Abstract
We report a unique case of primary hepatocellular carcinoma in an ectopic liver rest in the left renal hilum masquerading as a left adrenal tumor. Adrenal tumors have been reported within adrenal rests inside the liver but hepatocellular carcinoma in ectopic liver rests in the adrenal area is an extremely rare entity. To the best of our knowledge, this is the first case report from the Indian subcontinent to describe this event in the English literature.
Our patient, a sixty-year-old, non-diabetic, non-hypertensive male, presented with a history of left flank pain for the past six months. He was a chronic smoker and also consumed excessive amounts of alcohol. He had chronic obstructive pulmonary disease and was hepatitis B surface antigen positive. A contrast enhanced computer tomography scan of the abdomen showed an 8×8×8 cm, well-defined, heterogeneously enhancing mass with central necrosis, in the left suprarenal region. The provisional diagnosis of an adrenal tumor was made and open transperitoneal excision of the tumor along with two enlarged lymph nodes was done. Immunohistochemistry staining of the specimen revealed it to be a primary hepato cellular carcinoma. The patient died within six months of surgery owing to extensive metastases. We concluded that chronic hepatitis B infection and chronic and excessive alcohol consumption and/or chronic smoking may have been the predisposing factors for the occurrence of primary hepatocellular carcin oma in the liver rest in our patient. The prognosis appears to be poor despite surgical management.
Key words: carcinoma, hepatocellular, liver neoplasms
Introduction
Ectopic liver rests are present rarely inside the abdomen on the ligaments, mesentery, surface of the gall bladder, spleen, or adrenal gland, and in the retroperitoneum or thorax.1–3 The natural course of hepatocytes in the accessory liver is not clear owing to the paucity of literature on this topic. The majority of cases have been reported from Japan, and to the best of our knowledge, this is the first case report from the Indian subcontinent in the English literature that depicts primary hepatocellular carcinoma (HCC) in a liver rest in the left renal hilum.2–5 Initially, the mass appeared as a left adrenal tumor but after histopathological analysis it was found to be primary HCC. Although adrenal tumors have been reported within adrenal rests inside the liver, HCC within ectopic liver rests in the renal hilum/adrenal area is extremely rare. This finding makes this case report unique.
Case Report
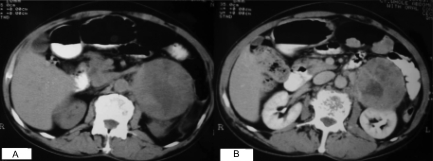
A sixty-year-old, non-diabetic, non-hypertensive male patient presented with a history of left flank pain for the past six months. There were no associated symptoms. The patient was a chronic smoker and consumed excessive amounts of alcohol. He was a known case of chronic obstructive pulmonary disease. On examination, the patient had an oval to round, hard, fixed lump in the left lumbar region. Even though he was found to be hepatitis B surface antigen (HBsAg) positive; his liver function tests were within normal limits. A contrastenhanced computer tomography (CECT) scan of the abdomen showed an 8×8×8 cm, well-defined, heterogeneously enhancing mass with central necrosis, in left suprarenal region (Figure 1A and B). The mass did not seem to be separate from the left adrenal gland; it was displacing the tail of the pancreas and the bowel loops anteriorly. This mass was indenting the superior pole of the left kidney and seemed to be in contact with the left renal vein, bowel loops, greater curvature of the stomach, and abdominal aorta. A few enlarged para-aortic and mesenteric lymph nodes were also seen.
Figure 1.
Computer tomography scans of the abdomen showing: (A), a left suprarenal mass; and (B), a round heterogeneous mass in the left suprarenal area.
A provisional diagnosis of adrenal tumor was made and a 24-hour urinary vinyl mandelic acid measurement was ordered, which was found to be normal. The fine needle aspiration cytology of the mass was inconclusive for malignancy. The patient was operated on under epidural anesthesia. A chevron incision was made and after entering the peritoneal cavity, the left colon was reflected and the tumor mass exposed. The tumor was highly vascular; multiple feeding vessels present over the tumor were ligated and divided. Although the tumor mass was at the renal hilum it could be dissected free from the hilum. A small atrophic adrenal gland was identified adjacent to the tumor. The tumor mass with two enlarged lymph nodes was excised in toto.
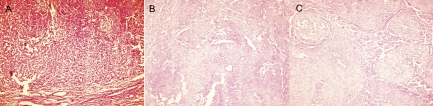
The postoperative period was uneventful. A biopsy of the mass revealed a highly cellular and pleomorphic tumor. The tumor was composed of proliferating large ovoid polygonal cells distributed in cords and trabeculae or as a solid mass (Figure 2A and B). The cells had round or ovoid nuclei and abundant dense eosinophilic cytoplasm. The tumor had irregular dilated thinwalled sinusoidal spaces, which were filled with blood (Figure 2C), along with areas of coagulative necrosis and hemorrhage. No adrenal gland tissue was seen within the tumor mass. The immunohistochemistry staining of the specimen revealed it to be a primary HCC. Details of the immunohistochemical staining are given in Table 1. The patient was investigated again after two weeks; his alpha-fetoprotein was 35 ng/mL at that time. Six months following surgery, the patient presented with ascites and jaundice and on further investigation was found to have secondaries in the native (mother) liver. He died after a couple of days owing to extensive metastases.
