Abstract
Objective
Varus and valgus alignment increase, respectively, medial and lateral tibiofemoral load. Alignment was associated with tibiofemoral osteoarthritis progression in previous studies; an effect on risk of incident osteoarthritis is less certain. We tested whether alignment influences the risk of incident and progressive radiographic tibiofemoral osteoarthritis.
Methods
In an observational, longitudinal study of the MOST (Multicenter Osteoarthritis Study) cohort, full-limb x-rays to measure alignment were acquired at baseline and knee x-rays were acquired at baseline and 30 months. Varus alignment was defined as ≤ 178° and valgus as ≥ 182°. Using logistic regression and GEE, we examined the association of baseline alignment and incident osteoarthritis at 30 months (in knees without osteoarthritis at baseline), and alignment and osteoarthritis progression (in knees with baseline osteoarthritis). All analyses were adjusted for age, gender, BMI, knee injury, laxity, and extensor strength, with neutral knees as referent.
Results
2958 knees (1752 participants) were without osteoarthritis at baseline. Varus (adj. OR 1.49, 95% CI 1.06, 2.10) but not valgus alignment was associated with incident osteoarthritis. 1307 knees (950 participants) had osteoarthritis at baseline. Varus alignment was associated with a greater risk of medial osteoarthritis progression (adj. OR 3.59, 95% CI 2.62, 4.92) and a reduced risk of lateral progression, and valgus with a greater risk of lateral progression (adj. OR 4.85, 95% CI 3.17, 7.42) and a reduced risk of medial progression.
Conclusion
Varus but not valgus alignment increased the risk of incident tibiofemoral osteoarthritis. In knees with osteoarthritis, varus and valgus alignment each increased the risk of progression in the biomechanically stressed compartment and reduced the risk of progression in the unloaded compartment.
INTRODUCTION
The load-bearing axis of the lower limb can be represented by a line extending from femoral head center to ankle joint center. In a varus (bow-leg) knee, this line passes medial to the center of the knee, increasing force across the medial tibiofemoral compartment. In a valgus (knock-knee) knee, the axis passes lateral to knee center, increasing force across the lateral compartment. Animal studies and human studies of complicated fractures provided some early evidence that alignment may influence development and progression of knee osteoarthritis (OA) (1).
In recent years, natural history studies of primary knee OA have revealed a link between alignment and subsequent OA progression (2–6). The effect of varus and valgus alignment on risk of incident knee OA is less certain (5,7). Alignment was found to have a stronger effect in knees with moderate tibiofemoral OA than in knees with mild OA, presumably relating to greater vulnerability of more diseased knees to altered load distribution (8). In view of this, it seems likely that any alignment effect on risk of incident knee OA is smaller, and possibly more difficult to detect, than the effect on progression.
Most paradigms of knee OA development and progression posit a central role for local mechanical factors acting within a systemic milieu. There is a particularly compelling biomechanical rationale to support a role for varus and valgus alignment. However, few longitudinal cohort studies have examined the alignment effect on risk of incident knee OA. To advance understanding of the pathways to knee OA development and to inform development of non-invasive prevention strategies, it is important to clarify the impact of alignment in knees without established OA.
In a prospective ancillary study to the Multicenter Osteoarthritis Study (MOST), we tested the hypotheses:
varus and valgus alignment increase the odds of incident radiographic tibiofemoral OA, in knees without tibiofemoral OA at baseline;
varus alignment increases the odds of medial OA progression, and valgus alignment increases the odds of lateral OA progression, in knees with OA at baseline.
METHODS
Sample
MOST is an observational cohort study of incident and progressive knee OA in 3026 community-dwelling men and women, ages 50–79 years. Participants were recruited using mass letter and brochure mailings and community outreach campaigns and enrolled at Iowa City, Iowa, or Birmingham, Alabama. To be eligible for MOST, persons were required to have symptomatic knee OA or characteristics that placed them at increased risk for developing it during the study (9,10). Exclusion criteria were: bilateral total knee replacement or plan for this within the next year; inability to walk without the aid of another person or a walker; serious health condition that would limit longitudinal study participation; ankylosing spondylitis, psoriatic arthritis, reactive arthritis, or rheumatoid arthritis; dialysis; cancer other than nonmelanoma skin cancer; a plan to move from the area within three years.
