Abstract
Extension of metastatic lung tumors into the left atrium via pulmonary veins is rare. Here, we report the first case of Ewing sarcoma exhibiting such extension. A 31-year-old man with pulmonary metastasis from Ewing sarcoma presented with a mass in the left lung, extending to the left atrium through the left inferior pulmonary vein. As the patient was considered to be at risk of tumor embolism, the mass was excised surgically.
Key words: Ewing sarcoma, lung metastasis, left atrial tumor extension, tumor invasion of pulmonary veins
Introduction
While cases of primary pulmonary tumor with intra-left atrial extension via the pulmonary vein have been well documented, particularly in patients with primary lung cancer,1–3 reports of metastatic lung tumors exhibiting such extension are extremely rare. Indeed, in our examination of the literature, we noted only 10 cases over the past 44 years:4–13 four from chondrosarcoma, 5,11–13 two from osteosarcoma,8,9 and one each from leiomyosarcoma,4 malignant fibrous histiocytoma,6 synovial sarcoma,7 and carcinoma of the cervix.8 To our knowledge, the case presented here is the first citing intra-left atrial extension by metastatic Ewing sarcoma.
Intra-pulmonary veins and -atrial masses can induce widespread emboli and circulatory impairment via outflow obstruction. In fact, sudden severe complications, including cerebral infarction,4,5,12,13 peripheral arterial occlusion,4 and syncopal attack9 have been reported in patients with this type of extension. While no standard timing or type of surgery has yet been agreed on for treating the lesion, we recommended excision of the intra-atrial tumor under cardiopulmonary bypass and cardiac arrest for this particular patient.
Case Report
A 31-year-old man had been experiencing leg paralysis and lower back pain from the age of 30 years. Magnetic resonance imaging (MRI) revealed a large mass in his pelvic region, including the fifth lumbar vertebra, with no evidence of distant metastasis noted on positron emission tomography-computed tomography (PET/CT). Following open biopsy, he was diagnosed with Ewing sarcoma.
The patient was scheduled for complete resection of the primary tumor after four courses of chemotherapy (vincristine, dactinomycin, cyclophosphamide, and doxorubicin alternating with ifosfamide and etoposide) but refused the surgery citing concern regarding the strong expectation of resultant paresis of the lower extremities. Instead he received radiation therapy (50.1 Gy/31 fr) at the primary site followed by adjuvant chemotherapy.
The following year, pulmonary metastases were identified on a follow-up chest CT scan. Because the primary tumor had been well controlled, the patient received video-assisted thoracic surgery on the left inferior and right medial lobes. Vascular invasion into the small vein of the tumor was identified by elastic van Gieson staining. Eight months after the surgery, a CT scan revealed multiple unilateral pulmonary and pelvic node metastases. Because these new pulmonary tumors were unresectable, systemic chemotherapy was performed with a targeted agent against the mammalian target of rapamycin (mTOR) and PI3K as a phase I trial. Three months later, a follow-up contrast chest CT scan revealed a 1.5×2.5 cm mass extending into the left atrium through the pulmonary vein (Figure 1).
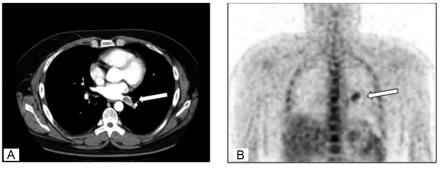
Figure 1.
(A) Axial chest computed tomography scan. A mass can be seen moving toward the left atrium via the pulmonary vein (arrow). (B) Coronal F-18 FDG PET images. The arrow indicates uptake at the site of the mass.
The physical examination revealed no remarkable findings, and the patient presented no further symptoms. Laboratory findings were all within normal ranges, except for a slightly elevated level of lactic dehydrogenase. Pulmonary function was normal, and transthoracic echocardiography confirmed normal cardiac function. Although neither transthoracic nor transesophageal echocardiography revealed the intravascular mass, the PET/CT scan showed it (Figure 1B).
