Abstract
Global scale-up of antiretroviral therapy (ART) has focused on clinical outcomes with little attention on its impact on existing health systems. In June–August 2008, we conducted a formative evaluation on ART scale-up and clinic operations at three clinics in Uganda to generate lessons for informing policy and larger public health care systems. Site visits and semistructured interviews with 10 ART clients and 6 providers at each clinic were used to examine efficiency of clinic operations (patient flow, staff allocation to appropriate duties, scheduling of clinic visits, record management) and quality of care (attending to both client and provider needs, and providing support for treatment adherence and retention). Clients reported long waiting times but otherwise general satisfaction with the quality of care. Providers reported good patient adherence and retention, and support mechanisms for clients. Like clients, providers mentioned long waiting times and high workload as major challenges to clinic expansion. Providers called for more human resources and stress-release mechanisms to prevent staff burnout. Both providers and clients perceive these clinics to be delivering good quality care, despite the recognition of congested clinics and long waiting times. These findings highlight the need to address clinic efficiency as well as support for providers in the context of rapid scale-up.
Introduction
The HIV epidemic has put huge pressure on health systems in sub-Saharan Africa. The number of clients starting ART has increased exponentially since 2003 and will need to continue to do so if universal access to antiretroviral therapy (ART) is to be achieved.1,2 By the end of 2008, approximately 3 million people in sub-Saharan Africa were on ART, which represents roughly 44% of those who need treatment.3,4 In Uganda the number of those accessing ART increased from 45,000 in 2004 to over 141,000 by June 2008, representing 40% of those who are eligible and in urgent need of treatment.5
In the frenzy to scale-up ART provision, resources and energy have been focused on the immediate challenges of training personnel, improving drug distribution systems, installing laboratory equipment, introducing education and counseling, and developing monitoring systems. Most research has focused on clinical outcomes, related public health questions, and delivery infrastructure with little attention to how health systems are adjusting to increased demands and needs for scaling up ART. For universal access to ART to be achieved, models of ART scale-up must be efficient and cost effective. Yet, despite the increase of ART scale-up activities throughout Uganda, sub-Saharan Africa, and other parts of the developing world, there are few examinations of the process of scale-up operations.
Aside from published recommendations outlining key factors in successful ART scale-up,6–9 which are largely based on expert opinions, there are very few published evaluations of in-field operations. Wagner et al.10 conducted a formative evaluation of scale-up operations at clinics in Uganda and other parts of sub-Saharan Africa and observed that for rapid ART scale-up, it requires community outreach, efficient clinics with minimal bottlenecks for client flow, and systems for detecting and supporting the return to care of clients who have dropped out of care. A greater understanding of how to make ART scale-up more cost effective and efficient in ensuring steady uptake of care, and smooth client flow in delivering care is critical to continued ART scale-up.10 With numerous ART scale-up programs throughout sub-Saharan Africa, many of which have been operating for over 5 years, the field is in dire need of more vigorous evaluations and lessons learnt so that programs, both new and old, can become sustainable and cost-effective.
In this article we report the findings from a formative evaluation of operations at three ART clinics that use different models of care (clinic-based and physician-driven; clinic-based and nurse-driven; and community-based integrated care). The aim of the study was to better understand the factors that are critical for effective and efficient scale-up with regard to quality of care and clinic efficiency.
We examined clinic efficiency in terms of client flow, specific staff allocation to appropriate clinical duties, clinic visit schedules, and record management systems. We also examined organizational management and human resource policies as well as the extent to which clinics are using HIV clients as a source of labor. For quality of care dimensions, we mainly focused on whether clinic operations address client and provider needs, provide access to HIV care, and support client treatment adherence and retention.
We attempted to answer the following questions: What models of care are being used to scale-up ART in these clinics? How effective and efficient are these models of ART scale-up? How can these models function more efficiently and still maintain quality of care? By identifying in detail the problems each clinic encounters and the solutions they devise, we aim to provide important lessons learned for overcoming barriers and identifying strategies to optimize ART scale-up. Such lessons can then be used by program administrators, governmental agencies, nongovernmental organizations, and donors to establish guidelines for scale-up operations that meet local needs and enhance the success and sustainability of scale-up.