The study protocol was approved by the institutional review boards at each participating site.
Measurement of Varus-Valgus Alignment and other Factors at Baseline
Alignment was assessed from full-limb radiographs, including hip and tibio-talar joints, acquired at baseline using a previously described protocol (2). Participants stood with the tibial tubercle facing forward. The x-ray beam was centered at the knee at a distance of 2.4 m. A setting of 100 to 300 mA/s and 80–90 kV was used, depending on limb size and tissue characteristics. One AP radiograph of both limbs was obtained. The full limb of tall participants was included by using a 51 × 14 inch graduated grid cassette (Iowa) and a CR-based system of overlapping cassettes and simultaneously exposed subimages forming a stitched image (Birmingham).
Alignment (the hip-knee-ankle angle) was measured as the angle at the intersection of the line connecting femoral head and intercondylar notch centers with the line connecting ankle talar surface center and tibial interspinous sulcus base. Image analysis (11) was completed in batches of 50 by one of three trained readers using a customized program (Surveyor 3 OAISYS Inc., Kingston, Ontario) and blinded to all other data. Each batch was reviewed by a manager prior to transmission. In a reliability study of 200 full-limb pairs assessed by the three readers, the inter-reader and intra-reader ICCs for the hip-knee-ankle angle were 0.95 and 0.96, respectively (12). In analyses, varus alignment was defined as ≤ 178°, valgus as ≥ 182°, and neutral as 179–181°.
Concentric knee extensor strength was measured for each lower limb with a Cybex 350 isokinetic dynamometer (Avocent, Huntsville AL) at 60° per second (13). The average torque (Nm) of 4 maximum effort repetitions was analyzed. Medial-lateral laxity (°) was measured using a protocol and device previously described (14), consisting of a bench and attached arc-shaped track, and providing thigh and ankle immobilization, a stable knee flexion angle, and fixed medial and lateral load. Weight (kg) without shoes or heavy clothes was measured on a balance beam scale and height without shoes using a stadiometer. Injury was defined as any knee injury severe enough to limit ability to walk without a gait aid for at least two days.
Knee X-Ray Acquisition and Assessment
At baseline and 30 months, knee radiographs were acquired using the posteroanterior (PA) “fixed-flexion” weightbearing protocol (15), in which knees are flexed to 20–30° and feet internally rotated 10° using a plexiglass positioning frame (SynaFlexer™). The right and left knees were imaged together on 14 × 17 film with a 72 inch film-to-focus distance. Lateral weight-bearing films were also obtained, following a Framingham Osteoarthritis Study protocol (16).
An experienced rheumatologist and musculoskeletal radiologist independently assessed each PA film for Kellgren and Lawrence (K/L) grade and each PA and lateral film for medial and lateral joint space narrowing grade. The readers were blinded to clinical data and knew the time sequence of the images (17). Joint space narrowing grade was scored (0–3) separately for the medial and lateral compartments using a modified version of the OARSI scale (18,19). Previous studies (3) revealed worsening of joint space narrowing over time not sufficient to move one full OARSI grade. When this occurred in knees with joint space narrowing at baseline, readers were instructed to use ½ grades, an approach which has been validated (19). If readers disagreed on whether incident OA had developed or joint space narrowing grade had worsened, the reading was adjudicated by a panel of three readers. Weighted kappas for agreement between the two readers were: K/L grade 0.79; medial and lateral joint space narrowing grade 0.81 and 0.86, respectively.
Definition of Key Outcomes
All outcomes were knee-based and assessed from baseline and 30-month radiographic images. Using the established and widely applied approach, radiographic knee OA required definite osteophyte presence (K/L ≥ 2) at standard image size; incident OA was defined as the new onset of K/L 2 or greater at 30 months, in knees graded K/L 0 or 1 at baseline.
OA progression was assessed in knees K/L 2 or greater at baseline using a compartment-specific approach. Medial OA progression was defined as any worsening of modified OARSI grade of medial joint space narrowing, and lateral OA progression as any worsening of lateral joint space narrowing grade. Knees with advanced OA that could not progress further (K/L grade 4 or joint space narrowing grade 3) were excluded from analyses.