The patient was referred to thoracic surgeons for potential surgical resection. At a multidisciplinary conference, we decided to recommend removal of the tumor to prevent massive tumor emboli and sudden cardiac dysfunction owing to intracardiac extension. The operation involved thoractomy via a midline sternotomy, after which the patient was placed on cardiopulmonary bypass and systemically cooled to a body temperature of 28°C. The heart was then fibrillated and arrested at this temperature. The left atrium was opened, revealing the invasive front of the tumor extending into the left atrium (Figure 2). The intra-atrial tumor was excised, and the pulmonary vein was ligated. A left lower lobectomy was not performed. Seven months after the surgery, the patient reported feeling well with no evidence of tumor emboli or myocardial dysfunction.
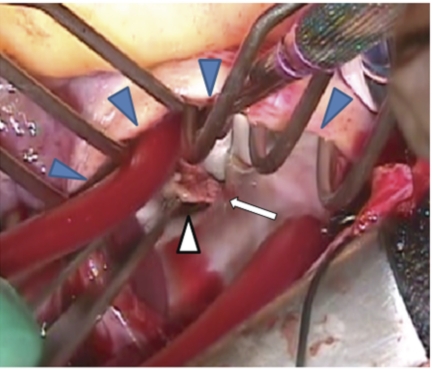
Figure 2.
View from surgical window of left atrium. The blue triangles indicate the surgical section of the left atrium, while the white triangle indicates the pulmonary vein. The white arrow indicates the tumor extending into the left atrium from the pulmonary vein.
Histology and immunohistochemistry
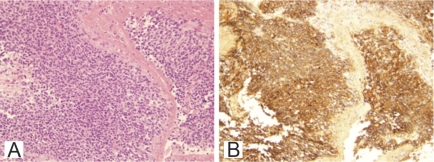
The tumor showed proliferation of small hyperchromatic cells with a high nucleus:cytoplasm ratio and a structureless array (Figure 3A). Immunoreactivities were all negative for AE1/AE3, S-100, LCA, and SMA, but positive for CD99 (Figure 3B). These features are all consistent with a diagnosis of Ewing sarcoma.
Figure 3.
Microscopic findings of the tumor (magnification: 100×). (A) Tumor consists of highly proliferating small round cells with a high nuclear-to-cytoplasmic ratio (hematoxylin-and-eosin stain). (B) Immunoreactivity was strongly positive for CD99.
Discussion
Tumor infiltration of great vessels is not uncommon, and a number of instances of primary pulmonary malignancies with intra-left atrial extension via the pulmonary vein have been reported.1–3 Such extension occurs most frequently in non-small cell carcinomas, but has also been reported in primary pulmonary sarcoma. In their review of 215 lung cancer patients who had undergone CT for staging, Takahashi et al. found 20 patients with tumors potentially invading the proximal portion of the pulmonary veins and left atrium.14 Further evaluation of these patients using breath-hold gadolinium-enhanced three-dimensional MR angiography found nine with invasion of the pulmonary vein and two with extension into the left atrium.14
In contrast to the above findings with primary tumors, however, left atrial extension of metastatic lung tumors through pulmonary veins is extremely rare. Indeed, only 11 cases, including patient, have been reported in the literature. Histological types for these cases were chondrosarcoma (n=4),5,11,13 osteosarcoma (n=2),8,9 leiomyosarcoma,4 malignant fibrous histiocytoma,6 synovial sarcoma,7 and carcinoma of the cervix (n=1 each).8 To our knowledge, ours is the first case report of Ewing sarcoma exhibiting such extension. Although carcinomas of the colon, breast, kidneys, and head and neck frequently metastasize to the lungs, only one case of cervical cancer has been reported to show this type of extension. Given that sarcomas tend to metastasize through the vasculature instead of the lymphatic system, sarcomas may exhibit invasion distinct from carcinoma.