Materials and Methods
Study setting
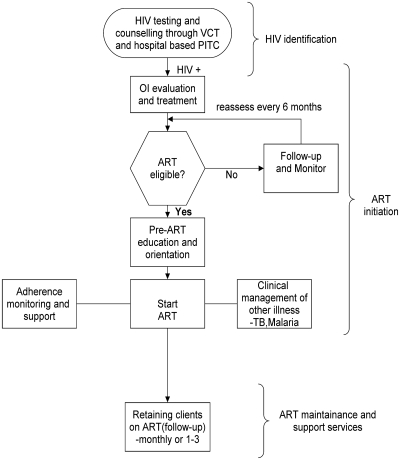
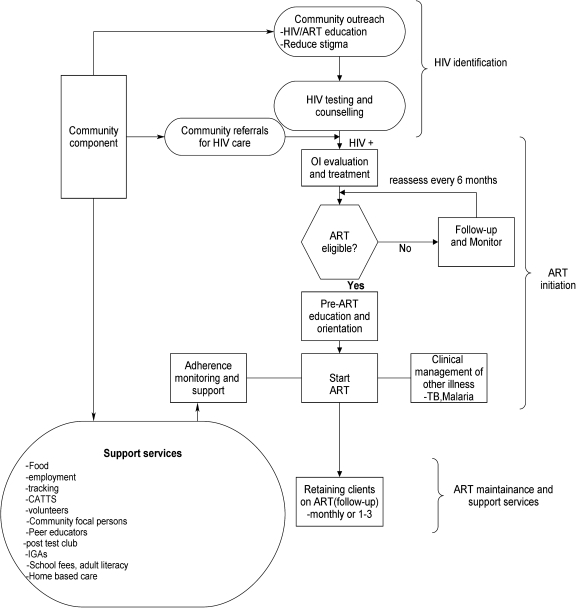
This study constitutes the first phase of a larger, multimethod evaluation of models of care for clinic efficiency, quality of care and cost effectiveness of ART scale-up in Uganda. We conducted the study in June–August 2008 at three selected clinics in Uganda: Mulago HIV Clinic, Mbarara Municipality Clinic (MMC), and Reach Out Mbuya (ROM). Mulago and MMC Clinics are located at the national and regional referral hospitals, respectively, and serve clients from many districts. Mulago Clinic uses a clinic-based care model that is primarily physician-driven, while MMC is clinic-based but combines both nurse- and physician-driven approaches (Fig. 1). On the other hand, ROM runs a nurse-driven clinic whose catchment population is restricted to one parish on the outskirts of Kampala and uses community volunteers of whom more than 65% are themselves HIV clients (Fig. 2). As part of this community-based approach, ROM uses Community ARV and TB Treatment Supporters (CATTS) who conduct weekly home visits for adherence and psychosocial support, notify doctors in cases of emergencies, and refer clients to supplementary support programs.
FIG. 1.
The HIV care model at MMC and Mulago Clinics.
FIG. 2.
The Reach Out Model of HIV care.
The clinics vary on several other dimensions including size of client population, number of clients seen daily, size and composition of clinic staff and the laboratory capacity (Table 1). While Mulago and MMC employ pharmacy technicians to dispense drugs, the nurses dispense drugs at ROM.
Table 1.