Statistical Analysis
Both knees from each person were examined. Knee characteristics were calculated separately among knees without radiographic knee OA (K/L < 2) at baseline and knees with knee OA (K/L ≥ 2) at baseline by alignment group [varus (≤ 178°), valgus (≥ 182°), and neutral (179–181°)]. Multiple logistic regression with generalized estimating equations (GEE), to account for potentially correlated observations for knees from the same person, was used to evaluate:
the relationship of varus and valgus alignment at baseline to incident knee OA at 30 months, among knees without tibiofemoral OA at baseline and therefore at risk for incident OA;
the relationship of varus and valgus alignment to medial and lateral tibiofemoral OA progression at 30 months, among knees with OA at baseline and therefore at risk for progression.
Neutral knees constituted the reference group in all analyses. All analyses were adjusted for age (continuous), gender, BMI (continuous), knee injury (dichotomous), laxity (continuous), and extensor strength (continuous). Results from each model are reported as adjusted odds ratios (ORs) with associated 95% confidence intervals (CIs); a 95% CI excluding 1 represents a statistically significant association. In secondary analyses, severity of varus and valgus alignment were analyzed as continuous variables. Sensitivity analyses were run separately for men and women to determine if results were consistent across gender. Analyses were performed using SAS software version 9.2 (SAS Institute Inc., Cary NC).
The funding source played no role in: study design and conduct; collection, management, analysis, and interpretation of data; and preparation, review, or approval of the manuscript.
RESULTS
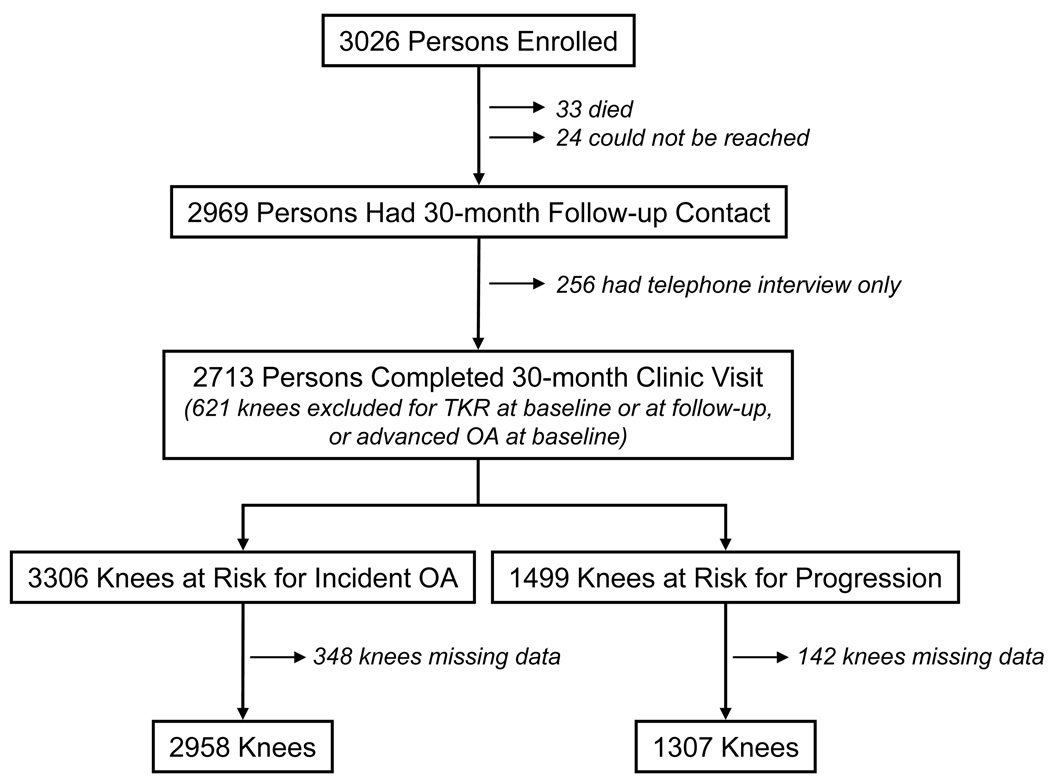
Of 3026 persons enrolled in MOST, 30-month follow-up contact occurred in 2969 (see Figure 1). Of the 57 with no 30-month contact, 33 had died and 24 could not be reached. Of the 2969 persons with 30-month contact: 2713 completed both telephone interview and clinic visit; 215 completed only the telephone interview and a missed clinic visit telephone interview; and 41 completed only the telephone interview. Reasons for not completing the 30-month clinic visit were: too busy (77 persons); health problems (70); caregiving responsibilities (31); deceased (30); clinic too far (21); moved out of area (20); not satisfied with study (19); unable to contact (16); refused to give reason (8); personal problems (7); and other reasons in the remaining 14. Those not completing the 30-month clinic visit did not differ in age, gender, or alignment distribution in the dominant knee (32% neutral, 47% varus, 21% valgus) but had a higher BMI (32.0 ± 6.9, S.D. vs. 30.6 ± 5.8) than those who completed this visit.