In this particular case, determining the appropriateness of offering surgical resection for the tumor was difficult. Alexander and Haight's proposed criteria for resection of metastatic lung lesions are as follows: metastatic disease is limited to the lung, the primary neoplasm has been treated definitively and is being controlled, and the patient is capable of tolerating complete resection of all metastases.15 In the present case, however, the patient had multiple unresectable metastases (lung and pelvic nodes). In addition, even though palliative resections are often performed in oncology practice to ease certain tumor-related symptoms, this patient was asymptomatic. However, of the cases listed in Table 1, five patients experienced cerebral infarction with hemiplegia (n=3)4,10,12 and facial drop (n=2).5,13 Furthermore, in the case reported by Nicholas et al., widespread embolism occurred soon after detection of the intracardiac extension of the leiomyosarcoma.4 In yet another case, an intra-atrial lesion induced syncopal attack and palpitation.9 In our case, we considered that the growing tumor might induce sudden cardiac arrest owing to obstruction of cardiac inflow. In light of this possibility, we recommended prophylactic surgical resection of the tumor.
Table 1. Extension of metastatic tumors into the left atrium via invasion of pulmonary veins.
| Case | Reference | Age at diagnosis of extension | Sex | Tumor type | Symptom at diagnosis | Treatment for intra-atrial tumor | Consequence after diagnosis |
|---|---|---|---|---|---|---|---|
| 1 | Funakoshi Y et al. (present study) | 31 | M | Ewing sarcoma | None | Palliative operation | Alive (6 mo AO) |
| 2 | Collins et al.4 | 57 | F | Leiomyo sarcoma | None | None* | Arterial occlusion and stroke soon after detection* |
| 3 | Woodring et al.5 | 64 | M | Chondrosarcoma | Headache, left-side facial drop | (Refused surgery) Palliative RT and adriamycin | Died from metastases (9 mo AD) |
| 4 | Ishibashi et al.6 | 63 | F | Malignant fibrous histiocytoma | None | CR | Alive (15 mo AO) |
| 5 | Heslin et al.7 | 23 | F | Synovial sarcoma | None | CR | Alive (16 mo AO) |
| 6 | Gandhi et al.8 | 63 | M | Osteosarcoma | Hemiplegia | Best supportive care | Not described |
| 7 | Senbo et al.9 | 35 | F | Osteosarcoma | Palpitation, syncopal attack | CR, adjuvant cisplatin | Died from metastases (11 mo AO) |
| 8 | Vargas-Barron et al.10 | 55 | F | Carcinoma of the cervix | Hemiplegia, aphasia | CR | Alive and well (2 y AO) |
| 9 | Gardner et al.11 | 28 | M | Chondrosarcoma | Chest pain | CR | Died from local recurrence, lung (10 mo AO) |
| 10 | Boland et al.12 | 26 | M | Chondrosarcoma | Hemiplegia, pleuristic chest pain, shortness of breath | CR | Died from metastases (4 mo AO) |
| 11 | Maclowry et al.13 | 28 | F | Chondrosarcoma | Headache, facial weakness, blurred vision | Chemotherapy | Died from brain metastases (23 d AS) |
All surgeries were conducted under cardiopulmonary bypass.
Soon after detection by X-ray and CT scan, the patient developed systemic emboli (peripheral arterial occlusion and stroke).
Treatment was an embolectomy for peripheral occlusion. Prognosis and follow-up period were not described.
RT, radiation therapy; CR, complete resection (gross complete resection); AO, after operation; AD, after detection; AS, after symptoms.
In summary, we experienced a case of metastatic lung tumors extending into the left atrium via the pulmonary vein. Metastatic tumors exhibiting this type of extension are extremely rare, and this particular case is the first known report of its occurrence with Ewing sarcoma. Given the severe complications that have been reported in patients with this type of extension, immediate prophylactic surgery should be considered.