Characteristics of the Clinics and Client Population
| Mulago HIV clinic | Mbarara Municipality clinic | Reach Out Mbuya Clinic | |
|---|---|---|---|
| Cumulative total number of clients registered | 8500 | 4231 | 3100 |
| Active clients | 6700 | 2700 | 2800 |
| Clients on ART (active) | 2300 | 1346 | 1100 |
| New clients/week | 80 | 32 | 15 |
| New ART clients/wk | 45 | 26 | 20 |
| Clients seen/day | 270 | 150 | 100 |
| Percentage female | 65% | 60% | 67% |
| Percentage male | 35% | 40% | 33% |
| Baseline Mean CD4 | 152 per mm3 | 398 per mm3 | 102 per mm3 |
| MDs | 6 | 2 | 2 |
| COs | 1 | 1 | 1 |
| Nurses | 8 | 1 | 12 |
| Community workers/volunteers | 0 | 0 | 25 |
| Support staff | 8 | 2 | 6 |
| CD4 machine | Yes | Yes | No |
| HIV testing | Yes | Yes | Yes |
| Visit Schedule | Monthly | Monthly | Monthly |
| No. of years clinic has been in operation | 4 years | 3 ½ years | 7 years |
MD, physician with medical degree; CO, clinical officer.
These clinics serve the needs of a wide range of clients including subsistence farmers, rural and urban wage laborers, and the unemployed. Most clients have significant social and economic needs that go beyond their physical health. Unlike Mulago and MMC, ROM combines medical care with social and economic support programs. These support programs include outreaches for HIV prevention and income generating programs for client households.
Assessment procedures
At each of the clinics, we conducted semistructured interviews with clients, health care providers, and administrators. We also carried out observations of client flows and how each clinic operates. We interviewed 10 ART clients including 5 men and 5 women at each of the clinics. The clients were selected (from among those in attendance at the clinic on the day of interviewing) by the registry staff and were approached by the interviewers for participation in the study. We also interviewed six clinic staff that included at least a nurse, a doctor, and a pharmacy attendant at each of the clinics. At ROM, we also interviewed four providers involved in providing support services. The study team included investigators from the three clinics. However, to increase objectivity and encourage free discussions with providers and patients, the interviewers were external to the programs. We assessed the operations of each clinic with regard to the following key factors to ART scale-up:
HIV care and ART uptake.
Efficiency of the model of care in enabling smooth client flow.
Retention of clients in care.
Efficiency of information and record management.
Impact of human resource policies on operations management and staff morale.
An interview guide for each type of informant (client, provider, administrator) was developed to provide a structure for the interviews, to ensure that the above factors were addressed and to permit comparisons across individuals and groups. Open–ended questions were used to explore new and unexpected leads and to identify areas that were most important to respondents. Open-ended questions were followed by standard probes and closed–ended questions that served to verify, compare, and contrast responses. The interviewers worked in teams of two so that one could take notes while the other conducted the interview. The interviews, which ranged in duration from 30 to 45 min, were tape-recorded. After transcription, themes from the interviews were pulled from the notes and discussed among interviewers until consensus was reached regarding the major themes that were revealed. Data were analyzed manually along the emerging themes.
Results
HIV care and ART uptake
Each of the clinics we studied follows three critical stages in uptake of HIV clients: (1) HIV identification (HIV testing and counseling; community outreach and education); (2) ART initiation (ART eligibility screening, treatment of opportunistic infections, initiation and stabilization on ART); and (3) ART maintenance and support (retention in care; monitoring and follow-up; support services to augment medical impact). However, at ROM, the level of effort on community outreach and support services to augment medical treatment is more pronounced than at the other two clinics.
HIV identification
HIV counseling and testing (HCT) is a critical focal point in funneling HIV-infected individuals into care. Most of the clients in the clinics are referred from HIV testing centers and hospitals. HCT not only identifies who is HIV seropositive and in need of HIV care in some form, but also provides counseling and referrals to ART clinics, as well as prevention counseling to those who test negative. There were varied options of access to HCT services including stand alone voluntary counseling and testing (VCT) centers and testing through hospital-based provider initiated routine counseling and testing (PITC). Apart from ROM, no emphasis on outreach or improving linkages between testing programs and clinics were mentioned. The ROM outreach, CATTS and volunteers encourage the community to go for free HIV testing and links those who are HIV positive within the catchment area to HIV care from ROM. Because of the restriction of clients from only the catchment area, the rate of new clients entering ROM care is much lower than at the Mulago and MMC Clinic sites.