Figure 1.
The figure illustrates how the samples of 2958 knees for analyses of incident knee OA and 1307 knees for analyses of knee OA progression were derived.
In the 2713 persons who completed the 30-month clinic visit, 621 knees were excluded from analysis for a total knee replacement at baseline or at follow-up or for advanced OA at baseline that could not progress further. In these 2713 persons, 1614 right knees and 1692 left knees did not have OA at baseline and were at risk to develop incident OA. Of these 3306 knees, 348 were excluded for missing data (predominantly strength or laxity), resulting in a sample of 2958 knees for analyses of incident tibiofemoral OA. OA was present at baseline in 797 right and 702 left knees; these knees were at risk for OA progression. Of these 1499 knees, 192 were excluded for missing data, resulting in a sample of 1307 knees for analyses of OA progression.
The 1752 participants who contributed 2958 knees for analyses of incident OA had a mean age of 61.3 years (± 7.8, SD), a mean BMI of 29.5 kg/m2 (± 5.1), and included 1034 (59%) women. Baseline characteristics of these knees are summarized in Table 1. The 950 participants who contributed the 1307 knees for analyses of OA progression had a mean age of 63.6 years (± 7.8), a mean BMI of 31.7 kg/m2 (± 5.9), and included 592 (62%) women. Characteristics of these knees are summarized in Table 2. In total, 4265 knees in 2287 persons were analyzed; 415 persons contributed to both analysis samples.
Table 1. Characteristics of Knees without Radiographic Tibiofemoral OA.
The table includes characteristics of knees without tibiofemoral OA at baseline. There were 2958 knees without tibiofemoral OA from 1752 persons. In the Table, data from only one knee per person is included, i.e. the right knee. (If only the left knee was without tibiofemoral OA, then data from the left knee is included.)
| Neutral alignment 688/1752 knees (39.2%) |
Varus alignment 725/1752 knees (41.4%) |
Valgus alignment 339/1752 knees (19.4%) |
|
|---|---|---|---|
| Number (%) knees in group with injury | 127 (18%) | 141 (19%) | 72 (21%) |
| Laxity, mean (S.D.), ° | 4.1 (2.6) | 3.9 (2.5) | 3.8 (2.7) |
| Extensor strength, mean (S.D.), Nm | 86.4 (39.5) | 95.2 (42.9) | 71.9 (35.2) |
| K/L grade 0, number (%) | 490 (71%) | 466 (64%) | 246 (73%) |
| K/L grade 1, number (%) | 198 (29%) | 259 (36%) | 93 (27%) |
Table 2. Characteristics of Knees with Radiographic Tibiofemoral OA.