References
- 1.Lin MT, Ku SC, Wu MZ, et al. Intracardiac extension of lung cancer via the pulmonary vein. Thorax. 2008;63:1122–1122. doi: 10.1136/thx.2007.090373. [DOI] [PubMed] [Google Scholar]
- 2.Chan V, Neumann D. Small cell lung carcinoma invading the pulmonary vein and left atrium as imaged by PET/CT. Eur J Nucl Med Mol Imaging. 2005;32:1493–1493. doi: 10.1007/s00259-005-1930-9. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe N, Kubo K. Images in cardiology: Intra-left atrial invasive mass extended via the pulmonary vein. Heart. 2001;85:271–271. doi: 10.1136/heart.85.3.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins NJ, Barlow MA, Woodford PA, et al. Intracardiac extension of metastatic pulmonary leiomyosarcoma. Heart Lung Circ. 2005;14:121–2. doi: 10.1016/j.hlc.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Woodring JH, Bognar B, van Wyk CS. Metastatic chondrosarcoma to the lung with extension into the left atrium via invasion of the pulmonary veins: presentation as embolic cerebral infarction. Clin Imaging. 2002;26:338–41. doi: 10.1016/s0899-7071(02)00445-x. [DOI] [PubMed] [Google Scholar]
- 6.Ishibashi H, Akamatsu H, Egi K, et al. A case of pulmonary metastasis of malignant fibrous histiocytoma with left atrial infiltration via the pulmonary vein. Kyobu Geka. 2001;54:895–7. [PubMed] [Google Scholar]
- 7.Heslin MJ, Casper ES, Boland P, et al. Preoperative identification and operative management of intraatrial extension of lung tumors. Ann Thorac Surg. 1998;65:544–6. doi: 10.1016/s0003-4975(97)01335-0. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi AK, Pearson AC, Orsinelli DA. Tumor invasion of the pulmonary veins: a unique source of systemic embolism detected by transesophageal echocardiography. J Am Soc Echocardiogr. 1995;8:97–9. doi: 10.1016/s0894-7317(05)80364-5. [DOI] [PubMed] [Google Scholar]
- 9.Senbo J, Sasaki T, Hasegawa Y, et al. [Resection of metastatic pulmonary lesion of osteosarcoma extended into the left atrium and ventricle via the pulmonary vein] Kyobu Geka. 1991;44:929–32. [PubMed] [Google Scholar]
- 10.Vargas-Barron J, Keirns C, Barragan-Garcia R, et al. Intracardiac extension of malignant uterine tumors. Echocardiographic detection and successful surgical resection. J Thorac Cardiovasc Surg. 1990;99:1099–103. [PubMed] [Google Scholar]
- 11.Gardner MA, Bett JH, Stafford EG, et al. Pulmonary metastatic chondrosarcoma with intracardiac extension. Ann Thorac Surg. 1979;27:238–41. doi: 10.1016/s0003-4975(10)63282-1. [DOI] [PubMed] [Google Scholar]
- 12.Boland TW, Winga ER, Kalfayan B. Chondrosarcoma: a case report with left atrial involvement and systemic embolization. J Thorac Cardiovasc Surg. 1977;74:268–72. [PubMed] [Google Scholar]
- 13.MacLowry JD, Roberts WC. Metastatic choriocarcinoma of the lung. Invasion of pulmonary veins with extension into the left atrium and mitral orifice. Am J Cardiol. 1966;18:938–41. doi: 10.1016/0002-9149(66)90446-2. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi K, Furuse M, Hanaoka H, et al. Pulmonary vein and left atrial invasion by lung cancer: assessment by breath-hold gadolinium-enhanced three-dimensional MR angiography. J Comput Assist Tomogr. 2000;24:557–61. doi: 10.1097/00004728-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Alexander J, Haight C. Pulmonary resection for solitary metastatic sarcoma and carcinoma. Surg Gynecol Obset. 1947;85:129. [PubMed] [Google Scholar]