The major reasons why clients decided to take an HIV test were experiences of frequent illness and the loss of a spouse or a child to HIV, reported by most of the clients who were interviewed across the three clinics. Most people are not seeking testing and care until they are experiencing symptoms and thus are later in the disease stage. At the time of the study, health care providers reported that some of the new clients who presented to the clinics were in the late stages of the disease and eligible for ART at entry into care.
ART initiation
Although the staffing and mode of delivering care differed across the three clinics, the basic model for determining ART eligibility and monitoring disease was similar across the sites. As depicted in Figs. 1 and 2, when clients enter care, the stage of illness is determined as well as evaluating eligibility for ART (CD4 cell count less than 200 or AIDS-defining opportunistic infections). Once clients have been found to be eligible for ART, they are given 2–3 sessions of education about ART. They are also asked to bring a friend or relative, who would encourage and provide support to the client in helping to adhere to treatment (i.e., treatment supporter). They are encouraged to disclose their HIV serostatus to their spouses and family members, although this is not a mandatory prerequisite for ART initiation. Once they are started on treatment, clients are seen 2–3 times in the first month of ART in order to address any side effects that may develop, stabilize the dosage, and ensure that the client is adhering to treatment. For clients who are not eligible for ART, symptoms are managed and the immune system is monitored (CD4 cell counts) every 6 months until the illness progresses to the point of becoming eligible for ART.
ART maintenance and augmentative support
Once clients are on ART and stable medically, the main goal of the clinics is to maintain the client in care and on ART. Because clients are now medically stable, follow-up visits for medication refills and monitoring of health and adherence are scheduled variably from monthly to every 3 months. As ART scale-up continues and treatment becomes more available, more resources and stronger focus may be needed to ensure that clients remain in care. Thus Mulago and MMC conduct limited home visits only for ART clients who have missed appointments and are not available by telephone. On the other hand, ROM employs persons living with HIV/AIDS (PLWHAs) to perform some of the clinic activities including home visits, client retention activities, support and monitoring of adherence through CATTS.
Both the clients and providers said access to the clinic and the care it provides is good, but the clinics are very busy, congested, and overwhelmed. All the providers said they were not eager to take on more clients citing the need for more space, more trained staff, and more resources before they can expand access to ART care.
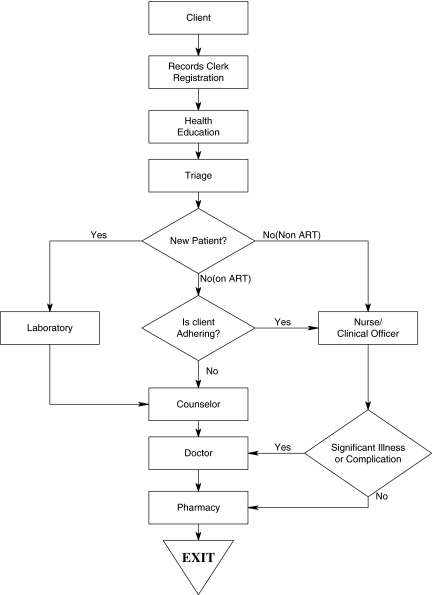
Client flow
Figure 3 illustrates the flow of clients during a single clinic visit at one of the three study clinic sites. On a typical visit to each of the clinics, new clients are taken through the following stages: Registration where a new file is opened for each client and the client is allocated a unique identification number. Registration also entails filling an elaborate mandatory Ministry of health form that captures all the client details. The new client is then entered into the clinic register before being directed to triage. At each of the three clinics, triage is preceded by a health education session. Existing or regular clients (both non-ART and ART) have their files retrieved from records/registry on, a “first-come first-serve basis” before proceeding for a health education session.
FIG. 3.
Client flow at Mulago Clinic.
Health education entails orientation of new clients to the services at the clinic and expectations of the clinic, including strict adherence to clinic appointments and treatment, disclosure and positive living.
Triage involves identification of the very ill clients for urgent attention. During triage, vital observations (temperature, blood pressure, weight, and height) are measured. After triage, client files are taken to the clinicians or counselor at Mulago and MMC Clinics while at ROM clients files are sent to counselors at an adherence desk, before they are finally channeled to the nurse–clinician.