The table includes characteristics of knees with tibiofemoral OA at baseline. There were 1307 knees without tibiofemoral OA from 950 persons. In the Table, data from only one knee per person is included, i.e. the right knee. (If only the left knee had tibiofemoral OA, then data from the left knee is included.)
| Neutral alignment 232/950 knees (24%) |
Varus alignment 550/950 knees (58%) |
Valgus alignment 168/950 knees (18%) |
|
|---|---|---|---|
| Number (%) knees in group with injury | 72 (31%) | 212 (39%) | 42 (25%) |
| Laxity, mean (S.D.), ° | 3.9 (2.5) | 3.8 (2.5) | 4.4 (2.6) |
| Extensor strength, mean (S.D.), Nm | 72.2 (35.1) | 80.0 (42.0) | 54.5 (30.8) |
| K/L grade 2, number (%) | 165 (71%) | 208 (38%) | 95 (57%) |
| K/L grade 3, number (%) | 67 (29%) | 342 (62%) | 73 (43%) |
As shown in Table 3, the odds of developing incident tibiofemoral OA were significantly elevated in knees with varus, but not in knees with valgus alignment at baseline, compared to neutral knees, in analyses adjusting for age, gender, BMI, knee injury, laxity, and strength. The magnitude of the OR was comparable in the smaller strata of women and men considered separately. We secondarily analyzed alignment as a continuous variable. Including only neutral and varus knees, greater severity of varus at baseline was associated with greater odds of incident OA approaching significance [adjusted OR 1.07/1° varus (95% CI 0.99, 1.16)]. Among valgus and neutral knees, greater severity of valgus was not associated with greater odds of incident OA [adjusted OR 0.98/1° valgus (95% CI 0.85, 1.14)].
Table 3. Varus and Valgus Alignment and Incident Radiographic Tibiofemoral OA.
The table shows, first for both genders together and then for women and men separately, the OR and 95% CI for varus and valgus alignment, each compared to neutral alignment as the referent group. The dependent variable is incident radiographic tibiofemoral OA. ORs are adjusted for age, gender, BMI, knee injury, laxity, and extensor strength.
| Gender | Alignment | # knees without OA at baseline (2958 knees) |
# (row %) knees with incident OA at 30 months (181 knees, 6.1%) |
Adjusted OR (95% CI) |
|---|---|---|---|---|
| Both women and men | Neutral (reference) | 1231 | 66 (5.4%) | Reference |
| Varus | 1191 | 88 (7.4%) | 1.49 (1.06, 2.10) | |
| Valgus | 536 | 27 (5.0%) | 0.87 (0.54, 1.43) | |
| Women only | Neutral (reference) | 758 | 44 (5.8%) | Reference |
| Varus | 580 | 49 (8.5%) | 1.47 (0.95, 2.26) | |
| Valgus | 422 | 24 (5.7%) | 0.93 (0.54, 1.63) | |
| Men only | Neutral (reference) | 473 | 22 (4.7%) | Reference |
| Varus | 611 | 39 (6.4%) | 1.41 (0.80, 2.49) | |
| Valgus | 114 | 3 (2.6%) | 0.51 (0.15, 1.82) |
As shown in Table 4, the odds of medial OA progression were significantly elevated in knees varus at baseline. Medial OA progression risk was significantly reduced in valgus knees. On the other hand, the odds of lateral OA progression were significantly elevated in knees valgus at baseline and significantly reduced in varus knees (see Table 4). The results were similar in men and women considered separately. The finding for valgus alignment and lateral progression in men may reflect that there were only 28 valgus knees with OA in men. We secondarily analyzed alignment as a continuous variable. Including only neutral and varus knees, greater severity of varus at baseline was significantly associated with greater odds of medial OA progression [adjusted OR 1.29/1° varus (95% CI 1.22, 1.37)]. Among valgus and neutral knees, greater severity of valgus was significantly associated with greater odds of lateral OA progression [adjusted OR 1.47/1° valgus (95% CI 1.30, 1.65)].
Table 4. Varus and Valgus Alignment and Radiographic Tibiofemoral OA Progression.
