hyperechoic areas in the absence of cystic degeneration and of intralesional calcifications.
Positron emission tomography
Data concerning the role of positron emission tomography (PET) with 18F-fluoro-2-dexoxy-D-glucose (FDG) in the evaluation of patients with SFTP are scarce. Cortes and co-workers reported no FDG uptake in 2 patients and only minimal FDG uptake (SUV 2.1) in one patient.15
Conclusions
SFTP is usually discovered incidentally on chest radiographs of asymptomatic patients.
The pre-operative differential diagnosis of any mass lesion of the chest ranges from the carcinoma of the lung to various intrapleural sarcomas and pleural mesothelioma, but SFTP should also be considered.
The usual well-circumscribed appearance of the SFTP mass generally rules out malignant pleural mesothelioma since the latter invariably consists of multiple scattered pleural masses or a more diffuse mass encasing the lung.
A posterior paraspinal location might suggest a neurogenic tumor, while a more anterior and para-mediastinal location might raise the possibility of a thymic neoplasm, germ cell tumor, or teratoma.
When SFTP reaches a large size the diagnosis should be considered in consideration of the absence of local invasion, lymphadenopathy, or metastatic spread in patients usually presenting in good health.
References
- 1.Klemperer P, Rabin CB. Primary neoplasm of the pleura: a report of five cases. Arch Pathol. 1931;11:385–412. [Google Scholar]
- 2.Hanau CA, Miettinen M. Solitary fibrous tumor: histological and immunohistochemical spectrum of benign and malignant variants presenting at different sites. Hum Pathol. 1995;26:440–9. doi: 10.1016/0046-8177(95)90147-7. [DOI] [PubMed] [Google Scholar]
- 3.de Perrot M, Fischer S, Bründler MA, et al. Solitary fibrous tumors of the pleura. Ann Thorac Surg. 2002;74:285–93. doi: 10.1016/s0003-4975(01)03374-4. [DOI] [PubMed] [Google Scholar]
- 4.Kim HJ, Lee HK, Seo JJ, et al. MR Imaging of solitary fibrous tumors in the head and neck. Korean J Radiol. 2005;6:136–42. doi: 10.3348/kjr.2005.6.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosado-de-Christenson ML, Abbott GF, McAdams HP, et al. Localized fibrous tumors of the pleura. Radiographics. 2003;23:759–83. doi: 10.1148/rg.233025165. [DOI] [PubMed] [Google Scholar]
- 6.Mahesh B, Clelland C, Ratnatunga C. Recurrent localized fibrous tumor of the pleura. Ann Thorac Surg. 2006;82:342–5. doi: 10.1016/j.athoracsur.2005.09.057. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher CDM, Unni KK, Mertens F. Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press; Lyon: 2002. World Health Organization Classification of Tumours. [Google Scholar]
- 8.Yousem SA, Flynn SD. Intrapulmonary localized fibrous tumor. Am J Clin Pathol. 1988;89:365–9. doi: 10.1093/ajcp/89.3.365. [DOI] [PubMed] [Google Scholar]
- 9.Clayton AC, Salomão DR, Keeney GL, Nascimento AG. Solitary fibrous tumor: a study of cytologic features of six cases diagnosed by fine-needle aspiration. Diagn Cytopathol. 2001;25:172–6. doi: 10.1002/dc.2032. [DOI] [PubMed] [Google Scholar]
- 10.Ferretti GR, Chiles C, Choplin RH, Coulomb M. Localized benign fibrous tumors of the pleura. AJR. 1997;169:683–6. doi: 10.2214/ajr.169.3.9275877. [DOI] [PubMed] [Google Scholar]
- 11.Dedrick CG, McLoud TC, Shepard JAO, Shipley RT. Computed tomography of localized pleural mesothelioma. AJR. 1985;144:275–80. doi: 10.2214/ajr.144.2.275. [DOI] [PubMed] [Google Scholar]
- 12.Cardinale L, Allasia M, Ardissone F, et al. CT features of solitary fibrous tumor of the pleura: experience in 26 patients. Radiol Med. 2006;111:640–50. doi: 10.1007/s11547-006-0062-z. [DOI] [PubMed] [Google Scholar]
- 13.Ferretti GR, Chiles C, Cox JE, Choplin RH, Coulomb M. Localized benign fibrous tumors of the pleura: MR appearance. J Comput Assist Tomogr. 1997;21:115–20. doi: 10.1097/00004728-199701000-00023. [DOI] [PubMed] [Google Scholar]
- 14.Tateishi U, Nishihara H, Morikawa T, Miyasaka K. Solitary fibrous tumor of the pleura: MR appearance and enhancement pattern. J Comput Assist Tomogr. 2002;26:174–9. doi: 10.1097/00004728-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Cortes J, Rodriguez J, Garcia-Velloso MJ, et al. [(18)F]-FDG PET and localized fibrous mesothelioma. Lung. 2003;181:49–54. doi: 10.1007/s00408-003-1002-5. [DOI] [PubMed] [Google Scholar]