Figure 2.
Microphotographs showing: (A), the tumor composed of proliferating large ovoid or polygonal cells distributed in cords, or trabeculae, or a solid mass; (B), tumor cells with round or ovoid nuclei and abundant dense eosinophilic cytoplasm; (C), tumor containing irregular, dilated, thin-walled sinusoidal spaces filled with blood.
Table 1. Details of immunohistochemical staining of the tumor.
| Variables | Results |
|---|---|
| Hepatocyte antibody | Positive+++ |
| Alpha-fetoprotein | Strongly positive |
| HMB-45 | Negative |
| Neuron specific enolase | Negative |
| Chromogranin A | Negative |
| LCA (CD 45) | Negative |
| βHCG | Negative |
| Epithelial membrane antigen | Negative |
| S-100 | Negative |
Discussion
Ectopic liver is also called an accessory lobe if it is visibly attached to the liver.2,3 Because of the diversity in the location and size of these ectopic liver rests, it is difficult to grasp the anatomy of ectopic liver with respect to the degree of completeness of liver structure. Liver tissue supplied by an artery that is not derived from the hepatic artery may not have a portal venous system, and some of these ectopic liver rests may not have a ductal connection with the biliary tract.2–4 A review of the literature suggests that approximately 21 cases of primary HCC in ectopic liver have been reported to date and most of these case reports are from Japan.2–5 These case reports described the occurrence of HCC in the ectopic liver and one report described the occurrence of HCC within both the ectopic liver as well as the native (mother) liver.2 HCC seems to evolve in ectopic liver tissue several years prior to that in the native liver because small ectopic liver tissue does not have a complete (functional) architecture, and may be handicapped metabolically, which accelerates the carcinogenetic process.2 Asymptomatic HBsAg infection and excessive consumption of tobacco and/or alcohol are among the better known predisposing factors for the development of primary HCC in the inhabitants of Asia.6 The presence of these etiological factors might hasten the process of carcinogenesis within the ectopic liver tissue.
In the case of our patient, the tumor was on the left side, in the region of the adrenal gland; thus, we made a provisional diagnosis of adrenal tumor but postoperative histopathological examination revealed it as primary HCC. A further search for primary malignancy within the mother liver was done with the help of a CT scan but it did not reveal any evidence of tumor in the native liver. The alpha-fetoprotein level was moderately raised (35 ng/mL) afterwards, which correlated with the lymph node involvement in the region of the tumor mass. The demise of the patient within six months of surgery is suggestive of poor prognosis in such cases.
Conclusions
Hepatocellular carcinoma within an ectopic liver rest is an extremely rare entity. It may masquerade as an adrenal tumor if present in the adrenal area or at the renal hilum. Chronic HBsAg infection and chronic and excessive alcohol consumption and/or chronic smoking may be predisposing factors for the occurrence of primary HCC in these liver rests. The prognosis appears to be poor despite prompt surgical management.
References
- 1.Winless IR. Anatomy, histology, embryology, and developmental anomalies of the liver. In: Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger and Fordtran's Gastrointestinal and Liver disease. 8th ed. Philadelphia: Saunders (Elsevier); 2006. pp. 1544–1544. [Google Scholar]
- 2.Arakawa M, Kimura Y, Sakata K, et al. Propensity of ectopic liver to hepatocarcinogenesis: case reports and review of the literature. Hepatology. 1999;29:57–61. doi: 10.1002/hep.510290144. [DOI] [PubMed] [Google Scholar]
- 3.Lasser A, Wilson GL. Ectopic liver tissue mass in the thoracic cavity. Cancer. 2006;36:1823–6. doi: 10.1002/1097-0142(197511)36:5<1823::aid-cncr2820360537>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 4.Kim KA, Park CM, Kim CH, et al. Hepatocellular carcinoma in an ectopic liver: CT findings. Eur Radiol. 2003;13:L45–7. doi: 10.1007/s00330-003-1908-6. [DOI] [PubMed] [Google Scholar]
- 5.Algin C, Yaylak F, Olgun EG, et al. Laparoscopic removal of an incidental ectopic liver: Short report of a case. Gastroenterology. 2008;2:134–7. doi: 10.1159/000121283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raoul JL. Natural history of hepatocellular carcinoma and current treatment options. Semin Nucl Med. 2008;38:S13–8. doi: 10.1053/j.semnuclmed.2007.10.004. [DOI] [PubMed] [Google Scholar]