The table shows, first for both genders together and then for women and men separately, the OR and 95% CI for varus and valgus alignment, each compared to neutral alignment as the referent group. The dependent variable is medial tibiofemoral OA progression in the top half of the table, and lateral tibiofemoral OA progression in the bottom half of the table. ORs are adjusted for age, gender, BMI, knee injury, laxity, and extensor strength.
| Gender | Alignment | # knees with OA at baseline (1307 knees) |
# (row %) knees with MEDIAL OA progression at 30 months (558 knees, 42.7%) |
Adjusted* OR (95% CI) |
|---|---|---|---|---|
| Both women and men | Neutral (reference) | 317 | 88 (27.8%) | Reference |
| Varus | 758 | 443 (58.4%) | 3.59 (2.62, 4.92) | |
| Valgus | 232 | 27 (11.6%) | 0.34 (0.21, 0.55) | |
| Women only | Neutral (reference) | 221 | 56 (25.3%) | Reference |
| Varus | 408 | 242 (59.3%) | 4.21 (2.84, 6.24) | |
| Valgus | 204 | 23 (11.3%) | 0.37 (0.21, 0.65) | |
| Men only | Neutral (reference) | 96 | 32 (33.3%) | Reference |
| Varus | 350 | 201 (57.4%) | 2.75 (1.63, 4.66) | |
| Valgus | 28 | 4 (14.3%) | 0.34 (0.11, 1.03) | |
| Alignment | Gender | # knees with OA at baseline (1307 knees) | # (row %) knees with LATERAL OA progression at 30 months (163 knees, 12.5%) | Adjusted* OR (95% CI) |
| Both women and men | Neutral (reference) | 317 | 46 (14.5%) | Reference |
| Varus | 758 | 17 (2.2%) | 0.12 (0.07. 0.21) | |
| Valgus | 232 | 100 (43.1%) | 4.85 (3.17, 7.42) | |
| Women only | Neutral (reference) | 221 | 24 (10.9%) | Reference |
| Varus | 408 | 8 (2.0%) | 0.15 (0.06, 0.33) | |
| Valgus | 204 | 88 (43.1%) | 6.35 (3.76, 10.75) | |
| Men only | Neutral (reference) | 96 | 22 (22.9%) | Reference |
| Varus | 350 | 9 (2.6%) | 0.08 (0.04, 0.19) | |
| Valgus | 28 | 12 (42.9%) | 1.88 (0.69, 5.12) |
Further adjustment for baseline K/L grade, baseline knee pain severity, and concurrent change in BMI had minimal impact on these results.
DISCUSSION
Varus but not valgus alignment increased the risk of incident radiographic tibiofemoral OA. In the more vulnerable milieu of the knee with established OA, varus and valgus alignment each increased the risk of OA progression in the biomechanically stressed compartment and reduced the risk of progression in the unloaded compartment. A substantial proportion of knees were varus or valgus: 41% and 19%, respectively, in knees without tibiofemoral OA; 58% and 18% in knees with OA.
The pattern of results in the stressed and unloaded tibiofemoral compartments further supports that the mechanism of action of malalignment relates to its effect on load distribution. Varus alignment shifts the load-bearing axis medial to knee center, creating a moment arm that increases forces across the medial compartment and reduces lateral load; the lateral shift of the load-bearing axis due to valgus alignment increases forces across the lateral compartment and reduces medial load.
We found that varus but not valgus alignment increased the risk of incident OA. Similarly, Brouwer et al (5) observed that varus had a significant effect, while valgus had a borderline effect, in a study using a comparable definition of varus and valgus and defining, as we did, neutral knees as reference. The relationship between alignment and knee OA development was also examined in a case-control study involving Framingham cohort members; in this study, the most varus (1–7° varus) was compared not to neutral knees but to the most valgus quartile (5–10° valgus) as referent (7), modeling a different question than what we posed.
From a biomechanical perspective, a stronger finding for varus alignment is not surprising. Due to a stance phase knee adduction moment, greater load passes medially than laterally even in neutrally aligned, healthy knees (20,21). The adduction moment magnitude increases as varus alignment increases (22). Adduction moment magnitude predicted knee OA progression (23); an adduction moment increase may lie in the causal pathway between varus alignment and knee OA progression. Varus alignment further increases total load passing medially (24). Although valgus alignment is associated with an increase in lateral compartment peak pressures (25), the medial compartment often continues to bear more load until more severe valgus is present (26,27).