The clinician (medical/clinical officer or nurse–clinician) takes the history of the client, carries out physical examination, diagnoses, and prescribes medications for any other infections as well as request for the relevant laboratory (baseline or monitoring) investigations, depending on whether the client is new or pre-existing. The clinicians also check and document patient adherence to ART. Depending on identified needs, the client's file may or may not be referred back to the counselor. At this stage the client's next return date is fixed.
At the laboratory, specimens for investigations are taken off and urgent laboratory requests are dealt with first, the results of which are sent to the clinician. Thereafter, the laboratory results are taken to the data section for recording and then taken to the registry/records for filing.
At the counseling stage, the counselor assesses the client needs and provides appropriate counseling. This may include the initial counseling for new clients, ongoing counseling for pre-ART and ART clients. The counselor also fills a form for the type of counseling given. According to the clinic procedures, both ART and non-ART patients also receive prevention counseling once in 3 months.
At the pharmacy the staff dispense dugs to clients, enter client information in a record book, and later in the computer. For existing or regular clients (both non-ART and on ART), the pharmacy staff also carry out pill counts to assess the level of adherence. The pharmacy issues the client a card denoting the next return date before the client exits the clinic.
There were observed differences in flow of clients across the clinics. New clients at Mulago and ROM Clinics are first seen by the records clerk while at MMC new clients first interface with a counselor. Mulago gives separate health education to new clients while at MMC, both old and new clients are combined in one health education session. ROM staff and clients jointly have a 30-minute period of prayer and reflection before both old and new clients are combined in one health education session. Every new client at Mulago must be seen by a medical officer but a new client can be seen by a clinical officer at MMC or nurse at ROM. New clients at Mulago have blood samples for CD4 cell counts and other baseline investigations taken on the same day while at MMC and ROM new clients are scheduled for a later date to have their blood samples for CD4 cell count taken.
At MMC and Mulago Clinics, existing clients first see the receptionist or records personnel, and then go through triage, followed by a clinician and then the counselor, before exiting through the pharmacy. At ROM, existing clients first interface with the registry staff that channels their files to the adherence section before they go through the process similar to MMC and Mulago Clinics. On average, new and existing clients will interface with 5–8 providers per visit at each site. Across all three clinics, both the clients and providers said the clients had long waiting times through the clinics. The average length of a clinic visit was reported to be 5 h at ROM, 4 h at Mulago, and 3 h at MMC. The model of care and type of providers who see the clients may influence the long waiting time. ROM has an adherence support desk, which does not exist at MMC and Mulago. At the adherence desk, the adherence supporters/counselors can spend close to 1 h with the client discussing adherence issues and counting all the returned pills. At Mulago and MMC, adherence support is integrated into the counselor visit but the clinicians and pharmacy technicians also check on patient adherence by pill counts and clients' reports. The overall stay in the clinic at ROM may also be increased by the mandatory half-hour yoga reflection exercises for both clients and staff before clinical work begins.
We observed that while the nurse-driven and use of volunteer approach at ROM may be useful in addressing shortage of personnel, the model does not appear to resolve issues related to client flow and waiting times. Another salient observation is that none of the three clinics issue clients specific clinic appointments according to times of the day. The clients are told to come to the clinic on a specific day irrespective of the time of day. Thus most of the clients arrive at the clinic before 9:00 am, creating more clinic congestion in the morning hours. These circumstances pose challenges to staff allocation because the staffs have more clients to attend to in the mornings but are seeing fewer clients in the afternoons. Yet, if the clients were evenly spread out through the day, the clinics would be less congested in the mornings.
Significant bottlenecks in client flow across all the three clinics were cited at the following areas. The records/registry, where it takes long to retrieve the client data and file. For example, at MMC, many clients arrive at the clinic before the clinic opens and pile their medical forms in the order of “first-come first-serve” basis. This pile of medical forms is forwarded to the records/registry. At the registry, the files for the entire batch of medical forms are retrieved and sent to the triage. Providers thought that this causes delays; if the records person encounters difficulty in retrieving one file, the entire batch is delayed. The triage area where several vital signs (blood pressure, weight, and temperature) are measured for every client irrespective of whether they are new, stable, non-ART, or on ART. Clients also often wait in relatively long queues before seeing clinicians.