Alternatively, the inability to detect an association between valgus alignment and incident OA may reflect a lower sensitivity of the measure of incident OA vs. the measure of OA progression. In the vast majority of knees, osteophyte development precedes joint space narrowing. The definition of incident OA hinges upon these osteophytes. Because osteophyte formation is neither specific to the involved nor to the spared compartment, at the earliest stage of OA (K/L 2), radiographs cannot reveal whether a knee has medial or lateral OA. It is possible that the greater overall frequency of medial vs. lateral OA dilutes the detected valgus effect upon a non-compartment specific measure of incident OA. In contrast, the measure of progression allows specific examination of the compartment stressed by the alignment (medial for varus, lateral for valgus). As such, in the analysis of the impact of alignment, the measure of incident OA, which is not compartment-specific, is generally inferior to the measure of progression
In the analyses of knees with OA at baseline, varus and valgus alignment were associated with medial and lateral OA progression, respectively, in keeping with previous studies (2–6). Brouwer et al also found significant results for varus only; the association between valgus and lateral progression was significant only for those who were obese (5). As the authors note, the inability to detect the valgus effect may relate to use of K/L worsening to define progression and the relatively small numbers with progression (5).
The source of malalignment predating knee OA may be genetic, developmental, or traumatic. Prior to the study by Brouwer et al (5), evidence that malalignment may contribute to OA development came from animal models and human fracture studies. Our findings and those of Brouwer et al support that, in knees without radiographic tibiofemoral OA, varus alignment increases the risk of OA development. The prevalence of varus and valgus alignment in knees without radiographic OA – i.e., before any loss of bone and cartilage height that could contribute to malalignment – support that not all malalignment is a consequence of disease. And, whatever the original cause of the alignment, varus and valgus alignment each increase the risk of subsequent knee OA progression. It seems likely that worsening of tibiofemoral OA in turn increases malalignment at least in some knees. With only one time point of alignment measurement, we could not explore this. The existence of a vicious cycle does not lessen the impact of our findings; strategies that interrupt a vicious cycle may be a potent means of delaying progression. These results support further development and testing of non-invasive modalities to improve tibiofemoral load distribution in varus-aligned and valgus-aligned knees.
It is important to acknowledge that MOST participants without knee OA were at higher risk to develop it. Those at higher risk to develop knee OA are of particular public health importance (9), and it is crucial to understand the relationship of alignment to incident OA in them. Varus alignment was associated with incident OA by the established definition. We lacked sufficient power to separately examine incidence within K/L 0 and 1 strata. With or without these analyses, it cannot be concluded from any radiographic study that any factor initiates knee OA, given the insensitivity of x-rays to early OA pathology and the inability to identify the point of OA onset. Although there is no consensus as yet about what knee MRI feature(s) constitute OA, future studies should explore the relationship between alignment and OA development in knees without MRI-based measures of OA pathology. We were not able to assess change in alignment between baseline and follow-up. Those who did not complete the 30-month visit had a higher BMI; it is uncertain what impact this may have had on the results.
In conclusion, varus but not valgus alignment increased the risk of incident radiographic tibiofemoral OA. In knees with established OA, varus and valgus alignment each increased the risk of OA progression in the biomechanically stressed compartment and reduced the risk of progression in the unloaded compartment.
Acknowledgments
Support:
NIH NICHD RO1 HD43500
NIA U01 AG18820, AG18832, AG18947, AG19069
Footnotes
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd to permit this article (if accepted) to be published in ARD and any other BMJPGL products and sublicenses such use and exploit all subsidiary rights, as set out in our license (http://ARD.bmjjournals.com/ifora/licence.pdf).