When posed with the challenge of providing care to greater numbers of clients, and reducing the waiting time, all the clinic administrators and providers called for more human resources at the clinics. None of the clinics mentioned improving efficiency of clinic operations as an option for reducing waiting time and increasing the number of clients in care.
Adherence and retention of clients in care
All the ART clients interviewed reported to be adhering very well to their treatment. Like clients, the providers reported good adherence and patient retention. All the clients said they receive adherence counseling regularly from all the clinic staff as part of the group sessions and individually with clinicians. Most of the clients reported receiving support and reminders from family members (children, spouses, siblings) and friends to take their medicines.
Information and record management
All three clinics capture demographic data, clinical events, medical prescriptions and follow-up examination information in client files. Providers write in the charts during consultations and data entry clerks transfer the data into electronic data bases. None of the clinics had provision for direct electronic data entry during consultations. Thus, there is duplication of work at the clinics to maintain the records in the computer and hard copy files. At one of the clinics (MMC), the very same staff enters the data in a book and later transfers it to the computer. The staff worried about computer failures and loss of data and felt that the hard copy files are a useful backup. Although the process of documentation and record keeping seemed cumbersome, providers at the clinics reported that it met satisfactory standard reporting requirements of the Ministry of Health and partner funding agencies.
Human resource management and operations policies on staff morale
Most of the health care providers reported having clear job descriptions. However, a few of them mentioned unclear job descriptions and communication gaps between them and their supervisors. Apart from pharmacy and laboratory technicians, the other provider types (doctors, nurses, and counselors) reported performing multiple and overlapping tasks in the clinics. For example, a medical doctor at MMC treats clients and works as the clinic administrator. While most of the staff were willing to take on additional roles, they said they were already overloaded by their own responsibilities.
Despite having regular administrative and technical meetings to discuss work experiences and challenges, all of them expressed a feeling of burnout, emotional fatigue and low morale. Providers at Mulago reported that the clinic had stress release events (e.g., retreats), but this was not adequate. Similarly, providers at MMC said the clinic's annual end-of-year party was ineffective in relieving stress and burnout. No mechanisms to address emotional fatigue and burnout were reported at ROM.
Discussion
Our findings show that both providers and patients appreciate the quality of HIV treatment. The outcomes in terms of patient retention and adherence are good. However, there are various gaps in terms of the efficiency of clinic operations as well as support for the providers. These findings are consistent with studies that have examined challenges of ART provision at HIV clinics in Uganda.10,11–14
Our study revealed poor client flow at each of the clinics. There were evident bottlenecks with queues of clients waiting to be seen and most of them spending 4–5 hours at the clinic on each visit. These long visit times were observed at all the three clinics despite the variations in patient load; Mulago provides care to 250–300 patients a day and at MMC and ROM, serve 100–150 clients per day. ROM, which utilizes the strongest task-shifting approach, also faces significant challenges related to efficiency and client flow. Activities such as scheduling the clients to come on another day for laboratory investigations or offering health education to new clients along with those who have come only for refills may create unnecessary inconvenience to the clients and added congestion at the clinics. Furthermore, clients see 5–8 providers per visit and this begs the question of whether or not there is redundancy in terms of tasks undertaken by these providers. For example, at Mulago and MMC several providers including clinicians, counselors, and pharmacy technicians monitor adherence and/or conduct pill counts. While this may be important to reinforce adherence, it also creates overlap in activities and increased delays.
To significantly reduce the time that clients spend waiting to receive care and thus increase the possibility for scale-up of care, strategies are needed to make the flow of clients through the clinics more smooth and efficient. Despite the stated goal of universal access to ART, we did not detect any sense of urgency about making necessary changes to accelerate scale-up; rather, the clinics were most concerned about not adding further burden on the clinic staff. A more urgent approach might be to help the clinics to look at the importance of improving efficiency and maximizing the potential output and productivity with the current staffing levels, as opposed to the common perception that the only way to break thorough this ceiling is to hire more people.
The faster and smoother clients can quickly move through the clinic, the more clients that can be cared for at the clinic on any given day. Optimally, clients should be able to complete a visit in 1–2 h, and much less for those who are stable and simply being monitored. Scale-up programs must balance the need to ensure that care is provided with a level of quality that achieves treatment success with the necessity of being efficient with regard to time and staff allocation in providing care. This is important not only for the clients' satisfaction with care but also for the clinic's goal of accelerating scale-up to reach the large number of people who remain in need of treatment, particularly in the context of staff shortages. Optimally, a clinician should be able to attend to 30 clients in a day without compromising the quality of care provided. In order to achieve efficiency, the clinics need to reconsider the model of care they use to provide HIV care and ART. This includes the composition of clinic staff, which staff provides what type of care, and the schedule of client visits and how this schedule varies by the client's stage of care.
The potential strategies to improve client flow include:
Scheduling pre-ART education sessions to coincide with medical clinic visits, rather than requiring separate visits.
Use of a longer follow-up period for stable and adherent clients. This is yet another important additional option for addressing the bottleneck in client flow and clinic efficiency. Revising follow-up visit schedule to be flexible and correspond to level of client need could substantially improve clinic efficiency and provide room for ART provision scale-up. At the time of this evaluation all clients on ART were seen monthly after the first month of treatment, regardless of the health status of the client. On the other hand, clients who are stable medically and demonstrating good adherence could be allowed to come to the clinic for refills. Pharmacy only visits and nurses only visits would reduce the number of providers seen by a client on a clinic day, and likely reduce the amount of time the client spends at the clinic, while offering the providers more time to attend to new clients and those with complications.
Schedule clinic visits in two daily shifts—morning and afternoon. Currently, most of the clients come to the clinic early in the morning. Having all the clients show up at relatively the same time results in a crowding. Splitting the daily client volume into two shifts could reduce the density of clients waiting for consultation at any one time.
To address the shortage of manpower needed to meet the ever-increasing workload associated with scaling up of HIV care, ART programs are increasingly incorporating HIV clients into the clinic's work force, assisting with adherence education and support, and nontechnical tasks such as clerical support.15–17 Unlike Mulago and MMC, ROM places a strong emphasis on utilizing volunteers, most of whom are HIV clients, and has documented that their community-based approach to providing care results in similar quality of care and clinical outcomes as more conventional models.12
We observed glaring bottlenecks in management of medical records across all the three clinics. While individual client care and program evaluation are pivotal for the success of ART programs, as the number of clients grows, it becomes evident that efficient monitoring of this huge client base will not be possible without new innovations. Large ART programs will eventually need to adopt computerized record management systems. The benefits of a computerized medical records system in terms of efficiency may outweigh the costs associated with its establishment and maintenance.
The findings of this study highlight clinic efficiency as a key challenge to further scale-up of HIV care treatment in resource-limited settings such as Uganda. Regardless of differences in the model of care used, the clinics participating in this study experienced similar challenges and barriers to efficient clinic operations. For sustained scale-up and improved access to HIV services, there is need to incorporate assessment and improvement of efficiency by all HIV clinics.
Acknowledgments
We acknowledge clients and health personnel from the three participating clinics for providing this important information. We thank the Ugandan Ministry of Health for the deliberate effort to scale up HIV care including ART provision. The U.S. President's Emergency Plan for AIDS Relief is acknowledged for the funding of HIV care at the three participating clinics. The work reported herein was supported by a grant provided by the National Institutes of Health, Department of Health and Human Services, Public Health Services (grant number 1R24HD056651-D1).