REFERENCES
- 1.Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25:367–377. [PubMed] [Google Scholar]
- 2.Sharma L, Song J, Felson DT, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 3.Felson DT, McLaughlin S, Goggins J, et al. Bone marrow edema and its relation to progression of knee osteoarthritis. Ann Intern Med. 2003;139:330–336. doi: 10.7326/0003-4819-139-5_part_1-200309020-00008. [DOI] [PubMed] [Google Scholar]
- 4.Cicuttini F, Wluka A, Hankin J, et al. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford) 2004;43:321–324. doi: 10.1093/rheumatology/keh017. [DOI] [PubMed] [Google Scholar]
- 5.Brouwer GM, van Tol AW, Bergink AP, et al. Association between Valgus and Varus Alignment and the Development and Progression of Radiographic Osteoarthritis of the Knee. Arthritis Rheum. 2007;56:1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 6.Sharma L, Eckstein F, Song J, et al. The relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum. 2008;58:1716–1726. doi: 10.1002/art.23462. [DOI] [PubMed] [Google Scholar]
- 7.Hunter DJ, Niu J, Felson DT, et al. Knee alignment does not predict incident osteoarthritis: the Framingham Osteoarthritis Study. Arthritis Rheum. 2007;56:1212–1218. doi: 10.1002/art.22508. [DOI] [PubMed] [Google Scholar]
- 8.Cerejo R, Dunlop DD, Cahue S, et al. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–2636. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 9.Felson DT, Nevitt MC. Epidemiologic studies for osteoarthritis: new versus conventional study design approaches. Rheum Dis Clin North Am. 2004;30:783–797. doi: 10.1016/j.rdc.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, Anderson JJ, Mainmark A, et al. Obesity and knee osteoarthritis: The Framingham Study. Ann Intern Med. 1988;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 11.Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34:1796–1801. [PubMed] [Google Scholar]
- 12.Sled EA, Sheehy LM, Felson DT, et al. Reliability of lower limb alignment measures using an established landmark-based method with a customized computer software program. Rheumatology. :in press. doi: 10.1007/s00296-009-1236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Segal NA, Torner JC, Felson D, et al. Effect of thigh strength on incident radiographic and symptomatic knee osteoarthritis in a longitudinal cohort. Arthritis Rheum. 2009;61:1210–1217. doi: 10.1002/art.24541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma L, Lou C, Felson DT, et al. Laxity in healthy and osteoarthritic knees. Arthritis Rheum. 1999;42:861–870. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 15.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32:128–132. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 16.LaValley MP, McLaughlin S, Goggins J, et al. The lateral view radiograph for assessment of the tibiofemoral joint space in knee osteoarthritis: its reliability, sensitivity to change, and longitudinal validity. Arthritis Rheum. 2005;52:3542–3547. doi: 10.1002/art.21374. [DOI] [PubMed] [Google Scholar]
- 17.Felson DT, Nevitt MC. Blinding images to sequence in osteoarthritis: evidence from other diseases. Osteoarthritis Cartilage. 2009;17:281–283. doi: 10.1016/j.joca.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altman R, Hochberg M, Murphy W, et al. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3(A):3–70. [PubMed] [Google Scholar]
- 19.Felson DT, Nevitt MC, Yang M, et al. A new approach yields high rates of x-ray progression in knee osteoarthritis. J Rheumatol. 2008;35:2047–2054. [PMC free article] [PubMed] [Google Scholar]
- 20.Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25:395–403. [PubMed] [Google Scholar]
- 21.Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3:51–61. doi: 10.1016/0021-9290(70)90050-3. [DOI] [PubMed] [Google Scholar]
- 22.Hurwitz DE, Ryals AB, Case JP, et al. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res. 2002;20:101–107. doi: 10.1016/S0736-0266(01)00081-X. [DOI] [PubMed] [Google Scholar]
- 23.Miyazaki T, Wada M, Kawahara H, et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsu RWW, Himeno S, Coventry MB, et al. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop. 1990;255:215–227. [PubMed] [Google Scholar]
- 25.Bruns J, Volkmer M, Luessenhop S. Pressure distribution at the knee joint. Influence of varus and valgus deviation without and with ligament dissection. Arch Orthop Trauma Surg. 1993;133:12–19. doi: 10.1007/BF00440588. [DOI] [PubMed] [Google Scholar]
- 26.Johnson F, Leitl S, Waugh W. The distribution of load across the knee. A comparison of static and dynamic measurements. J Bone Joint Surg. 1980;62-B:346–349. doi: 10.1302/0301-620X.62B3.7410467. [DOI] [PubMed] [Google Scholar]
- 27.Harrington IJ. Static and dynamic loading patterns in knee joints with deformities. J Bone Joint Surg. 1983;65-A:247–259. doi: 10.2106/00004623-198365020-00016. [DOI] [PubMed] [Google Scholar]