The following authors made substantial intellectual contributions to the study according to details stated below: M.K., F.W.–M., G.W., G.A., R.W., and S.A. conceived the study, and participated in its design; G.A., R.W., S.A., and M.K. coordinated the study and helped to draft the manuscript; D.K., P.S., and G.S., coordinated data collection and analysis; G.W. participated in the sequence alignment of the manuscript. All authors read and approved the final manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.World Health Organization. Geneva: World Health Organization; 2003. Treating 3 Million by 2005. Making It Happen. The WHO Strategy. [Google Scholar]
- 2.World Health Organization. UNAIDS, UNICEF: Towards Universal Access. Scaling up priority HIV/AIDS interventions in the health sector. Apr, 2007. Progress Report.
- 3.UNAIDS. Report on Global AIDS Epidemic. Joint United Nations Program on HIV/AIDS. 2009. 2009.
- 4.World Health Organization. Towards universal access. Scaling up priority HIV/AIDS interventions in the health sector. Jun, 2008. Progress Report.
- 5.World Health Organization. Bulletin of World Health Organization. 2008 Jun;8686(6):417–496. [Google Scholar]
- 6.UNAIDS. Report on Global on Global AIDS epidemic. Joint United Nations Program on HIV/AIDS. 2006. 2006.
- 7.Institute of Medicine. Washington, DC: The National Academic Press; 2005. Scaling Up Treatment for Global AIDS Epidemic: Challenges and Opportunities. [Google Scholar]
- 8.World Health Organization. Scaling Up Antiretroviral Therapy in Resource-Limited Settings. Treatment Guidelines for a Public Health Approach. 2003. Revision.
- 9.Rizeenthhaler R. Kenya and Rwanda: Family Health International; Jul, 2005. Delivering antiretroviral therapy in resource-constrained settings: Lessons from Ghana. [Google Scholar]
- 10.Wagner G. Ryan G. Taylor S. Formative evaluation of antiretroviral therapy scale-up efficiency in sub-Saharan Africa. AIDS Patient Care STDs. 2007;21:871–887. doi: 10.1089/apc.2007.0008. [DOI] [PubMed] [Google Scholar]
- 11.Amuron B. Namara G. Birungi J. Nabiryo C. Coutinho A. Jaffar S. Mortality and loss-to-follow-up during the pre-treatment period in an antiretroviral therapy program under normal health service conditions in Uganda. BMC Public Health. 2009;9:290. doi: 10.1186/1471-2458-9-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang LW. Alamo S. Guma S, et al. Two-year virologic outcomes of an alternative AIDS care model: Evaluation of a peer health worker and nurse-staffed community-based program in Uganda. J Acquir Immune Defic Syndr. 2009;50:276–282. doi: 10.1097/QAI.0b013e3181988375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uys L. Chirwa M. Kohi T, et al. Evaluation of a health setting-based stigma intervention in five African countries. AIDS Patient Care STDs. 2009;23:1059–1066. doi: 10.1089/apc.2009.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiene SM. Bateganya M. Wanyenze E, et al. Initial outcomes of provider-initiated routine HIV testing and counseling during outpatient care at a rural Ugandan hospital: Risky sexual behavior, partner HIV testing, disclosure, and HIV care seeking. AIDS Patient Care STDs. 2010;24:117–126. doi: 10.1089/apc.2009.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hermann K. Van Damme W. Pariyo GW, et al. Community health workers for ART in sub-Saharan Africa: Learning from experience—Capitalizing on new opportunities. Hum Resour Health. 2009;7:31. doi: 10.1186/1478-4491-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cellettia F. Wrighta A. Palenb J, et al. Can the deployment of community health workers for the delivery of HIV services represent an effective and sustainable response to health workforce shortages? Results of a multicountry study. AIDS. 2010;24(Suppl 1):S45–S57. doi: 10.1097/01.aids.0000366082.68321.d6. [DOI] [PubMed] [Google Scholar]
- 17.Torpey KE. Kabaso ME. Mutale LN, et al. Adherence support workers: a way to address human resource constraints in antiretroviral treatment programs in the public health setting in Zambia. PLoS One. 2008;3:e2204. doi: 10.1371/journal.pone.0002204. [DOI] [PMC free article] [PubMed] [Google Scholar]